Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: D'Hooghe E, Vujanic GM. Congenital mesoblastic nephroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumormesoblastic.html. Accessed September 2nd, 2025.
Definition / general
- Mesoblastic nephroma is a mesenchymal / myofibroblastic renal tumor of low grade malignancy
- It typically occurs in infancy, often congenital but not always
- First described by Bolande et al. in 1967 (Pediatrics 1967;40:272)
Essential features
- Most common renal tumor in the first month of life
- 90% of cases diagnosed in the first 9 months of life
- Virtually never after 3 years of age
- Adult mesoblastic nephroma does not exist
- 3 histologic subtypes: classic (~25% of cases), cellular (~65%) and mixed (~10%)
- Cellular type: ETV6-NTRK3 gene fusion in ~70% of cases
- Classic type: EGFR internal tandem duplication mutation
- Most important prognostic factor is completeness of surgical resection
Terminology
- Historic synonyms: renal leiomyomatous hamartoma, congenital mesoblastic nephroma
- Although "congenital" is a part of the WHO stated name for this tumor, it is sometimes a misnomer as the tumor is not always present from birth
ICD coding
Epidemiology
- Represents 3 - 4% of all renal tumors of childhood (Pediatr Blood Cancer 2011;56:744)
- Most common renal tumor in the first month of life (Pediatr Blood Cancer 2008;50:1130)
- 90% of cases occur in the first 9 months of life (Pediatr Blood Cancer 2008;50:1130)
- Median age < 1 month in 63% of cases (Pediatr Blood Cancer 2017;64:e26437)
- Median age differs between classic (7 days), mixed (1.9 months) and cellular (4.6 months) types (Pediatr Blood Cancer 2011;56:744)
- Virtually never occurs after the age of 3 years (Pediatr Blood Cancer 2017;64:e26437)
- Adult mesoblastic nephroma does not exist
- Not associated with syndromes or congenital anomalies
Sites
- Kidney; never bilateral, never multifocal
Pathophysiology
- Unknown
Etiology
- No recognized risk factors
- No familial cases have been reported
- Cellular type associated with t(12;15)(p13;q25) in ~70% of cases (Pediatr Blood Cancer 2018;65:e26925)
- Classic type associated with EGFR internal tandem duplication mutation (Histopathology 2020;77:611)
- Not associated with nephrogenic rests
Clinical features
- Abdominal mass (~75% of patients) (Pediatr Blood Cancer 2017;64:e26437)
- ~15% detected prenatally, usually associated with polyhydramnios
- Hypertension (~20%)
- Hematuria (~10%)
- Never presents as metastatic or bilateral disease
- Virtually never associated with syndromes or anomalies typical for Wilms tumor
Diagnosis
- Imaging techniques cannot distinguish it from other renal tumors (J Pediatr Surg 2008;43:1301)
- Biopsy not recommended
- Diagnosis made on nephrectomy
Laboratory
- No specific laboratory findings
- Hypercalcemia (4% of cases)
- Hyperreninemia (1% of cases) (Pediatr Blood Cancer 2017;64:e26437)
Radiology description
- Unilateral, well demarcated, hypoechogenic mass
Prognostic factors
- Most important prognostic factor is completeness of surgical resection
- Histologic type is of no prognostic significance
- Overall survival reported as ~96% but is almost certainly higher since cases with unfavorable outcome are more likely to be reported (Pediatr Blood Cancer 2008;50:1130)
- Of 12/276 patients with mesoblastic nephroma who died, 5 died of tumor related and 7 of treatment related causes (Pediatr Blood Cancer 2017;64:e26437)
- Very rare local relapses and metastases; 38 cases reported in the literature (Pediatr Surg Int 2017;33:1183)
- Relapses and metastases occur within 12 months after the diagnosis (range 1 - 12 months, median 6 months)
- Local relapses in 27/38 (71%) of these cases
- 21/27 (76%) had incomplete resection (stage 3)
- All but 1 patient had cellular type but even then, cellular type had no significant difference in prognosis
- Metastases developed in 18 children (7 also had local recurrence)
- Lung metastases in 7/18 (39%), liver in 5/18 (28%), brain in 4/18 (22%) and heart, bone and peritoneum in 5.5% each
- 38% of patients with metastases died (all who had brain, bone, heart and peritoneum metastases)
Case reports
- Prematurely born boy presented with neonatal hypertension (Turk J Pediatr 2018;60:198)
- Prematurely born boy with a prenatal diagnosis of polyhydramnios (Urol Case Rep 2015;3:157)
- 7 day old boy presented with abdominal distension and vomiting (J Neonatal Surg 2017;6:45)
- 11 month old boy presented with a renal mass (Urol Case Rep 2019;26:100979)
Treatment
- Complete surgical resection (total nephrectomy) with wide resection margins (Pediatr Blood Cancer 2017;64:e26437, Pediatr Surg Int 2017;33:1183)
- Even stages II and III treated with surgery only
- Relapses also treated with surgery
- Chemotherapy treatment of relapses only in unresectable cases
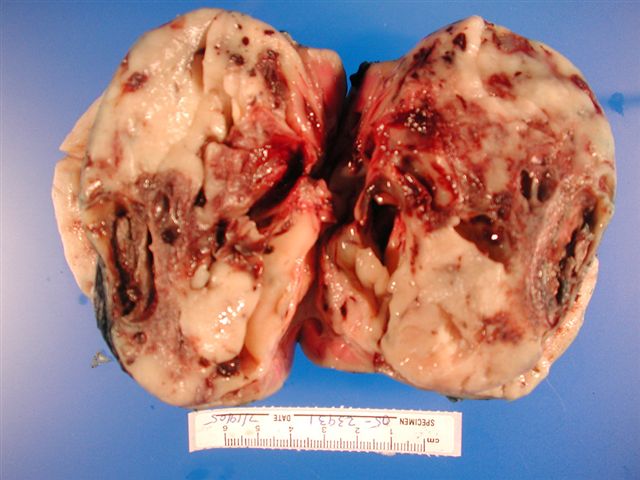
Gross description
- Always unilateral and solitary (Adv Anat Pathol 2003;10:243)
- Typically found in the medial renal sinus
- Classic type:
- Firm, whorled, leiomyomatous consistency
- Poorly demarcated from the normal renal parenchyma
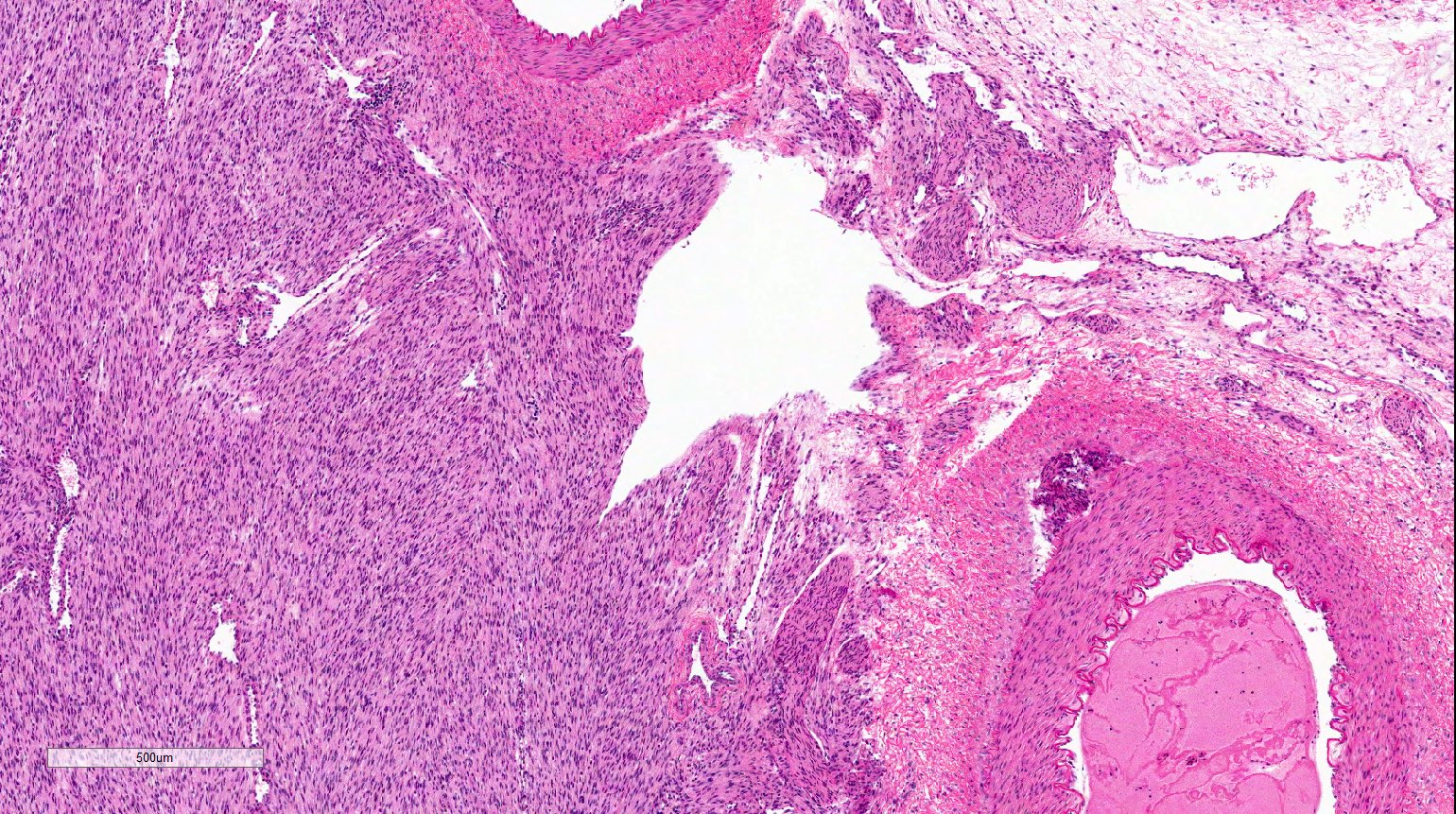
- Cellular type:
- Usually soft
- Tumor-kidney junction relatively clearly demarcated
- Cystic areas
- Can show hemorrhage and necrosis
Gross images
Microscopic (histologic) description
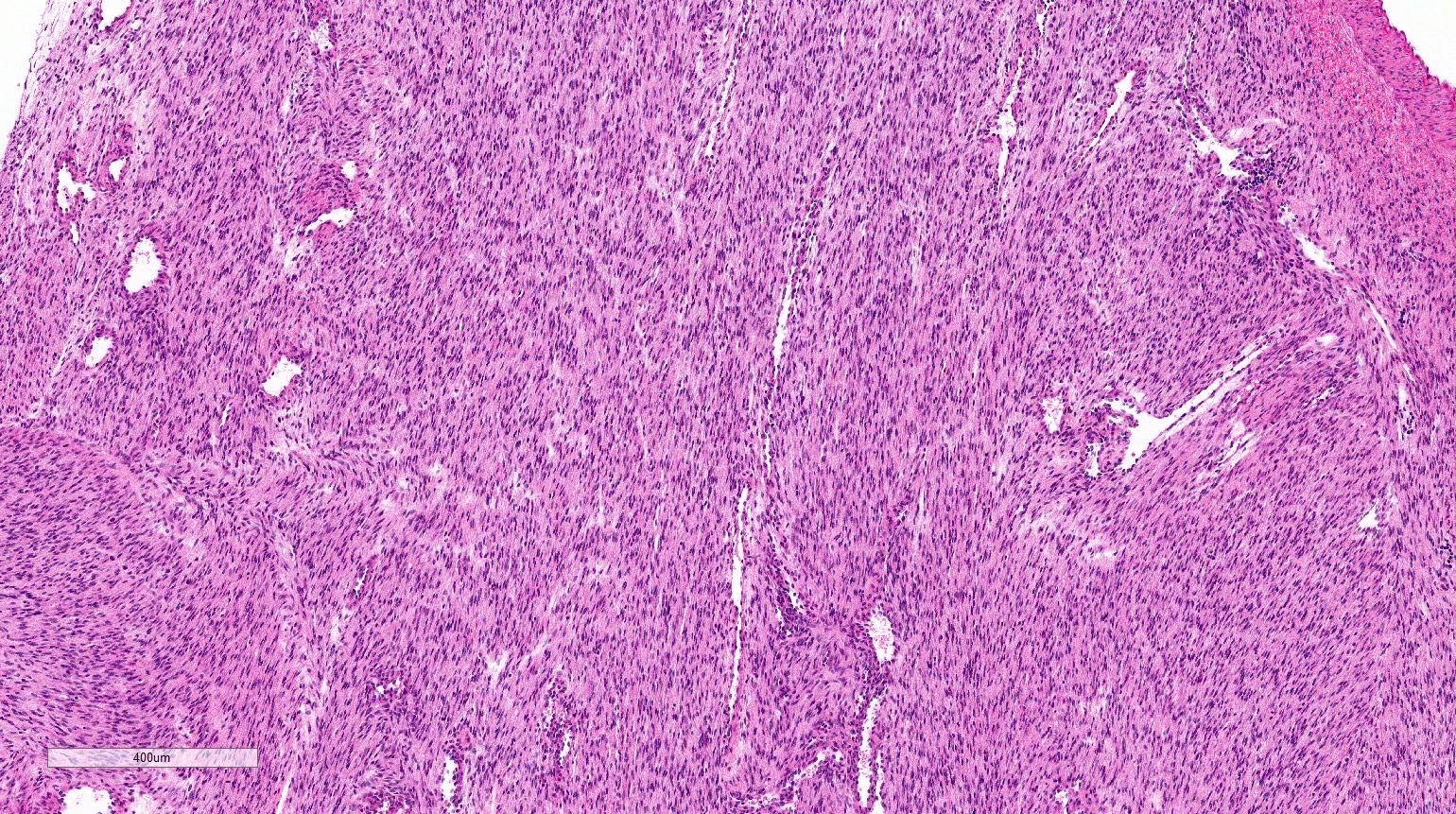
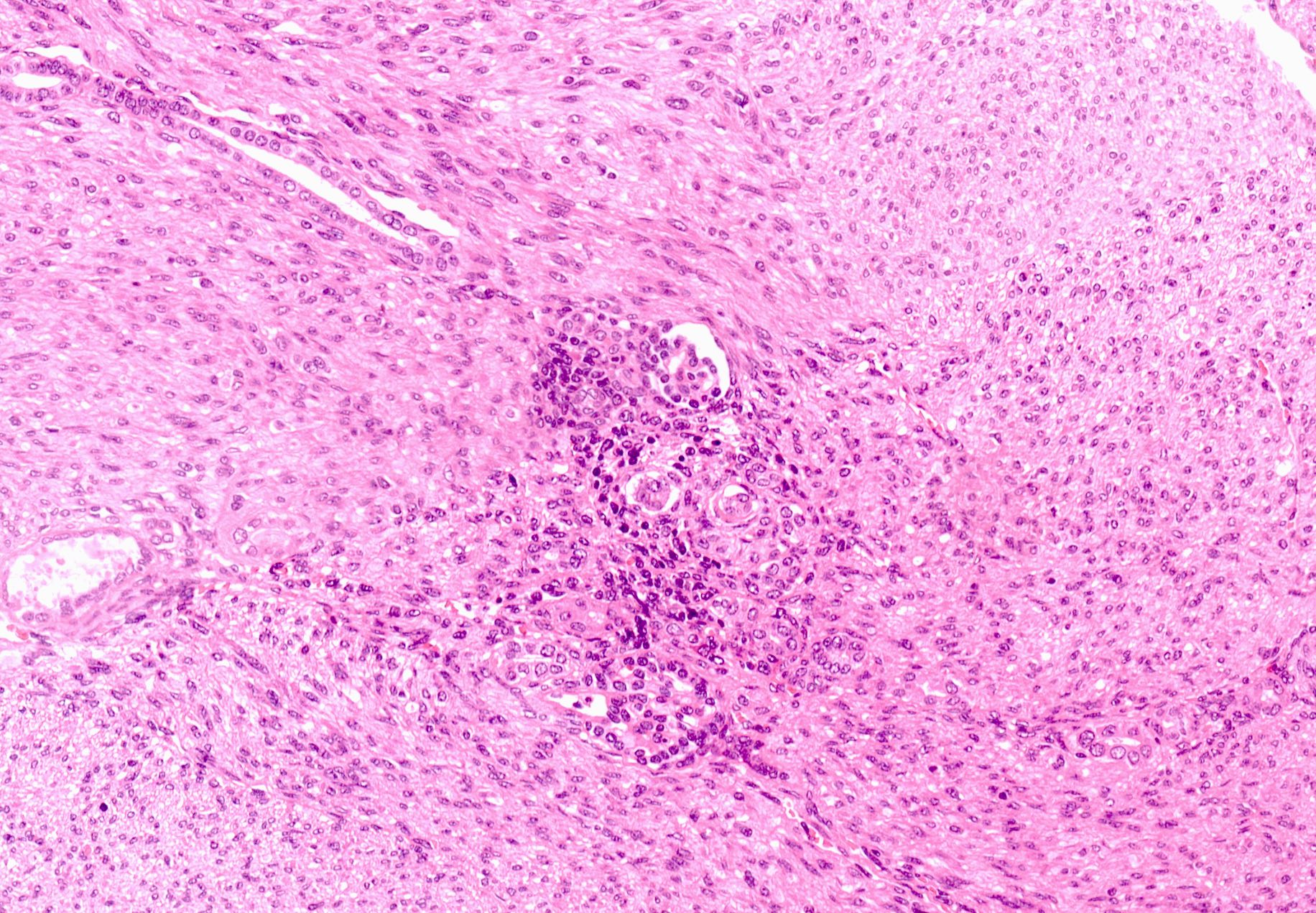
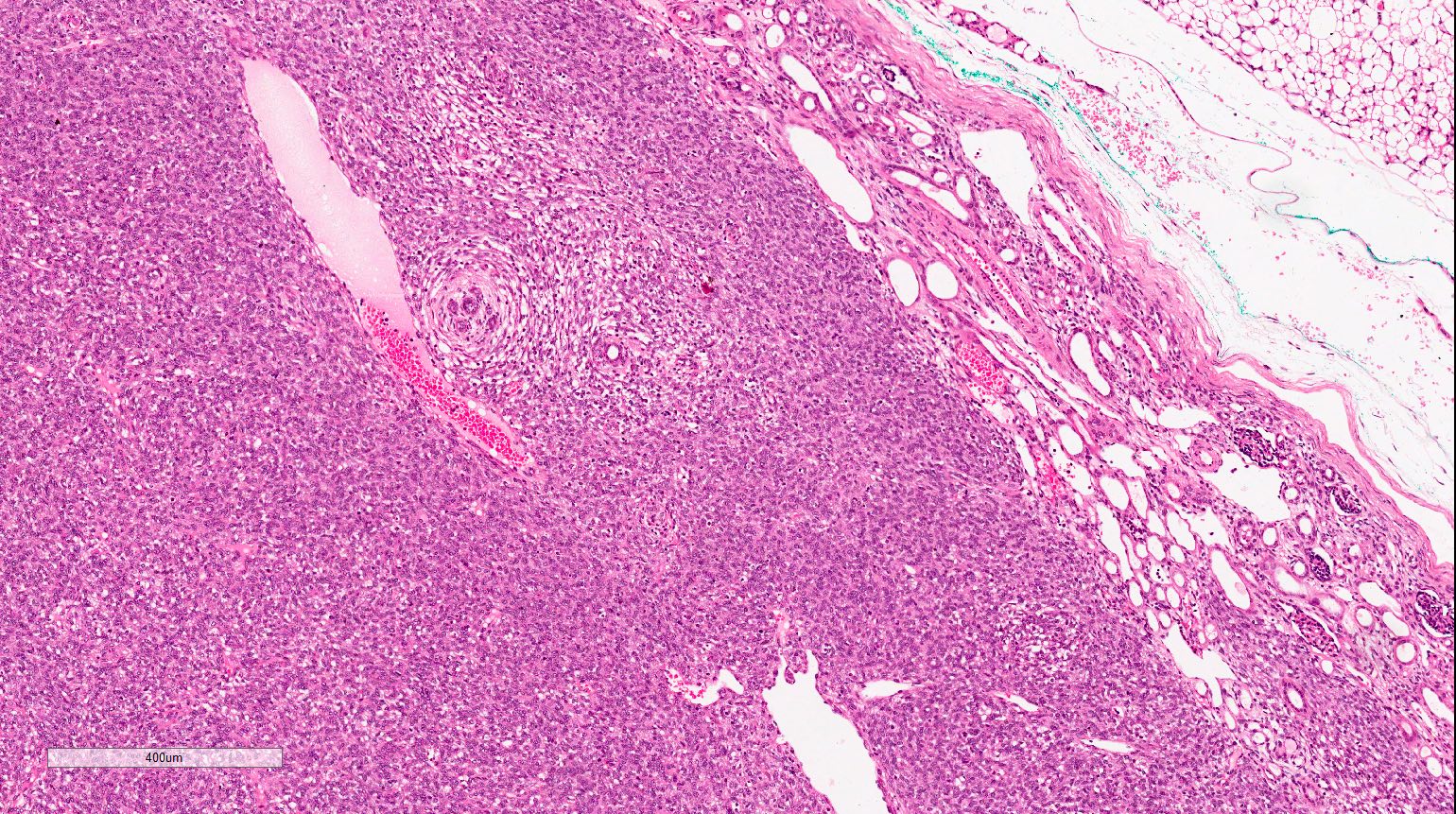
- Classic type (~25% of cases) (Adv Anat Pathol 2003;10:243, Histopathology 1985;9:741):
- Intermingling fascicles of spindle cells with low mitotic activity
- Collagen deposition
- Often prominent dilated, thin walled vascular spaces
- No capsule
- Tumor-kidney border is irregular with finger-like protrusions of the tumor into the renal parenchyma
- Islands of hyaline cartilage can be seen at the tumor-kidney interface
- Entrapped islands of renal parenchyma
- Foci of extramedullary hematopoiesis common
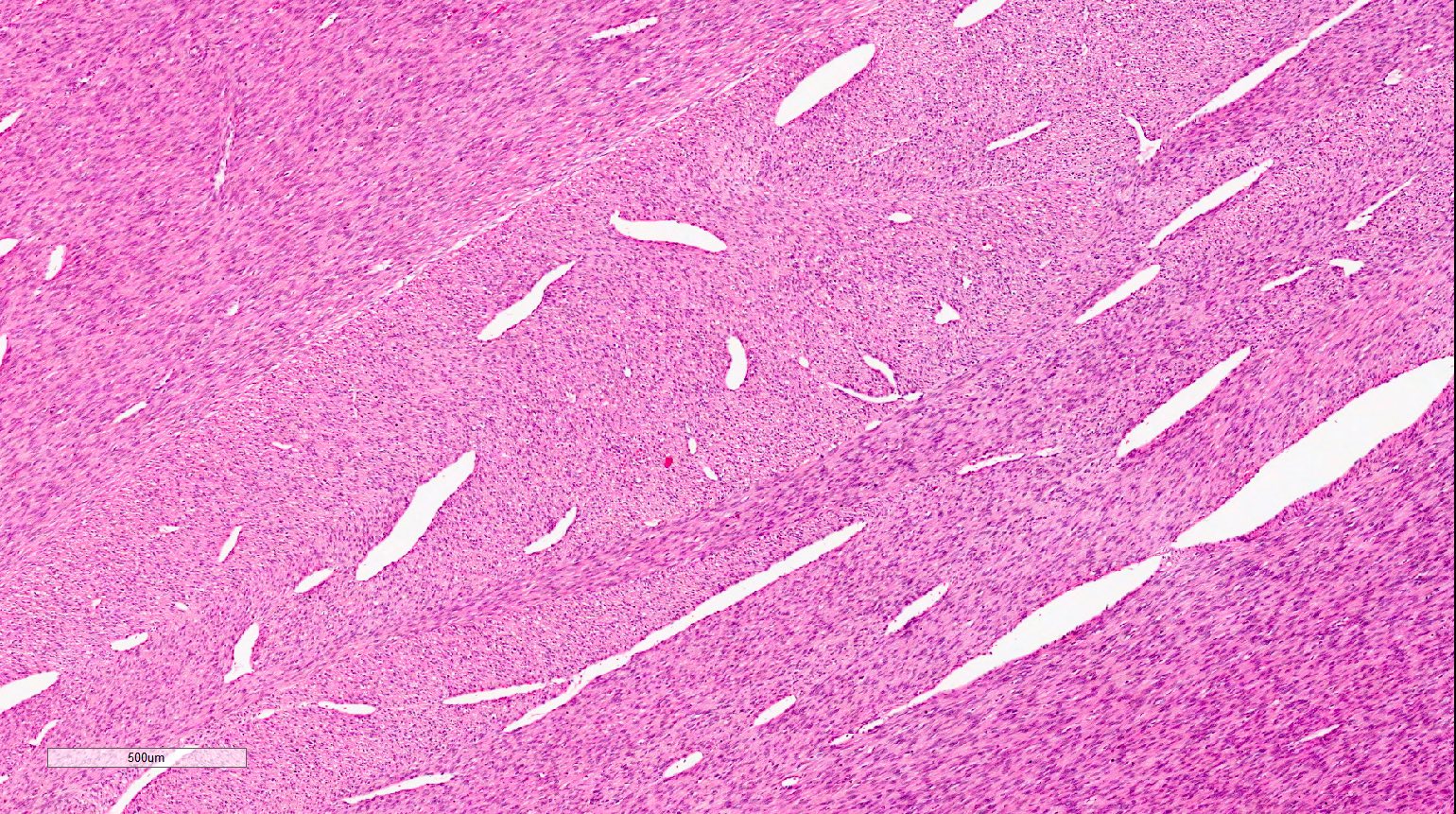
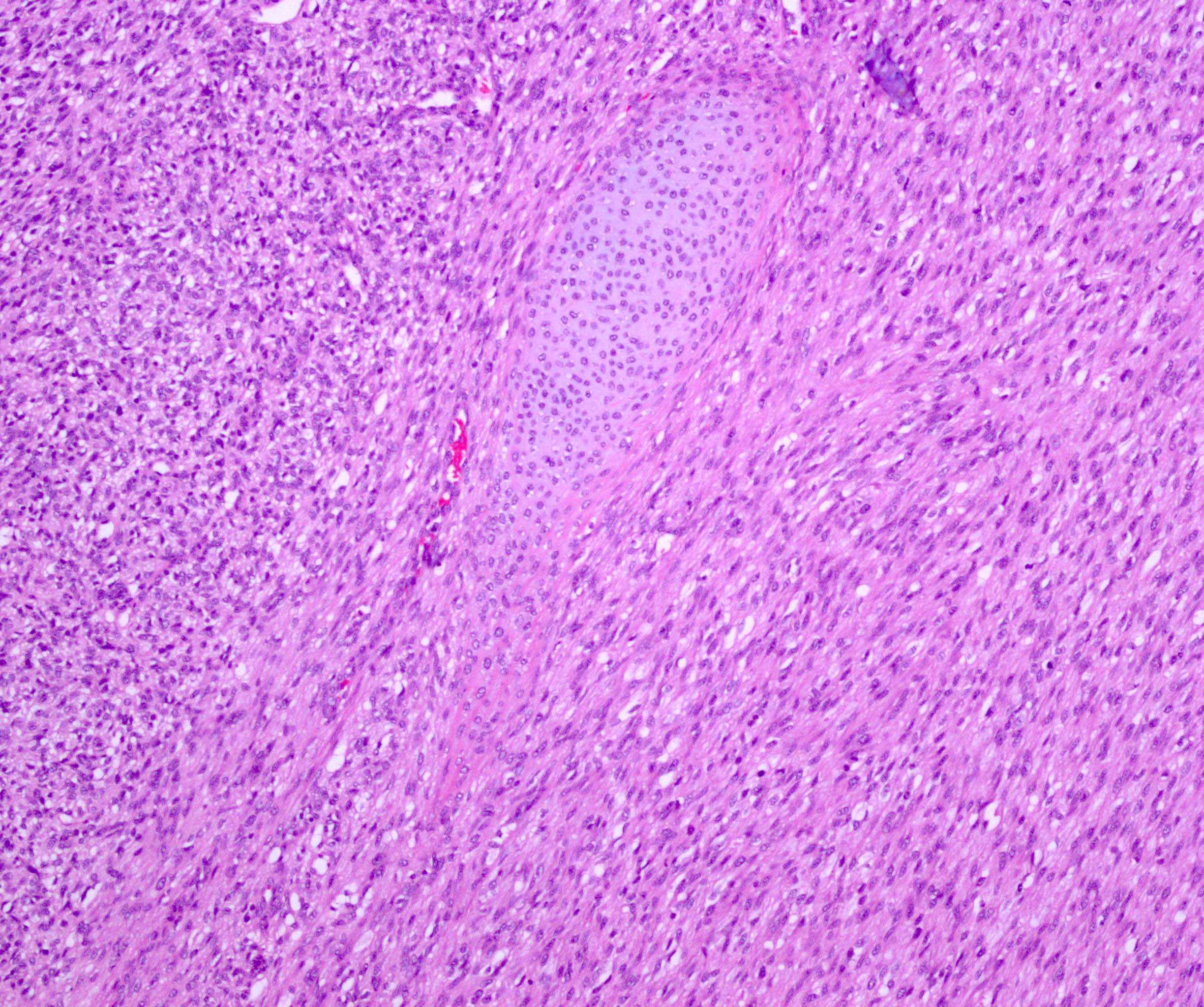
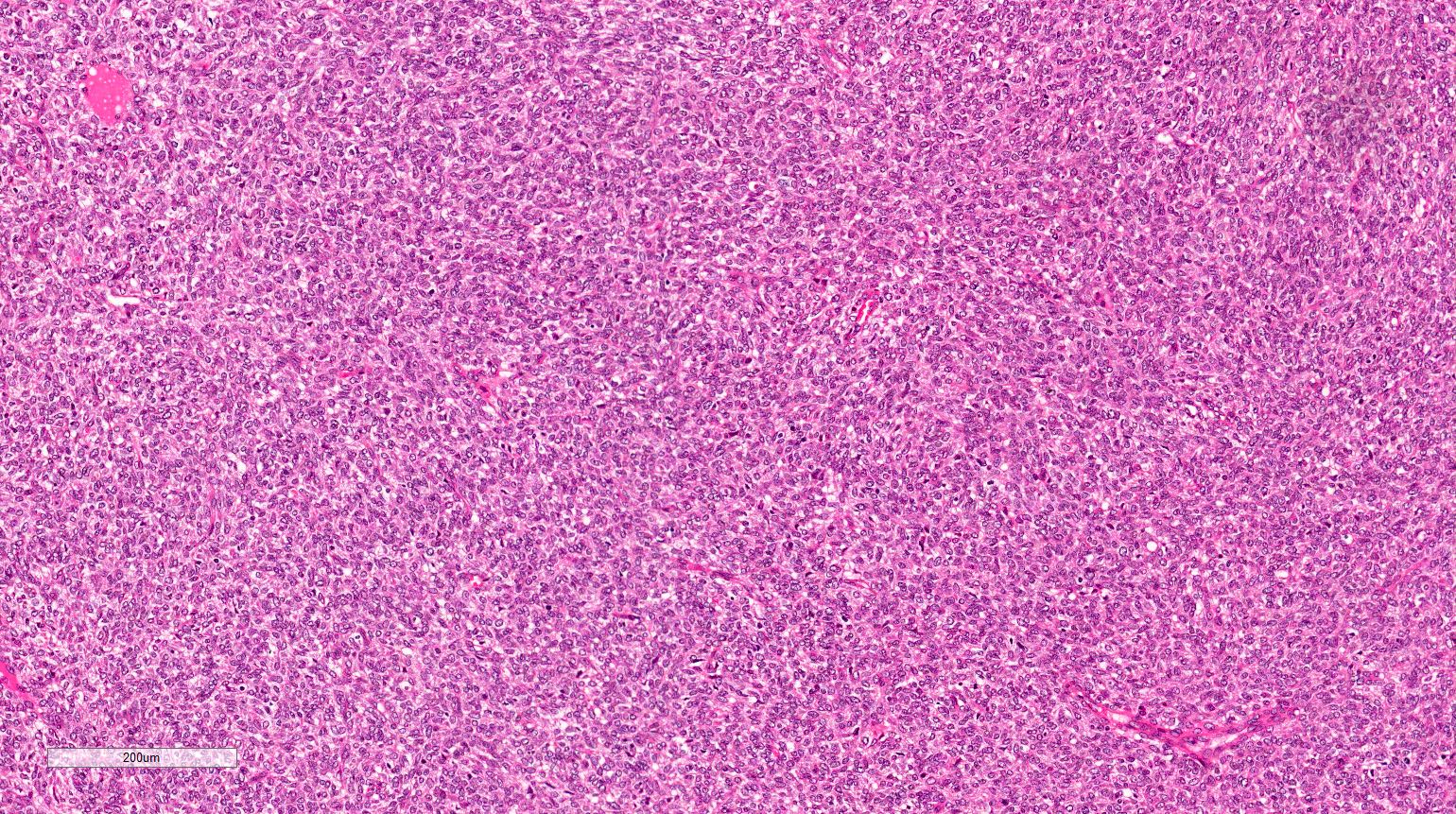
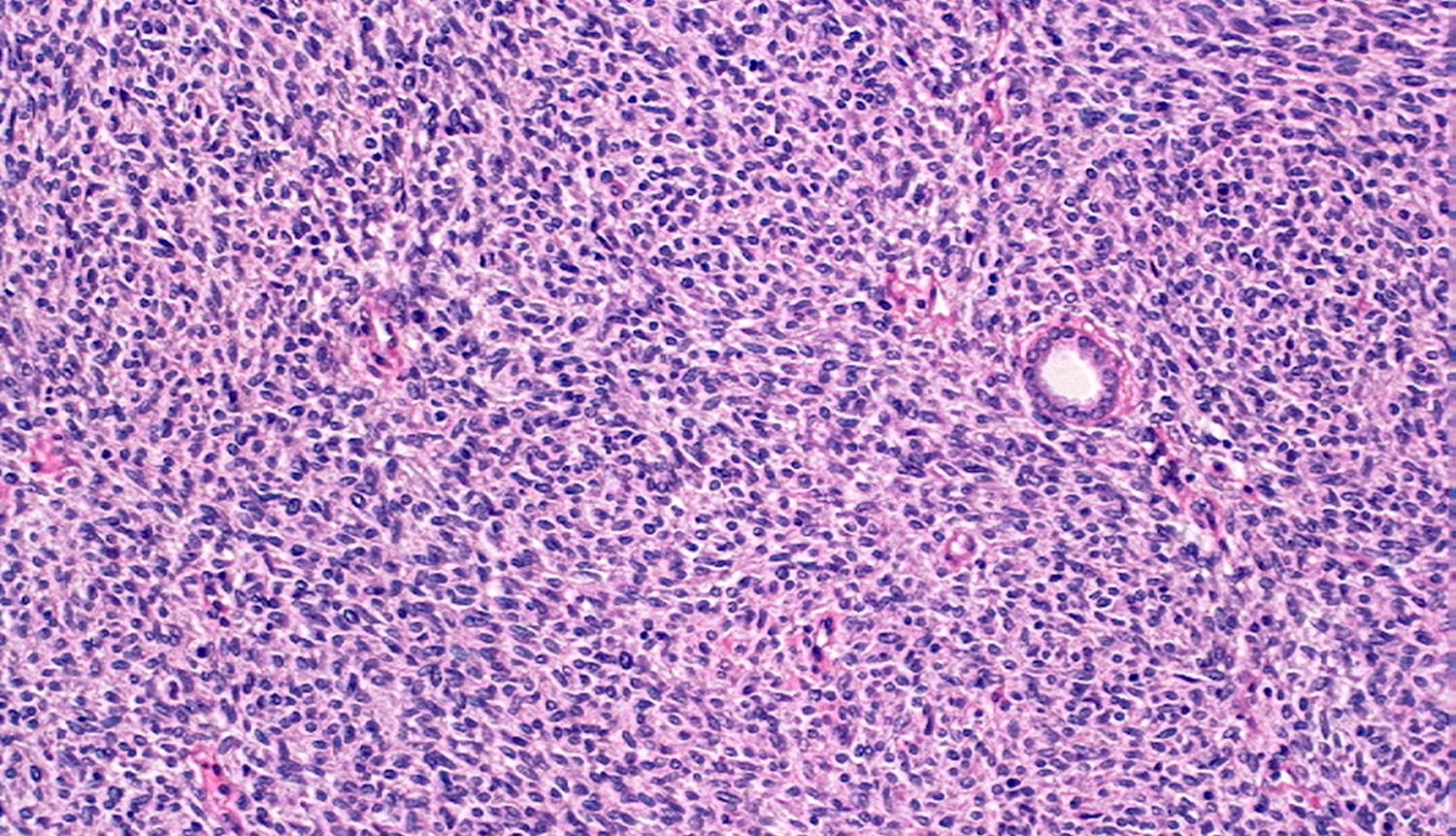
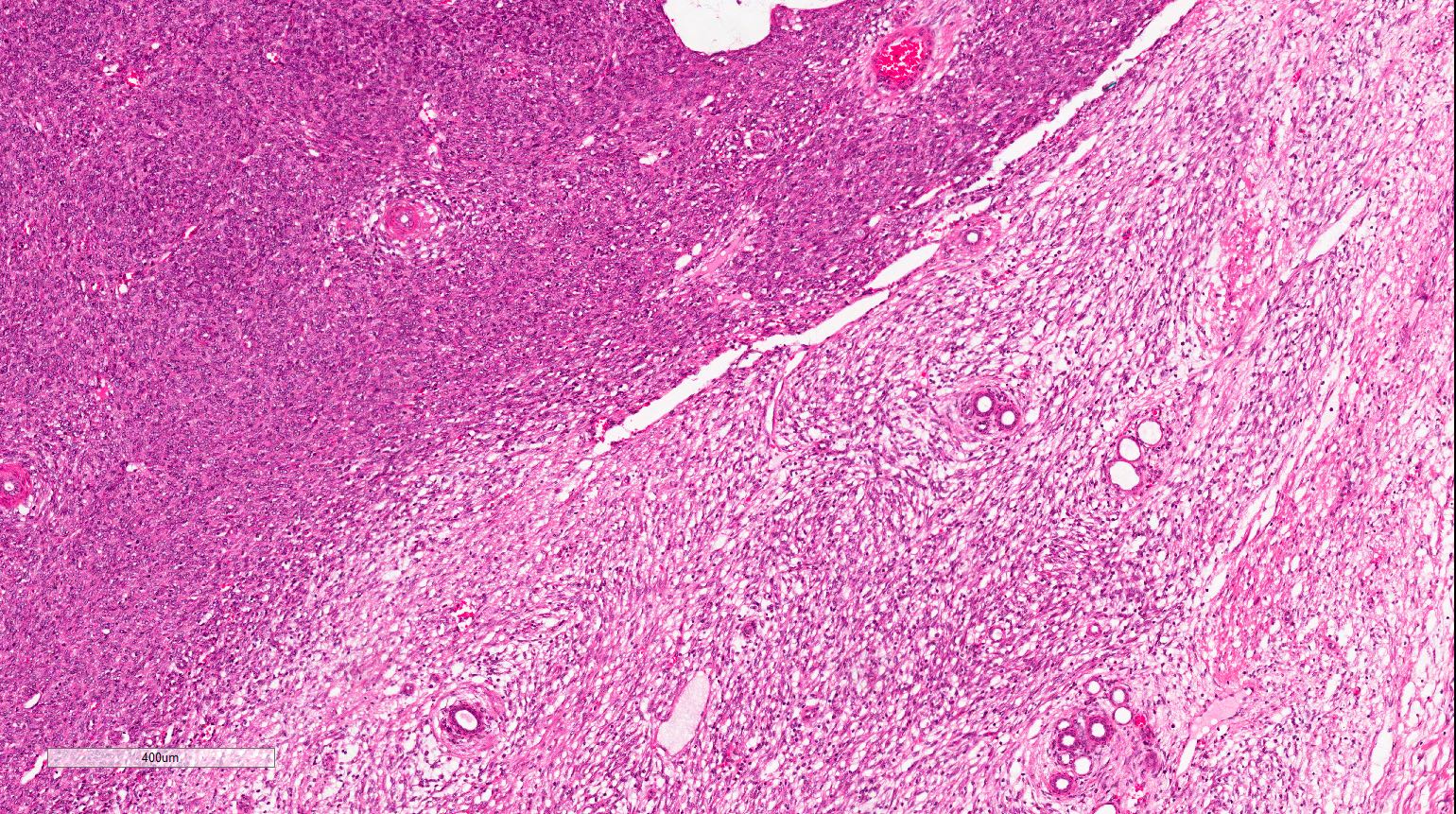
- Cellular type (~65% of cases):
- High cellularity of plump cells with vesicular nuclei, moderate amount of cytoplasm
- Sheet-like growth pattern
- High mitotic activity (which is of no prognostic significance)
- No capsule
- Clear tumor-kidney border but subtle infiltration into the renal parenchyma
- Isolated entrapped tubules, which may be mistaken for neoplastic tubules
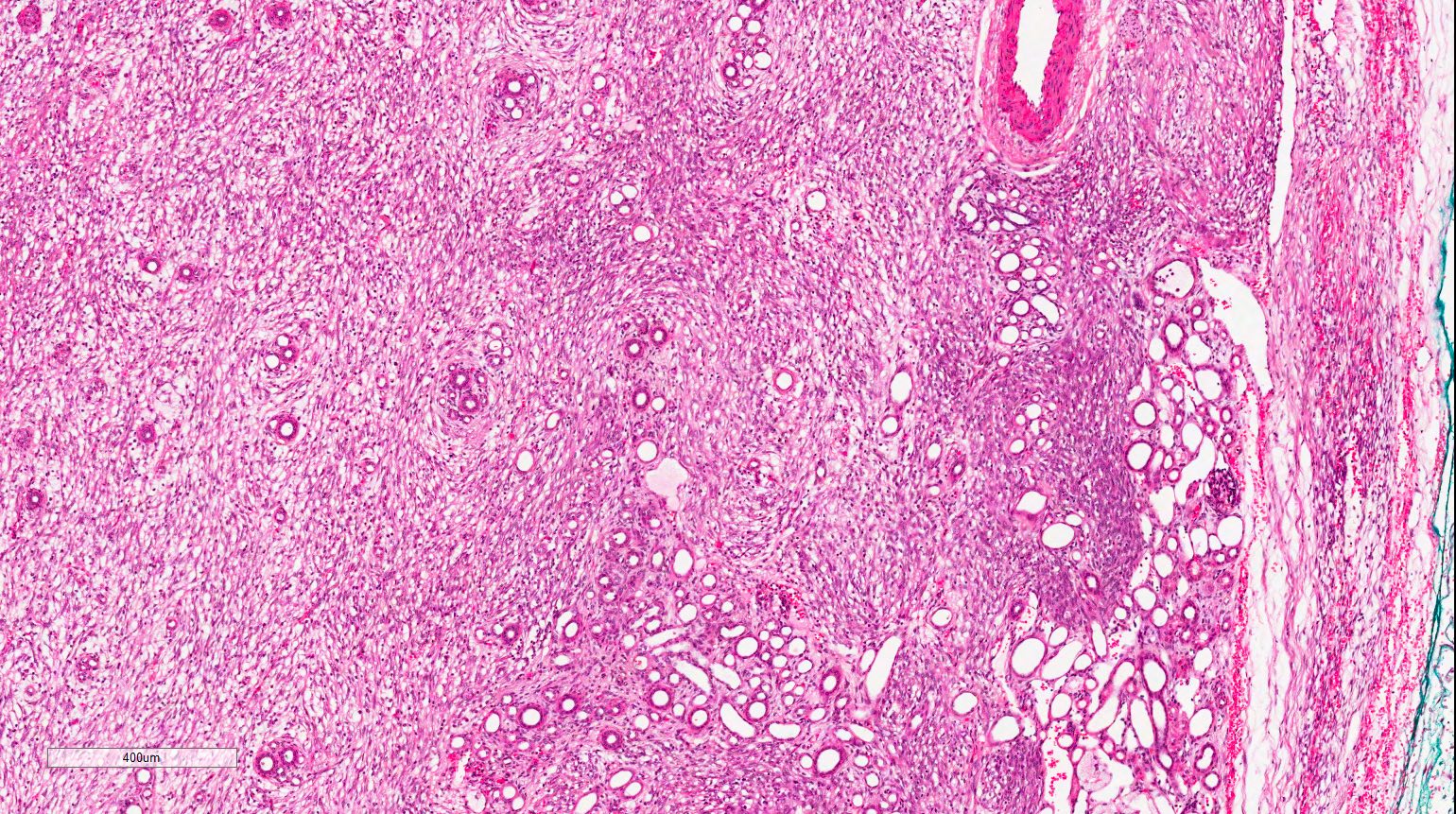
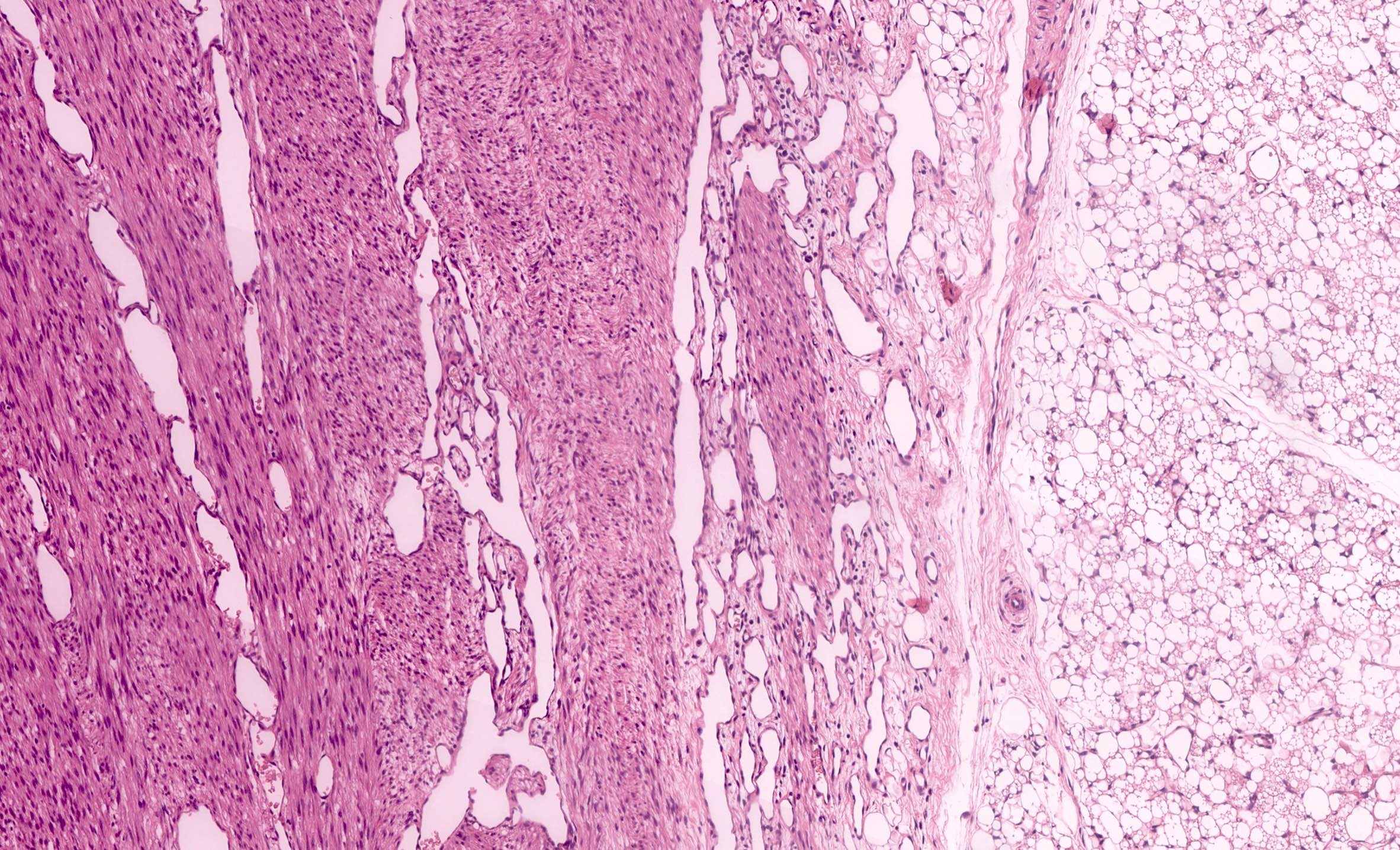
- Mixed type (~10% of cases):
- Features of both types in a variable proportion
- Staging criteria are as for nephroblastoma
- Vast majority are stage 2 due to tumor's infiltrative growth into the renal sinus or perirenal fat
Microscopic (histologic) images
Contributed by Ellen D’Hooghe, M.D. and Gordan M. Vujanic, M.D., Ph.D.
Cytology description
- Fine needle aspiration is not indicated
Positive stains
- Cyclin D1: diffuse in ~70% of cases (Histopathology 2015;67:306)
- Pan-TRK: cytoplasmic or nuclear positivity in cellular type with ETV6-NTRK3 gene fusion (Am J Surg Pathol 2018;42:927)
- Alpha smooth muscle actin
- Vimentin
Negative stains
Molecular / cytogenetics description
- Cellular type:
- Specific chromosomal translocation t(12;15)(p13;q25), which results in a fusion of ETV6 and NTRK3 genes in ~70% of cases (Pediatr Blood Cancer 2017;64:e26925)
- The same translocation is found in infantile fibrosarcoma (Mod Pathol 2000;13:29, Mod Pathol 2001;14:1246)
- Few cases reported with EGFR internal tandem duplication (ITD) mutation (Nat Commun 2018;9:2378)
- Rare cases with BRAF rearrangements but not BRAF V600E mutation (Histopathology 2020;77:611, Nat Commun 2018;9:2378)
- Classic type: EGFR ITD mutation is a consistent and recurrent genetic event (Histopathology 2020;77:611)
- Mixed type: may have either EGFR ITD or ETV6-NTRK3 gene fusion
Sample pathology report
- Right kidney, total nephrectomy:
- Mesoblastic nephroma, cellular type, stage II (due to renal sinus and perirenal fat invasion) (see comment)
- Comment: Tumor shows dense cellularity with plump cells with vesicular nuclei and with a high mitotic activity. Tumor is infiltrating the renal sinus and perirenal fat but is not reaching the resection margins. Lymph nodes are free of tumor.
Differential diagnosis
- Metanephric stromal tumor:
- Alternating, nodular cellularity, angiodysplasia, onion skinning
- CD34+
- BRAF V600E mutation
- Stromal type Wilms tumor:
- Often rhabdomyoblasts and adipose tissue
- Often associated with nephrogenic rests
- More sampling might reveal epithelial and or blastemal elements
- BCL2+
- Clear cell sarcoma of the kidney:
- Characteristic arborising vascular pattern
- BCOR+
- Rhabdoid tumor of the kidney:
- INI1 loss
- Inflammatory myofibroblastic tumor:
- ALK+
Additional references
Practice question #1
An 11 month old boy presents with an abdominal mass noticed by parents. Imaging studies show a right sided renal mass. Total right nephrectomy is performed. The tumor is composed of undifferentiated cells with no particular pattern, shown above. Which finding is most characteristic for this entity?
- BCOR+
- BRAF V600E mutation
- ETV6-NTRK3 gene fusion
- INI1 loss
Practice answer #1
C. ETV6-NTRK3 gene fusion. This is a mesoblastic nephroma, cellular type.
Comment Here
Reference: Congenital mesoblastic nephroma
Comment Here
Reference: Congenital mesoblastic nephroma
Practice question #2
Practice answer #2