Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Differential diagnosis | Additional referencesCite this page: Ozer E. Pleuropulmonary blastoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorPPB.html. Accessed April 20th, 2024.
Definition / general
- Pleuropulmonary blastoma (PPB) is a rare, primitive primary neoplasm of the thorax in young children
- The tumor, which is often but not always associated with cystic lung lesions, may arise in pulmonary parenchyma, the mediastinum and pleura
- It was initially proposed to be a distinct entity in 1988 (Cancer 1988;62:1516)
- An international registry has been established (ppbregistry.org)
Essential features
- Three subtypes of PPB exist (Types I, II and III), and are a continuum from the least to most malignant lesions (Cancer 2015;121:276, Pediatr Dev Pathol 2015;18:504)
- Type I is multicystic; it is now considered the same clinical and pathologic entity as CPAM (congenital pulmonary airway malformation) type IV (Neonatology 2017;111:76)
- Type II shows thickening areas (nodules) within this cystic lesion
- Type III shows solid masses
Terminology
- PPB
- Pneumoblastoma
- Mesenchymal cystic hamartoma
- Cystic mesenchymal hamartoma
- Pulmonary rhabdomyosarcoma
- Rhabdomyosarcoma in lung cyst
- Pediatric pulmonary blastoma
ICD coding
- M8973/3
Epidemiology
- PPB is encountered in childhood, mostly in the first years of life (90% are between 0 - 2 years old)
- Type I may be found in very young children (birth to 2 years of age)
- Types II and III tend to be found after 2 years of age (Pediatr Dev Pathol 2015;18:504)
Sites
- PPB may arise in the lung, mediastinum and pleura
Pathophysiology
- It arises from a primitive mesenchymal cell, likely a stem cell (Am J Surg Pathol 2008;32:282)
Etiology
- PPB is associated with PPB family tumor and dysplasia syndrome in 33% of cases
- Many of these patients have a mutation of the DICER1 gene (Cancer 2015;121:276)
Clinical features
- Children usually present with difficulty breathing or other respiratory problems including persistent pneumonitis, coughing or atelectasis
- 10% may also present with multilocular cystic nephroma and very rarely, Wilms tumor
Diagnosis
- MRI or CT can help diagnose, but biopsy is suggested
Radiology description
- Findings that favor PPB are a right sided, pleural based, peripherally located mass (Cancer Imaging 2009;9:1)
Prognostic factors
- The prognosis of PPB, especially Types II and III is poor because of frequent relapses and distant metastases which are often seen in the brain and bone (Pediatr Pulmonol 2015;50:698)
Case reports
- A neonate with pleuropulmonary blastoma and myelomeningocele (Fetal Diagn Ther 2016;39:234)
- 8 month old infant with difficulty feeding and shortness of breath (Case of the Week #166)
- 2 year old infant that first manifested as recurrent pneumothorax (J Pediatr Hematol Oncol 2012;34:e42)
- 3 year old boy with Type III PPB (Turk Patoloji Derg 2015;31:68)
- 44 month old child with PPB presenting as a solid and cystic mass (Fetal Pediatr Pathol 2014;33:1)
Treatment
- At present, the treatment of PPB is multimodal and includes surgery, chemotherapy or radiation therapy
- The combination depends on the type and aggressiveness of the disease (Pediatr Pulmonol 2015;50:698)
Gross description
- Type I PPB is a peripherally located, multicystic and thin walled structure
- Type II PPB is a mixed solid and cystic tumor characterized by variable thickened or nodule-like areas
- Type III PPB is characterized by a well circumscribed, mucoid, white-tan solid mass attached to the pleura and involves a lobe or entire lung; necrosis and hemorrhage may be present in the friable areas
Gross images
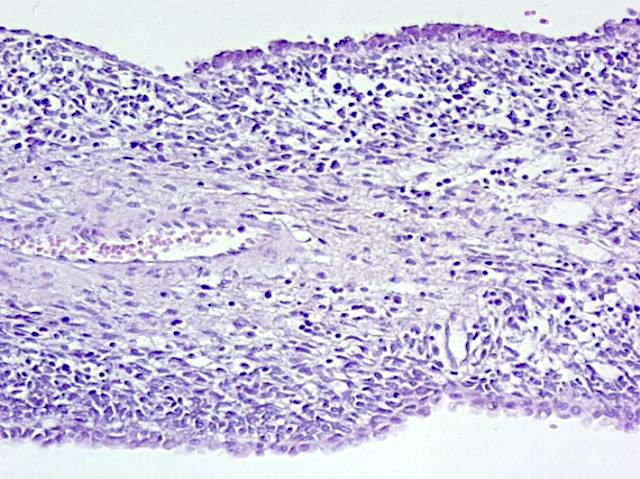
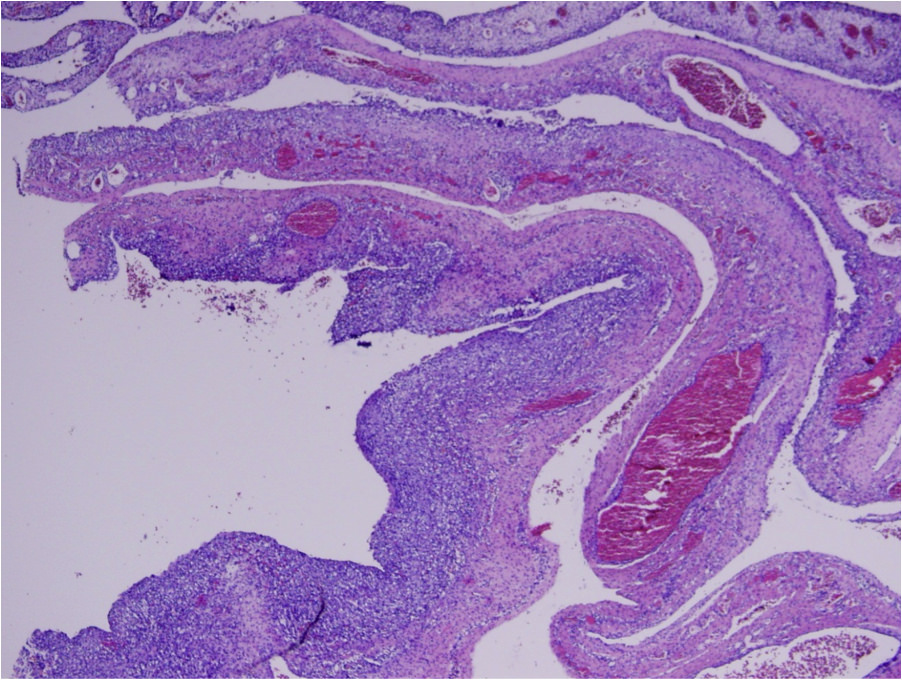
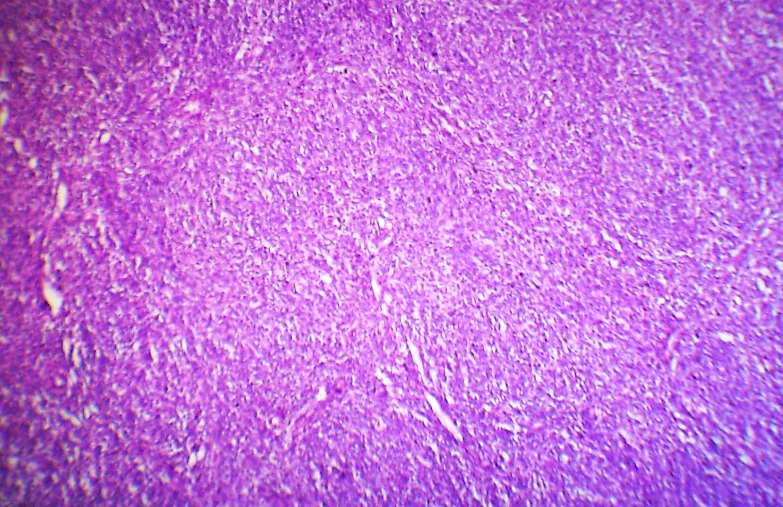
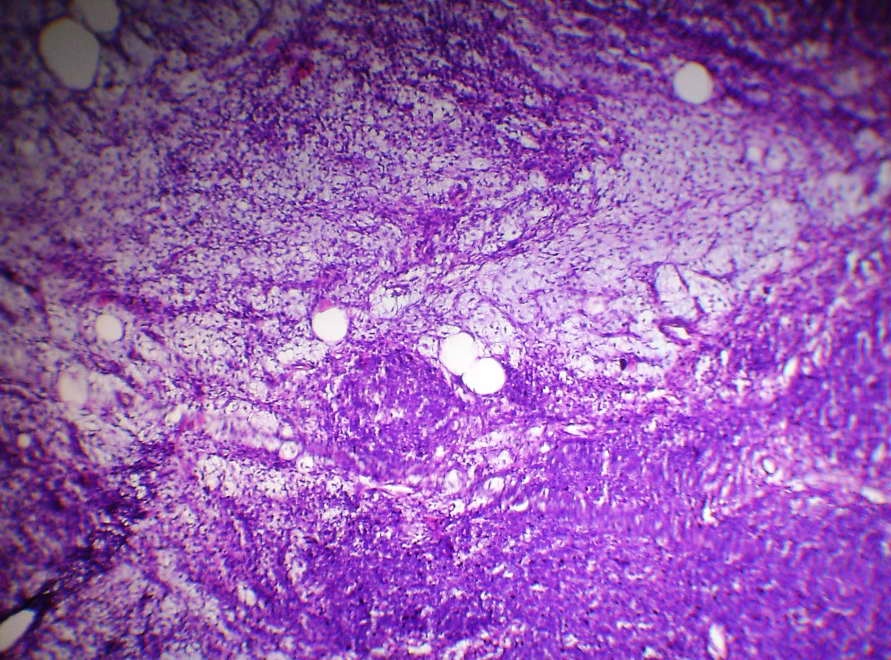
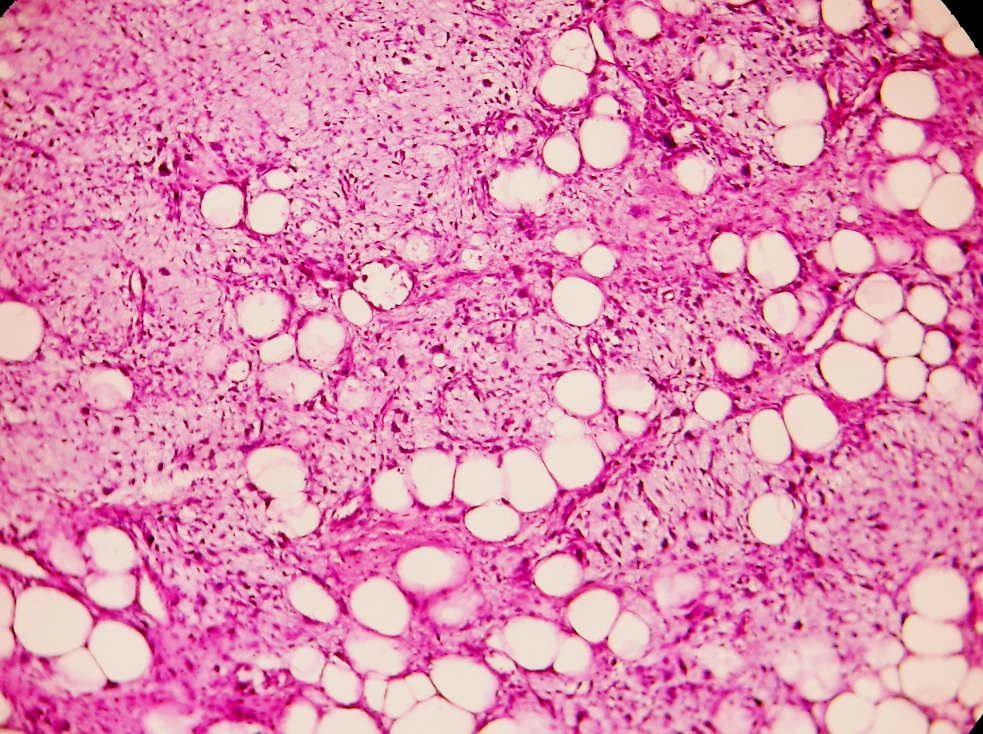
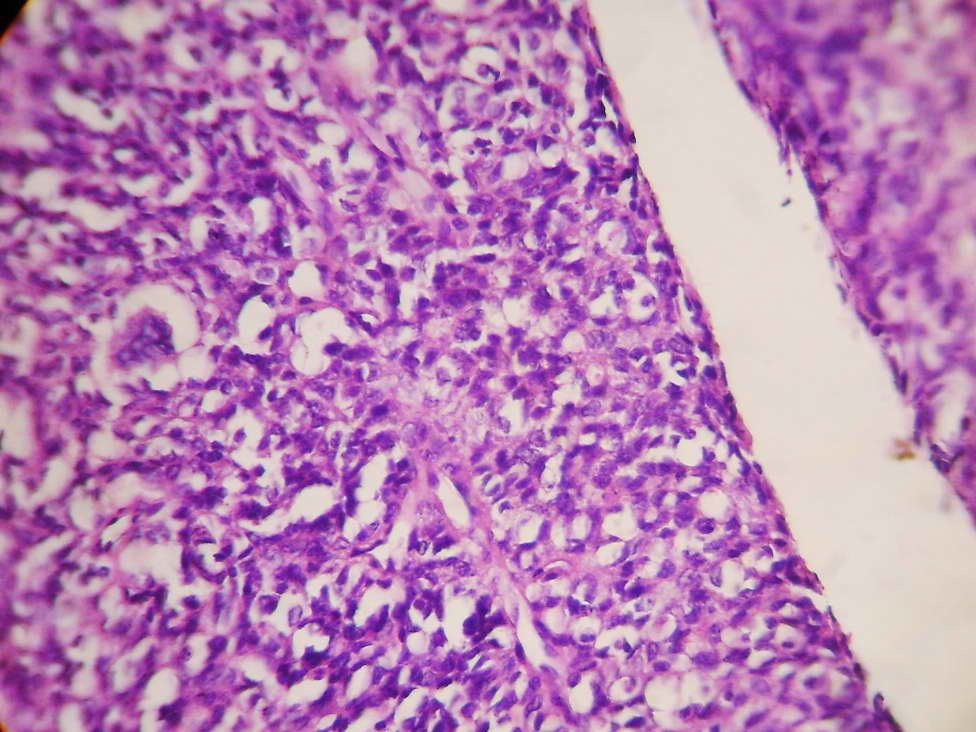
Microscopic (histologic) description
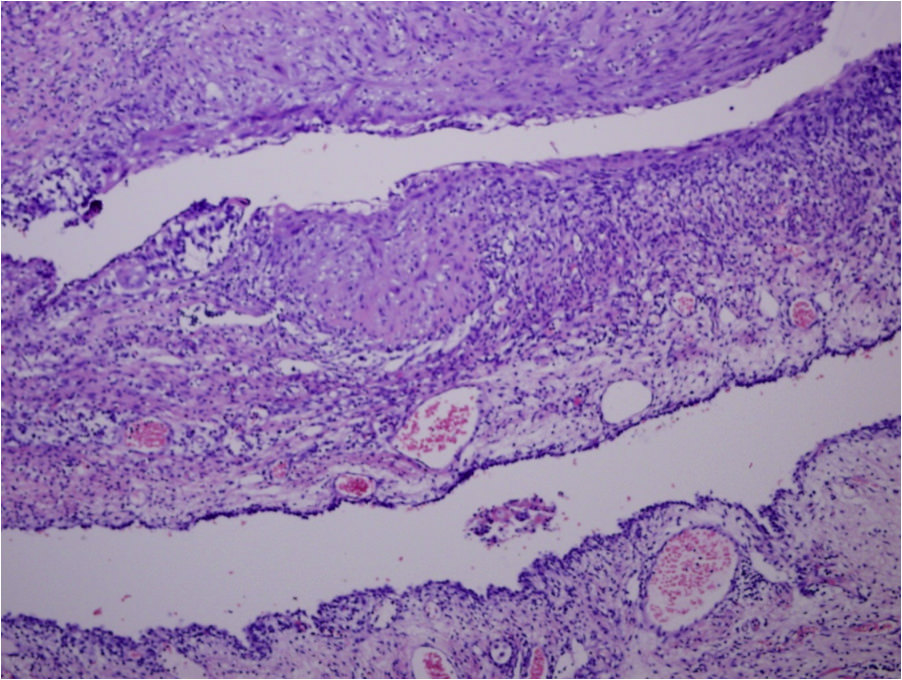
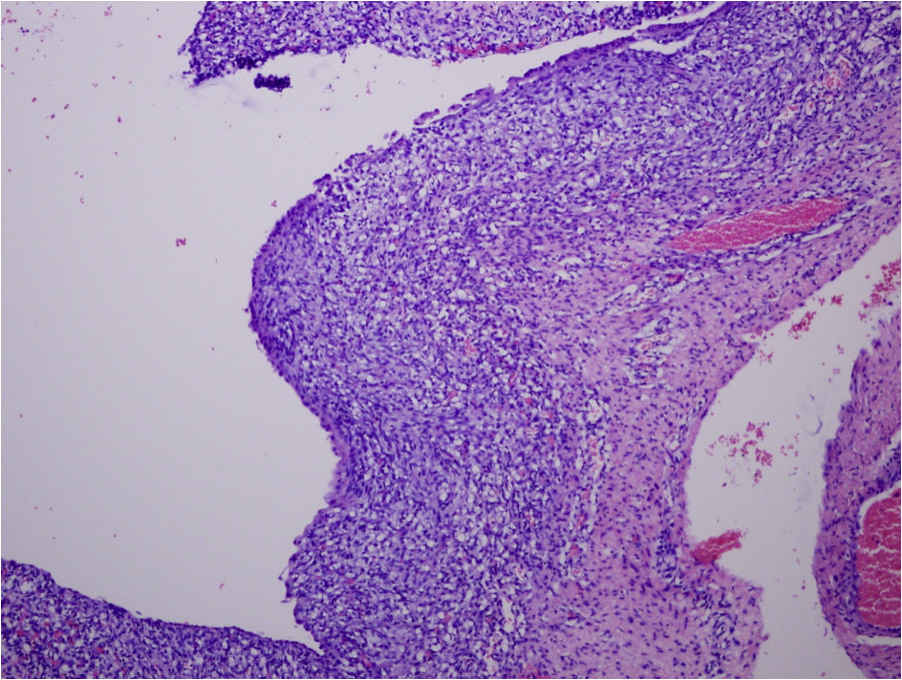
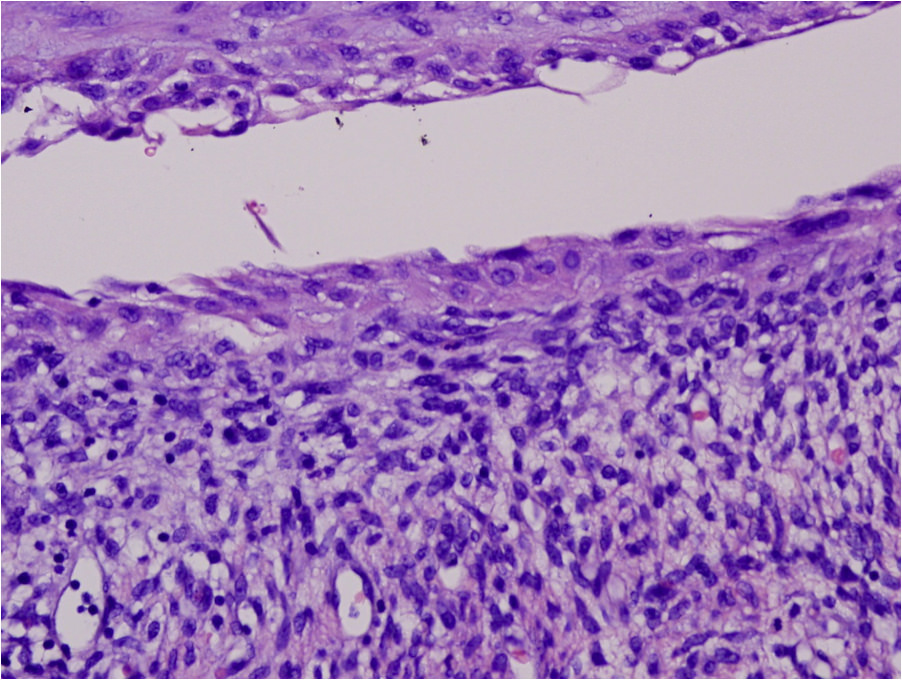
- Type I PPB is a peripherally located, multicystic and thin walled structure
- Type II PPB is a mixed solid and cystic tumor with variable thickened or nodule-like areas
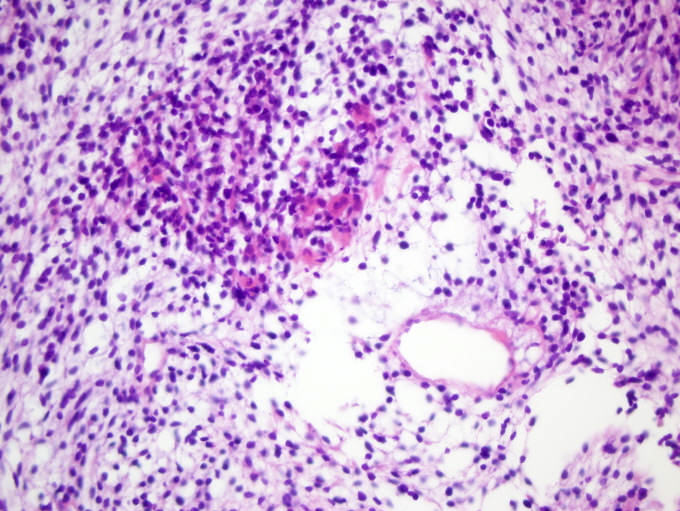
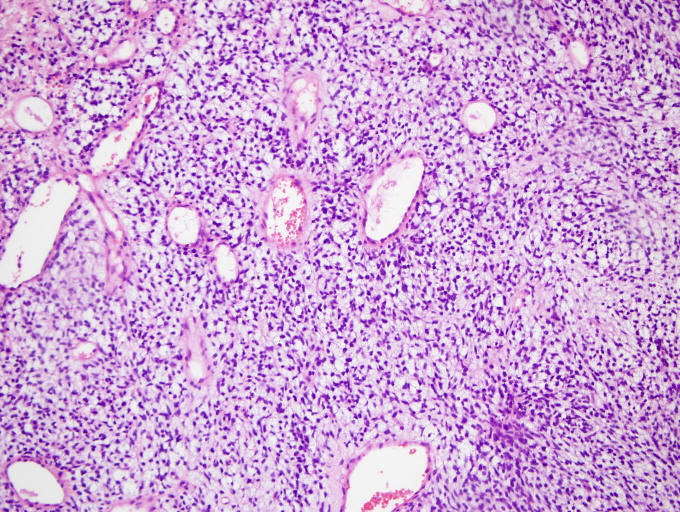
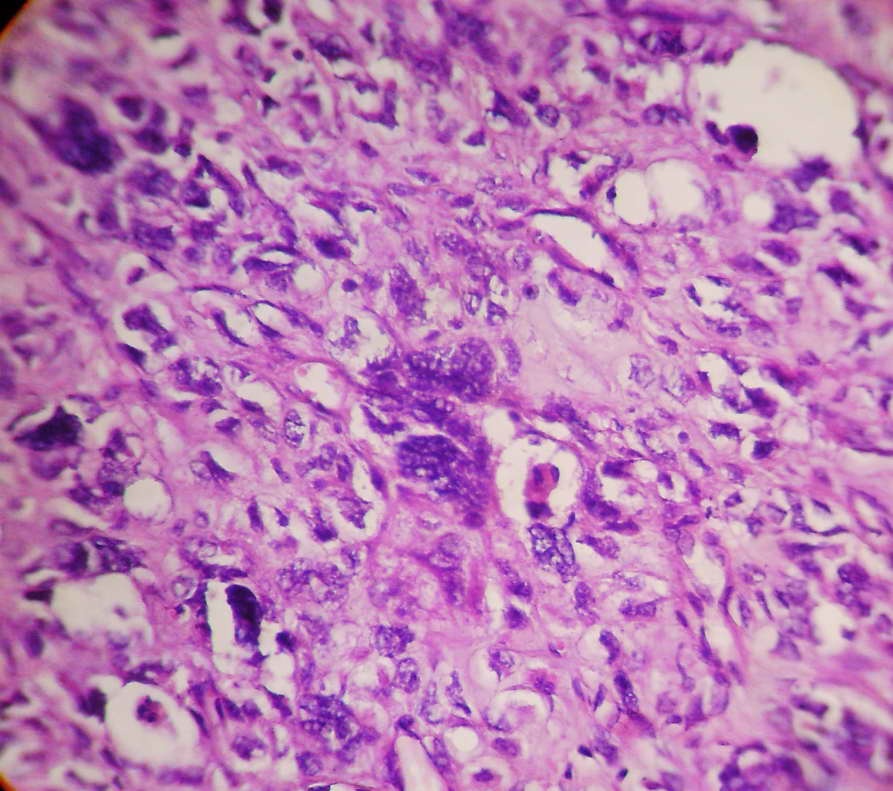
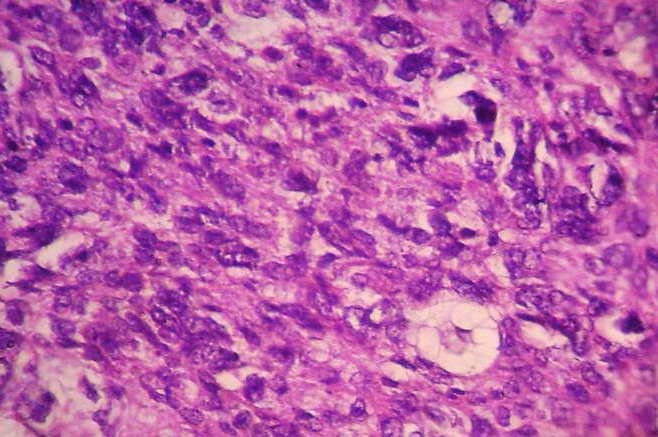
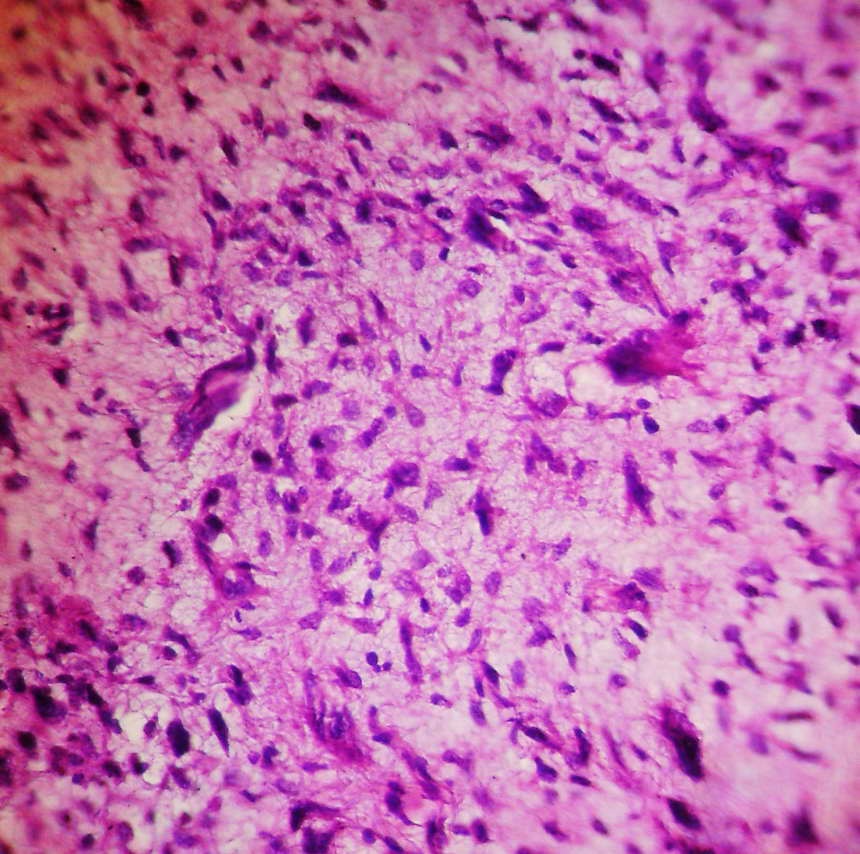
- Type III PPB is an apparently heterogeneous tumor composed of one or more of the following elements:
- Primitive blastema-like small cells with hyperchromatic nuclei, high nuclear to cytoplasmic ratio and abundant mitoses
- Spindled and ovoid cells embedded in a myxoid stroma
- Nodules of immature or malignant chondroid elements
- Isolated or clusters of large anaplastic cells with pleomorphic nuclei, atypical mitotic figures or eosinophilic hyaline bodies
Microscopic (histologic) images
Cytology description
- Cellular smear with both dispersed single cells and cohesive aggregates (Arch Pathol Lab Med 2000;124:416)
- Uniform cells (small round blue cells) may lack cytoplasm, typically display nuclear molding with round or oval nuclei containing darkly stained fine chromatin
- Scattered malignant giant cells have more abundant cytoplasm with indistinct edges and more dispersed chromatin
- Some malignant cells may be spindled with high N/C ratios, eosinophilic cytoplasm and irregular nuclear membranes
- There is no evidence of rosette or glandular formation (Journal of Clinical and Diagnostic Research 2011;5:1656)
Positive stains
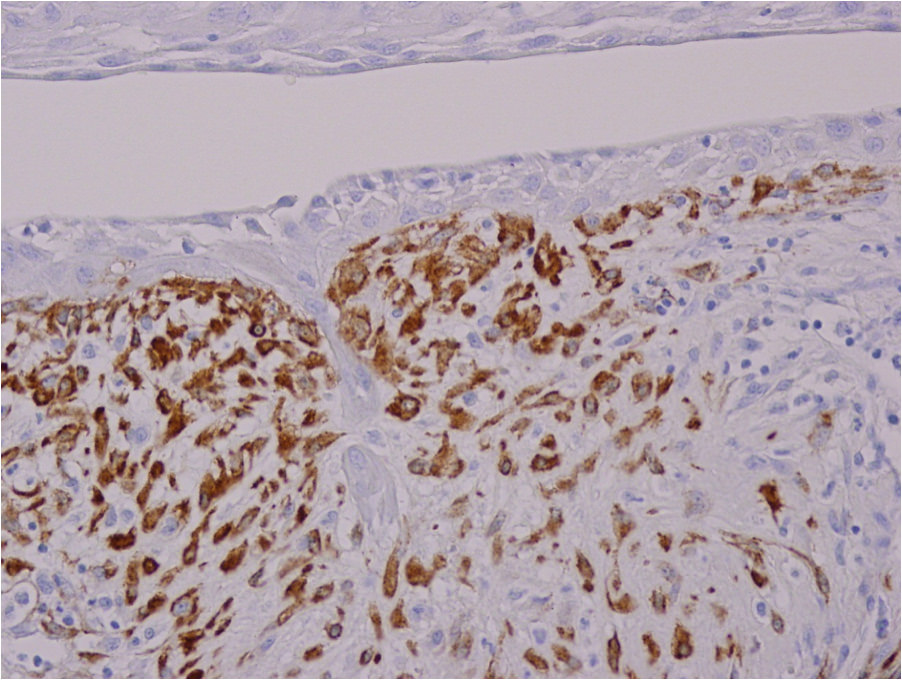
- Neoplastic cells: vimentin (diffuse), CD117 (focally), alpha-1-antitrypsin (focally) and CD99 (weakly)
- Surface epithelium: cytokeratin
- Rhabdomyoblasts and primitive cells: muscle specific actin and desmin
Negative stains
Differential diagnosis
- Embryonal rhabdomyosarcoma (for Type III)
- Large bronchogenic cyst / lung cyst (for Type I)
- Other tumors to consider include (for Type III):
- FLIT (fetal lung interstitial tumour)
- Malignant peripheral nerve sheath tumor
- Malignant teratoma
- Mesothelioma
- Monophasic synovial sarcoma
- PNET
- Undifferentiated sarcoma
Additional references