Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Wu R. Pulmonary capillary hemangiomatosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorhemangiomatosis.html. Accessed April 25th, 2024.
Definition / general
- Proliferation of benign appearing capillaries in alveolar septa that appear to compress pulmonary veins
- May represent a secondary angioproliferative process of veno-occlusive disease caused by postcapillary obstruction rather than a distinct entity (Am J Surg Pathol 2006;30:850)
- Poor prognosis, median survival after symptom onset is 3 years
Essential features
- Disordered proliferation of capillaries within interstitial tissue, including involvement of larger pulmonary vessel walls and airways
- Closely related to pulmonary veno-occlusive disease (PVOD) and could be secondary process, manifests as pulmonary hypertension
- CD31 and CD34 immunohistochemistry can help distinguish capillary proliferation from congestion
Terminology
- Controversial whether a distinct entity from pulmonary veno-occlusive disease (PVOD)
- Consider diagnosis of "secondary PCH" or PCH-like changes for proliferations seen in association with other disorders, reserving "primary PCH" for extremely rare cases without recognizable causative background disease (Am J Surg Pathol 2006;30:850)
Epidemiology
- Very rare, mostly in adults
- Mean age 30 years, range 2-71 years
Sites
- Vascular transformation of sinuses in lobar, hilar and mediastinal lymph nodes is common, with intra-sinusal hemorrhage, erythrophagocytosis, lymphoid follicular hyperplasia (Virchows Arch 2008;453:171)
- Capillaries less frequently invade pericardium, pleura and mediastinal lymph nodes
Pathophysiology
- Chronic passive congestion may lead to capillary proliferation
Etiology
- Not known; thought to be neoplastic but not entirely clear
Clinical features
- Clinically mimics PVOD or atypical interstitial lung disease due to presence of pulmonary hypertension
- Nonspecific symptoms: progressive dyspnea, cough, chest pain, fatigue, small amount of hemoptysis
- Pulmonary function tests show normal FVC and FEV with reduced diffusion capacity
Diagnosis
- Clinically and radiographically indistinguishable from PVOD; diagnosis requires microscopic diagnosis by lung biopsy
- Diagnosis frequently made on explant specimen or after death
Radiology description
- Findings seen in pulmonary hypertension; i.e. cardiomegaly, enlarged pulmonary arteries
- Chest Xray: interstitial infiltrates, thick interlobular septa, bibasilar reticulonodular or micronodular areas of opacity, lymphoadenopathy
- HRCT: diffuse centrilobular ground glass opacity (Cardiovasc Pathol 2013;22:287), peripheral sparing
Prognostic factors
- Prostacyclin therapy (used in pulmonary hypertension) may cause sudden respiratory distress and death in these patients
Case reports
- 47 year old man with coexisting pulmonary fibrosis (Pathol Int 2011;61:306)
- 60 year old woman with PCH incidentally discovered in lobectomy for metastatic colon cancer (Pathol Int 2006;56:350)
Treatment
- Lung transplantation is only definitive treatment but recurrence has been reported
- Drugs for other causes of pulmonary hypertension are relatively ineffective
- Case reports suggest Interferon α-2a or doxycycline may be effective
Clinical images
Gross description
- Multiple, red-brown, ill defined, nodular lesions
- Congested, edematous, without significant fibrosis
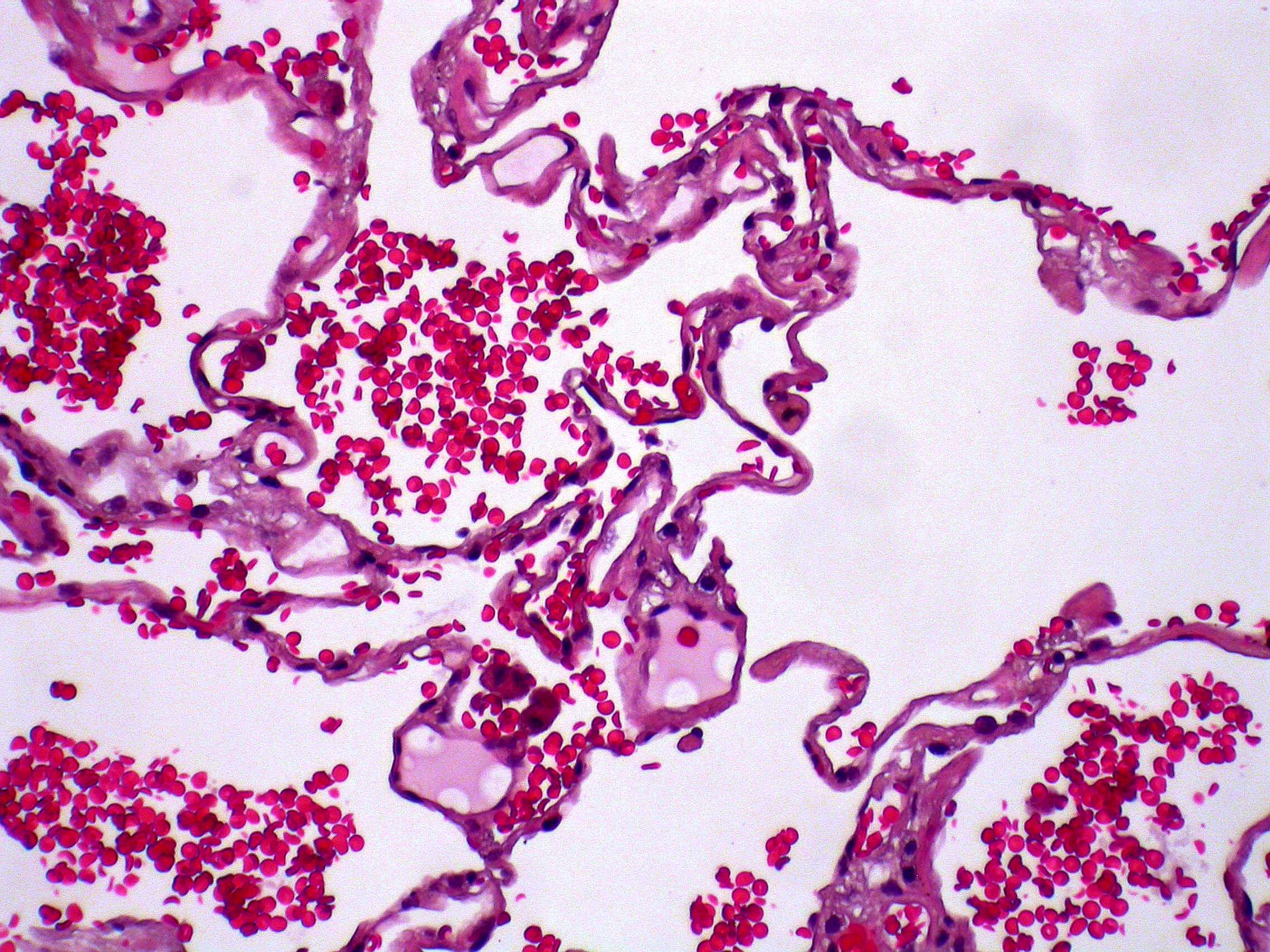
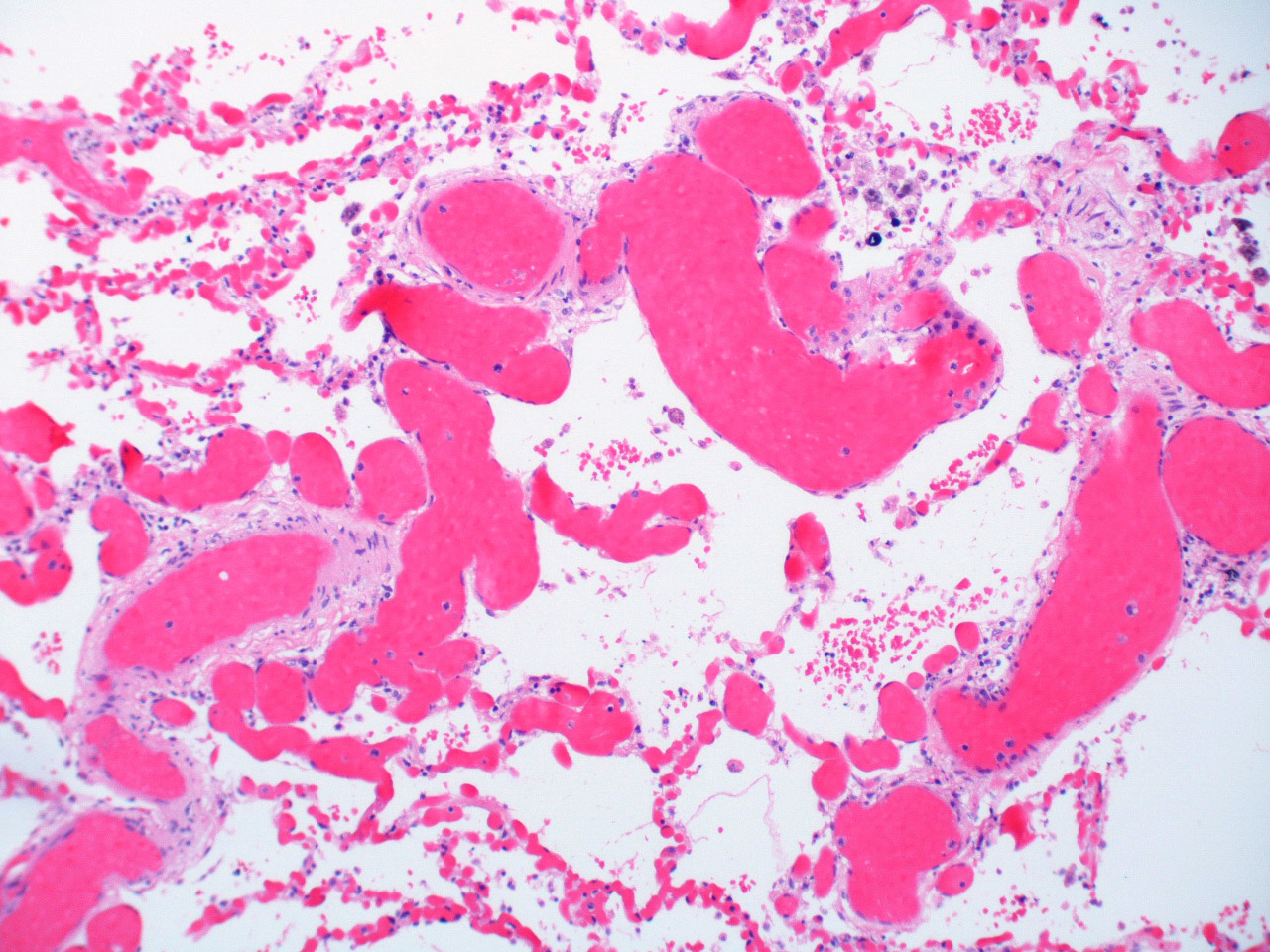
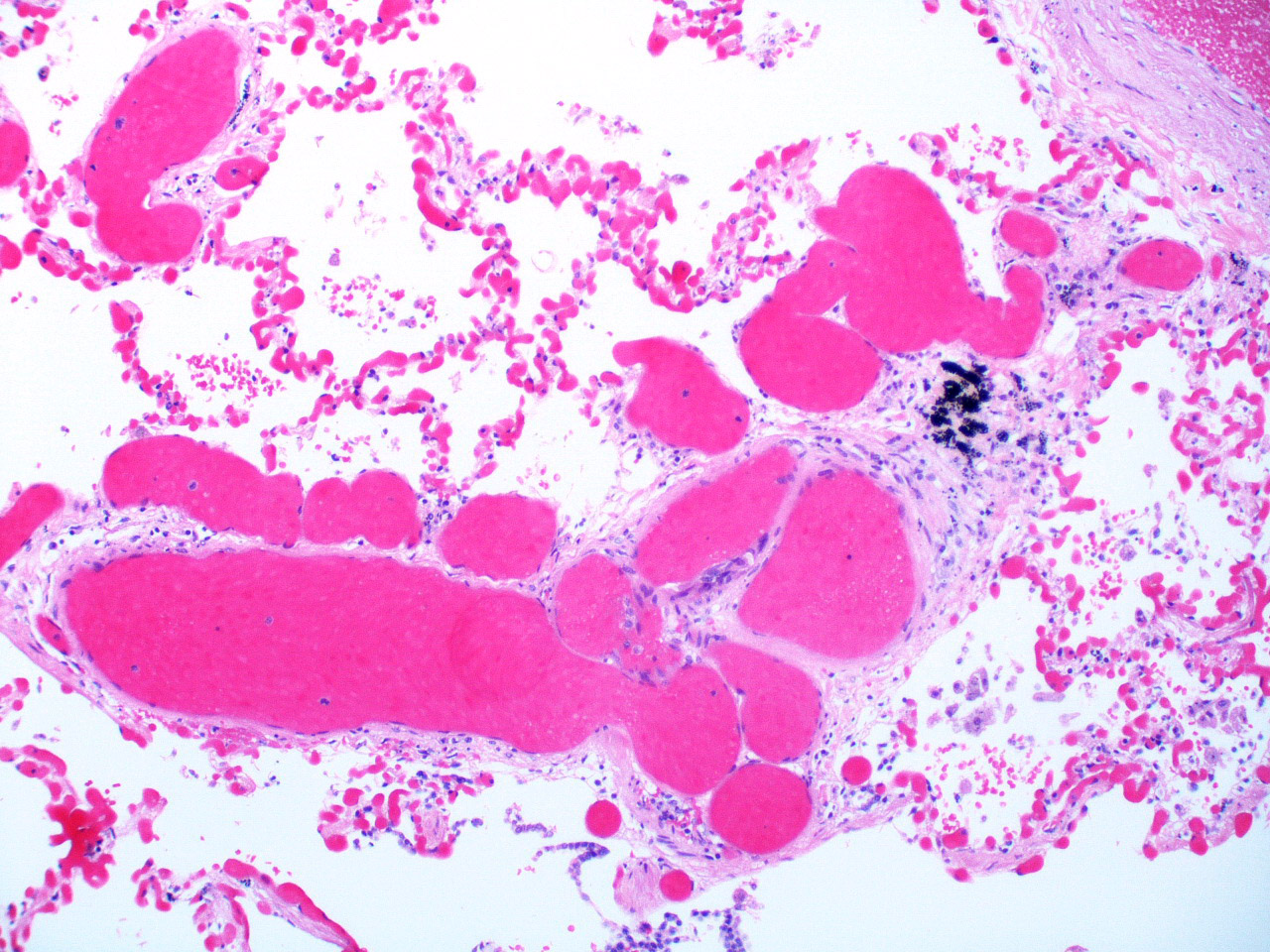
Microscopic (histologic) description
- Preserved architecture with areas of involvement admixed with areas of normal lung
- Proliferation of benign appearing capillaries expanding alveolar septa that appear to compress pulmonary veins
- Proliferation around bronchovascular bundles creating nodular appearance
- At least 2 layers of aberrant capillaries within alveolar wall (Arch Pathol Lab Med 2015;139:274)
- Bland endothelial cells, no mitoses
- Intra-alveolar hemosiderin-laden macrophages, small areas of acute or old hemorrhage, hemosiderosis
- Small pulmonary arteries with intimal thickening/medial hypertrophy
Microscopic (histologic) images
Cytology description
- Alveolar lavage often with increased hemosiderin-laden macrophages
Molecular / cytogenetics description
- Mutations in EIF2AK4 described in some cases of familial and sporadic PCH; encodes for a translation initiation factor (Chest 2014;145:231, Appl Clin Genet 2015;8:181)
- Case of 16q deletion in FOXF1 enhancer leading to neonatal PCH (BMC Med Genet 2015;16:94)
Differential diagnosis
- Capillary congestion
- Veno-occlusive disease: associated with PCH; eccentric intimal thickening of venules in lobular septa with some septal veins completely occluded, increased elastic fibers in venous media (highlighted with elastin stain); intimal fibrosis narrows and occludes the pulmonary veins, causing dilatation of capillaries
Additional references