Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ravindran A, Rech KL. Follicular dendritic cell sarcoma (FDCS). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesFDCsarcoma.html. Accessed April 25th, 2024.
Definition / general
- Rare mesenchymal neoplasm arising from follicular dendritic cells (FDC) of lymphoid follicles at nodal and extranodal sites
- Nodal follicular dendritic cell sarcoma (FDCS) first characterized in 1986 (Am J Pathol 1986;122:562)
- Extranodal follicular dendritic cell sarcoma first described in 1994 (Am J Surg Pathol 1994;18:148)
Essential features
- Presents as a painless solid mass in nodal and extranodal sites
- Behaves as a low grade sarcoma
- Immunohistochemistry showing expression of ≥ 2 FDC markers is essential for diagnosis
Terminology
- Previous designation: follicular dendritic cell tumor (in WHO classification prior to 2008)
- Classified under histiocytic / dendritic cell neoplasms in the WHO Classification of Haematolymphoid Tumours (4th revised edition, 2017)
- Classified under mesenchymal dendritic cell neoplasms in the category of stroma derived neoplasms of lymphoid tissues in the current WHO Classification of Haematolymphoid Tumours (5th edition, 2023)
ICD coding
- ICD-10: C96.4 - sarcoma of dendritic cells (accessory cells)
Epidemiology
- Wide age range; median age is 50 years (Crit Rev Oncol Hematol 2013;88:253)
- M = F
Sites
- Lymph nodes: cervical (most common); second most common is axillary or supraclavicular lymph nodes
- Extranodal FDCS occurs in a wide variety of sites, including head and neck, gastrointestinal tract, retroperitoneum, tonsil and lung (Adv Anat Pathol 2021;28:21)
Pathophysiology
Etiology
- May arise in the context of follicular dendritic cell proliferation in Castleman disease, hyaline vascular variant
- Cases that show association with Epstein-Barr virus (EBV) and predominantly involve the liver or spleen are now considered a distinct entity: EBV positive inflammatory follicular dendritic cell sarcoma (Am J Surg Pathol 2001;25:721)
Clinical features
- Nodal and extranodal involvement characterized by slow growing, painless solid mass
- B symptoms (fever, night sweats, weight loss) are usually absent
- Surgical resection results in complete remission in a majority of cases
- ~33% of cases recur locally
- May show late metastasis by hematologic spread to bone, lungs, liver
- Rarely, may be associated with paraneoplastic autoimmune multiorgan syndrome (PAMS) (Am J Surg Pathol 2018;42:1647)
Diagnosis
- Morphologic evaluation supplemented by immunophenotype of follicular dendritic cells is key to diagnosing FDCS
- FDCS can coexist with Castleman disease (Pathologica 2021;113:316)
Radiology description
- Nodal involvement presents as a homogeneous mass, slightly hypoattenuating on CT, hypointense or isointense on T1 weighted MRI and hyperintense on T2 weighted MRI (AJR Am J Roentgenol 2021;216:835)
- Extranodal sites of involvement appear heterogeneous with hyperattenuation on unenhanced CT or hyperintense foci on T1 weighted MRI, with or without associated necrosis and calcifications, often accompanied by regional lymphadenopathy (AJR Am J Roentgenol 2021;216:835)
Radiology images
Prognostic factors
- Poor prognostic factors include size of tumor (> 6 cm), nuclear pleomorphism, increased mitoses (> 5/10 high power fields), necrosis and intra-abdominal location (Arch Pathol Lab Med 2017;141:596)
- Association with paraneoplastic autoimmune multiorgan syndrome follows an aggressive course related to respiratory morbidity and mortality (Am J Surg Pathol 2018;42:1647)
Case reports
- Man in his early 30s presented with jaundice, abdominal pain and weight loss (J Int Med Res 2022;50:3000605221142401)
- 34 year old man with Birt-Hogg-Dubé syndrome presented with mass at the ileocecal junction (Diagn Pathol 2022;17:64)
- 66 year old woman with intermittent right upper quadrant pain (World J Clin Cases 2019;7:785)
- 66 year old man with no significant medical history presented with right cervical mass (Mol Clin Oncol 2020;13:23)
- 72 year old man presented with enlarged mediastinal lymph nodes (Cureus 2023;15:e37715)
Treatment
- Includes complete surgical resection with or without radiation therapy
- Role of adjuvant chemotherapy or radiation is unclear (Cancers (Basel) 2014;6:2275)
- Role of chemotherapy in advanced disease is not well established (Crit Rev Oncol Hematol 2013;88:253)
Gross description
- Usually round to ovoid, well circumscribed fleshy solid mass (Arch Pathol Lab Med 2016;140:186)
- Size ranges from 1 cm to 15 cm, largely dependent on the site of the tumor
- May show areas of hemorrhage and necrosis
Gross images
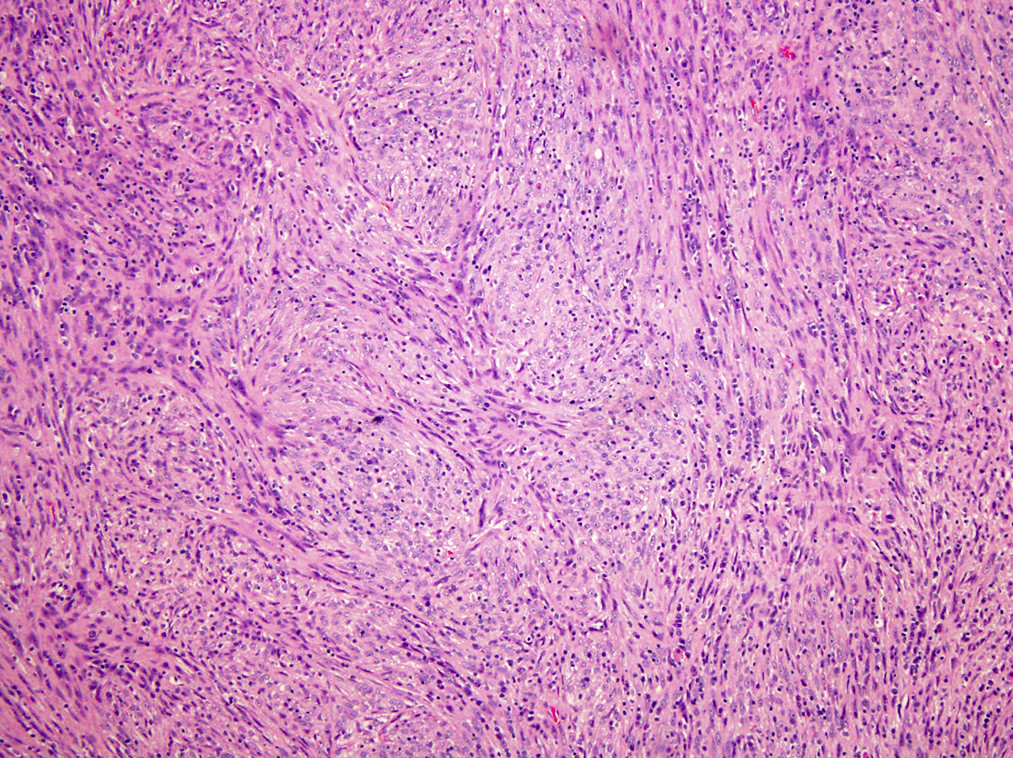
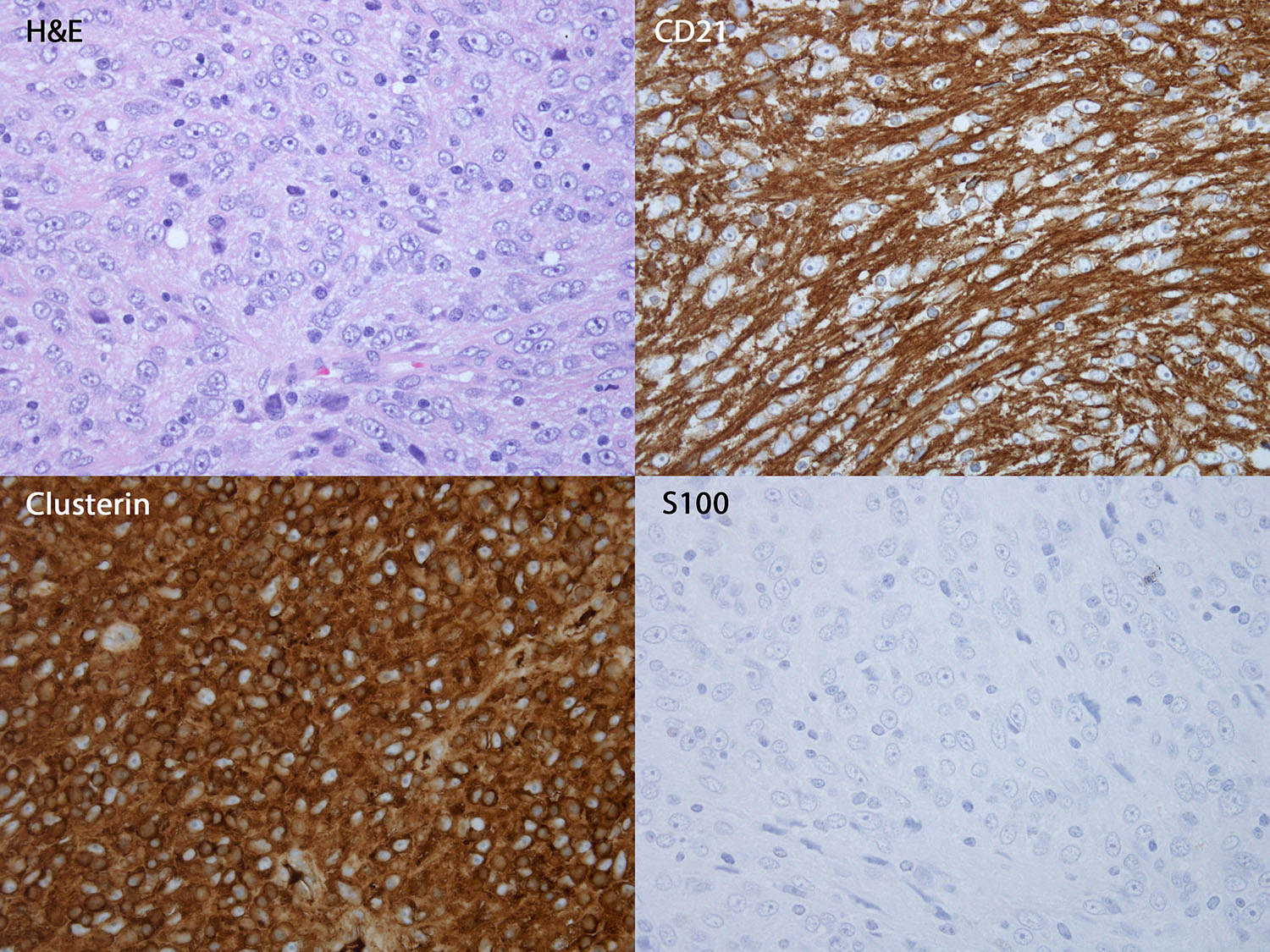
Microscopic (histologic) description
- Oval to spindled cells with dispersed chromatin, small nucleoli, eosinophilic and fibrillar cytoplasm with syncytial borders arranged in fascicles, whorls or storiform patterns
- Often binucleate or occasional multinucleate forms, nuclear pseudoinclusions
- Perivascular lymphocyte cuffs and admixed population of lymphocytes, eosinophils, plasma cells or neutrophils may be present (Am J Surg Pathol 2004;28:988)
Microscopic (histologic) images
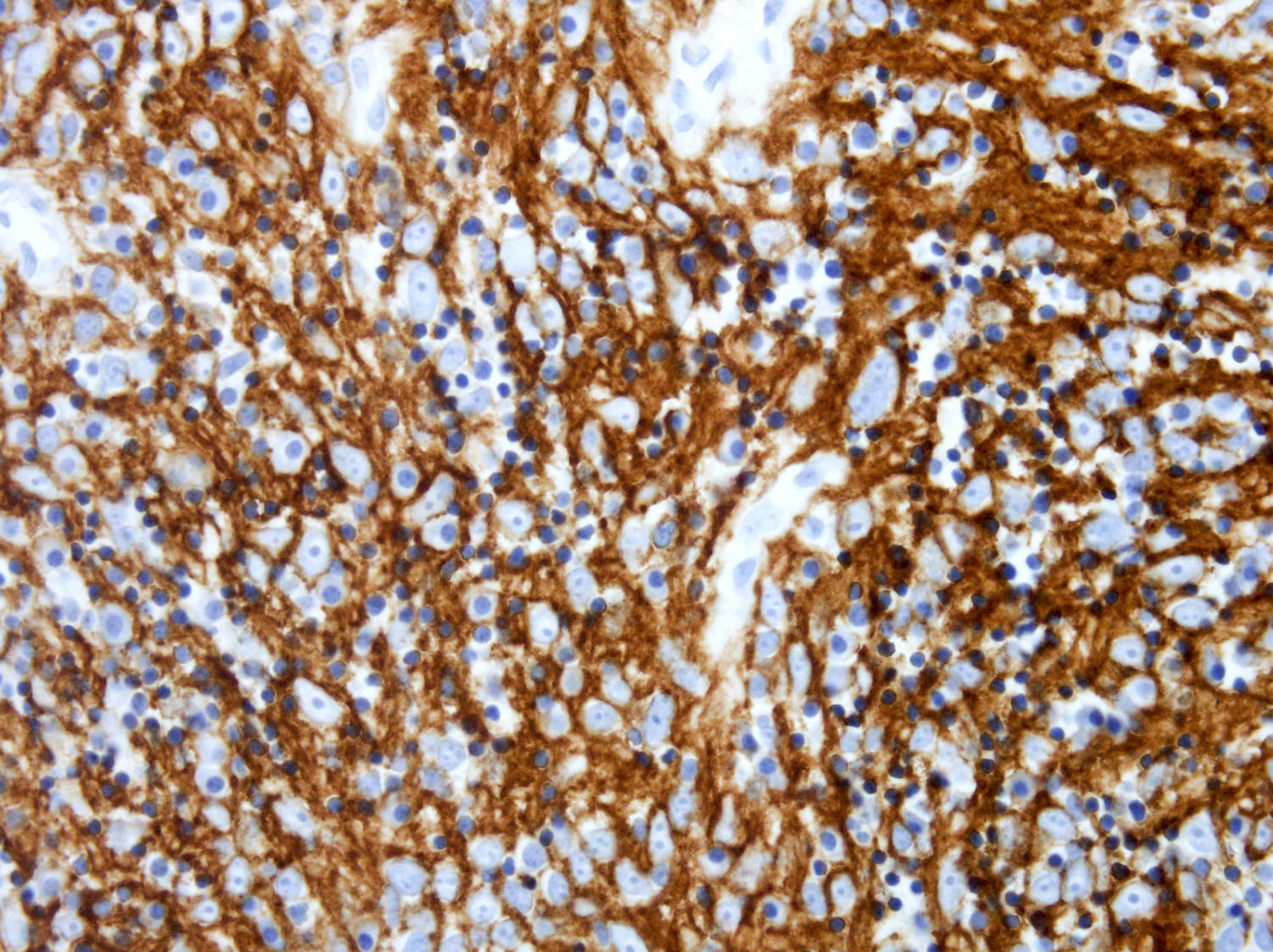
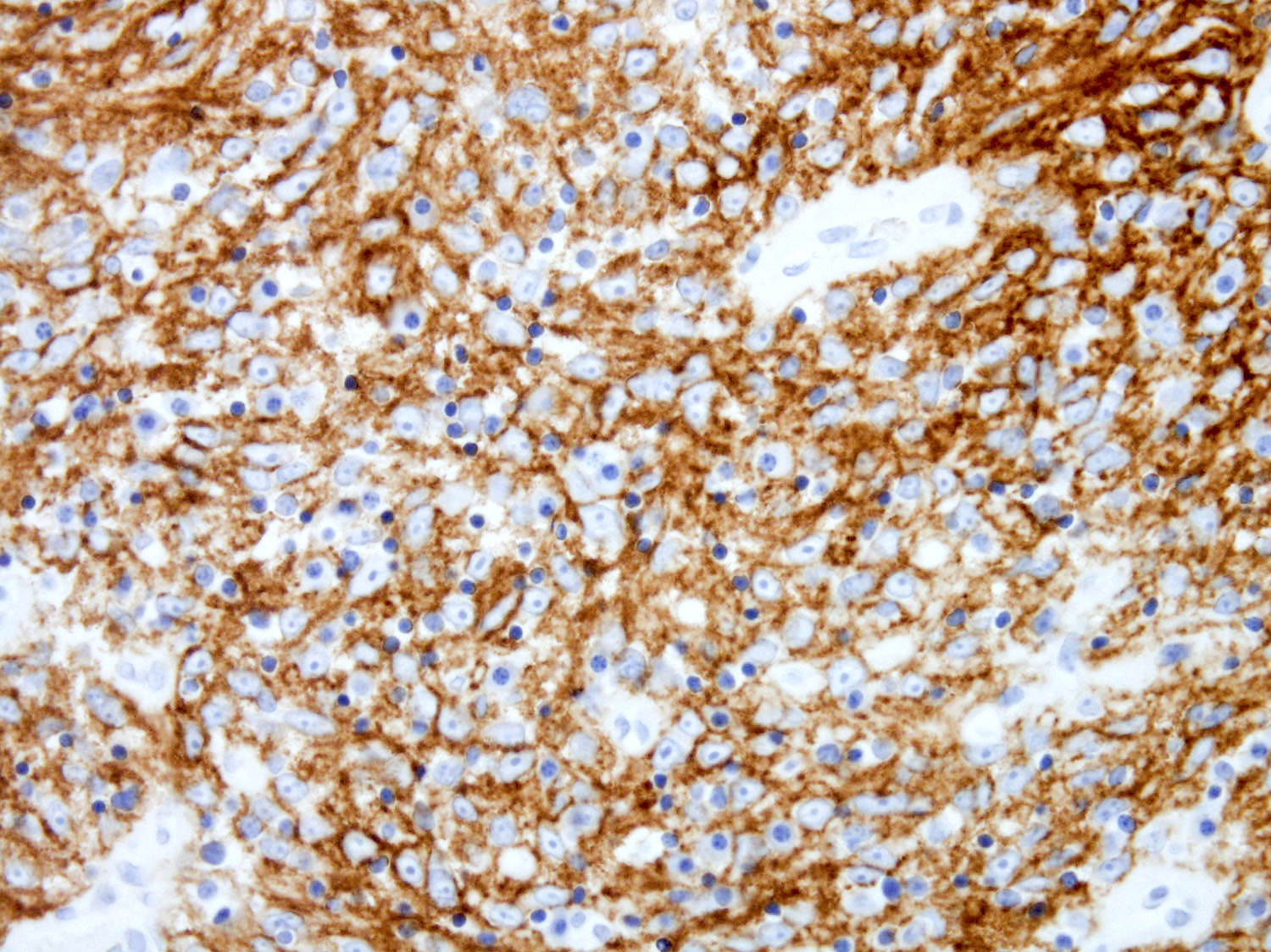
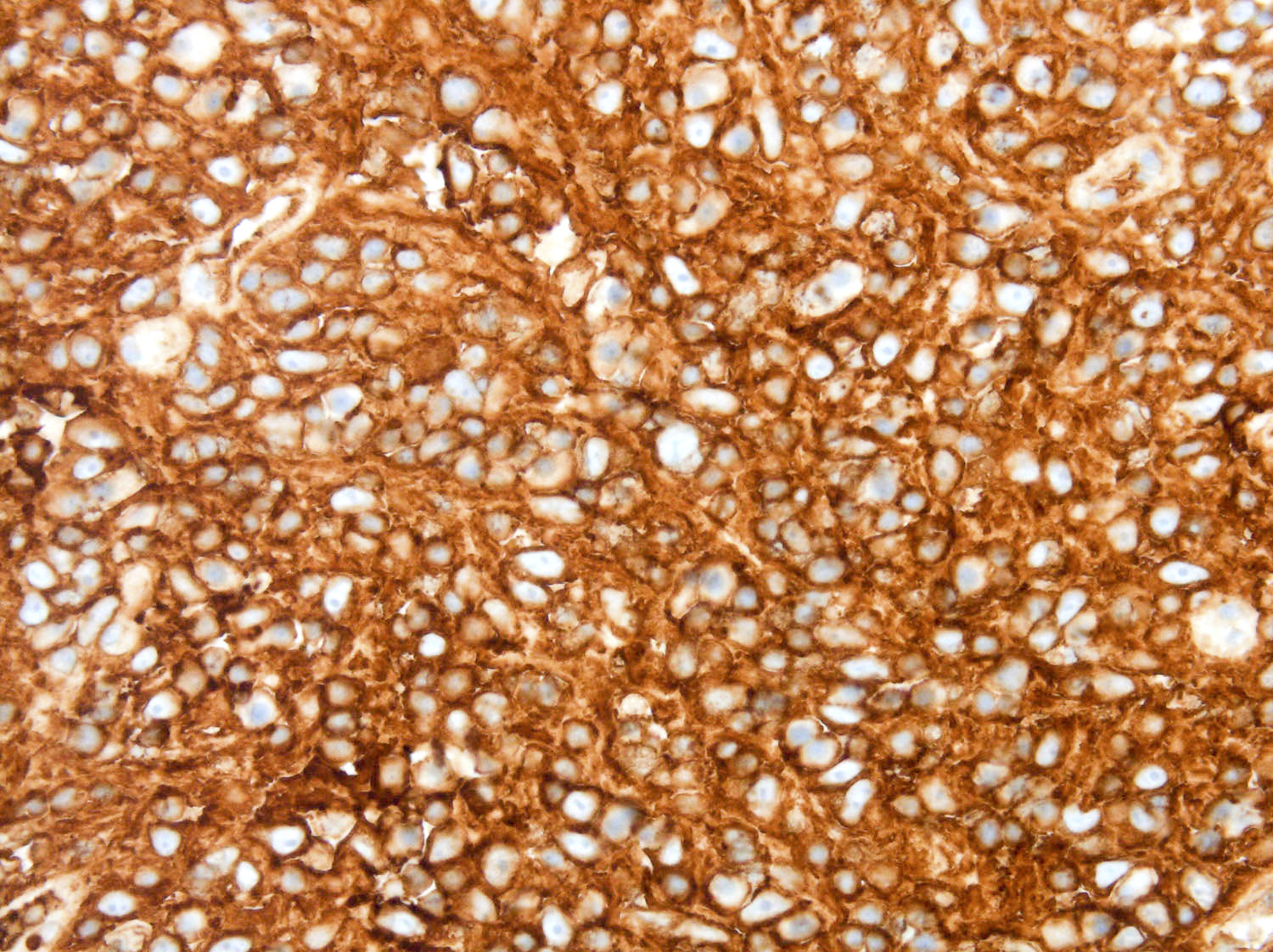
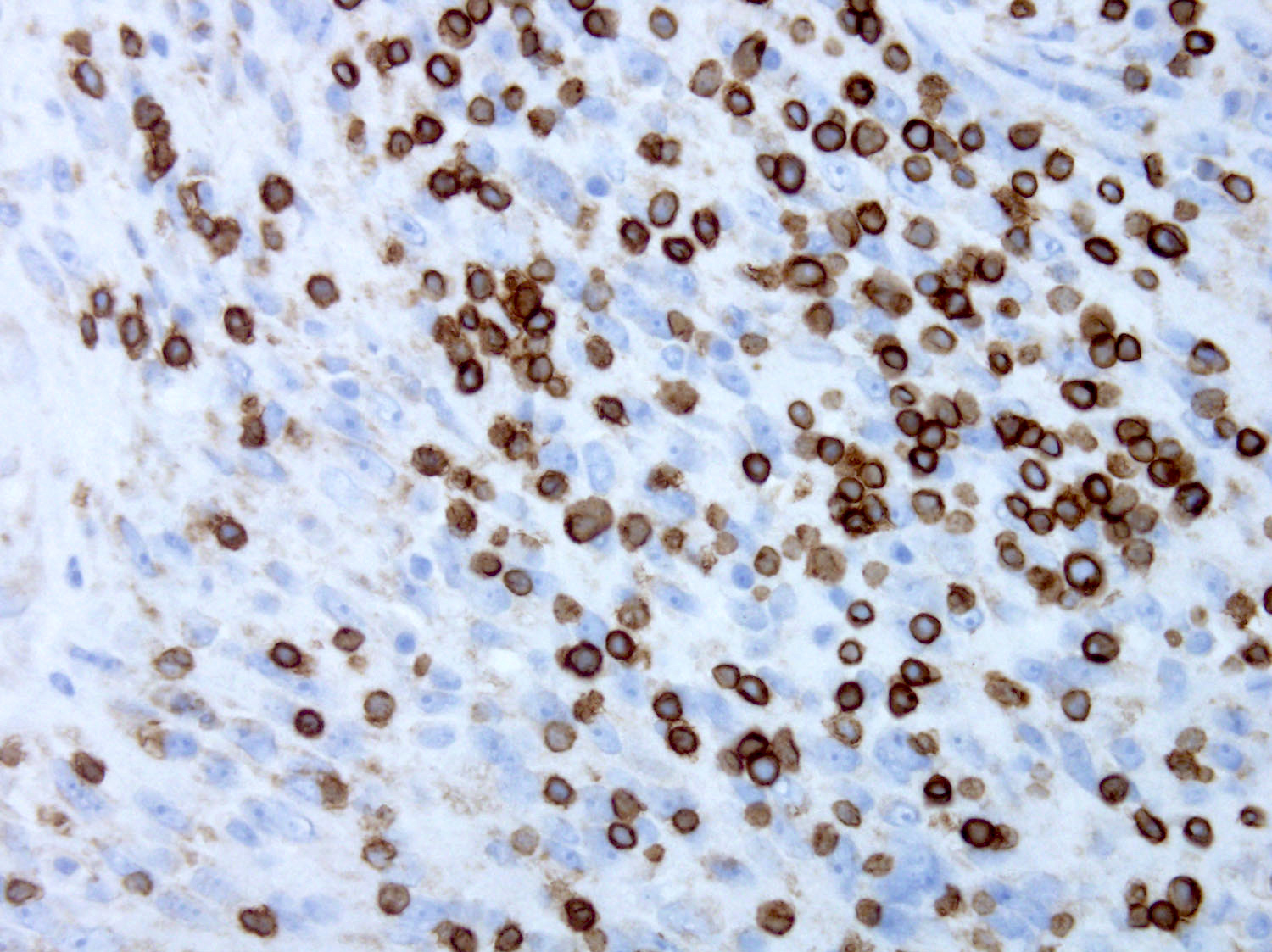
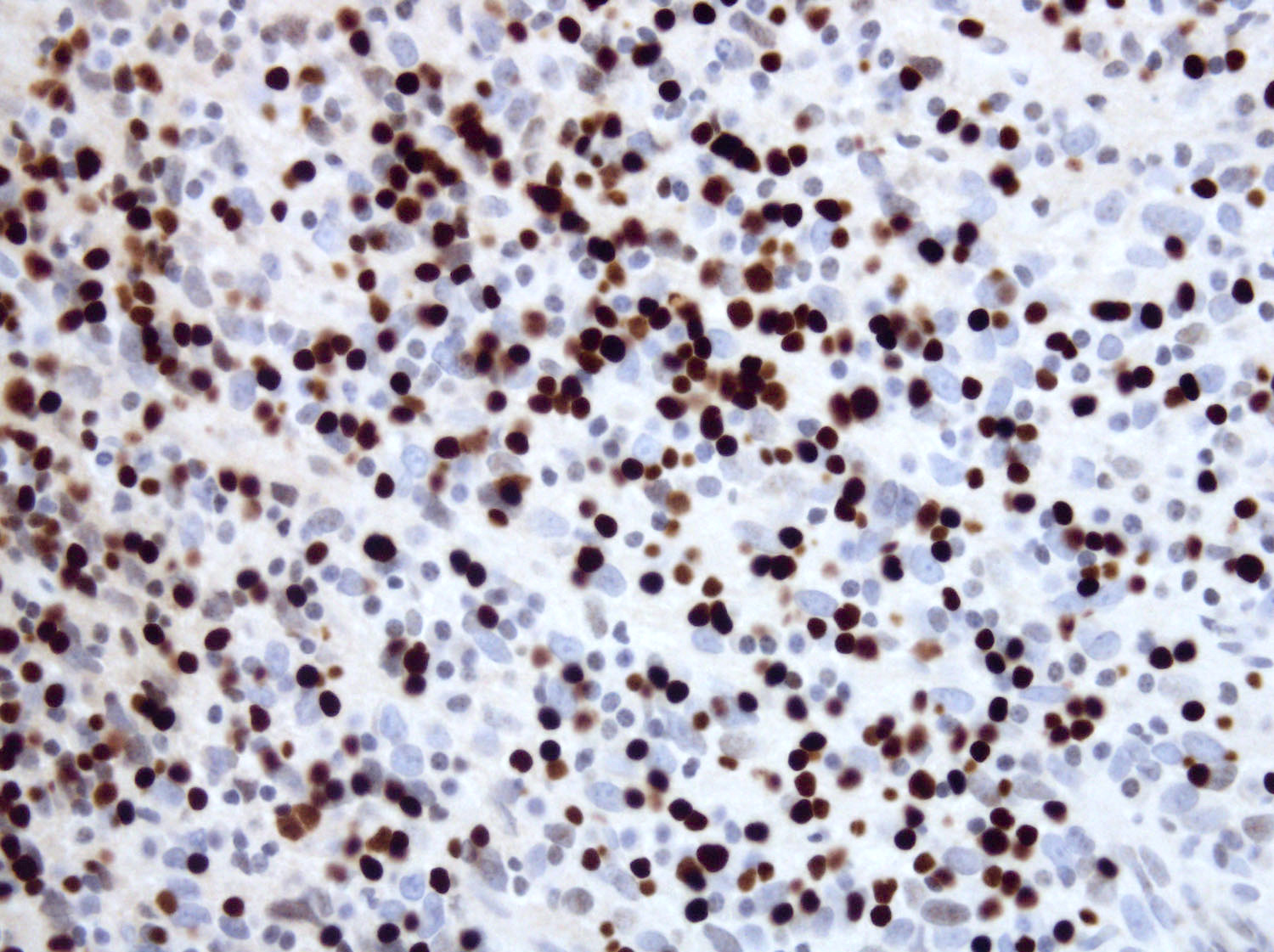
Positive stains
- Most sensitive FDC markers: clusterin, CD21, CXCL13 (J Pathol 2008;216:356, Am J Surg Pathol 2004;28:988)
- Most specific FDC markers: CXCL13, CD21, CD23, CD35
- Other FDC markers: podoplanin / D2-40, SSTR2a, follicular dendritic cell secreted protein (FDCSP) and serglycin (SRGN) (Am J Clin Pathol 2007;128:776, Am J Surg Pathol 2019;43:374, Oncotarget 2017;8:16463)
- Other positive stains: fascin, PDL1, desmoplakin, EGFR and vimentin (Mod Pathol 2005;18:260)
- TdT highlights immature T cell lymphoblastic proliferation in 45% of cases; when abundant, this finding may be associated with paraneoplastic autoimmune multiorgan syndrome (Am J Surg Pathol 2018;42:1647)
Negative stains
Molecular / cytogenetics description
- Proposed molecular pathogenesis involves activation of nuclear factor κβ genes as a consequence of recurrent loss of function alterations in nuclear factor κβ regulatory genes (NFKBIA, CYLD, BIRC3, SOCS3, TRAF3, TNFAIP3), tumor suppressor genes (CDKN2A, RB1, TP53) and genes involved in immune evasion (CD274, PDCD1LG2) (Mod Pathol 2016;29:67)
- Genetic alterations, including copy number variations, somatic mutations involving oncogenes / tumor suppressors (ZBTB7A, SETD2), chromatin remodeling genes (CABIN1, NCAPH) and other genes, have been reported (Blood Adv 2018;2:481)
- BRAF V600E or other MAPK pathway mutations are uncommon (Histopathology 2014;65:261, Arch Pathol Lab Med 2023;147:896)
- Chromosome analysis typically reveals a complex karyotype (In Vivo 2013;27:211)
Sample pathology report
- Lymph node, left neck, excisional biopsy:
- Follicular dendritic cell sarcoma, completely excised (see comment)
- Comment: Lymph node architecture is partially effaced by an abnormal population of epithelioid to spindle shaped cells in a whorling pattern. The neoplastic cells have ovoid nuclei, delicate chromatin, small nucleoli and abundant eosinophilic cytoplasm. They are variably admixed with small lymphocytes. Immunohistochemical stains were performed on paraffin sections of the left neck lymph node (CD21, CD23, CD31, CD34, CD35, CD45, clusterin, CXCL13, epithelial membrane antigen, melanA, keratin [AE1 / AE3], HMB45, S100 and terminal deoxynucleotidyl transferase). The abnormal cells are positive for CD21, CD23, CD35, clusterin and CXCL13. There are small numbers of terminal deoxynucleotidyl transferase positive (TdT) cells mixed with the tumor. The neoplastic cells are negative for the other markers tested. Morphology and immunohistochemical stains support the diagnosis of follicular dendritic cell sarcoma.
Differential diagnosis
- Interdigitating dendritic cell sarcoma:
- Histologically may be indistinguishable from follicular dendritic cell sarcoma and immunohistochemical studies are required for a definite diagnosis
- Positive for S100, CD45, CD68; negative for FDC markers (Am J Surg Pathol 2004;28:988)
- Langerhans cell histiocytosis:
- Langerhans cells are oval and recognized by their grooved, folded or indented nuclei with fine chromatin, inconspicuous nucleoli and thin nuclear membrane with moderately abundant and slightly eosinophilic cytoplasm
- Positive for CD1a and langerin
- Kaposi sarcoma:
- Atypical spindled cells form slit-like vascular spaces containing red blood cells
- Positive for HHV8
- Spindle cell thymoma:
- Metastatic carcinoma:
- Metastatic melanoma:
- Inflammatory myofibroblastic tumor:
- Spindled myofibroblasts and fibroblasts with bland nuclei
- Positive for ALK1
- Pleomorphic sarcoma:
Additional references
Board review style question #1
An 88 year old man presented with significant snoring and increasing sleep apnea. Laryngoscopy revealed a pharyngeal mass. Computed tomography (CT) of the head and neck with intravenous (IV) contrast revealed a 6 cm enhancing mass in the right parapharyngeal space. An excisional biopsy was performed. Based on the immunophenotype (positive for CD21 and clusterin, negative for S100), what is the diagnosis?
- Follicular dendritic cell sarcoma
- Interdigitating dendritic cell sarcoma
- Langerhans cell sarcoma
- Pleomorphic sarcoma
Board review style answer #1
A. Follicular dendritic cell sarcoma. The immunophenotype indicated here is typical of follicular dendritic cells (FDC: CD21 positive, clusterin positive), supporting the diagnosis of follicular dendritic cell sarcoma. Answer B is incorrect because interdigitating dendritic cell sarcomas are characterized by positive expression of CD45, CD68 and S100, while they are negative for FDC markers. Answer C is incorrect because Langerhans cell sarcoma is positive for Langerhans cell markers (CD1a, Langerin) and negative for FDC markers. Answer D is incorrect because pleomorphic sarcoma is negative for FDC markers.
Comment here
Reference: Follicular dendritic cell sarcoma (FDCS)
Comment here
Reference: Follicular dendritic cell sarcoma (FDCS)
Board review style question #2
Which of the following molecular pathways is most frequently associated with follicular dendritic cell sarcoma (FDCS)?
- JAK-STAT
- MAPK-ERK
- NFκB
- PI3K-Akt
Board review style answer #2
C. NFκB. Genetic alterations involving NFκB pathway are present in over 50% of FDCS cases. Answers B and D are incorrect because MAPK-ERK and PI3K-Akt pathways are frequently associated with histiocytic / dendritic cell neoplasms, such as Erdheim-Chester disease, Rosai-Dorfman disease and Langerhans cell histiocytosis. Answer A is incorrect because JAK-STAT pathway is associated with other hematologic malignancies (such as myeloproliferative neoplasms) and not FDCS.
Comment here
Reference: Follicular dendritic cell sarcoma (FDCS)
Comment here
Reference: Follicular dendritic cell sarcoma (FDCS)