Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Haghighi Abyaneh M, Mohsin H, Brown RA. Indeterminate cell histiocytosis / indeterminate dendritic cell tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesindeterminatecelltumors.html. Accessed April 18th, 2024.
Definition / general
- Indeterminate cell histiocytosis is an extremely rare neoplastic proliferation of cells of dendritic / histiocytic lineage that share immunophenotypic features of Langerhans cells but lack Birbeck granules and langerin expression
Essential features
- Skin involvement can be solitary or multifocal
- Usually restricted to skin, with rare organ or lymph node involvement
- Indeterminate cells are histopathologically and antigenically similar to Langerhans cells but lack Birbeck granules and langerin (CD207) expression
- Clinical course varies: spontaneous regression, stable disease, rapid progression or recurrence
Terminology
- Indeterminate cell histiocytosis
- Indeterminate cell tumor
- Indeterminate dendritic cell tumor
ICD coding
- ICD-10: D76.3 - other histiocytosis syndromes
Epidemiology
- Rare neoplasm, with 85 cases reported between 1985 - 2016 (Am J Dermatopathol 2018;40:736)
- Reported in all age groups, with a median age of 45
- Near equal M:F
Sites
- Cutaneous involvement (88%) is most common (Am J Dermatopathol 2018;40:736)
- Lymph node (9%) and spleen (2.3%) involvement less common (Am J Dermatopathol 2018;40:736)
Etiology
- Etiology remains uncertain
- Multiple hypotheses on the relationship between indeterminate cells and Langerhans cells, including:
- Indeterminate cells are Langerhans cells that have lost their Birbeck granules
- Indeterminate cells are immature Langerhans cells
- A subset of cases express dendritic cell marker ZBTB46, raising the possibility that a subset of cases arise directly from bone marrow progenitors as opposed to embryonic precursors that locally renew in the skin (Mod Pathol 2018;31:1479)
- Association between other hematologic neoplasms has been reported (including B cell lymphoma, T cell lymphoma, acute myeloid leukemia and chronic myelomonocytic leukemia) (Am J Surg Pathol 2008;32:1868, J Cutan Pathol 2017;44:958, Am J Dermatopathol 2019;41:461, Dermatol Res Pract 2010;2010:569345)
- Indeterminate cell histiocytosis can share clonal abnormality of associated lymphoma or leukemia (Am J Surg Pathol 2008;32:1868)
Clinical features
- Reported in all age groups, with a median age of 45
- Near equal M:F patients
- Single cutaneous papulonodule or multiple lesions (few to innumerable)
- Can have plaques and tumors with leonine facies (J Cutan Pathol 2016;43:158)
- Usually restricted to skin with rare organ or lymph node involvement
- Clinical course varies: spontaneous regression, stable disease, rapid progression or recurrence
- Reference: Am J Dermatopathol 2018;40:736
Diagnosis
- Skin biopsy for localized lesions
- Systemic workup to exclude deep involvement
- CT scans and bone marrow biopsy
Laboratory
- Can have elevated lactate dehydrogenase, erythrocyte sedimentation rate and C reactive protein (Serbian J Dermatology Venereol 2018;10:18)
Radiology description
- True cutaneous indeterminate cell histiocytosis typically lacks evidence of deep organ involvement on imaging
Prognostic factors
- Cases restricted to the skin typically behave indolently
- Involvement of deep or visceral tissues or bone marrow may portend worse prognosis
Case reports
- 6 year old girl with polypoid and verrucoid lesions of the vulva (Am J Dermatopathol 2018;40:736)
- 13 year old girl with pityriasis rosea type rash (Acta Derm Venereol 2002;82:288)
- 28 year old man presented after a mosquito bite (Medicine (Baltimore) 2015;94:e1443)
- 48 year old woman with a later diagnosis of mycosis fungoides (Am J Dermatopathol 2019;41:461)
- 55 year old woman with a history of burning and confluent erythematous papules on the face and arms (Cureus 2021;13:e12850)
- 55 year old woman presented with leonine facies (J Cutan Pathol 2016;43:158)
- 55 year old man with complete response to ultraviolet phototherapy (J Cutan Pathol 2017;44:958)
- 61 year old man with recurrence after excision (J Pathol Transl Med 2018;52:243)
- 72 year old man with chronic myelomonocytic leukemia (J Cutan Pathol 2017;44:958)
- 74 year old woman with a prior history of follicular lymphoma demonstrating t(14;18) translocation (Am J Surg Pathol 2008;32:1868)
- 90 year old man with aggressive case mimicking angiosarcoma (Ann Dermatol 2017;29:614)
Treatment
- Surgical excision for isolated lesions
- Psoralen and ultraviolet A therapy (PUVA) (J Cutan Pathol 2017;44:958, Autops Case Rep 2016;6:33, Kaohsiung J Med Sci 2004;20:24)
- Chemotherapy can be considered for more aggressive disease or those cases associated with concurrent myeloid or lymphoid neoplasm
Clinical images
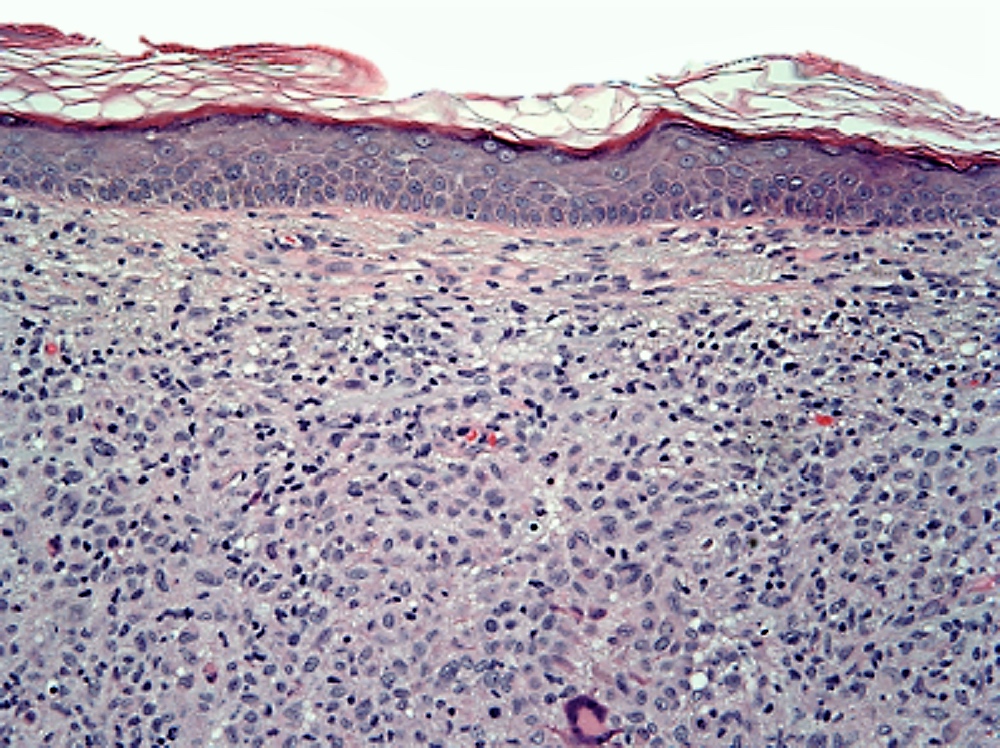
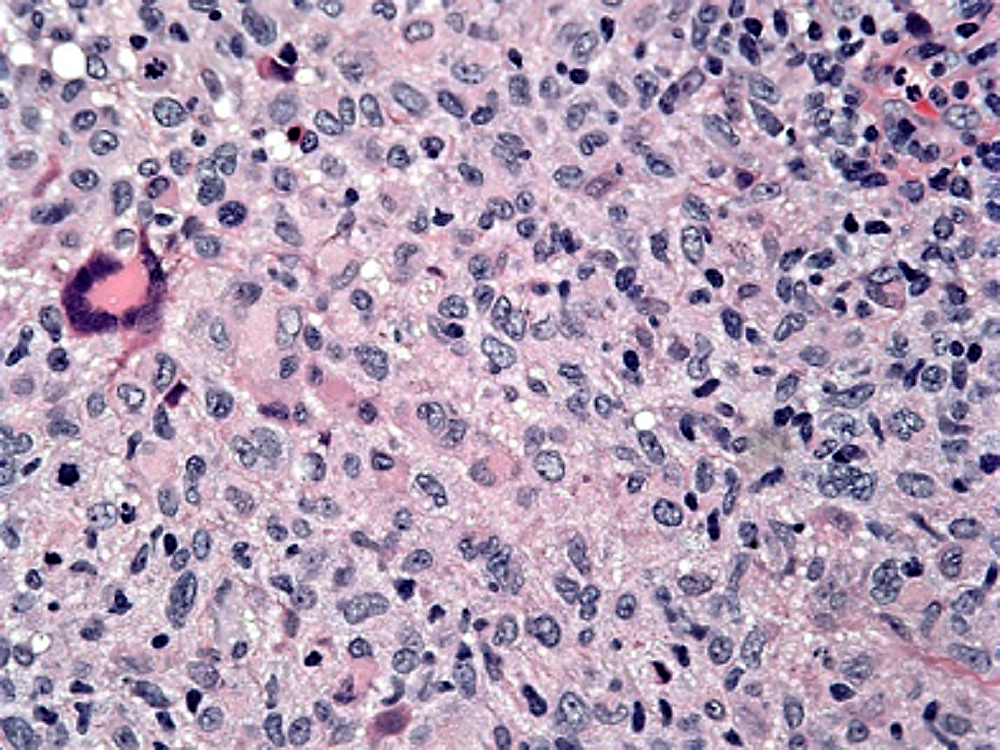
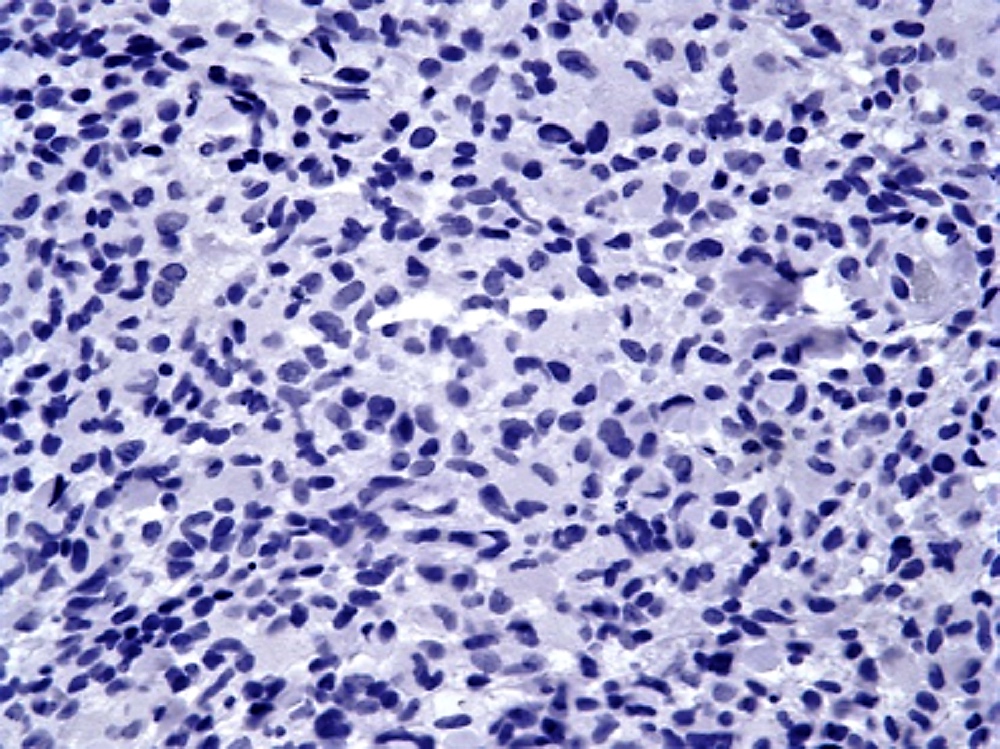
Microscopic (histologic) description
- Dermal infiltration by pale eosinophilic histiocytic cells with reniform nuclei
- Background reactive lymphocytes
- Scant to absent eosinophils
- Can have multinucleated cells
- Spindled morphology is less common
- References: Am J Dermatopathol 2018;40:736, Blood 2015;126:2344, Arch Pathol Lab Med 2003;127:748, Am J Surg Pathol 2008;32:1868, Cureus 2021;13:e12850
Microscopic (histologic) images
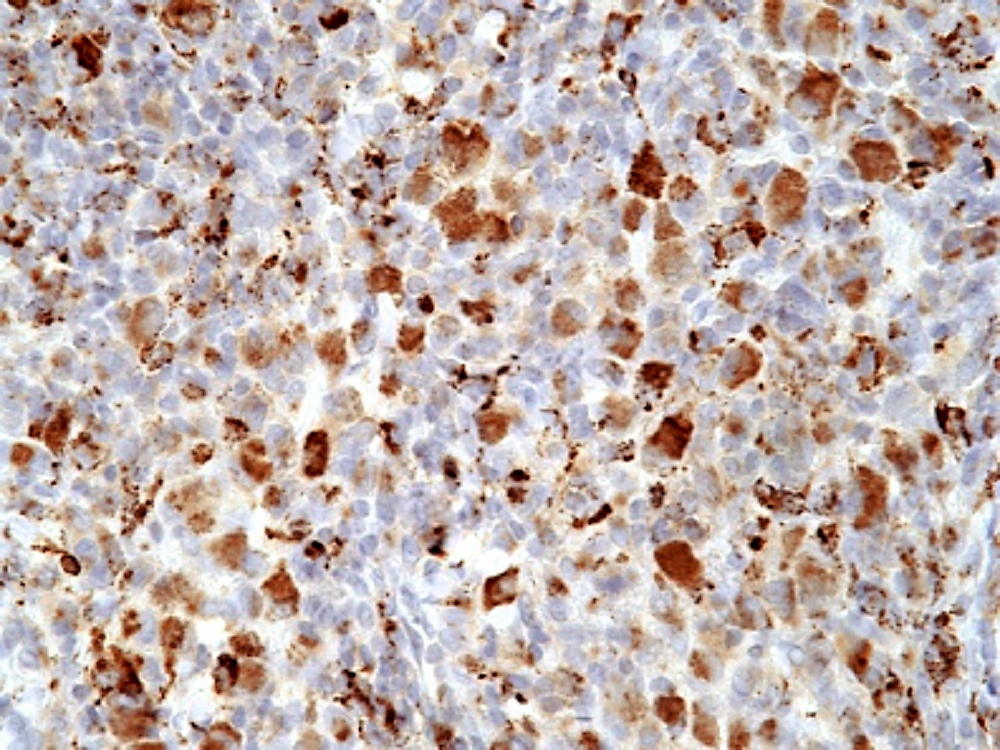
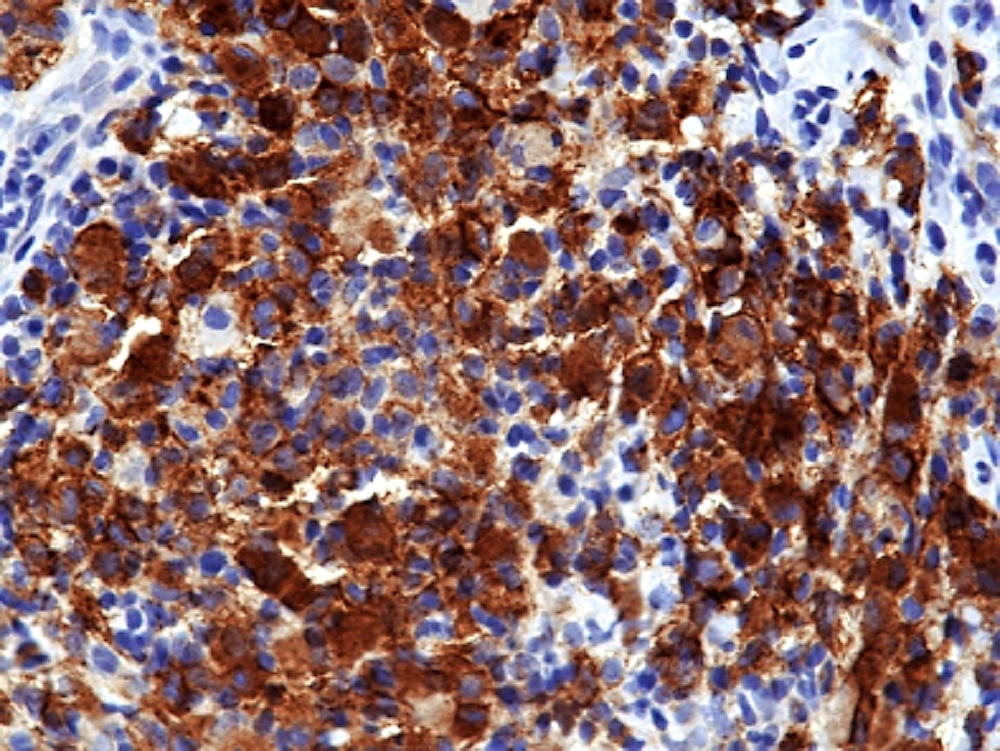
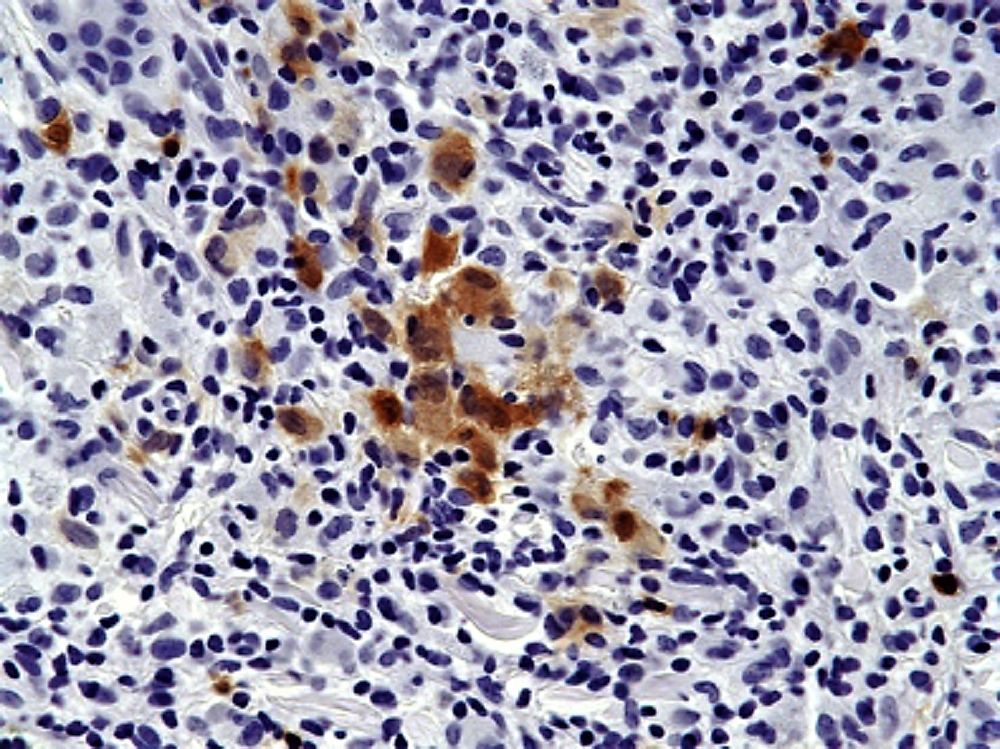
Positive stains
- Positive for S100, CD1a, CD68
- Variably express CD4, CD45, CD56, lysozyme
- References: Am J Dermatopathol 2018;40:736, Blood 2015;126:2344, Arch Pathol Lab Med 2003;127:748, Am J Surg Pathol 2008;32:1868
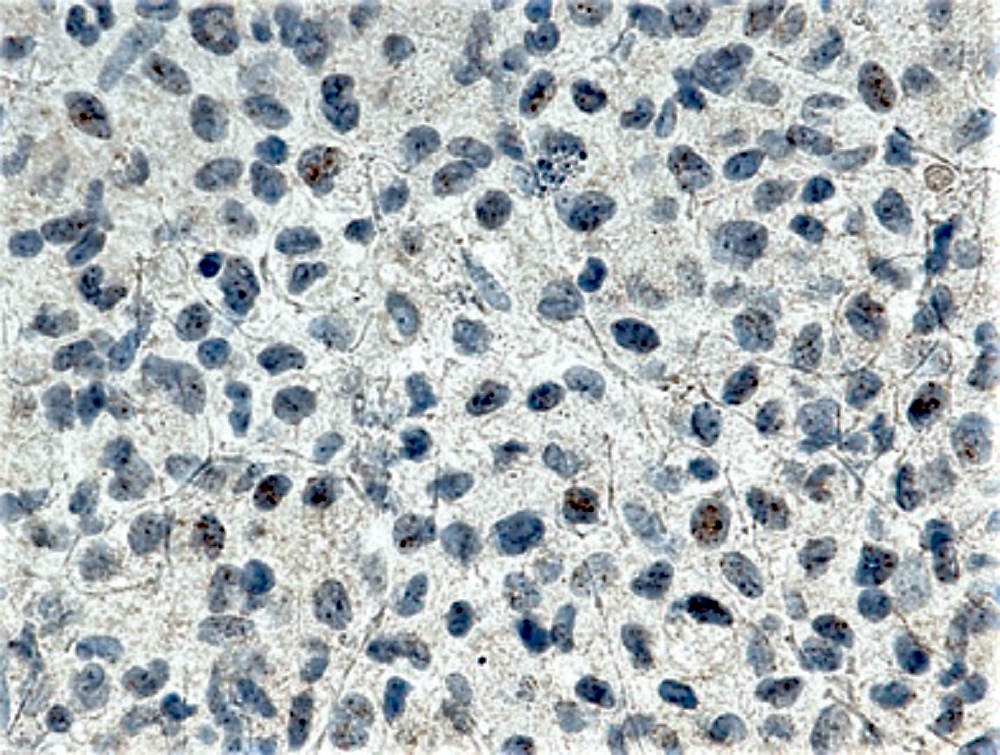
Negative stains
- Negative for langerin (CD207)
- Negative for histiocytic marker CD163
- B cell and T cell markers, follicular dendritic cell markers (CD21, CD23 and CD35), CD30 and MPO
- References: Am J Dermatopathol 2018;40:736, Blood 2015;126:2344, Arch Pathol Lab Med 2003;127:748, Am J Surg Pathol 2008;32:1868
Flow cytometry description
- No known abnormalities in peripheral blood flow cytometry in true cutaneous indeterminate cell histiocytosis
- For flow cytometry information for cases of chronic myelomonocytic leukemia with an indeterminate cell-like immunophenotype, please refer to chronic myelomonocytic leukemia
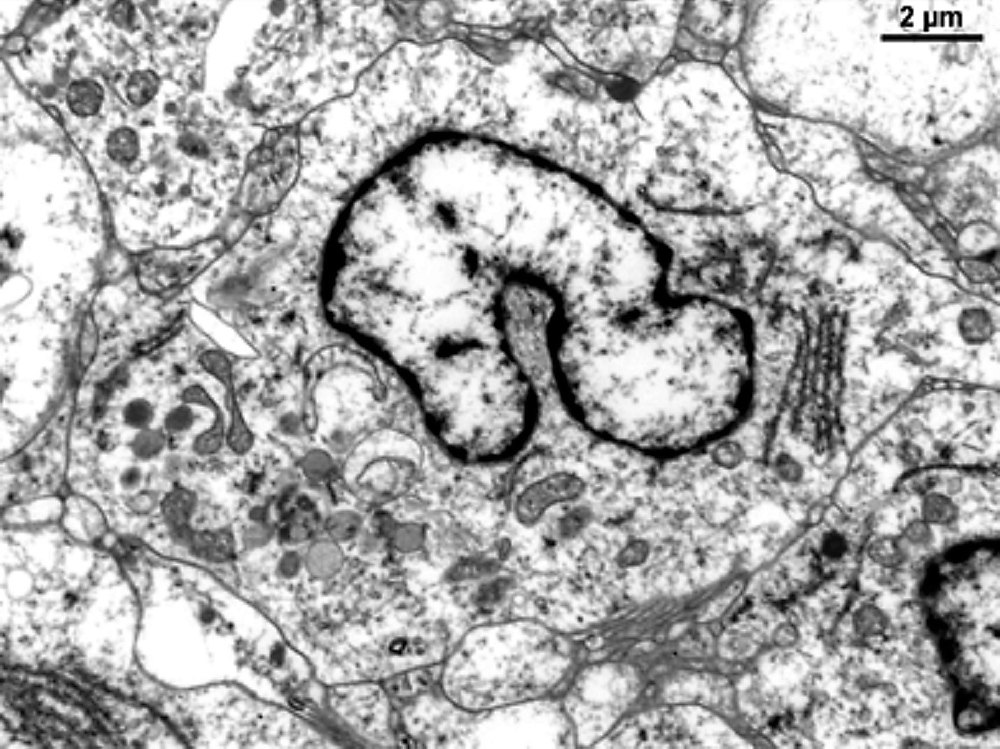
Electron microscopy description
- Histiocytic cells show nuclear infoldings with peripheral villi (Rare Tumors 2013;5:e13)
- Lamellated dense bodies but no Birbeck granules (Acta Derm Venereol 2002;82:288)
Molecular / cytogenetics description
- ETV3::NCOA2 in a subset (Blood 2015;126:2344, BMJ Case Rep 2017;2017:bcr2017221538)
- BRAF V600E in rare cases (Ann Diagn Pathol 2015;19:113, Virchows Arch 2017;471:467)
- Can share clonal abnormality of associated lymphoma or leukemia (Am J Surg Pathol 2008;32:1868)
- TP53 in 1 case (Leukemia 2022;36:573)
Sample pathology report
- Skin, left arm, biopsy:
- Compatible with indeterminate cell histiocytosis (see comment)
- Comment: The presence of histiocytes that express CD1a without langerin is compatible with a diagnosis of indeterminate cell histiocytosis (ICH). The definitive etiology of ICH is not known. ICH may represent a distinct entity, as suggested by the detection of ETV3::NCOA2 in a subset of cases or a variant of Langerhans cell histiocytosis (LCH) that has lost its Birbeck granules (Blood 2015;126:2344). Furthermore, chronic myelomonocytic leukemia (CMML) presenting with skin lesions rarely may mimic the immunohistochemical phenotype of ICH (J Cutan Pathol 2017;44:1075). If clinically indicated, correlation with genomic sequencing to assess for molecular aberrancies characteristic of ICH, LCH or CMML is recommended.
- Microscopic description: The histologic sections show skin with a nodular infiltrate of epithelioid cells with abundant eosinophilic cytoplasm, vesicular and variably reniform nuclei and prominent nucleoli present in sheets in the superficial and mid-dermis. On immunohistochemical staining, the lesional cells are positive for CD1a, S100 and CD68 and are negative for langerin, MPO and BRAF V600E.
Differential diagnosis
- Langerhans cell histiocytosis:
- CD1a+, langerin (CD207)+ (100%), S100+, CD68+, BRAF VE1 (~50%)
- Juvenile xanthogranuloma:
- CD1a-, langerin (CD207)-, S100 variable, CD68+
- Multicentric reticulohistiocytosis:
- CD1a-, langerin (CD207)-, S100 variable, CD68+
- Interdigitating dendritic cell sarcomas:
- CD1a-, langerin (CD207)-, S100+, SOX10+
- Histiocytic sarcoma:
- Significant cytologic atypia, CD1a-
- Chronic myelomonocytic leukemia secondarily involving the skin:
- Can have identical morphologic and immunohistochemical findings, correlate with molecular studies (J Cutan Pathol 2017;44:1075)
- Reactive indeterminate cell infiltrates:
Board review style question #1
Which of the following electron microscopy findings is most consistent with a diagnosis of indeterminate cell histiocytosis (ICH)?
- Lack of Birbeck granules
- Presence of Birbeck granules
- Presence of characteristic cytoplasmic inclusions
- Proliferation of Langerhans cells
Board review style answer #1
A. Lack of Birbeck granules. Electron microscopy shows a lack of Birbeck granules in indeterminate cell histiocytosis.
Comment Here
Reference: Indeterminate cell histiocytosis / indeterminate dendritic cell tumor
Comment Here
Reference: Indeterminate cell histiocytosis / indeterminate dendritic cell tumor
Board review style question #2
Board review style answer #2
D. CD207 (langerin) positivity in the Langerhans cells is specific for this disorder. Langerhans cells also typically stain for S100, CD1a and CD68 but CD1a is also expressed in indeterminate cell histiocytosis and CD68 and S100 can be seen in other histiocytic neoplasms. CD45 is a nonspecific leukocyte marker. CD20 is a B cell marker.
Comment Here
Reference: Indeterminate cell histiocytosis / indeterminate dendritic cell tumor
Comment Here
Reference: Indeterminate cell histiocytosis / indeterminate dendritic cell tumor