Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Immunohistochemistry & special stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Latchmansingh K, Chapman J. Primary cutaneous CD4+ small or medium T cell lymphoproliferative disorder. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomanonbcutaneouscd4.html. Accessed September 17th, 2025.
Definition / general
- Primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder affects primarily upper dermis and is composed of a predominance of small to medium sized pleomorphic CD4+ T cells that presents as a solitary skin lesion without evidence of an underlying cutaneous lymphoma, such as mycosis fungoides, that is characterized by longstanding patches or plaques
- By definition, the clinical course is benign
Essential features
- Solitary plaque or nodule on the face, neck or upper trunk
- Slow growing
- Epidermotropism only focal
- Small / medium pleomorphic CD4+ T cells with T follicular helper (TFH) markers
- Heterogenous background of hematolymphoid cells with hyperplastic B cells
- Low proliferation rate by Ki67 (5 - 20%)
- Large cells ≤ 30% of total infiltrating cells
Terminology
- Primary cutaneous CD4+ small / medium T cell lymphoma (no longer used due to benign clinical course)
ICD coding
- ICD-O: 9709/1 - primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder
Epidemiology
- Rare, approximately 2% of all cutaneous T cell lymphomas / lymphoproliferative disorders
- Usually adults or elderly; children rarely affected
- M = F
Sites
- Solitary plaque or nodule on face, neck, upper trunk
- Lower extremity, multifocal involvement is rare
Etiology
- Skin homing CD4+ T cells with follicular T helper phenotype
Clinical features
- Usually asymptomatic
- Usually a solitary, red-purple, slow growing skin lesion commonly located on the face, neck or upper trunk
- Rarely can present as multiple lesions; however, patches or plaques diagnostic of mycosis fungoides exclude the diagnosis
Diagnosis
- Tissue biopsy with complementary immunohistochemical stains, T cell receptor genes clonality studies and clinical correlation
Prognostic factors
- Excellent prognosis
- Spontaneous remission following biopsy has been reported
- Local recurrences are rare
Case reports
- 30 year old Chilean man with a 4 month history of multifocal, intermittently itchy, erythematous to violaceous nodules and plaques on the face (Clin Case Rep 2019;7:2405)
- 36 year old woman with a progressively growing purplish erythematous nodule on the left nasal ala (An Bras Dermatol 2019;94:99)
- 56 year old man with an 8 month history of multifocal cutaneous nodules, first appearing on his right leg with gradual progression to lesions on his left arm and bilateral legs (Cureus 2020;12:e8534)
Treatment
- Can be successfully treated with any of the following:
- Intralesional steroids
- Surgical excision
- Radiotherapy
Gross description
- Solitary skin colored / red-purple plaque or nodule
Frozen section description
- Frozen sections should not be performed in these lesions
Microscopic (histologic) description
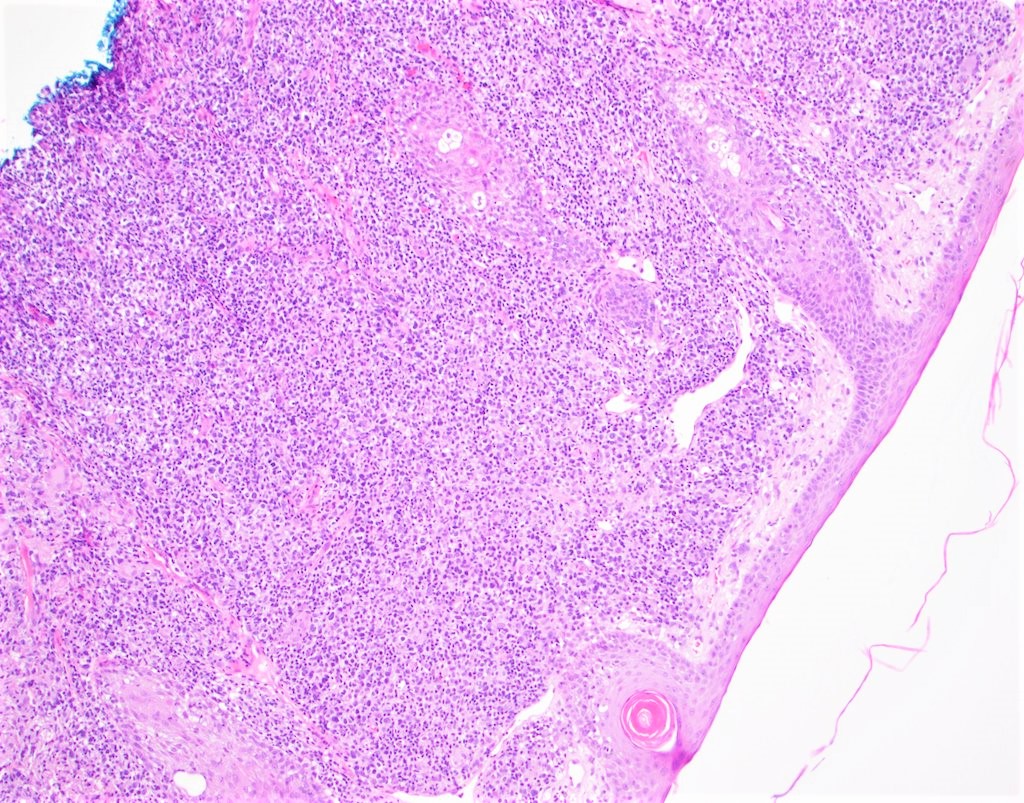
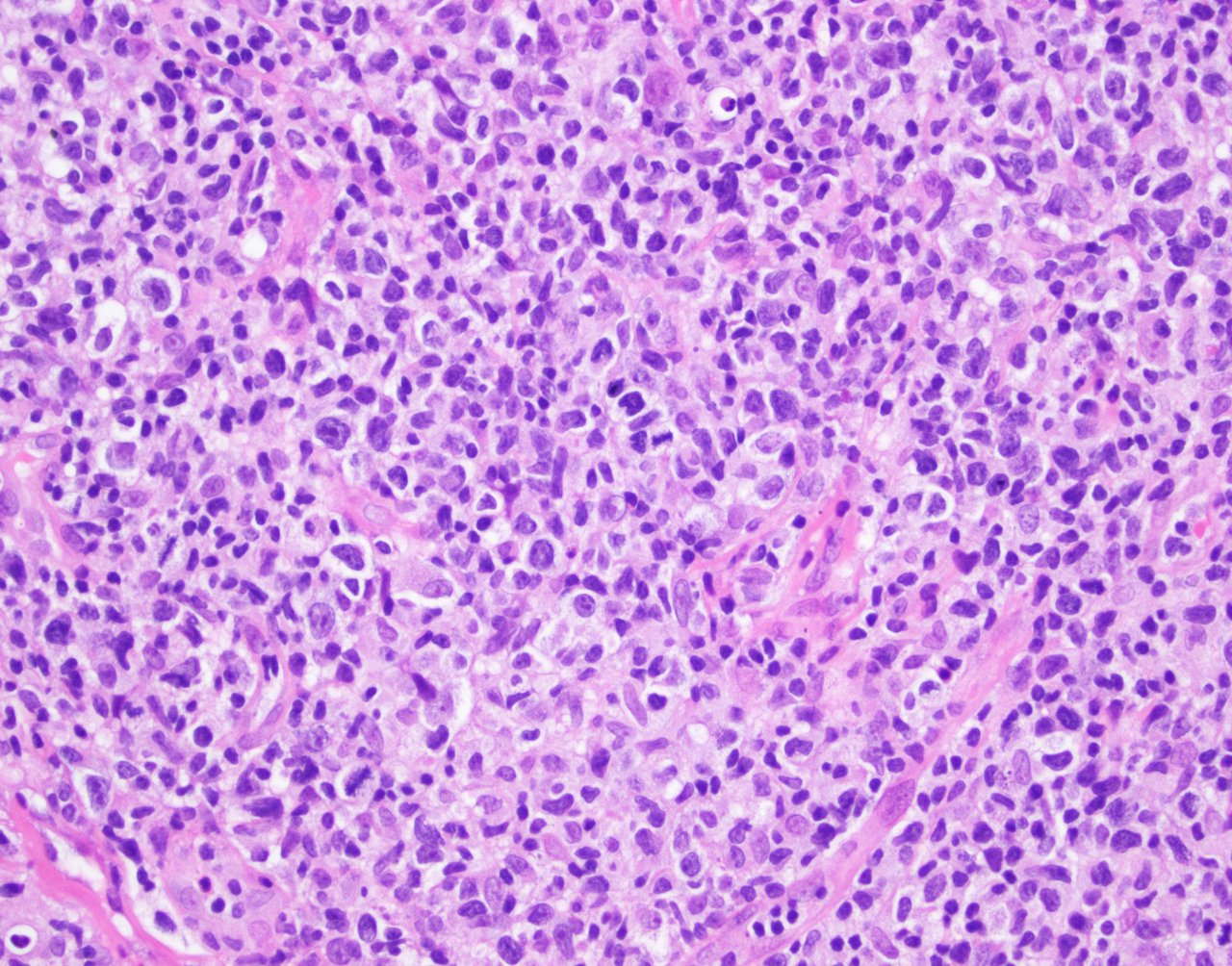
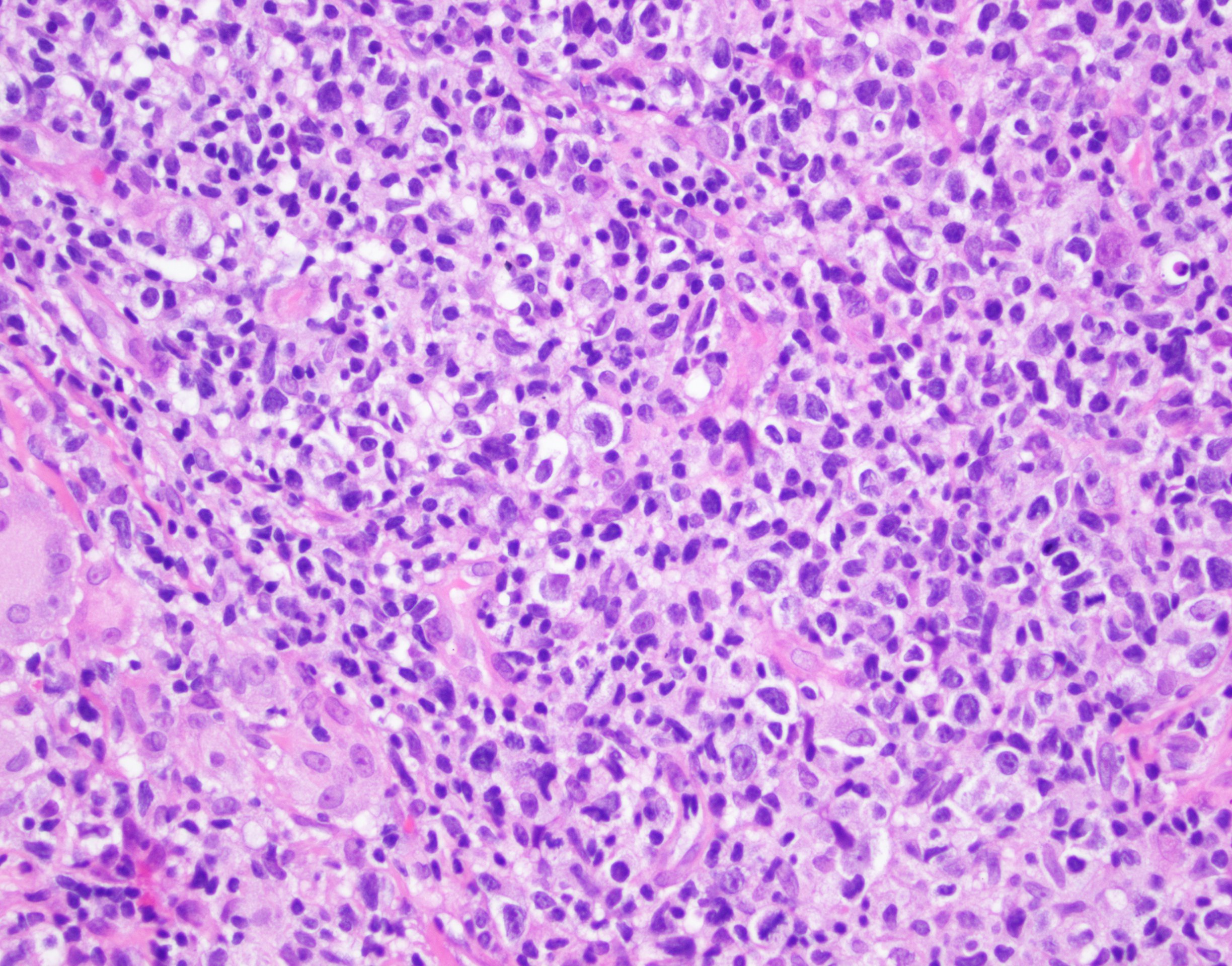
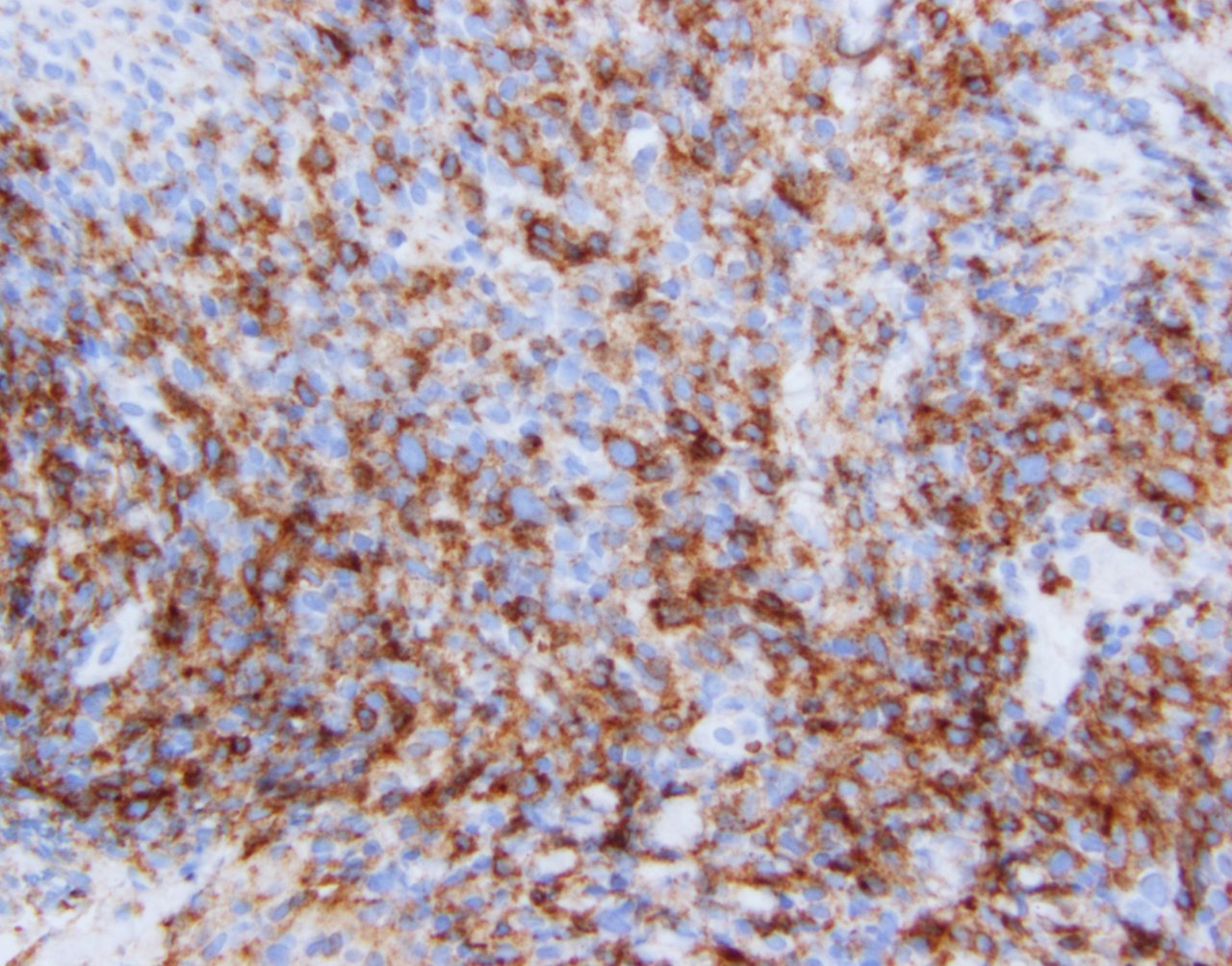
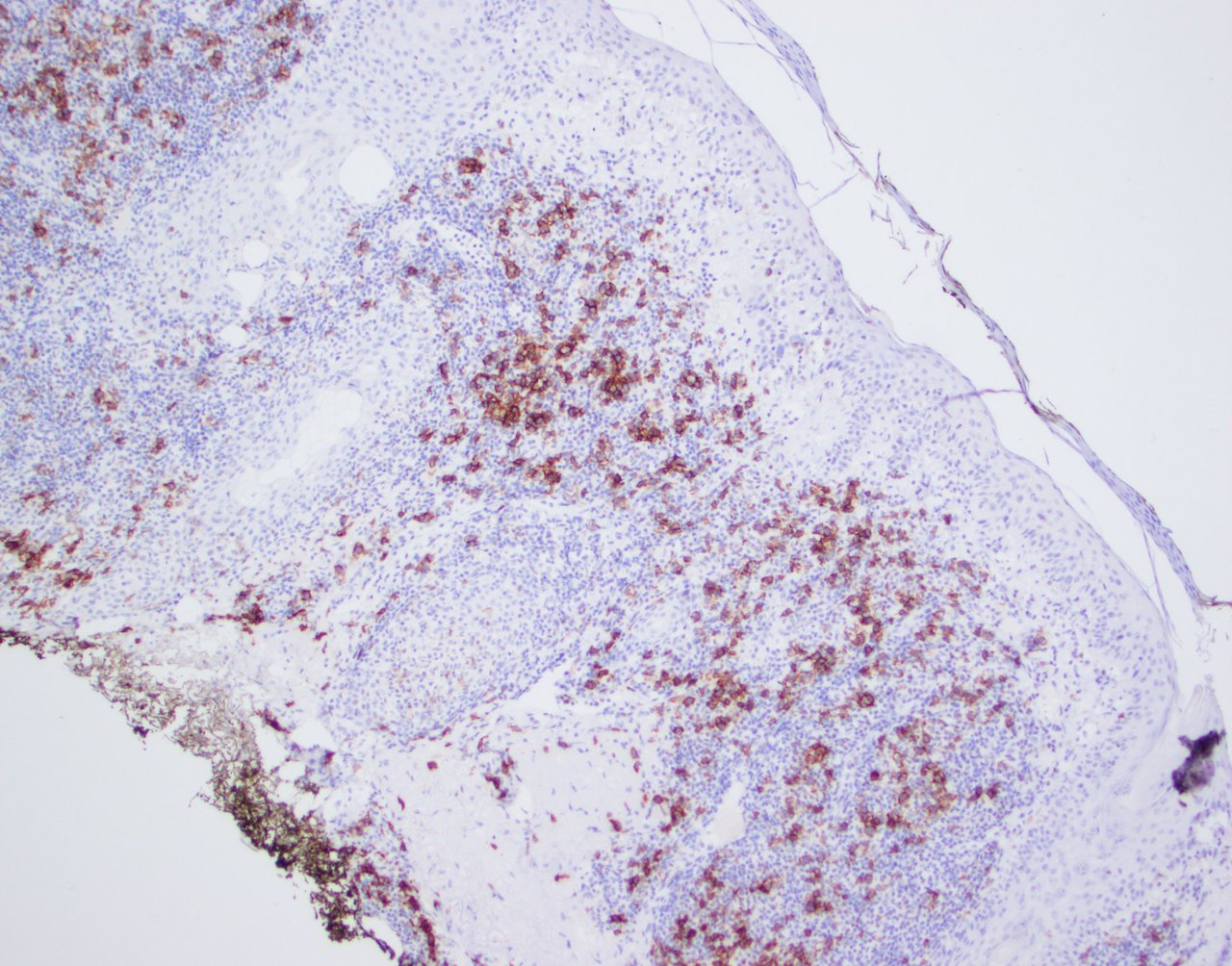
- Dense, diffuse or nodular dermal hematolymphoid infiltrates with extension into the subcutaneous tissue
- Focal epidermotropism may be present but should be limited; prominent epidermotropism should not be seen
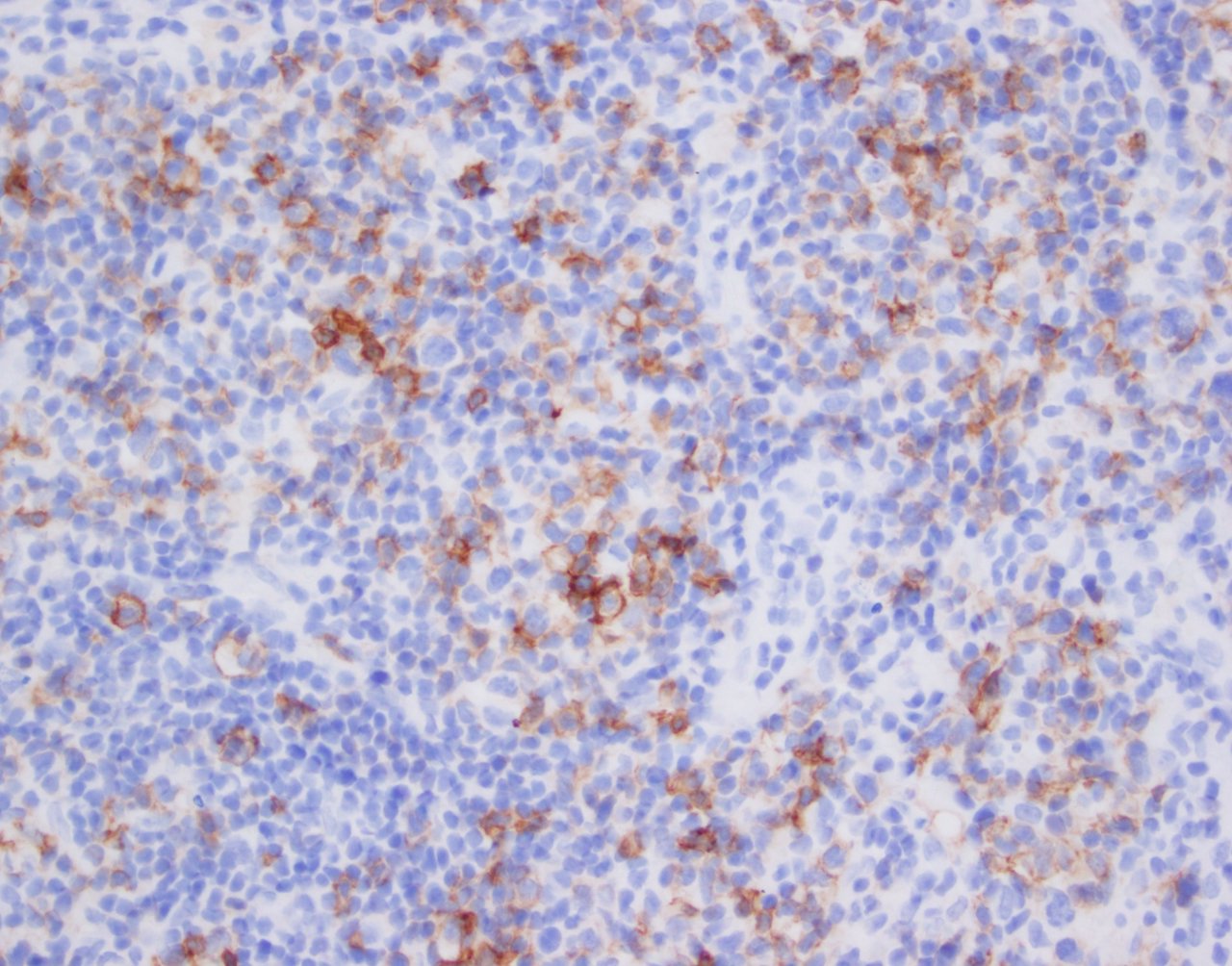
- Small / medium sized pleomorphic CD4+ T cells are frequent
- Large pleomorphic cells may be present but should be < 30% of all cells
- Polymorphic background, including small CD8+ T cells, B cells, plasma cells and histiocytes including multinucleated giant cells
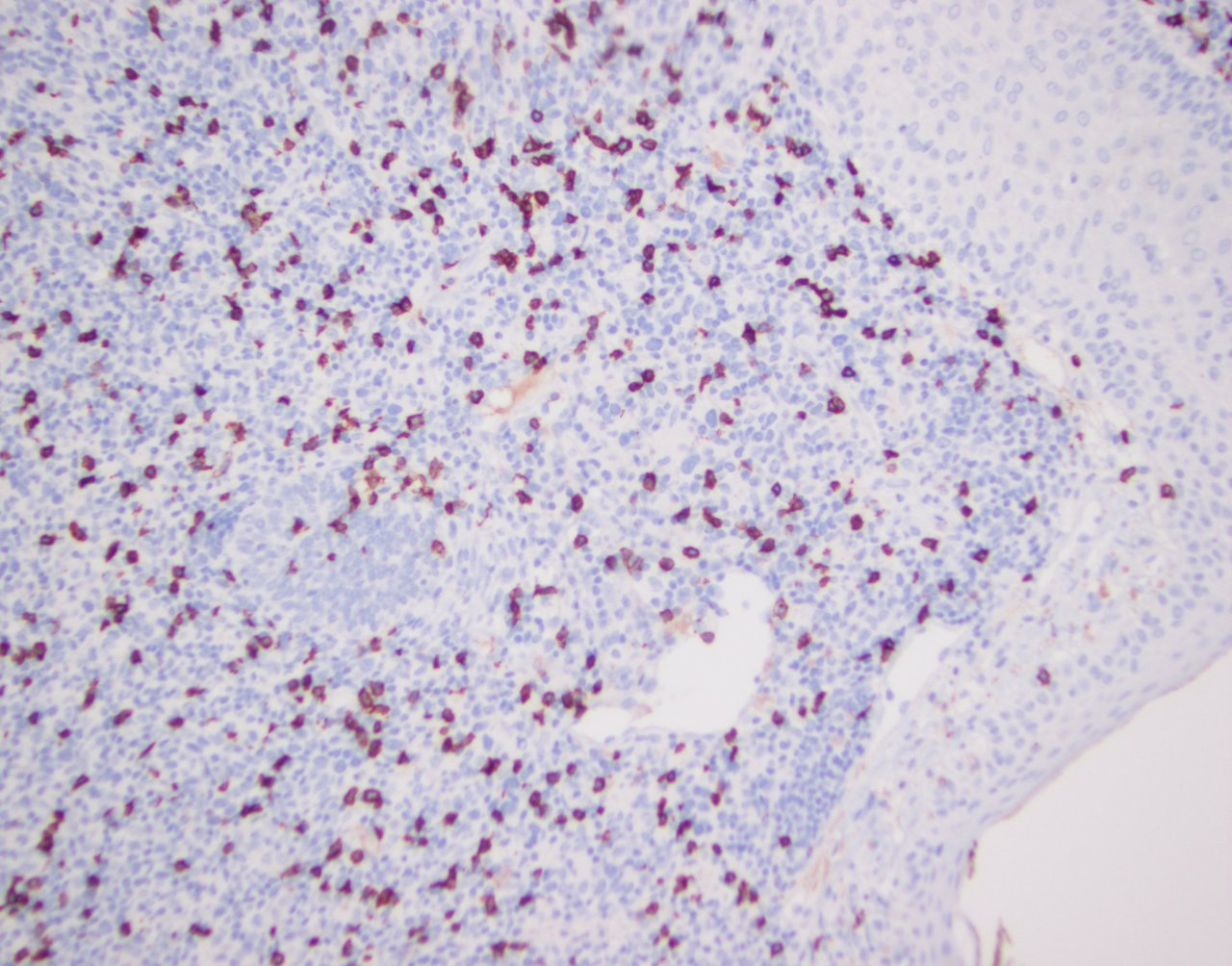
- Ki67 proliferation index is low (5 - 20%)
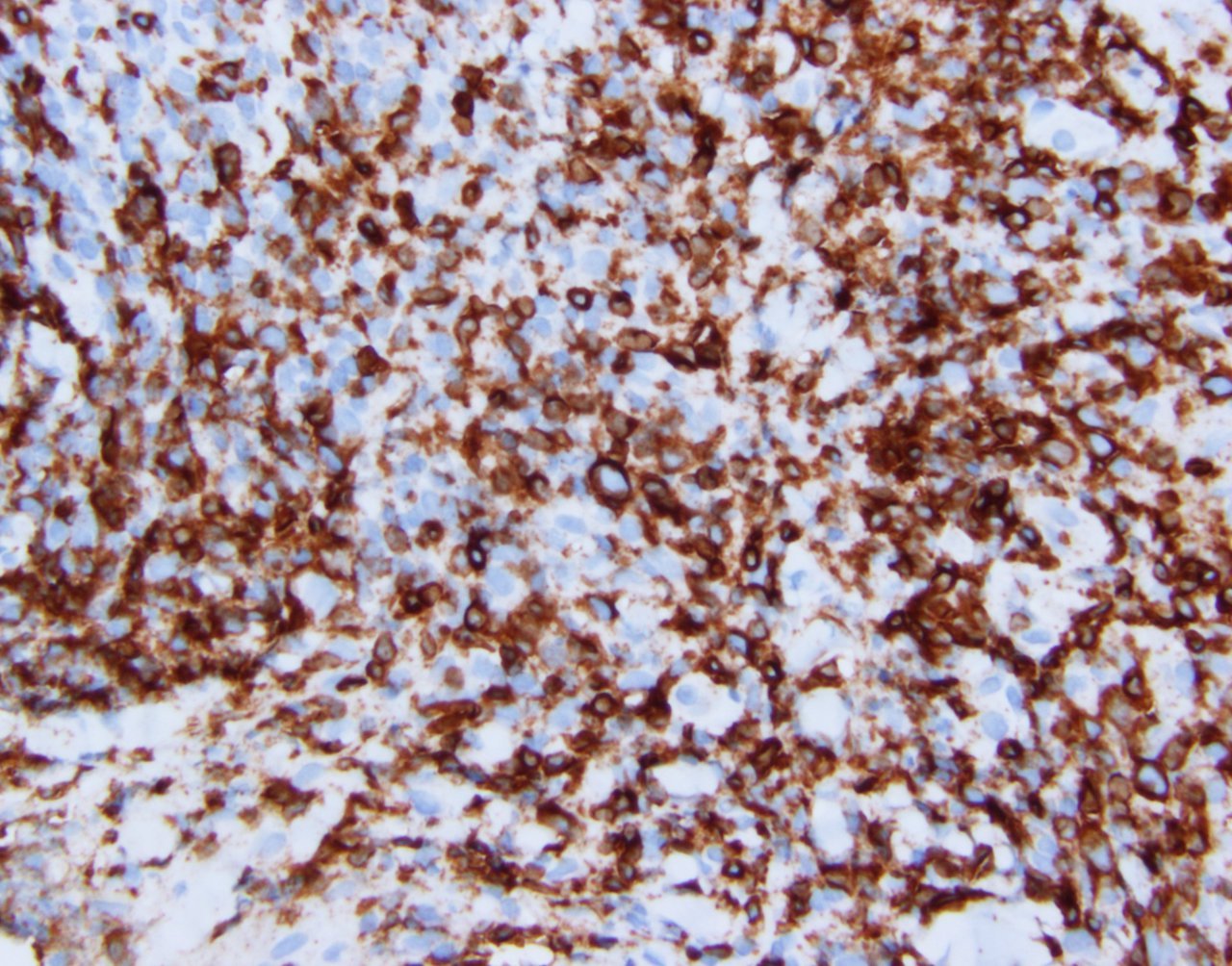
Microscopic (histologic) images
Contributed by Jennifer Chapman, M.D.
Cytology description
- Pleomorphic population of T cells: small to medium sized and occasional large lymphoid cells, which may have irregular nuclear contours
- Large cells < 30% of all cells in the infiltrate
- Heterogenous background of small lymphocytes, plasma cells, histiocytes and occasionally multinucleated giant cells
Immunohistochemistry & special stains
Flow cytometry description
Molecular / cytogenetics description
- Clonally rearranged TCR genes in most cases
- Specific genetic abnormalities have not been described
Sample pathology report
- Face, left central malar cheek, biopsy:
- Atypical CD4+ T cell infiltrate consistent with primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder in an appropriate clinical context (see comment)
- Comment: The patient is a 21 year old woman who recently developed a left cheek lesion. Histologic sections show skin punch biopsy with a dense dermal hematolymphoid infiltrate. The infiltrate is vaguely nodular and diffuse in distribution and is composed of mostly small to medium sized lymphocytes with scattered large, occasionally pleomorphic lymphoid cells. Clusters of small lymphoid cells and plasma cells are also present. Epidermotropism is focal. There is no diffuse growth of large cells.
- Immunohistochemical stains highlight predominantly small to medium sized cells and occasional large, pleomorphic cells that are positive for the T cell markers CD3 and CD5, as well as for the T follicular helper markers BCL6, CXCL13 and PD1 (subset) and negative for CD10. The majority of the T cells present are CD4+ with relatively fewer CD8+ cells. In comparison to CD4+ T cells, CD8+ cells are small and cytologically unremarkable. CD20+ and CD79a+ B cells arranged in vague aggregates are present. B cells are small and mature in appearance. Kappa and lambda light chain assessment by in situ hybridization highlights few scattered, polytypic plasma cells. CD30 stains few, scattered, variably sized lymphoid cells. Concurrent polymerase chain reaction (PCR) for TRB and TRG demonstrated monoclonal T cell receptor gene rearrangements.
- The overall findings are those of an atypical CD4+ T cell proliferation with histopathologic features consistent with those of primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder. If this patient is presenting only with a solitary, slow growing lesion on the face, this clinical presentation would support this diagnosis. However, if the patient has multiple lesions or a recurring rash, other differential diagnostic possibilities, such as mycosis fungoides, should be considered. Clinical correlation is therefore required.
Differential diagnosis
- Mycosis fungoides:
- Usually presents as unremitting patches or plaques with epidermotropism
- Cutaneous involvement by systemic T cell lymphoma of T follicular helper immunophenotype:
- There is a history of systemic T cell lymphoma with secondary involvement of skin
- Benign inflammatory infiltrate:
- Unable to differentiate histologically and clinically, except for clonality, however both have a benign course and respond to intralesional therapy
- Extranodal marginal zone lymphoma (MALT lymphoma):
- Adult T cell leukemia / lymphoma:
- Systemic involvement by large pleomorphic neoplastic CD4+ T cells that display a T regulatory phenotype
Additional references
Practice question #1
Which of the following features would be most helpful in favoring a diagnosis of primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder over angioimmunoblastic lymphoma involving the skin?
- Clinical history of localized single lesion
- Destructive architecture
- High degree of cytologic atypia in CD4+ T cells
- Immunophenotype positive for PD1 and CXCL13
- Polymorphic nature of infiltrate, with small lymphocytes, plasma cells and histiocytes
Practice answer #1
A. Clinical history of localized single lesion. Although angioimmunoblastic T cell lymphoma in primary sites (nodal) shows characteristic histologic features, including prominent arborizing vessels and expanded follicular dendritic cell meshworks, secondary involvement of cutaneous sites may not show these diagnostic features. The immunophenotype (answer D), degree of cytologic atypia (answer C) and polymorphic nature of associated nonneoplastic cells (answer E) is similar in angioimmunoblastic T cell lymphoma involving skin and CD4+ small / medium T cell lymphoproliferative disorder.
Comment Here
Reference: Primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder
Comment Here
Reference: Primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder
Practice question #2
A 75 year old man presents with a 3 cm nodule on his left neck. He reports he previously had small red plaque-like lesions in the same area and on his upper back 2 years ago, which were treated with steroids with minimal improvement. Biopsy of the nodule demonstrated abnormal small to intermediate in size CD4+ T cells showing epidermotropism and scattered CD30+ large cells. What is the most likely diagnosis?
- Angioimmunoblastic T cell lymphoma
- CD4+ small / medium T cell lymphoproliferative disorder
- Mycosis fungoides
- Peripheral T cell lymphoma, NOS
- Primary cutaneous anaplastic large cell lymphoma
Practice answer #2
C. Mycosis fungoides. The history of multiple, red plaque-like lesions unresolved following steroid treatment now presenting as a mass / nodule with epidermotropic atypical T cells is most likely consistent with mycosis fungoides, tumor stage. This clinical presentation is not consistent with that of CD4+ small / medium T cell lymphoproliferative disorder (answer B); that is characterized by the presence of a single lesion. The isolated cutaneous presentation would not be typical for angioimmunoblastic T cell lymphoma (answer A). Primary cutaneous anaplastic large cell lymphoma (answer E), characterized by the presence of sheets of large cells that express CD30, is excluded as a diagnostic possibility based on the description of only scattered CD30+ large cells. Since the histologic and clinical features are consistent with mycosis fungoides, this diagnosis would be favored as a more specific lymphoma classification over peripheral T cell lymphoma, NOS involving skin (answer D).
Comment Here
Reference: Primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder
Comment Here
Reference: Primary cutaneous CD4+ small / medium T cell lymphoproliferative disorder