Cite this page: Scungio D. Bloodborne pathogens. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/managementlabbloodbornepathogens.html. Accessed April 24th, 2024.
Definition / general
- The work performed in clinical and anatomical pathology laboratories is often performed while handling infectious patient samples of many types
- The hazards posed by these samples vary, and proper handling and use of protective equipment is imperative to ensure the safety of laboratory personnel
- OSHA's Bloodborne Pathogens standard oversees the proper transport, storage and handling of bio-hazardous substances in the laboratory
Regulation
- Bloodborne pathogens regulatory agencies:
- Occupational Safety and Health Administration (OSHA)
- 29 CFR 1910.1030: Bloodborne Pathogens - 1991
- U.S. Centers for Disease Control (CDC) / The National Institute for Occupational Safety and Health (NIOSH)
- Information for Employers Complying with OSHA's Bloodborne Pathogens Standard - 2009 (CDC)
- College of American Pathologists (CAP)
- Laboratory general inspection checklist
- Occupational Safety and Health Administration (OSHA)
Laboratory
- Laboratory requirements:
- Written exposure control plan (ECP)
- Updated annually
- Standard operating procedures
- Six major components:
- (1) Administration and exposure risk
- Define responsibilities of employees, supervisors and managers
- State who is responsible for the implementation and maintenance of the ECP
- State who is responsible for provision and maintenance of PPE, employee health administration and training
- Perform risk assessments to determine exposure risk for each employee category (technologist, phlebotomist, pathologist, etc.)
- Perform task assessments to determine exposure risk for laboratory procedures
- (2) Exposure control methods
- Describe the various methods the laboratory will use to prevent occupational exposure
- Mitigation of risk occurs through a "Hierarchy of Controls"
- Elimination of risk
- Preferred, but not usually feasible in the laboratory setting
- Engineering controls
- Physical change or application to the workplace to improve safety
- Ventilation hoods
- Safety shields
- Biological safety cabinets
- Administrative controls
- Require the employee to take an action to minimize the risk
- Include work practice controls
- No eating, drinking, smoking, applying cosmetics or lip balm and handling contact lenses in work areas
- Do not pick up broken glassware directly with hands
- Wash hands immediately or as soon as feasible after removal of gloves or other personal protective equipment
- Personal Protective Equipment (PPE)
- Considered least effective control in the hierarchy
- Requires the employee to wear something in order to reduce exposure risk
- Type of PPE used chosen based on the risk and task assessments
- Lab coats, gloves, face shields, aprons, respirators, etc.
- Elimination of risk
- (3) Vaccinations
- Hepatitis B vaccine must be offered to all potentially exposed employees
- Employees who refuse should fill out a vaccine declination form
- Employees who decline may reconsider later
- (4) Post-exposure follow-up
- ECP requires a complete exposure follow-up program
- First aid
- Clean the wound, flush eyes or other mucous membrane, etc.
- Incident evaluation
- Obtain information about how the exposure occurred and the route of entry
- Identify the source individual, if possible
- Obtain consent and make arrangements to have the source individual tested to determine HIV, HCV and HBV infectivity
- Ensure test results are given to the exposed employee
- Treat high-risk exposures as emergent in order to expedite the treatment or prophylaxis process
- Medical follow up
- Provided by licensed medical practitioner
- Provide employee with written evaluation of exposure and any further necessary treatment options within 15 days of the incident evaluation
- All involved parties document complete exposure incident evaluation
- Include review of engineering controls in place, work practices used, employee training, location and procedure being performed and PPE used
- First aid
- ECP requires a complete exposure follow-up program
- (5) Communication
- Provide information to laboratory employees about hazards in the workplace through labels and signage
- Use biohazard symbol for labeling (see figure 1)
- Label items that are used to contain or transport blood or OPIM
- Refrigerators / freezers
- Incubators
- Transport coolers
- regulated waste containers
- Biohazard symbol at the entryway to HIV and HBV Research Laboratory and Production Facilities required by OSHA
- CDC requires this entryway signage for all biological laboratories (CDC)
- (6) Training and records
- All employees need access to Bloodborne Pathogens standard
- All employees must be trained on all aspects of the ECP
- Training should occur upon employment, annually and whenever there is a change made to procedures which involve potential exposure
- Keep all training records for at least three years
- Employee medical records are maintained for the duration of employment plus 30 years
- Maintain a sharps injury log for any percutaneous injury acquired from a contaminated needle or other such device
Images hosted on other servers:
- Written exposure control plan (ECP)
Administration
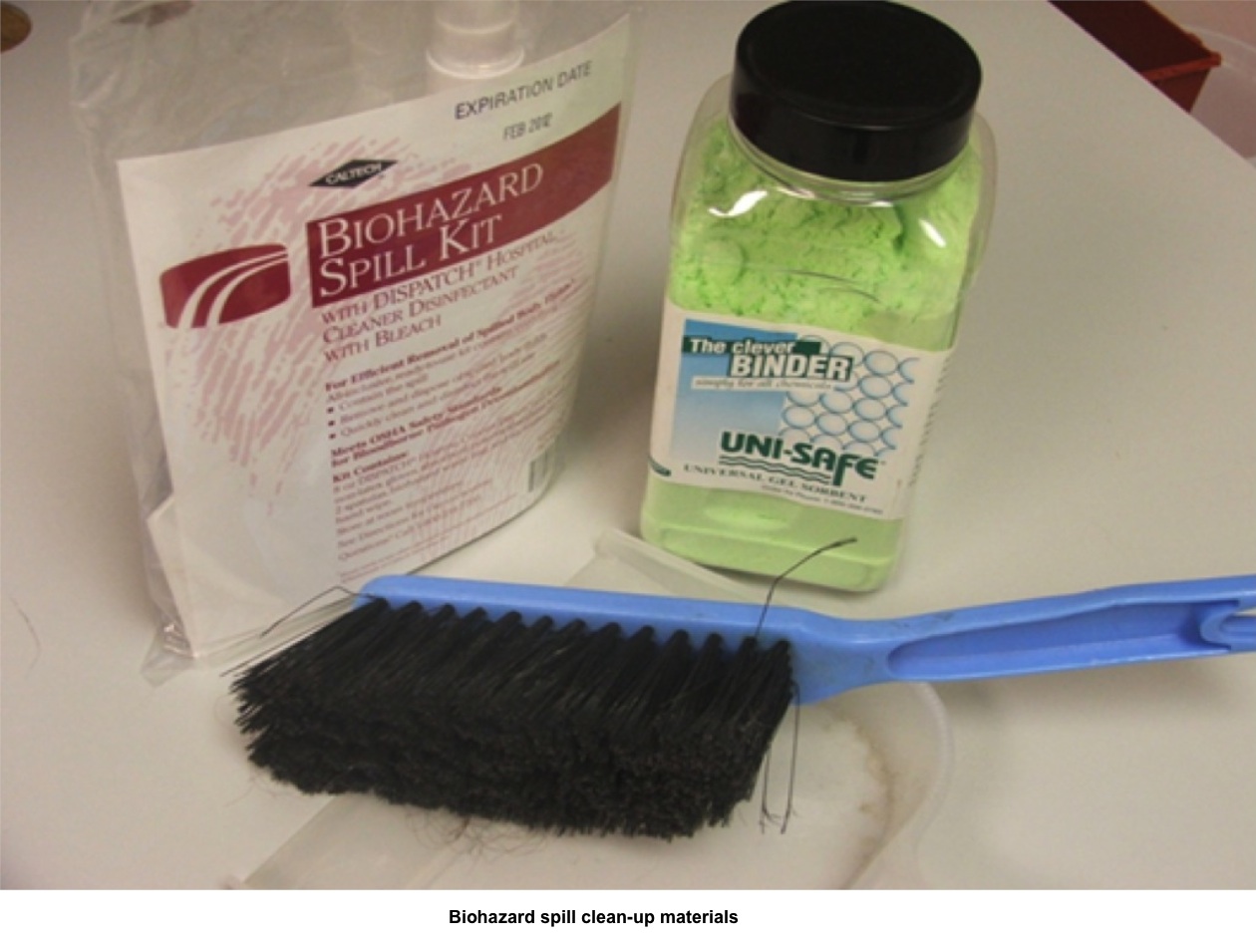
- Biohazard spill handling:
- Provide spill response training for all staff that handles blood or body fluids
- Ensure use of PPE
- Confine or contain the spill
- Inspect for broken glass
- Absorb with towels or spill pillows
- Use blood / body fluid absorbent if available (see figure 2)
- Mop or sweep up the spill
- Dispose of waste in proper receptacles
- Disinfect spill area with 10% bleach solution
- Annual review of exposure control plan:
- Analyze effectiveness of your ECP
- Review exposure incidents
- Review training
- Review blood / body fluid spills
- Update employee risk exposure documentation
- Review / update task assessments
- Provide annual bloodborne pathogens training
Contributed by Dan Scungio, MT (ASCP), SLS, CQA (ASQ)
- Analyze effectiveness of your ECP