Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Martinez A. Juvenile trabecular ossifying fibroma and psammomatoid ossifying fibroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillajuvossifyingfibroma.html. Accessed April 19th, 2024.
Definition / general
- Juvenile ossifying fibroma (JOF) is a rare variant of ossifying fibroma (OF), a benign fibro-osseous lesion
- It has aggressive behavior
- It has two histologic subtypes:
- Juvenile psammomatoid ossifying fibroma
- Juvenile trabecular ossifying fibroma
Essential features
- Diagnosis of JOF is dependent on clinical, radiologic and pathologic correlation
- JOF, OF, fibrous dysplasia (FD) and osseous dysplasia may show significant histologic overlap particularly on small biopsies, however, clinical / surgical management of these entities is markedly different
- IHC is typically not useful to distinguish the entities
- Identifying fibro-osseous lesions which occur in association with hyperparathyroidism-jaw tumor (HJT) syndrome is important, as HJT is associated with development of other tumors, including carcinoma
Terminology
- Juvenile ossifying fibroma (JOF)
- Active ossifying fibroma (AOF)
- Juvenile active ossifying fibroma (JAOF)
- Juvenile trabecular ossifying fibroma (JTOF)
- Juvenile psammomatoid ossifying fibroma (JPOF)
Epidemiology
- The average age of JPOF is younger than conventional OF, with a slight male predominance
- Most cases occur in patients < 12 years old, though a wide age range has been reported (3 months to 72 years)
- JTOF primarily affects males, ages 8 - 12
Sites
- JPOF mainly occurs in the bony walls of the paranasal sinuses
- Paranasal sinus involvement is overall the most common location for JOF
- JTOF occurs more often in the maxilla
Etiology
- Ossifying fibromas are thought to originate from the periodontal ligament
Clinical features
- Can demonstrate rapid growth, causing local destruction and facial asymmetry
- Paranasal sinus or orbital bone involvement can cause nasal obstruction, proptosis, exophthalmia and visual changes
- Some lesions are found incidentally on routine radiographic exams
Diagnosis
- Diagnosis dependent on clinical, radiologic and pathologic correlation
Radiology description
- Well circumscribed lesion that can be radiolucent, mixed or radiopaque depending on the degree of calcification and presence of cystic areas
- On CT, well circumscribed lesion with mixed soft tissue and bone density
- May have thin "egg shell" periphery of bone
- Usually unilocular
Radiology images
Prognostic factors
- Excellent prognosis following complete excision
- 30 - 58% recurrence rate for incompletely excised tumors
Case reports
- 7 year old girl with firm swelling localized at the upper right maxillary region (Med Arch 2016;70:470)
- 10 year old boy with swelling of maxilla (Arch Pathol Lab Med 2003;127:e359)
- 15 year old boy with rapidly growing expansile lesion of jaw (Arch Pathol Lab Med 2001;125:1117)
- 18 year old man with 6 weeks of headache and blurred vision (Springerplus 2016;5:1089)
- 20 year old man with swelling in the right lower jaw (Contemp Clin Dent 2015;6:581)
- 27 year old man with long standing nasal congestion and recurrent sinus infections (Head Neck Pathol 2015;9:384)
Treatment
- Surgical excision
Clinical images
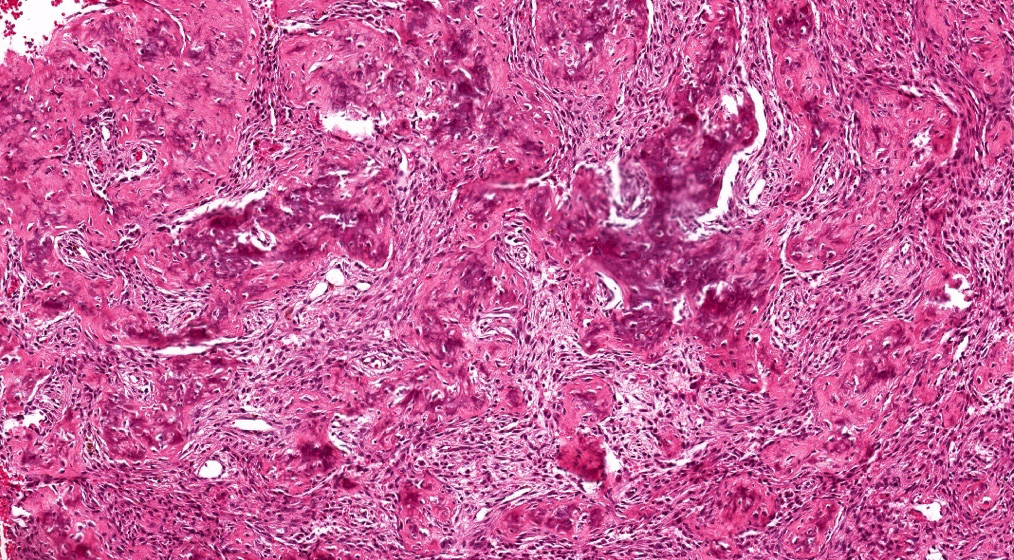
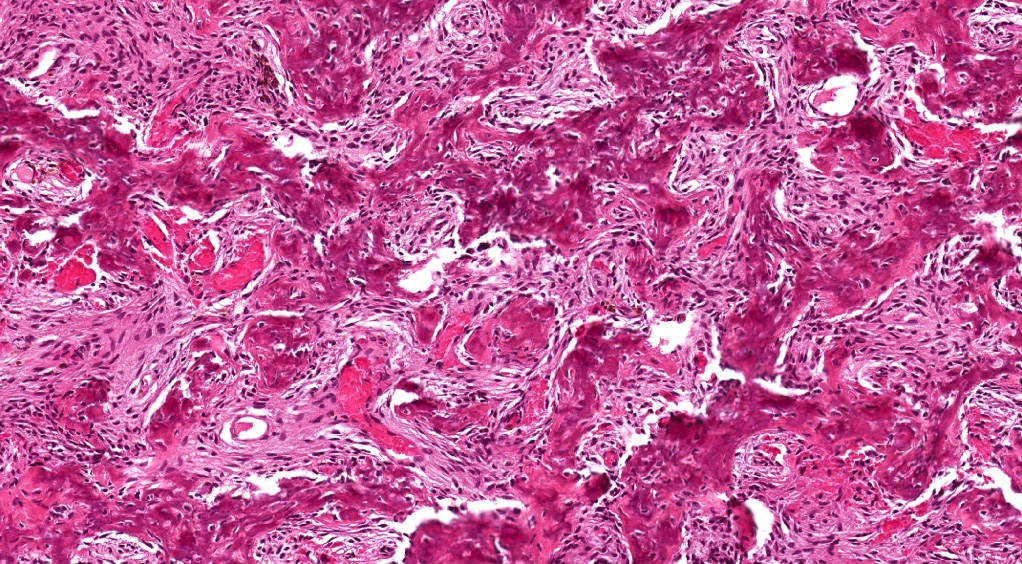
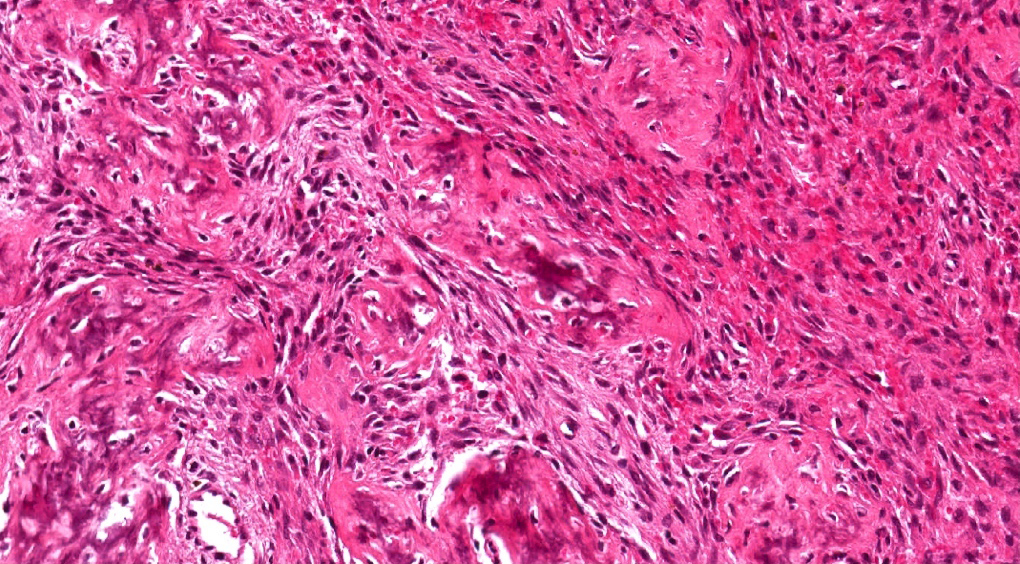
Microscopic (histologic) description
- Juvenile trabecular ossifying fibroma
- Cellular fibrous stroma composed of spindled to stellate fibroblastic cells with bands of osteoid without osteoblastic rimming together with immature bony trabeculae surrounded by plump osteoblasts
- Trabeculae can show an anastomosing or "lattice" pattern
- Mitoses can be present but without cytologic atypia
- Juvenile psammomatoid ossifying fibroma
- Fibroblastic stroma containing ossicles resembling psammoma bodies
- Ossicles may fuse to form trabeculae showing reversal lines
- Stroma can be cellular or loose / myxoid
- Fibroblastic stroma containing ossicles resembling psammoma bodies
- Both can have aneurysmal bone cyst type changes
- Pseudocystic stromal degeneration and hemorrhages
Microscopic (histologic) images
Contributed by Kelly R. Magliocca, D.D.S., M.P.H.
Images hosted on other servers:
Immunohistochemistry & special stains
- Stromal cells positive for RUNX2, an important transcription factor for the osteogenic lineage
- IHC may not be useful as other entities in differential, such as fibrous dysplasia, are RUNX2 positive
Molecular / cytogenetics description
- HPRT2 mutations have been found in OF (25 - 50%) associated with hyperparathyroidism-jaw tumor syndrome
Differential diagnosis
- Ossifying fibroma
- Conventional OF is more common than JOF
- May have similar radiographic appearance although conventional ossifying fibroma typically has a thin capsule
- More commonly occurs in the mandible
- Fibrous dysplasia
- Radiographic appearance is usually radiolucent, asymmetric with a "ground glass" appearance that blends into normal bone
- Histologically, has immature woven bone characterized by "Chinese letters" or "alphabet letters"
- Bony trabeculae usually without osteoblastic rimming
- Fibrous dysplasia tends to blend with surrounding bone and this continuity of normal and pathologic bone is not a typical feature of JOF
- Associated with GNAS mutations
- Osseous dysplasia
- Idiopathic process involving the periapical areas of teeth
- Many different types depending on location and extent of involvement
- Characterized by replacement of normal bone by metaplastic bone and fibrous tissue
- Cementoblastoma
- Neoplasm of cementum intimately involved with tooth root
- Radiographically is a radiopaque mass with a narrow radiolucent rim (pathognomonic)
- Histologically, consists of dense cementum-like tissue with reversal lines and fibroblastic stroma
- Most are in mandible
- Extra cranial (extra dural) meningioma
- Psamommatous meningioma variant most likely to create confusion
- Will be Somatostatin receptor subtype 2A (SSTR2A), EMA and variably PR positive
Additional references