Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Esmaeili A, Jassim SH. True thymic hyperplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mediastinumtruethymichyperplasia.html. Accessed April 19th, 2024.
Definition / general
- Defined as an increase of thymic gland size and weight while maintaining normal microscopic architecture
Essential features
- Thymus that is larger than normal limits for age (Ann Thorac Surg 1989;47:741)
- Expansion of the normal component of the thymic gland
- Incidental finding or compressive symptoms (J Vasc Nurs 2007;25:2)
Terminology
- True thymic hyperplasia
ICD coding
- ICD-10: E32.0 - persistent hyperplasia of thymus
Epidemiology
- Most often described in infants, children and young male patients
Sites
- Anterior mediastinum
Pathophysiology
- It is found to be the result of congenital neuroendocrine disturbances, usually within the hypothalamic hypophyseal system (Arkh Patol 1991;53:3)
Etiology
- Underlying pathogenesis of true thymic hyperplasia is largely unknown
Clinical features
- No symptoms, with the incidental finding of an anterior mediastinal mass on chest radiograph
- Compression of adjacent structures: respiratory distress, cough, wheezing, superior vena cava syndrome
- Acute or recurrent pulmonary infection
- Peripheral blood lymphocytosis
- References: Ann Thorac Surg 1989;47:741, J Vasc Nurs 2007;25:2
Diagnosis
- Diagnosis is based on the demonstration of an increased thymic weight with normal histology (Connolly: Autopsy Pathology - A Manual and Atlas, 3rd Edition, 2015, Arch Pathol 1962;74:244)
*Values from more recent studies show great variability depending on patient populationsApproximate thymus weight by age (mean ± standard deviation)* 1 month Male: 7.8 ± 5.3 g; female: 6.6 ± 4.9 g 12 months Male: 12 ± 5 g; female: 11 ± 8 g 6 - 25 years 25 g 26 - 35 years 20 g 36 - 65 years 16 g > 65 years 6 g
Laboratory
- Peripheral blood lymphocytosis (Ann Thorac Surg 1989;47:741)
Radiology description
- Diffuse symmetric enlargement of the thymic gland (neoplasm tends to manifest as a focal mass) (Cancer Imaging 2005;5:139)
Radiology images
Prognostic factors
- Overall, true thymic hyperplasia has a good prognosis
Case reports
- 9 month old girl with a very large left sided mediastinal mass (J Pediatr Surg 2010;45:1711)
- 25 year old woman with pure red cell aplasia (Interact Cardiovasc Thorac Surg 2022;34:697)
- 30 year old man with anterior mediastinal mass (Int J Surg Case Rep 2018;47:104)
Treatment
- Asymptomatic patients can be followed up periodically
- Main treatment for massive thymic hyperplasia is surgical resection
Gross description
- Enlarged thymus gland with no mass or lesion
Microscopic (histologic) description
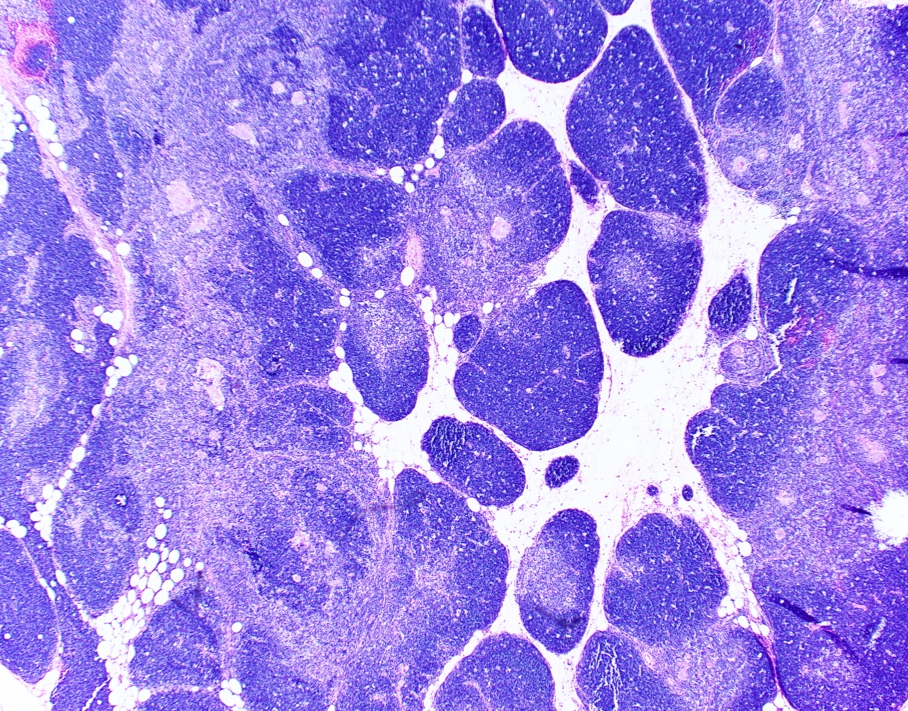
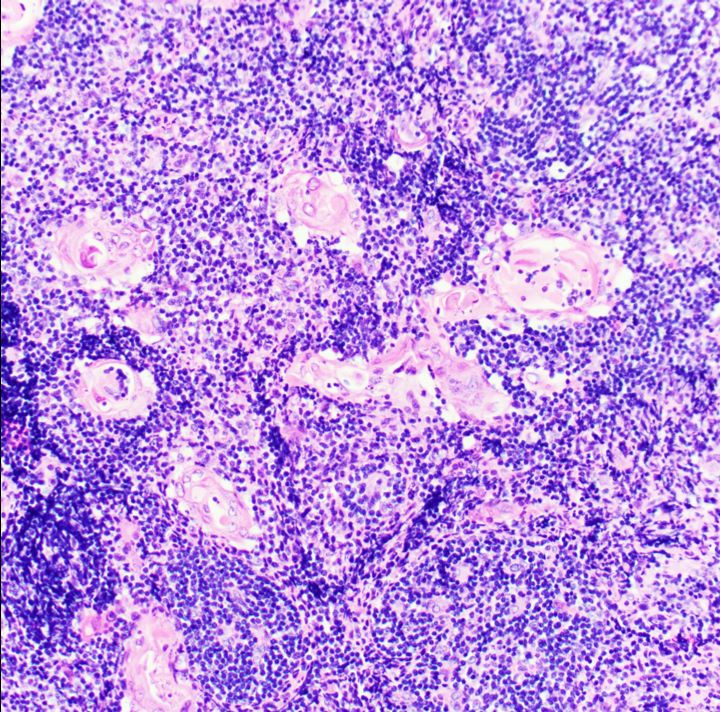
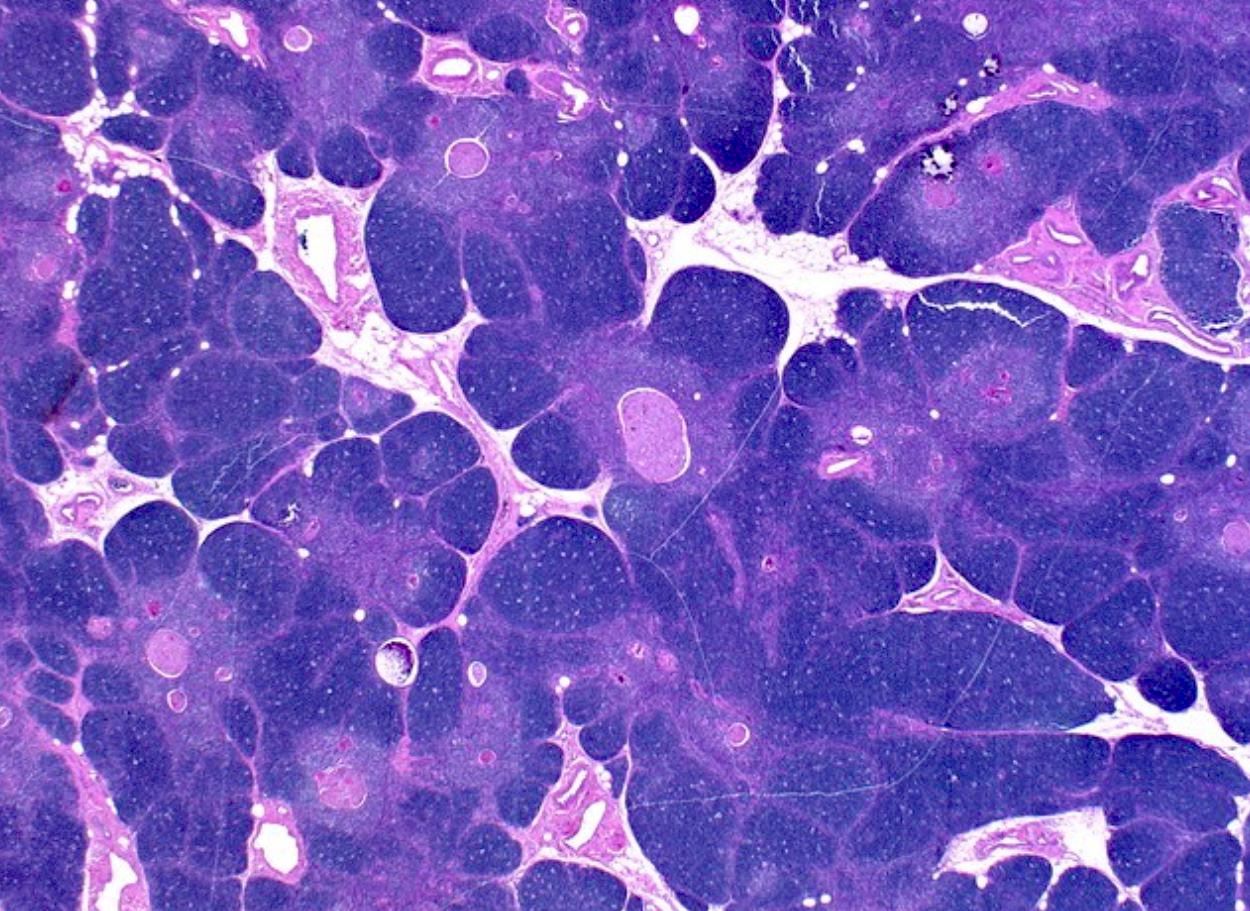
- Expansion of the normal component of the thymic gland (Histopathology 2009;54:69)
- Normal cortex, medulla and Hassall corpuscles
- No neoplasm
- No increased reactive germinal centers (Histopathology 2009;54:69)
- Lobular architecture and corticomedullary junction are preserved
Microscopic (histologic) images
Positive stains
Sample pathology report
- Thymus, thymectomy:
- True thymic hyperplasia (see comment)
- Comment: Sections show thymic tissue, characterized by lobular architecture featuring small cortical thymocytes that border interconnecting medullary tissue containing many Hassall corpuscles. The lobules are separated by mature fibroadipose tissue. There is no evidence of lymphoid hyperplasia. The average weight of the thymus gland in this age group is ~25 - 35 g. The thymus in this case weighs 90 g. These findings are consistent with true thymic hyperplasia.
Differential diagnosis
- Thymic follicular hyperplasia:
- Usually of normal size and weight; increased number of lymphoid follicles with germinal centers seen on histological analysis
- Thymoma, especially the WHO type B1 thymoma:
- Evidence of invasion, large lobules separated by fibrous bands and only rare Hassall corpuscles
- Thymic rebound hyperplasia:
- Rapidly growing anterior mediastinal mass in a postchemotherapy patient; some but not all cases exceed normal weight limits for age
- Histologically normal
- Lymphoproliferative disorders involving the thymus (e.g., T lymphoblastic lymphoma / leukemia, small B cell lymphomas, T cell lymphomas, classic Hodgkin lymphoma):
- Effaced architecture in lymphoma
- Germ cell tumors (e.g., seminoma):
- Usually morphology is different; however, seminoma can have lymphoid hyperplasia and remnant thymic tissue
Board review style question #1
Board review style answer #1
B. Expansion of the normal component of the thymic gland. Answers A and D are incorrect because effacement of normal thymic architecture and large lobules separated by fibrous bands are features of thymoma. Answer C is incorrect because reactive secondary follicles are features of thymic follicular hyperplasia.
Comment Here
Reference: True thymic hyperplasia
Comment Here
Reference: True thymic hyperplasia
Board review style question #2
Which type of thymoma can resemble the morphologic features of true thymic hyperplasia?
- Type A
- Type AB
- Type B1
- Type B2
- Type B3
Board review style answer #2
C. Type B1. Thymoma type B1 can closely resemble true thymic hyperplasia particularly in small biopsies; however, thymoma type B1 has larger lobules, thicker fibrous capsule and septa and predominance of cortical over medullary areas. There are no or very few Hassall corpuscles in type B1 thymoma in comparison to true thymic hyperplasia. Scattered large neoplastic epithelial cells (keratin+) obscured by a diffuse, small lymphocytic background are present.
Comment Here
Reference: True thymic hyperplasia
Comment Here
Reference: True thymic hyperplasia