Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Positive stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lee E, Handel A, Nachman S, Relich RF, Totten AH. Mpox / orthopoxvirus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologymonkeypox.html. Accessed April 20th, 2024.
Definition / general
- Monkeypox virus (MPXV) is a member of the Orthopoxvirus genus (family Poxviridae and subfamily Chordopoxvirinae), which also includes variola virus (the cause of smallpox), vaccinia virus and others
- Disease formerly known as monkeypox, nomenclature updated November 2022 (Mpox) (WHO: WHO Recommends New Name for Monkeypox Disease [Accessed 13 October 2023])
- Clades of MPXV: clade I (formerly Congo Basin clade) and clade II (formerly West African clade) (WHO: WHO Recommends New Name for Monkeypox Disease [Accessed 13 October 2023])
- Causative agent of Mpox disease
Essential features
- Traditionally thought to be endemic to West and Central Africa but global spread is increasing due to human to human transmission and zoonotic spillover events
- Mpox disease is akin to smallpox (deep seated, well defined, bordered umbilicated lesions), with much lower mortality rates dependent upon viral clade
- Unlike smallpox, Mpox lesions do not all appear at the same time
- Spread through intimate skin to skin contact (including sexual contact) with an infectious lesion or contaminated fomites (e.g., shared linens)
- Viral genomics suggest that the 2022 outbreak clade may differ significantly from prior zoonotic events (Proc Natl Acad Sci U S A 2023;120:e2220415120)
- Immunity is typically achieved with immunization with vaccinia virus based vaccines (JYNNEOS and ACAM2000); decreased vaccinations following the eradication of smallpox may be a partial driver in increased global susceptibility to pox viral disease
- Reference: WHO: Mpox (Monkeypox) [Accessed 13 October 2023]
Epidemiology
- Primarily zoonotic in nature but has shown increased human to human transmission with the 2022 pandemic
- Reservoirs include African rodents (thought to be natural reservoirs), monkeys, squirrels, rats, mice, monkeys, prairie dogs and humans
- Risk factors: living in rural and heavily forested areas of Central and Western Africa, handling of bushmeat, caregiving to infected individuals, exotic animal trade
- Contact with infected bodily fluids, skin lesions or respiratory droplets of infected animals / humans / contaminated fomites are main means of transmission
- Previously demonstrated limited human to human transmission but decreasing herd immunity to orthopoxviruses may reflect an increasing threat of disease spread
- Pandemic in 2022 was predominantly attributed to close contact human to human transmission during intimate contact and large gatherings
- Clades I and II have been linked to close human to human (intimate) contact (Emerg Infect Dis 2024;30:172)
- Reference: MMWR Morb Mortal Wkly Rep 2022;71:1449
Sites
- Skin to skin contact with infected sites (may precede vesiculopustular rash)
- Oropharyngeal exposure with infectious lesions or bodily fluids; respiratory droplet spread of infected animals / humans (less efficient than cutaneous exposure)
- Local or systemic lymphadenopathy / lymphadenitis may be present
- Reference: CDC: How It Spreads [Accessed 13 October 2023]
Pathophysiology
- Virus enters via oropharynx, nasopharynx or intradermal route
- MPXV replicates at the site of inoculation then spreads to local lymph nodes
- Initial viremia causes systemic spread and seeding of other organs
- Reference: StatPearls: Mpox (Monkeypox) [Accessed 13 October 2023]
Clinical features
- Incubation period is typically 3 - 17 days (up to 21 days)
- Symptoms usually present within 3 weeks of exposure and illness typically lasts 2 - 4 weeks
- Flu-like symptoms (fever, headache) and lymphadenopathy / lymphadenitis may develop, usually with characteristic rash appearing 1 - 4 days later
- Atypical presentation during the 2022 pandemic
- Absence of regional lymphadenopathy noted in this outbreak compared with historic outbreaks (CDC: Monkeypox Outbreak [Accessed 21 November 2023])
- Anogenital or oropharyngeal / perioral lesions are predominant symptoms, with rashes involving the limbs, face and trunk to a lesser extent
- Limited anatomic rash spread is noted compared to earlier outbreaks; in some individuals, rash appears prior to fever which is atypical of prior presentations
- Severely painful lesions that can coalesce and cause increased risk of localized secondary bacterial infection in vulnerable anatomic sites, including the genitals and oropharynx
- Early rash may present similarly to other viral processes such as herpes simplex virus (HSV) or varicella zoster virus (VZV)
- May also appear similar to acne vulgaris during early courses
- Data suggests infectiousness is highest when symptomatic at illness onset but asymptomatic shedding has been proposed (not fully elucidated if common)
- DNA studies suggest that viruses are detectable for > 35 days but infectiousness beyond the symptomatic period is unclear
- Reference: CDC: How It Spreads [Accessed 13 October 2023]
Diagnosis
- PCR testing is the mainstay of clinical diagnostics (Orthopoxvirus or MPXV specific assays)
- Currently there are no FDA approved assays, although research use only (RUO) assays are available
- Viral DNA is detectable in a wide variety of sample types and the virus has been isolated from skin, oropharyngeal, anal, urethral, conjunctival swabs and semen (Travel Med Infect Dis 2022:50:102459)
- Viral culture is possible but not clinically suggested due to safety concerns and select agent regulations around clade I of MPXV (CDC: Biosafety in Microbiological and Biomedical Laboratories (BMBL) [Accessed 13 October 2023])
- Electron microscopic negative stain for poxvirus scabrous material, IHC for viral antigens or serologic diagnosis are uncommon but have been used for clinical diagnostics
- RUO assays include lateral flow assays, point of care antigen capture enzyme linked immunosorbent assays (ELISA) and other nucleic acid amplification test (NAAT) based technologies, with the majority of assays detecting orthopoxviral specific sequences
Laboratory
- Retrospective analysis of laboratory findings in patients with Mpox virus infections showed elevated transaminases, leukocytosis, low blood urea nitrogen (BUN) levels, decreased blood albumin levels and rarely thrombocytopenia (Clin Infect Dis 2005;41:1742)
- Presence of a large number of oropharyngeal lesions was correlated with increased risk of abnormal laboratory values (Clin Infect Dis 2005;41:1742)
Prognostic factors
- Prognosis regarding mortality / outcome is associated with specific viral clade in endemic areas / outbreaks; clade I mortality rate (11%) is significantly higher than clade II (< 1%)
- Data suggest that access to comprehensive medical care is one of the main prognostic factors
- Supportive care measures, pain management and adequate medical access may impact outcomes and explain the discrepancy in death rates between areas of endemicity and outbreaks
- Surviving patients can fully recover with some potential for scarring and skin discoloration
- It is currently unknown whether mortality in the 2022 outbreak is associated with any specific factors; immunocompromised individuals (especially those with HIV / AIDS) are at risk of severe Mpox infection (MMWR Morb Mortal Wkly Rep 2023;72:404)
- Mpox can cause severe pain at affected anatomic sites, including eyes, genitals and oropharynx, potentially in association with complications such as bacterial superinfection, scarring, hyper / hypopigmentation, corneal scarring, pneumonia, dehydration, sepsis, encephalitis and death
- Data regarding infection in pregnancy are limited and severity is unknown
- Maternal to fetal transmission may be possible with prolonged skin to skin contact or an exchange of fluids
- Neonatal infections following intrapartum exposure to an acutely infected mother have been described
- Unknown if the virus is present in breast milk but breastfeeding is contraindicated until eligible to discontinue isolation
- Reference: CDC: Clinical Guidance - Mpox [Accessed 13 October 2023]
Case reports
- 4 and 7 year old girls and 30 year old man with familial Mpox virus infection (Emerg Infect Dis 2023;29:437)
- 9 year old boy with first recognized case of human Mpox (Bull World Health Organ 1972;46:593)
- 18 year old woman with Mpox virus infection after sexual intercourse (Emerg Infect Dis 2023;29:219)
- 33 year old man with HIV infection and fatal case of Mpox virus (N Engl J Med 2023;388:1246)
- 38 year old man with rectal pain, fever and vesiculopustular rash (Vaccines (Basel) 2022;10:1903)
Treatment
- Vaccination is suggested as either preexposure prophylaxis (PrEP) or postexposure prophylaxis (PEP)
- JYNNEOS vaccine currently under emergency use authorization
- Majority of infected immunocompetent patients will recover
- Supportive care is suggested; pain management is suggested if indicated
- For immunocompromised or patients with severe infection (i.e., severe disease, risk of infection based on anatomic site of lesions / lesional coalescence, pregnancy, etc.), treatment may be indicated: tecovirimat (oral or IV), brincidofovir (no data in humans), vaccinia immune globulin intravenous (VIGIV, investigational new drug through the CDC), cidofovir (no data in humans)
- In the U.S., treatment of patients should be managed in collaboration with the CDC to determine optimal means of treatment and access to approved or investigational drugs
- Investigational trials for drugs such as tecovirimat (STOMP trial) are accessible through the CDC and partner organizations for populations such as children and pregnant individuals
- References: CDC: Clinical Guidance - Mpox [Accessed 13 October 2023], CDC: Treatment Information for Healthcare Professionals [Accessed 13 October 2023], Clin Infect Dis 2020;71:e210, J Infect Dis 2017;216:824
Gross description
- Cutaneous presentations
- Papules, vesicles, pustules or scabs that are deep seated and well defined with round borders
- Lesions may be umbilicated, painful, painless or itchy
- Reference: J Am Acad Dermatol 2023;88:856
Microscopic (histologic) description
- Vesicular stage
- Characterized by spongiosis and mild acanthosis in the uninvolved epidermis near the edge of the bulla, with exocytotic lymphocytes, neutrophils and neutrophilic debris
- There is a band of mixed acute and chronic inflammation in the dermal epidermal junction that extends into the base of the bulla; the edge of the vesicle displays papillary dermal edema with fewer inflammatory cells
- Occasionally, multinucleated and ballooning keratinocytes can be seen with intact nuclear features and no obvious viral changes; diffuse cytoplasmic staining of antivaccinia IHC of ballooning keratinocytes is also seen
- Pustular stage
- Keratinocytes in the acanthotic epidermis of the bulla are mostly nonviable, cytoskeletal remnants result in a shadow of epidermal scaffolding
- Keratinocytes may show viral cytopathic effects of eosinophilic ground glass appearance within the central area of the nucleus, with the nuclear contents pushed to the periphery giving a basophilic halo
- Occasional multinucleated keratinocytes are seen, each with ~3 - 8 nuclei
- Homogenous, eosinophilic B type inclusions (Guarnieri bodies) are present in the cytoplasm of affected keratinocytes within a ghosted epidermal cytoskeleton scaffolding
- There are few viable keratinocytes and a myriad of inflammatory cells (lymphocytes, eosinophils, neutrophils); the edge of the vesicle shows more viable keratinocytes, whereas the center will exhibit more multinucleated keratinocytes
- Reference: J Cutan Pathol 2005;32:28
Positive stains
- IHC: antivaccinia virus antibody staining has been described (cytoplasmic staining) (J Am Acad Dermatol 2023;88:856)
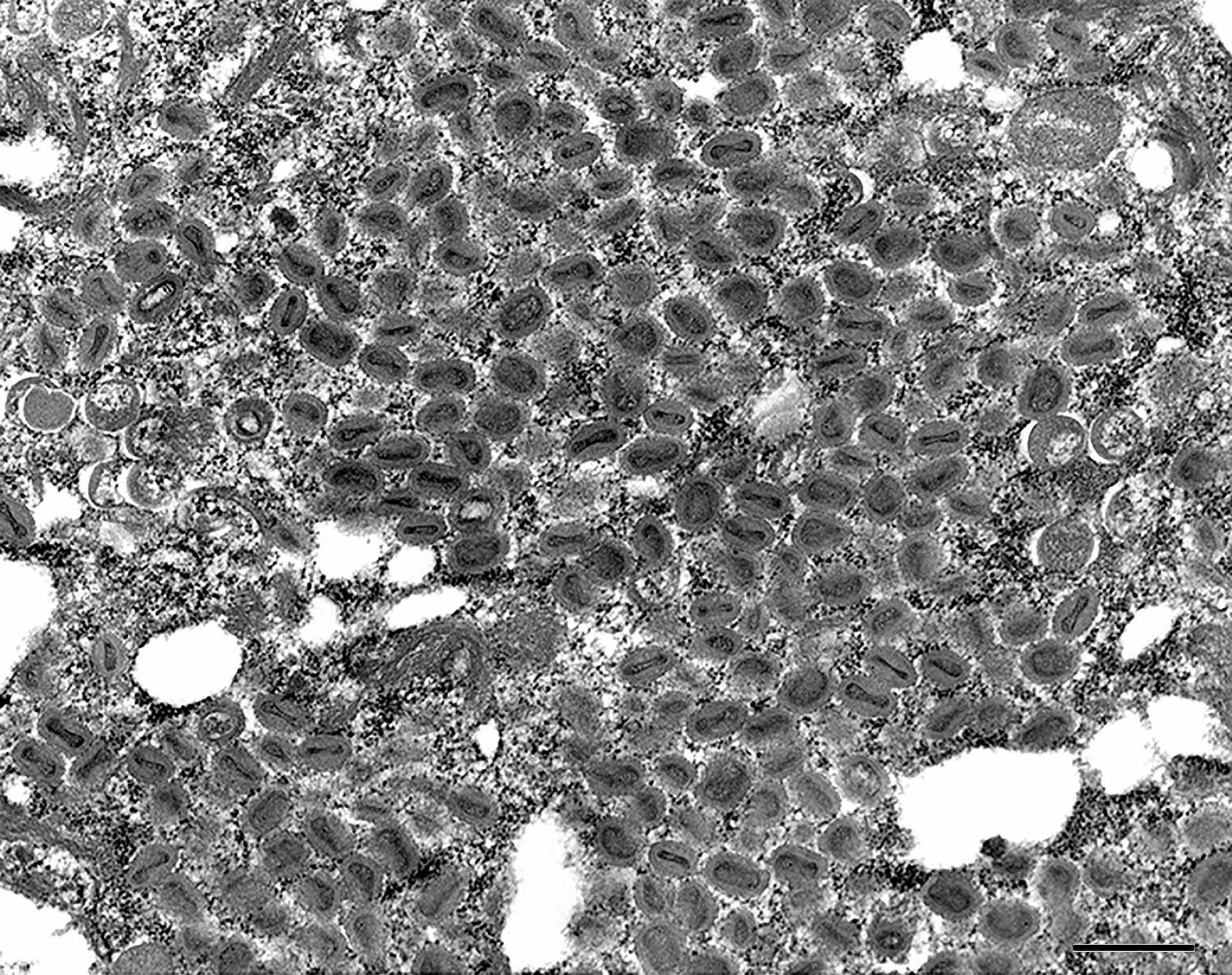
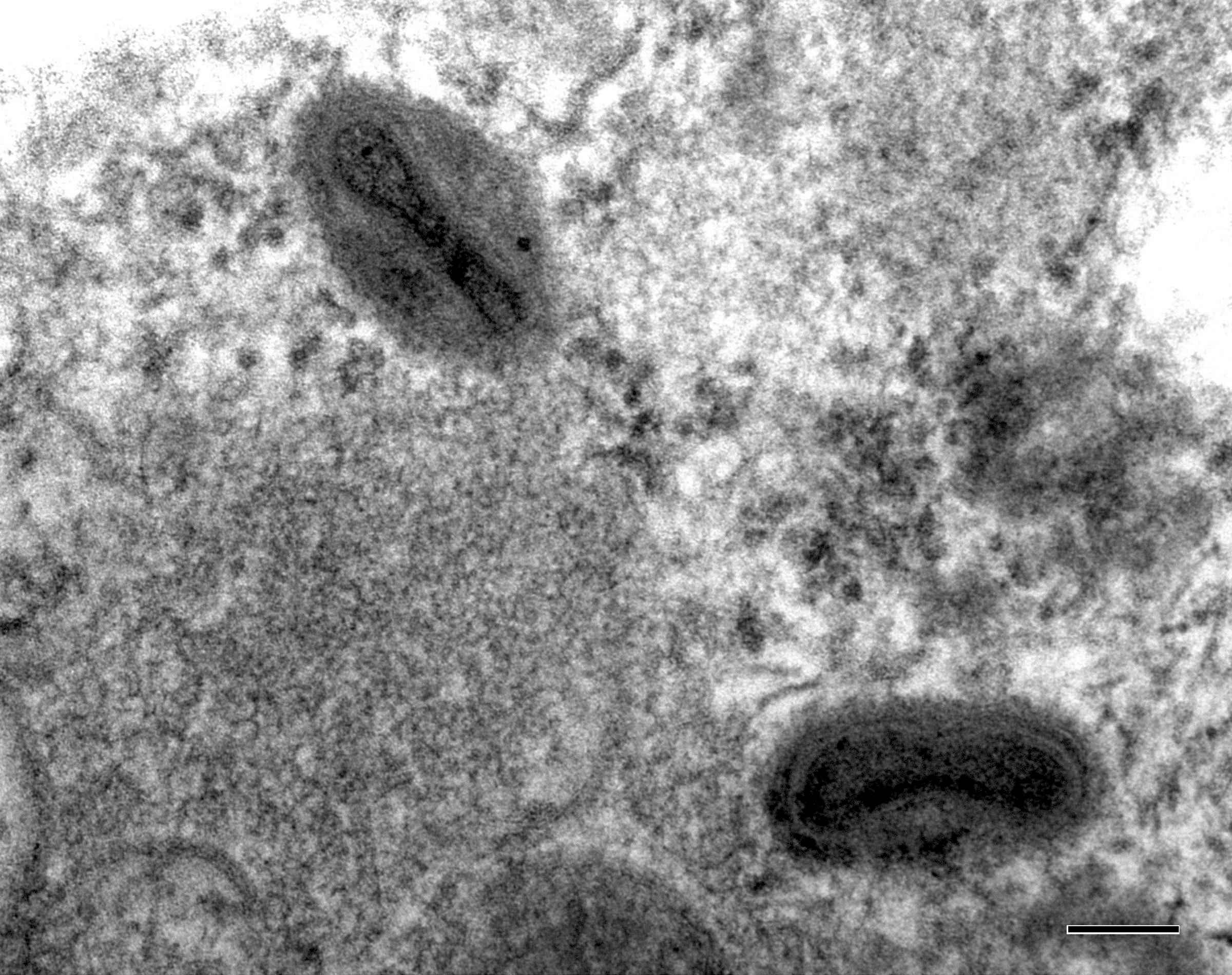
Electron microscopy description
- Relatively large (~240 - 300 nanometers)
- Pox viruses are typically brick shaped, enveloped viruses with a linear double stranded DNA genome (Baron: Medical Microbiology, 4th Edition, 1996)
Electron microscopy images
Molecular / cytogenetics description
- Poxviruses include all necessary replication, transcription, assembly and egress proteins in their genome, except for their reliance of host ribosomes for mRNA translation (Viruses 2020;12:1257)
Differential diagnosis
- Chickenpox (VZV) / herpes zoster:
- Pustules may be present in different stages; MPXV is less likely to cause pus filled lesions
- Rash associated with several dermatomes, normally presents with immunocompromise
- Smallpox (variola virus) / progressive vaccinia:
- Vesicles are normally more numerous and illness is more severe; lymphadenopathy is absent
- Limited illness based on vaccine exposure, lesions are normally located near inoculation site
- Herpes simplex (HSV) / disseminated HSV:
- Rash is normally not deep seated or generalized
- Insect bites:
- Lack of systemic disease, limited nonvesiculating lesions with insect exposure
- Acne:
- Comedones, inflammatory lesions and scars
- Comedones (open or closed) are cyst-like cavities filled with a mass of keratinous material and bacteria (C. acnes)
- Chancroid (Haemophilus ducreyi):
- Genital ulcers, tend to be soft without induration
- Buboes may be present at later stages with other urogenital symptomatology (discharge, dysuria)
- Disseminated Neisseria gonorrhoeae infection:
- Lesions tend to be present on extremities in many presentation types (bullae, petechiae)
- Joint pain or polyarthritis is present
- Urogenital symptoms can be absent
- Lymphogranuloma venereum (LGV):
- Painful inguinal or femoral lymphadenopathy
- Tertiary stages have presence of elephantiasis, draining sinus tracts or fistulae
- Hand, foot and mouth disease:
- Self limited, normally found in children
- Vesicles are generally limited to oropharynx and hands / feet
- Drug reaction / drug associated eruption:
- Eosinophils with marked vascular wall thickening
- May also cause granulomatous infiltrate
- Also vacuolar interface changes and lymphocytic exocytosis with eosinophilic parakeratosis and plasma cells in the dermis
- Eczema vaccinatum:
- Complication following smallpox vaccination, vaccinia outside inoculation site
- Clinical and vaccination history inform disease
- Eczema herpeticum:
- Monomorphic blisters may be filled with clear / yellow fluid, which may be purulent
- May have central umbliciations but older lesions will crust and can form sores
- Erythema multiforme:
- Severe dermal inflammatory infiltrates with many eosinophils, lymphocytes and histiocytes that form subepidermal bullae in the basement membrane due to dermal edema
- Overlying epidermis may show liquefactive necrosis along with dyskeratotic keratinocytes
- May also form dermoepidermal bullae at the layer of the basal lamina
- No microabscesses
- Meningococcal septicemia:
- Tends to be associated with purpuric lesions rather than pustules
- Measles:
- Koplik spots, rash tends to not vesiculate
- Tanapox:
- Lesions tend to be limited and nonvesiculating
- Geographically located in Kenya / Democratic Republic of Congo region
- Oral aphthous ulcers:
- Mucosal ulceration with varied infiltrative inflammatory cells and large granular lymphocytes
- Ulcer forms well below the surface and inflammation extends deep; the surface of these lesions is usually covered with a thin fibrinous exudate that is enriched with polymorphs
- Molluscum contagiosum:
- Normally limited to pediatric patients, young adults and immunocompromised patients
- May show central umbilication with limited vesiculation
- Lack of systemic disease
- Scabies:
- Presence of organismal burrows is common, lacks systemic disease and can cause crusted lesions
- Rickettsialpox:
- Presence of eschar, may be macular or papular (rarely vesicular)
- Syphilis (Treponema pallidum):
- Primary chancre is painless, secondary rash does not vesiculate and can be present on palms / soles
- References: Best Practice: Mpox (Monkeypox) [Accessed 13 October 2023], StatPearls: Mpox (Monkeypox) [Accessed 13 October 2023]
Board review style question #1
A 24 year old man presents to a sexual health clinic with raised, umbilical lesions adjacent to and on the penile shaft. Patient describes dysuria and intense pain but the vesiculopustular rash is not present elsewhere on the physical exam. He also mentions recent travel to a popular music festival with close skin to skin contact within the last week. Based on the symptoms, what clinical testing schema is most appropriate?
- Electron microscopy of scabrous material
- IHC of lesion for viral antigens
- PCR / NAAT for orthopoxvirus / MPXV
- Viral culture from the lesions
Board review style answer #1
C. PCR / NAAT for orthopoxvirus / MPXV is the most appropriate clinical testing regimen based on this presentation and history. Answers A and B are incorrect because while electron microscopy of patient material and IHC of lesions for viral antigens may be useful, these are cumbersome techniques with increased risk of nosocomial exposure and prolonged turnaround time. Answer D is incorrect because viral culture from lesions is typically not indicated as certain clades of MPXV are select agents and cell culture may take > 2 days for diagnosis.
Comment Here
Reference: Mpox / orthopoxvirus
Comment Here
Reference: Mpox / orthopoxvirus
Board review style question #2
What clinical symptom was common in prior outbreaks of Mpox but was greatly reduced in prevalence during the 2022 Mpox pandemic?
- Fever
- Lymphadenopathy
- Pain
- Umbilicated, vesiculopapular rash
Board review style answer #2
B. Lymphadenopathy. While prior outbreaks of MPXV have had all 4 of the listed symptoms above, the 2022 outbreak was distinct in the relative lack of lymphadenopathy. Answers A, C and D are incorrect because symptoms such as fever, umbilicated, vesiculopapular rash and pain at the site of infection are common.
Comment Here
Reference: Mpox / orthopoxvirus
Comment Here
Reference: Mpox / orthopoxvirus