Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Uses by pathologists | Prognostic factors | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Practice question #1 | Practice answer #1Cite this page: Parilla M. PML::RARA. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/molecularpmlrara.html. Accessed September 21st, 2025.
Definition / general
- Fusion of 2 genes:
- PML, which encodes promyelocytic leukemia protein
- RARA, which encodes retinoic acid receptor alpha
- PML is found on the long arm of chromosome 15 (15q24) and RARA is found on the long arm of chromosome 17 (17q21)
- PML::RARA fusions typically result from a translocation of chromosome 15 with chromosome 17, t(15;17)
- PML::RARA is found in acute promyelocytic leukemia (APL), a subtype of acute myeloid leukemia (AML) with recurrent genetic abnormalities
Essential features
- PML::RARA is found in 98% of acute promyelocytic leukemia (APL) cases and has not been described in other neoplasms (Blood 1994;83:10, Expert Rev Hematol 2014;7:347)
- Fusion protein resulting from PML::RARA arrests myeloid maturation to the promyelocyte stage and drives APL (Blood 1994;83:10)
- Tretinoin combined with arsenic trioxide treatment releases the fusion gene induced maturation arrest and typically result in a durable remission (Blood 1994;83:10)
Terminology
- PML-RARA (hyphen) and PML/RARA (forward slash) nomenclature has been retired in favor of PML::RARA (double colon) (Leukemia 2021;35:3040)
- PML-RAR alpha
- Promyelocytic leukemia protein (PML)
- Retinoic acid receptor alpha (RARA)
- t(15;17)
Pathophysiology
- PML::RARA fusions are most commonly the result of a balanced translocation between chromosome 15 and chromosome 17, although the fusion may be the result of more complex or cryptic rearrangements between the 2 genes (Cancers (Basel) 2020;12:624)
- The breakpoint within the RARA gene is almost always within intron 2 while the breakpoint within the PML gene is almost always in 1 of 3 locations: intron 6 (Bcr1), exon 6 (Bcr2) or intron 3 (Bcr3) (Cancers (Basel) 2020;12:624)
- Transcription and translation of the PML::RARA fusion gene results in a PML::RARA protein isoform that can be either long (Bcr1 or Bcr2 of PML) or short (Bcr3 of PML) (Cancers (Basel) 2020;12:624)
- PML::RARA oncoprotein arrests myeloid maturation (Cancer Cell 2017;32:552)
- All trans retinoic acid (ATRA, e.g., tretinoin) binds to the RARA component while arsenic trioxide (ATO) binds to the PML component of the fusion protein, resulting in maturation and cell death (Jaffe: Hematopathology, 2nd Edition, 2017)
- PML::RARA fusion can be detected via fluorescence in situ hybridization (FISH), classical karyotype or molecular methods such as reverse transcription polymerase chain reaction (RT-PCR) of the fusion mRNA
- PML::RARA will be detected during treatment and typically for weeks after treatment; detection of the fusion gene or fusion transcript during or shortly after treatment does not predict treatment failure (Jaffe: Hematopathology, 2nd Edition, 2017)
- After some time in complete remission the PML::RARA transcript should become undetectable; later detection of the transcript, after complete molecular remission, is strongly associated with relapse (Jaffe: Hematopathology, 2nd Edition, 2017)
Diagrams / tables
Clinical features
- PML::RARA fusion is diagnostic of APL (Jaffe: Hematopathology, 2nd Edition, 2017)
- Long PML::RARA fusion genes are typically associated with the classic morphology of APL (Leukemia 2006;20:103)
- Short PML::RARA fusion gene is commonly associated with the hypogranular variant of APL, as well as FLT3 alterations (Leukemia 2006;20:103)
Uses by pathologists
- Detection of PML::RARA via molecular methods such as RT-PCR or via cytogenetic techniques (e.g., FISH and karyotype) is diagnostic of APL (Jaffe: Hematopathology, 2nd Edition, 2017)
- Although rapid FISH or RT-PCR should be ordered in suspected cases of APL, presumptive treatment should not be delayed while awaiting confirmatory test result (Jaffe: Hematopathology, 2nd Edition, 2017)
Prognostic factors
- PML::RARA fusion is diagnostic of APL, a life threatening form of AML that can lead to disseminated intravascular coagulation (DIC) and rapid death (often due to intracranial hemorrhage) without prompt treatment (Jaffe: Hematopathology, 2nd Edition, 2017)
- With prompt treatment using ATRA (an active metabolite of vitamin A), usually in combination with ATO, approximately 95% of all APL patients reach complete molecular remission and are considered cured from disease (Cancer Cell 2017;32:552)
- Considered a favorable prognostic marker for AML due to its high response rate to treatment
Molecular / cytogenetics description
- Majority of APL cases are driven by PML::RARA via t(15;17) (q24;q21), a balanced translocation that can be seen by karyotype (Cancers (Basel) 2020;12:624)
- Remaining APLs driven by PML::RARA occur via cryptic or complex rearrangements that are often identified via FISH (Blood 1994;83:10)
- Molecular testing (RNA based) with RT-PCR or next generation sequencing can identify some rare additional cryptic PML::RARA cases, missed by cytogenetic techniques (karyotype and FISH) (Cancer Biol Ther 2020;21:309)
- 2% of non-PML::RARA driven APL cases have alternative fusions such as PML::PLZF, often from t(11;17); these cases are not typically responsive to treatment with ATRA and have less favorable prognosis (Blood 1999;93:3167)
Molecular / cytogenetics images
Sample pathology report
- Bone marrow, qualitative PML::RARA RT-PCR assay:
- PML::RARA fusion transcript is detected (see comment)
- Comment: Test and methodology: quantitative PML::RARA RT-PCR - this reverse transcription PCR based assay is designed to detect PML::RARA fusion transcripts. Diagnostic sensitivity: this assay is negative in < 1% of APL cases. Technical sensitivity: a clonal cell population at 0.001% may not be detected by this assay based on the RNA quality of the sample. Disclaimer: this result cannot be used as sole evidence for or against cancer and has to be interpreted in the context of all available clinical and pathological information. This test was developed and its performance characteristics determined, by the Laboratory of Diagnostic Molecular Pathology. It has not been cleared or approved by the U.S. Food and Drug Administration (FDA). The FDA has determined that such clearance is not necessary. This test is used for clinical purposes. Pursuant to the requirements of CLIA '88, our laboratory has established the accuracy and precision of this test. Laboratory notes: RNA quality: average / run number: 0000001.
Practice question #1
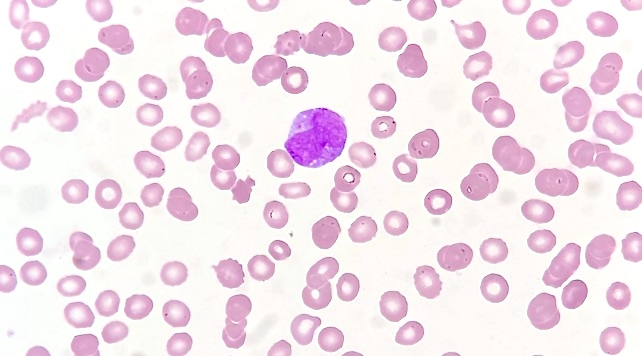
A 31 year old woman presents to an urgent care with new onset epistaxis and a petechial rash. A CBC found WBC to be 21.3 x 109/L, platelets to be 13 x 109/L and hemoglobin to be 5.8g/dL. Her PT / INR and PTT are elevated. Abnormal circulating cells are found in the peripheral blood smear shown above. Flow cytometry and special staining reveal a population of cells that are positive for MPO and CD33 with dim to negative CD34 expression. In addition to starting presumptive treatment, which of the following tests should be ordered first?
- FISH to look for PML::RARA
- Karyotype to look for inv(16)
- Karyotype to look for t(11;17)
- SNP array to look for t(15;17)
- Whole genome next generation sequencing
Practice answer #1
A. FISH to look for PML::RARA. The cell pictured here is markedly abnormal with more than 1 Auer rod in the cytoplasm, consistent with APL. Auer rods are linear structures and are not to be confused with the round and dark abnormal granules seen in eosinophilic precursors in inv(16) AML (answer choice B). APL is a clinical emergency and treatment should begin as soon as possible. Rapid FISH or RT-PCR for PML::RARA will return positive results fastest, helping to confirm a suspected diagnosis of APL, although treatment should not be delayed while awaiting confirmation. Most cases of APL are driven by PML::RARA, typically the result of t(15;17). t(11;17) (answer choice C) is a much less common cause of APL. SNP array (answer choice D) is not a method for identifying balanced gene fusions. Whole genome sequencing would likely be able to identify PML::RARA but has a much slower turnaround time than FISH or PCR and is more expensive (answer choice E).
Comment Here
Reference: PML::RARA
Comment Here
Reference: PML::RARA