Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Classification | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Cai C. Immune mediated necrotizing myopathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/muscleimmunemediated.html. Accessed April 25th, 2024.
Definition / general
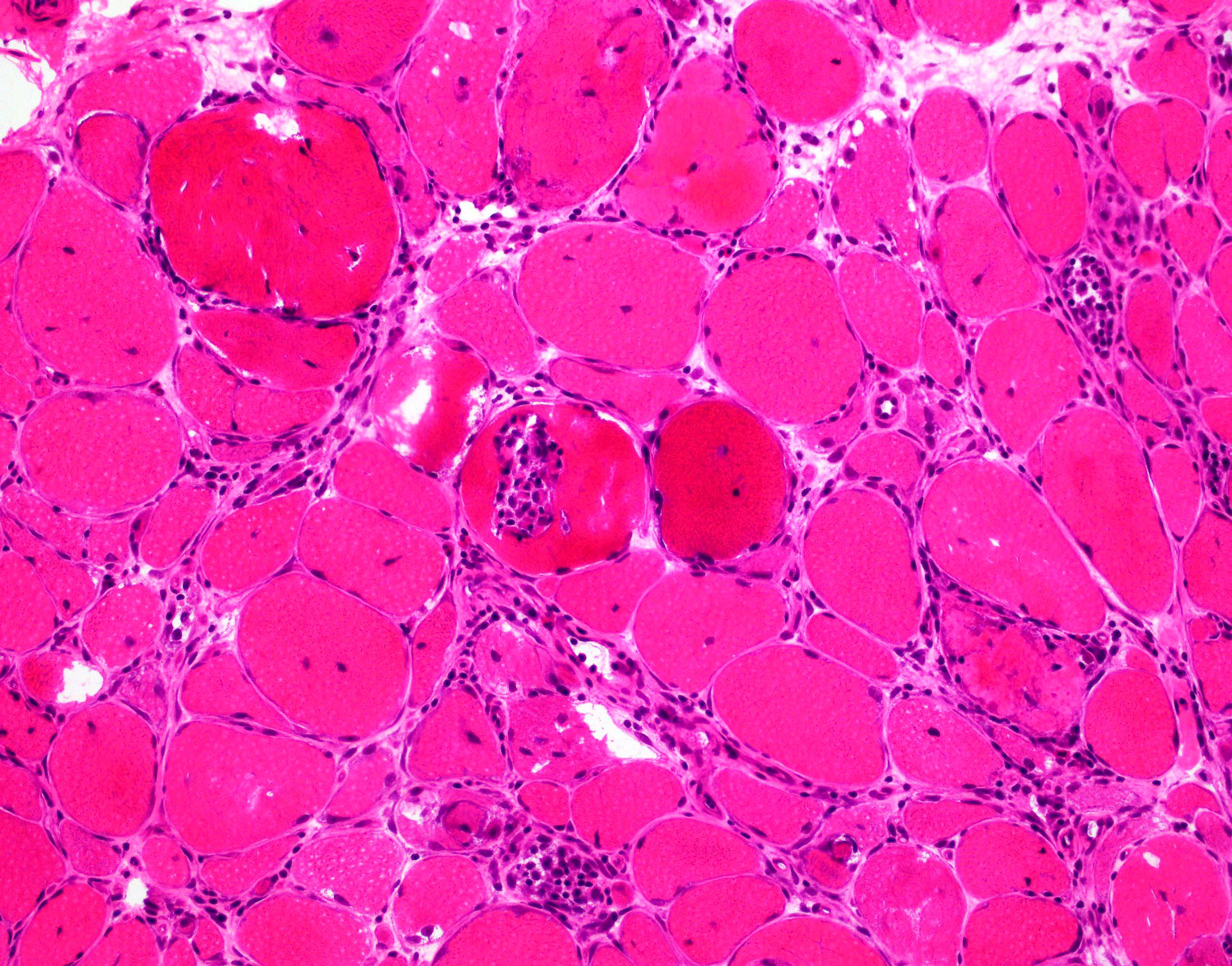
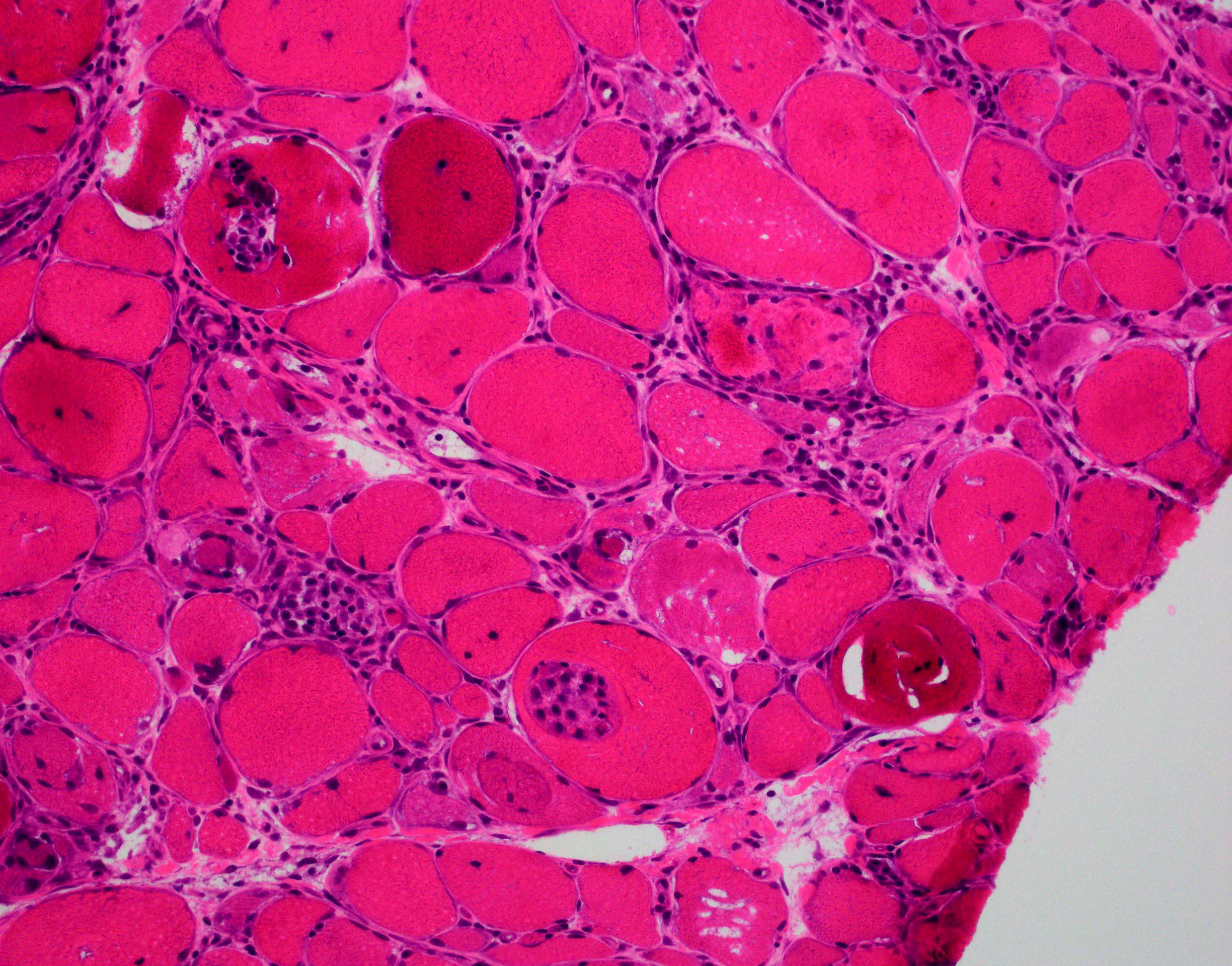
- Pathological definition of immune mediated necrotizing myopathy (IMNM) requires prominent myofiber necrosis, the absence of significant inflammatory infiltrates, negative major histocompatibility complex (MHC) class I expression and variable complement deposition on capillaries (Neuromuscul Disord 2018;28:87)
Essential features
- Histological hallmark of IMNM is pauci-inflammatory necrotizing myopathy
- Necrotic fibers are randomly distributed and at different temporal stages
Terminology
- Necrotizing autoimmune myopathy (NAM)
- HMGCR: 3-Hydroxy-3-Methylglutaryl-CoA Reductase
ICD coding
- ICD-10: G72.4 - inflammatory and immune myopathies, not elsewhere classified
Epidemiology
- Prevalence of IMNM is approximately 1 per 100,000 people; accounts for ~10% of autoimmune myopathies
- More common in women
- Mean age of anti-SRP and statin exposed anti-HMGCR is 40 years
- Mean age of nonstatin exposed anti-HMGCR is 55 years
- Reference: Curr Rheumatol Rep 2018;20:21
Sites
- Major target organ of anti-SRP and anti-HMGCR are muscles, leading to myofiber necrosis and weakness (J Neurol Neurosurg Psychiatry 2016;87:1038)
Etiology
- Statin exposure is highly associated with anti-HMGCR myopathy (Arthritis Rheum 2010;62:2757)
- In Asians, majority of anti-HMGCR myopathy is not associated with statin exposure (Medicine (Baltimore) 2015;94:e416)
- In adults, anti-HMGCR myopathy is strongly associated with the human leukocyte antigen (HLA) class DRB1*11:01 (Arthritis Care Res (Hoboken) 2012;64:1233)
- In children, anti-HMGCR myopathy is associated with HLA class DRB1*07:01 (Arthritis Care Res (Hoboken) 2017;69:1088)
Clinical features
- Hallmark clinical features of immune mediated necrotizing myopathy patients are proximal muscle weakness and elevated creatine kinase
- Severe limb muscle weakness, neck weakness, dysphagia, respiratory insufficiency and muscle atrophy are more frequent in patients with anti-SRP antibodies than in those with anti-HMGCR antibodies
- In anti-SRP positive patients, extramuscular organ involvement includes the heart, joints and lungs, with interstitial lung disease more common than in anti-HMGCR positive patients
- Reference: J Neurol Neurosurg Psychiatry 2016;87:1038
Classification
- IMNM is further classified by serum autoantibodies into anti-SRP, anti-HMGCR and seronegative groups (Neuromuscul Disord 2018;28:87)
- SRP group:
- Titer of anti-SRP antibody directly correlates with myofiber necrosis and serum creatine kinase levels (Arthritis Rheum 2011;63:1961)
- This group usually has more severe, rapidly progressive muscle weakness, frequent lung involvement, occasional cardiac muscle involvement and poor response to treatment but is not associated with risk of malignancy (Curr Opin Rheumatol 2016;28:619)
- HMGCR group:
- Majority of this group is developed in the setting of statin usage and generally responds very well to immune suppressive treatment (Arthritis Rheum 2010;62:2757)
- Serum creatine kinase level correlated with anti-HMGCR level only in the patients with statin exposure but not in the statin unexposed patients (Arthritis Rheum 2012;64:4087)
- There is a moderate risk of malignancy (Neurol Neuroimmunol Neuroinflamm 2016;3:e290)
- Seronegative group:
- This group has negative serum autoantibodies but a similar muscle pathology to IMNM
- Associated with a high risk of malignancy (Curr Opin Rheumatol 2018;30:655)
Diagnosis
- Anti-SRP and anti-HMGCR autoantibodies are considered specific for IMNM
- Patients with dermatomyositis-like rash but with positive anti-SRP or anti-HMGCR autoantibodies are classified as IMNM with dermatomyositis-like rashes (Neuromuscul Disord 2020;30:70)
- Patients without anti-SRP or anti-HMGCR but with elevated creatine kinase, proximal weakness and muscle biopsy with features of IMNM (outlined below) are diagnosed as seronegative IMNM
- Pathological diagnosis of IMNM requires (Neuromuscul Disord 2018;28:87):
- Presence of necrotic fibers with scattered distribution
- Different stages of necrosis, myophagocytosis and regeneration
- Macrophage predominant, pauci-lymphocytic inflammation
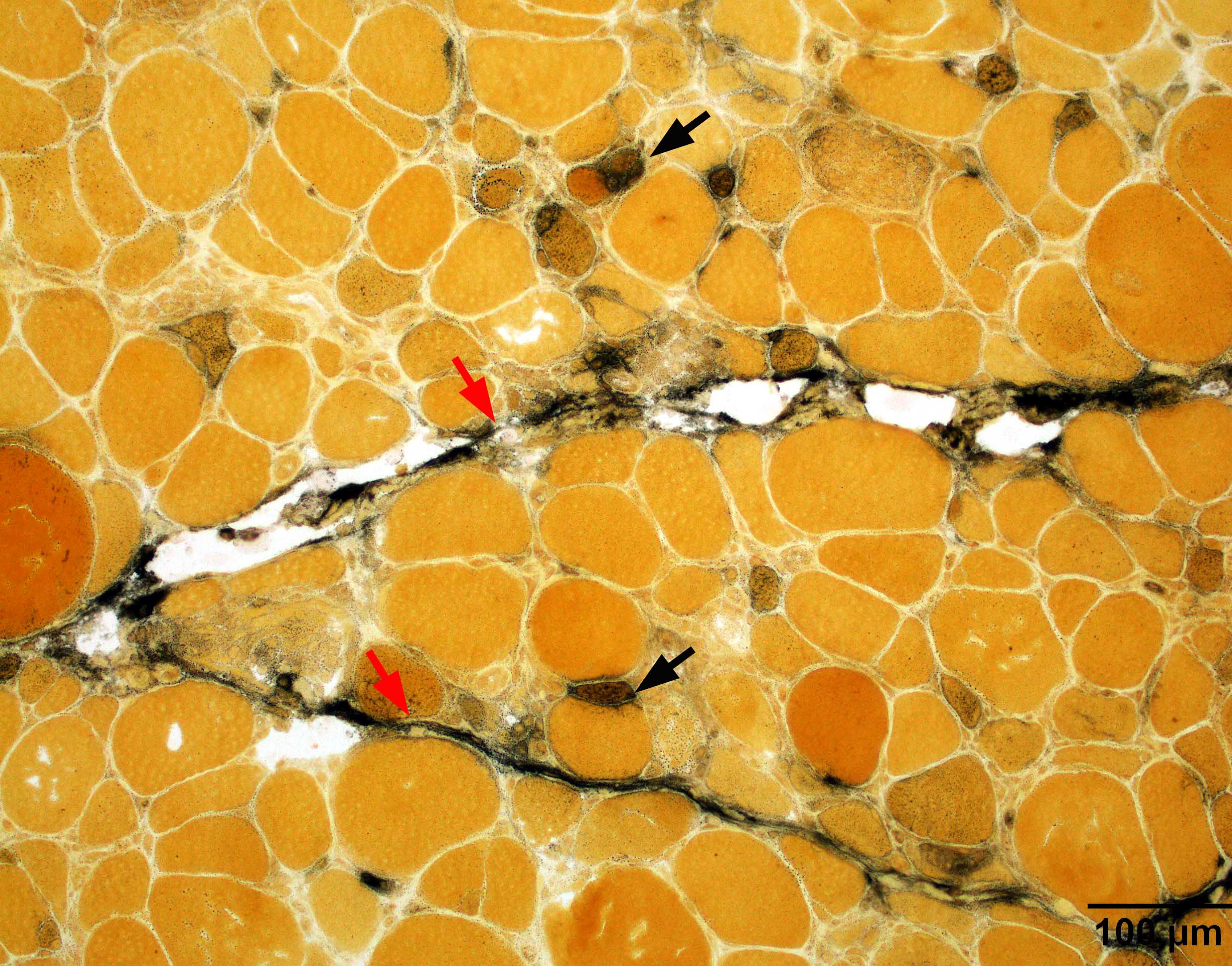
- Following features can be seen in IMNM (presence of these features does not exclude IMNM) (Neuromuscul Disord 2018;28:87):
- Sarcolemmal MHC class I expression in nonnecrotic / nonregenerating myofibers (typically small clusters)
- Patchy sarcolemmal C5b9 (terminal complement complex) deposition
- Endomysial fibrosis
- Enlarged capillaries
Laboratory
- Markedly elevated creatine kinase or persistently elevated creatine kinase after statin cessation
- Positive anti-HMGCR or anti-SRP
- Negative for autoantibodies specific to dermatomyositis (e.g. Mi2, NXP2, TIF1γ, MDA5, p155 / 140, SAE) or antisynthetase syndrome (e.g. Jo1, PL7, PL12)
- Reference: Neuromuscul Disord 2018;28:87
Radiology description
- Hyperintensities on short tau inversion recovery sequence (STIR) reflect active muscle edema associated with inflammation or myofiber necrosis
- T1 MRI can be used to assess fat replacement
- MRI does not distinguish IMNM from other types of myositis; however, it can be used to guide / target muscle biopsy and monitor the evolution of muscle disease
- Reference: Ann Rheum Dis 2017;76:681
Prognostic factors
- Prognosis of IMNM is in general worse than other types of myositis (Curr Rheumatol Rep 2018;20:21)
- Anti-SRP myopathy has more severe, rapidly progressive muscle weakness and poor response to treatment (Curr Opin Rheumatol 2016;28:619)
- Statin induced anti-HMGCR myopathy generally responds well to immune suppressive therapy (Arthritis Rheum 2010;62:2757)
Case reports
- 40 year old woman with anti-SRP antibody interstitial lung disease requiring double lung transplant (Cureus 2020;12:e7962)
- 63 year old woman with previous statin exposure presented with muscle weakness and raised creatinine kinase (BMC Rheumatol 2020;4:29)
- 87 year old woman with heart failure symptoms as the first clinical presentation (BMC Neurol 2020;20:29)
Treatment
- Initial treatment includes intravenous or oral steroids, along with the addition of another agent (e.g. methotrexate, rituximab, intravenous immunoglobulin) at the same time or within 1 month, depending on severity and treatment response
- Intravenous immunoglobulin (IVIG) should always be added within 6 months if other strategies are not effective; IVIG monotherapy can be considered in patients with steroid contraindications
- In patients requiring intensive care as well as in refractory patients, plasma exchange, cyclophosphamide or cyclosporine may be considered
- Reference: Neuromuscul Disord 2018;28:87
Microscopic (histologic) description
- See Diagnosis section
Microscopic (histologic) images
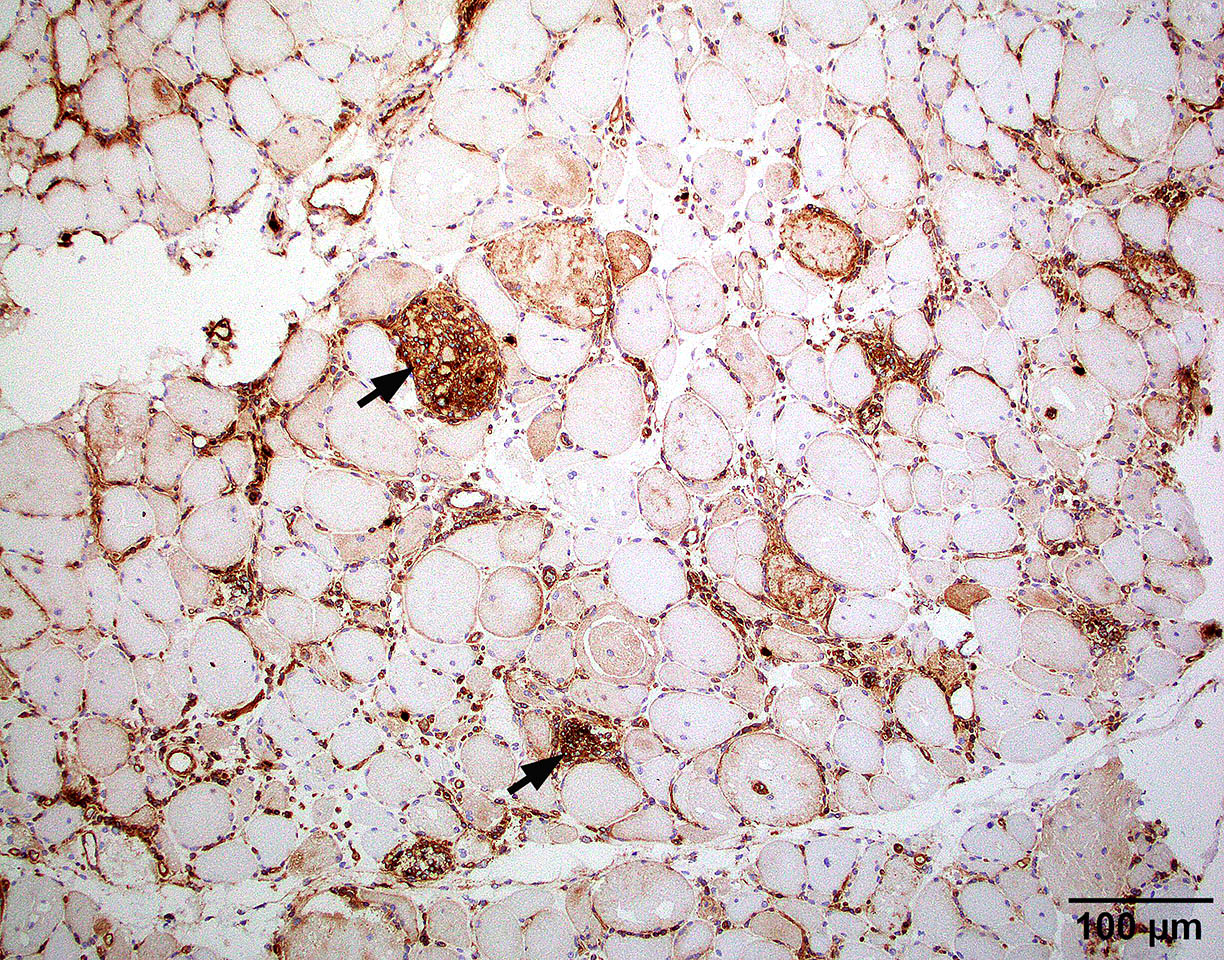
Positive stains
- Strong sarcoplasmic C5b9 expression is seen in acutely necrotic fibers of any causes (usually abundant but not limited to IMNM)
- Sarcolemmal C5b9 expression in a subset of viable myofibers can be seen in IMNM (Neuromuscul Disord 2018;28:87)
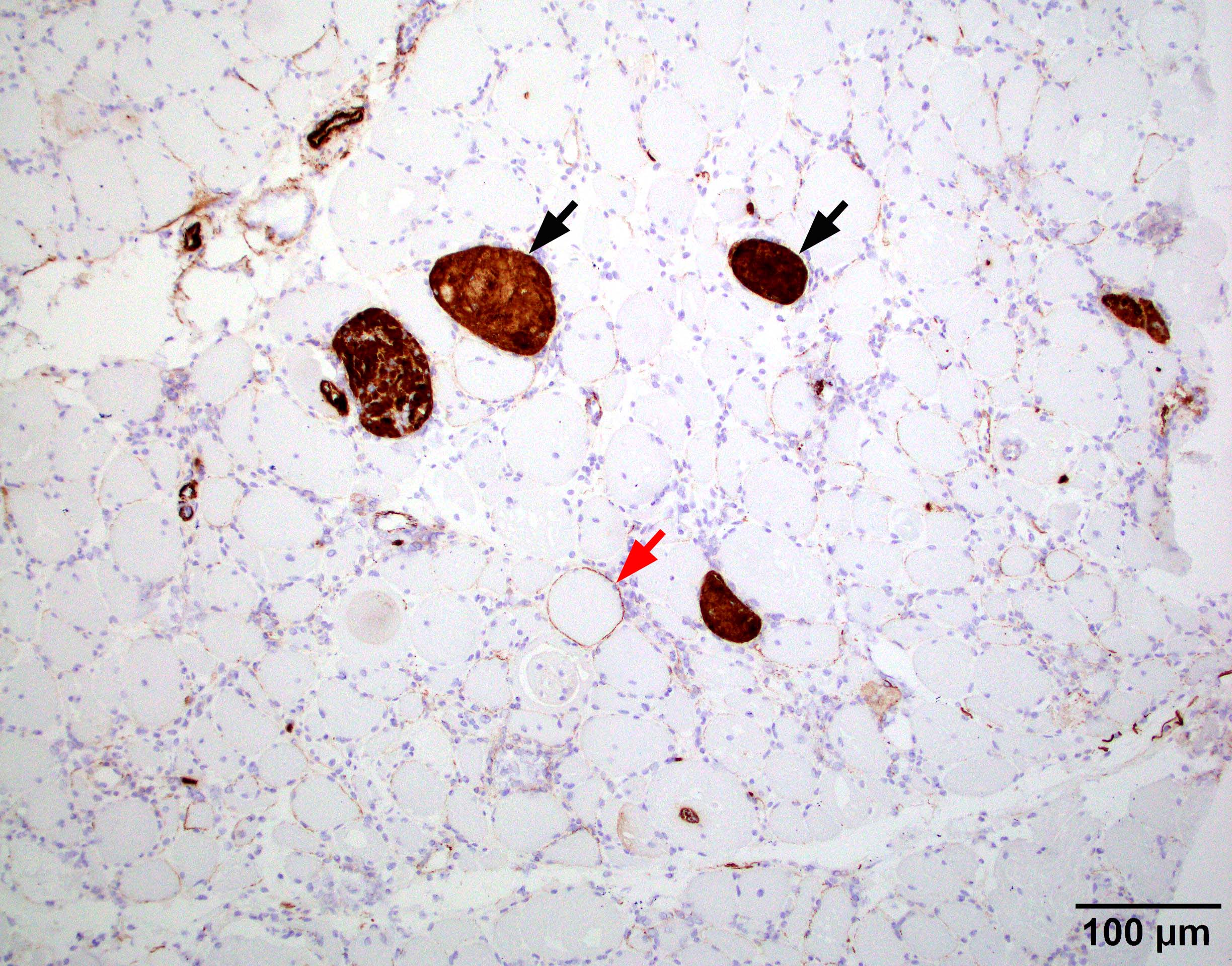
Negative stains
- IMNM is usually negative for MHC1; a subset of IMNM with anti-HMGCR may have some MHC1 expression in scattered myofibers but no diffuse expression (Arthritis Rheum 2010;62:2757)
Electron microscopy description
- There are no endothelial tubuloreticular inclusions in IMNM
Sample pathology report
- Skeletal muscle, left quadriceps, biopsy:
- Necrotizing myopathy (see comment)
- Comment: The muscle demonstrates a pauci-inflammation necrotizing myopathy. Necrotic fibers are randomly distributed and temporally heterogeneous, including all stages of acute necrosis, myophagocytosis and regeneration. There are no specific features, such as perifascicular atrophy, lymphocytic invasion in myofibers or rimmed vacuoles, to suggest dermatomyositis, polymyositis or inclusion body myositis, respectively.
- The primary differential consideration is an immune mediated necrotizing myopathy (IMNM). Clinical correlation with serological myositis specific markers including anti-SRP and anti-HMGCR antibodies may be of additional diagnostic value. Alternatively, exogenous toxins or medication such as statins may cause acute myofiber damage. Clinical correlation is needed. Metabolic disease can present as acute myofiber damage or rhabdomyolysis but this is less likely given the age of the patient, presentation and lack of storage material in muscle fibers.
Differential diagnosis
- Rhabdomyolysis:
- Necrotic fibers in rhabdomyolysis are more monophasic (temporally homogeneous), while necrotic fibers in IMNM are more temporally heterogeneous (include all stages of acute necrosis, myophagocytosis, regeneration)
- Polymyositis:
- Polymyositis requires the presence of lymphocytic inflammation surrounding or invading myofibers; IMNM typically lacks visible lymphocytic inflammation
- MHC1 is usually diffuse upregulated in polymyositis but negative in IMNM
- Muscular dystrophy:
- Besides abundant necrotic fibers, muscular dystrophy typically has prominent chronic dystrophic changes (i.e. fatty replacement, interstitial fibrosis, prominent fiber size variation), which are usually lacking in IMNM
- Antisynthetase syndrome associated myositis:
- Antisynthetase syndrome associated myositis typically shows prominent perifascicular necrotizing myopathy and perimysial connective tissue damage that is distinctive from the randomly distributed pattern from IMNM (Brain 2015;138:2485, Brain 2016;139:e50)
Board review style question #1
A 55 year old man presented with 2 weeks of proximal muscle weakness and myalgia. Muscle biopsy shows finding in the above image. Which of the following serum autoantibodies is most supportive of the diagnosis of an immune mediated necrotizing myopathy?
- Anti-ANA
- Anti-Jo1
- Anti-Mi2
- Anti-NT5c1a
- Anti-SRP
Board review style answer #1
E. Anti-SRP. Anti-SRP autoantibody is a specific marker for immune mediated necrotizing myopathy. Anti-Mi2 is a specific serum marker for dermatomyositis. Anti-Jo1 is a specific marker for antisynsthetase syndrome associated myositis. Anti-ANA is a nonspecific autoantibody present in many systemic autoimmune diseases. Anti-NT5c1a is an autoantibody most commonly associated with sporadic inclusion body myositis.
Comment Here
Reference: Immune mediated necrotizing myopathy
Comment Here
Reference: Immune mediated necrotizing myopathy
Board review style question #2
A 55 year old man presented with 2 weeks of proximal muscle weakness, myalgia and elevated creatine kinase. Muscle biopsy shows necrotizing myopathy. Serology workup is positive for anti-SRP autoantibody. Which of the following additional tests is highly recommended?
- Abdominal CT
- Cancer screening tests
- Chest CT
- EKG
Board review style answer #2
C. Chest CT. Anti-SRP myopathy is highly associated with interstitial lung disease, therefore a chest CT is highly recommended. Cardiac involvement can be seen in association with anti-SRP myopathy but is uncommon. Anti-SRP myopathy is not associated with occult malignancy.
Comment Here
Reference: Immune mediated necrotizing myopathy
Comment Here
Reference: Immune mediated necrotizing myopathy