Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Xu B. Nasopharyngeal angiofibroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalangiofibroma.html. Accessed April 17th, 2024.
Definition / general
- Locally aggressive fibrovascular neoplasm of the nasopharynx developed almost exclusively in adolescent and young male patients
Essential features
- Nasopharyngeal location
- Affecting adolescent or young male patients
- Histologically composed of vasculature of various sizes and cellular fibrotic stroma with fibroblasts
Terminology
- Juvenile nasopharyngeal angiofibroma, juvenile fibroma, angiofibroma
Epidemiology
- 0.05 - 0.5% of all head and neck tumors (StatPearls: Nasopharyngeal Angiofibroma [Accessed 10 June 2020])
- Occurs almost exclusively in adolescent and young males, with a median age of diagnosis of 15 years (range: 8 - 27 years) (Acta Otorrinolaringol Esp 2019;70:279, Head Neck Pathol 2018;12:52)
- Although a handful of case reports describe nasopharyngeal angiofibroma in female patients, the documentation of these cases is not convincing to represent this particular entity (Mol Clin Oncol 2018;9:702, J Laryngol Otol 2018;132:184, Eur Arch Otorhinolaryngol 2006;263:657, Indian J Dent Res 2004;15:145, AMA Arch Otolaryngol 1951;54:620)
- May occur in patients with familial adenomatous polyposis (Gastroenterology 1993;105:1550, Otolaryngol Head Neck Surg 1995;113:435, ANZ J Surg 2013;83:387)
Sites
- Arises in the nasopharynx or posterolateral wall of nasal cavity (Otolaryngol Head Neck Surg 2019;161:352)
- May be locally aggressive, show extension into paranasal sinus, pterygopalatine fossa, infratemporal fossa and orbit (Otolaryngol Head Neck Surg 2019;161:352)
- 10 - 37% have intracranial extension, usually into the middle cranial fossa (Otolaryngol Head Neck Surg 2019;161:352, StatPearls: Nasopharyngeal Angiofibroma [Accessed 10 June 2020])
Etiology
- Etiology remains unclear
- May be hormonally affected given the predilection for adolescent male
Clinical features
- Highly vascular lesion with one or more feeding arterials
- The most common feeding vessel is the internal maxillary artery, a branch of the external carotid artery (StatPearls: Nasopharyngeal Angiofibroma [Accessed 10 June 2020])
- Most frequently presents with epistaxis followed by nasal obstruction and rhinorrhea (Head Neck Pathol 2018;12:52, J Oral Maxillofac Pathol 2016;20:330)
Diagnosis
- Diagnosis is typically rendered using angiography, which allows visualization of the feeding vessels and preoperative embolization
- Given the risk of massive hemorrhage, preoperative biopsy and fine needle aspiration is strongly discouraged
Radiology description
- Angiography allows identification of a highly vascularized mass with a central feeding vessel
Prognostic factors
- Although considered as a benign mesenchymal neoplasm, nasopharyngeal angiofibroma is locally aggressive with approximately 20% local recurrence (Otolaryngol Head Neck Surg 2019;161:352, J Laryngol Otol 2018;132:978)
- Cranial or orbital involvement and postoperative residual vascularity on imaging study are associated with increased risk of local recurrence (Otolaryngol Head Neck Surg 2019;161:352)
Case reports
- 17 year old boy with nasopharyngeal angiofibroma extending intraorally (J Oral Maxillofac Pathol 2016;20:330)
- 18 year old man with nasal mass, recurrent epistaxis and nasal obstruction (J Clin Diagn Res 2017;11:MD03)
- 21 year old man with bilateral nasopharyngeal angiofibroma (Eur Arch Otorhinolaryngol 2016;273:3435)
- 31 year old man with Proteus syndrome and nasopharyngeal angiofibroma (Hippokratia 2017;21:147)
- 32 year old man with severe epistaxis and nasopharyngeal mass (BMJ Case Rep 2018)
Treatment
- Complete surgical resection is the treatment of choice
- Preoperative embolization through angiography may be performed
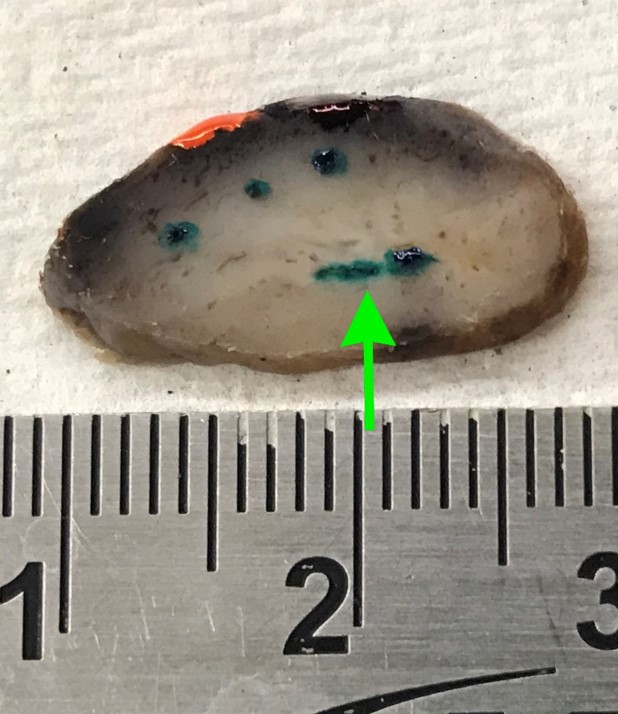
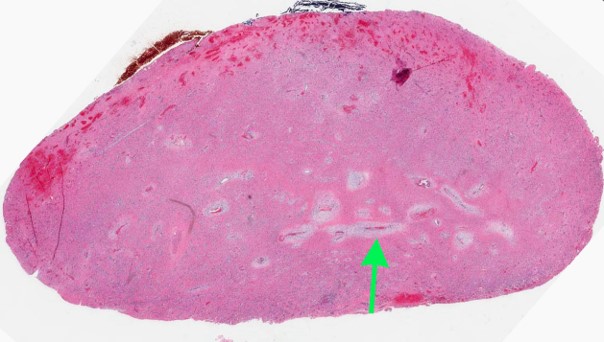
Gross description
- Polypoid firm mass
- Color varies from yellow to dark red or black, depending on the extent of intraoperative hemorrhage
Gross images
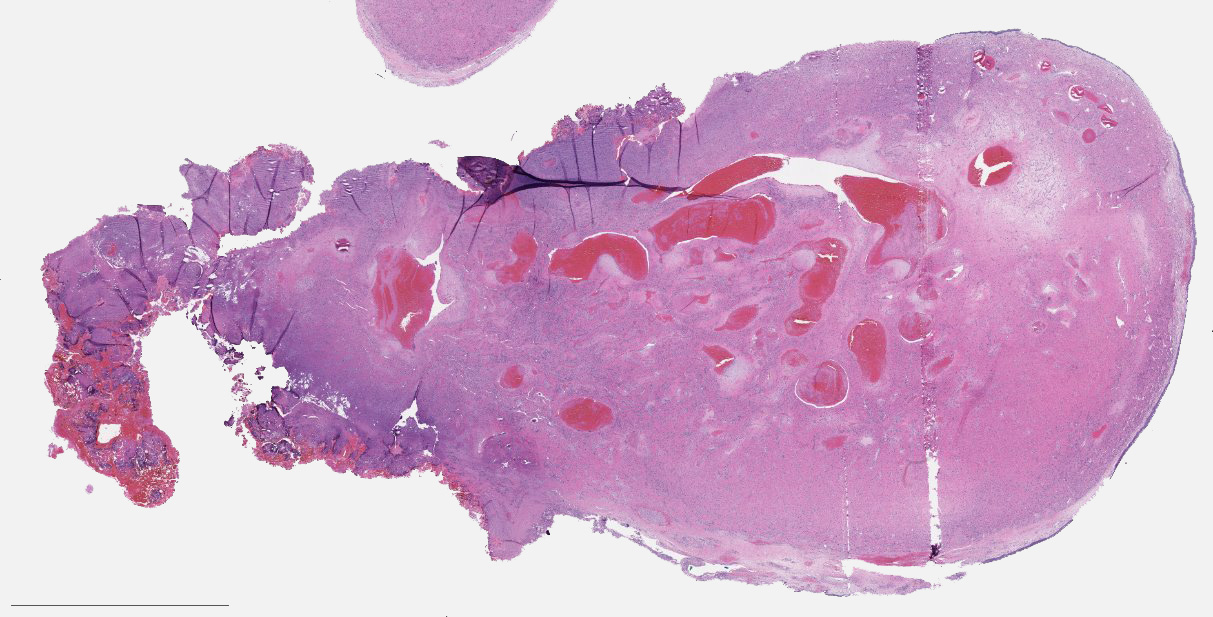
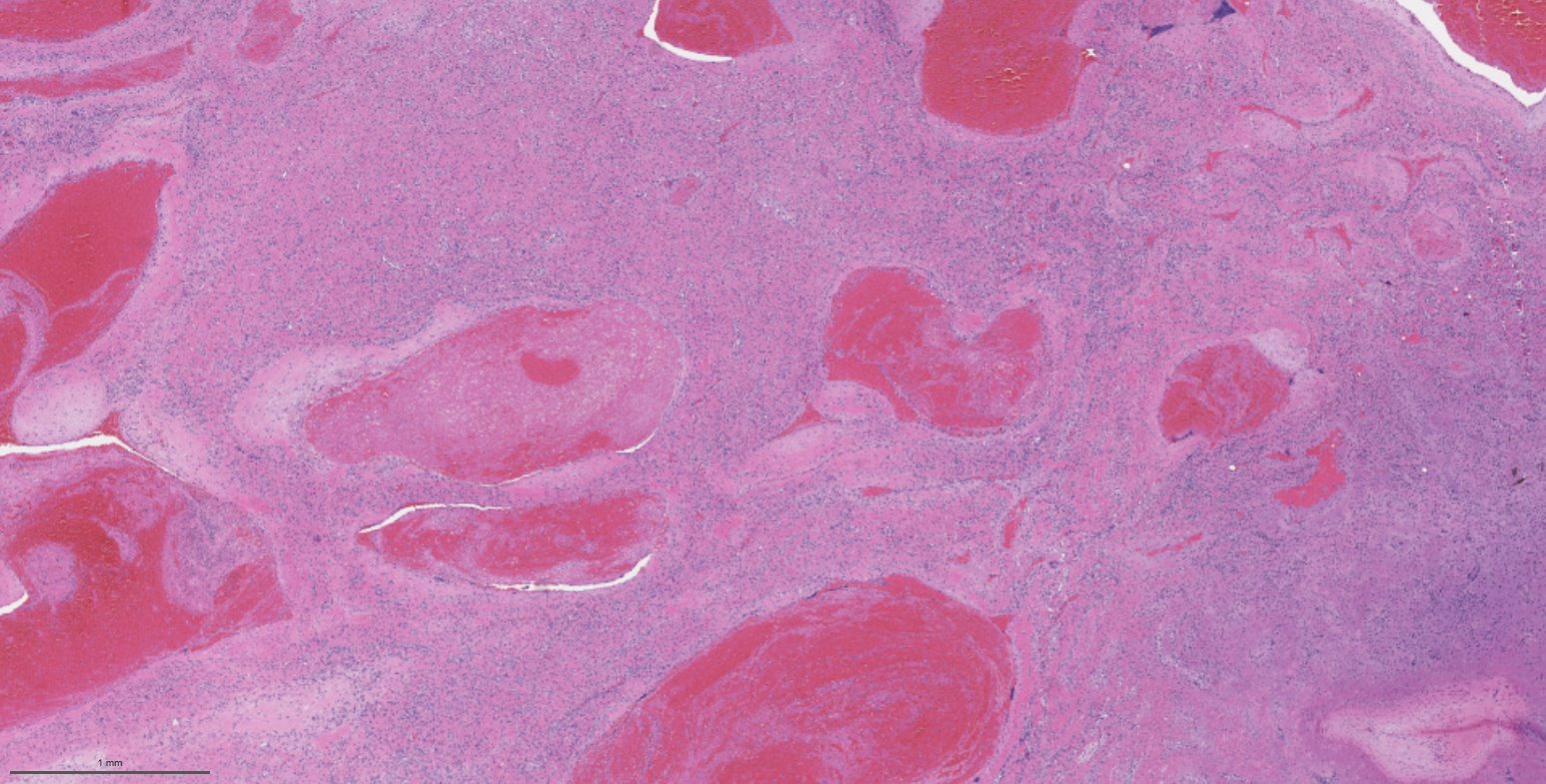
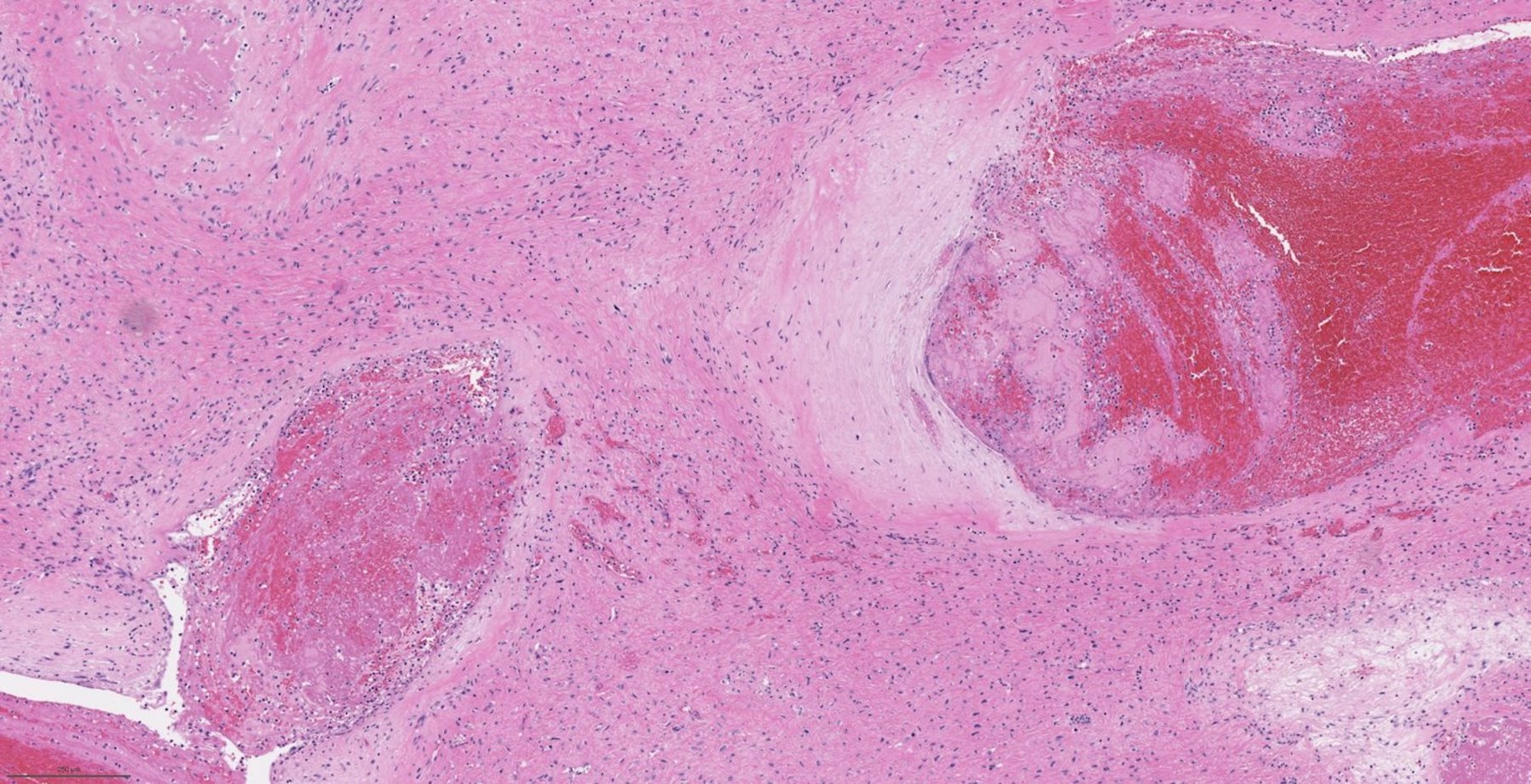
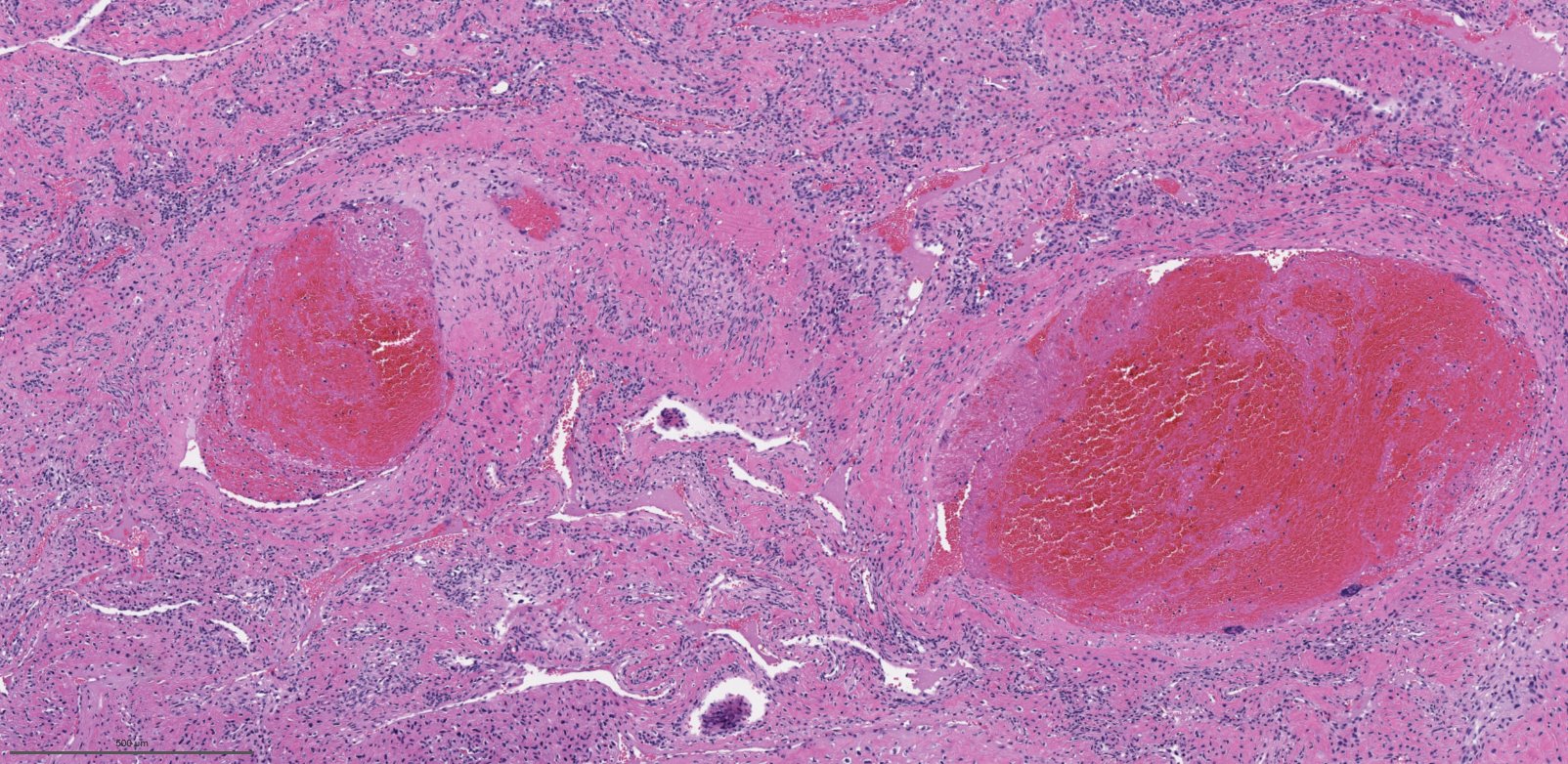
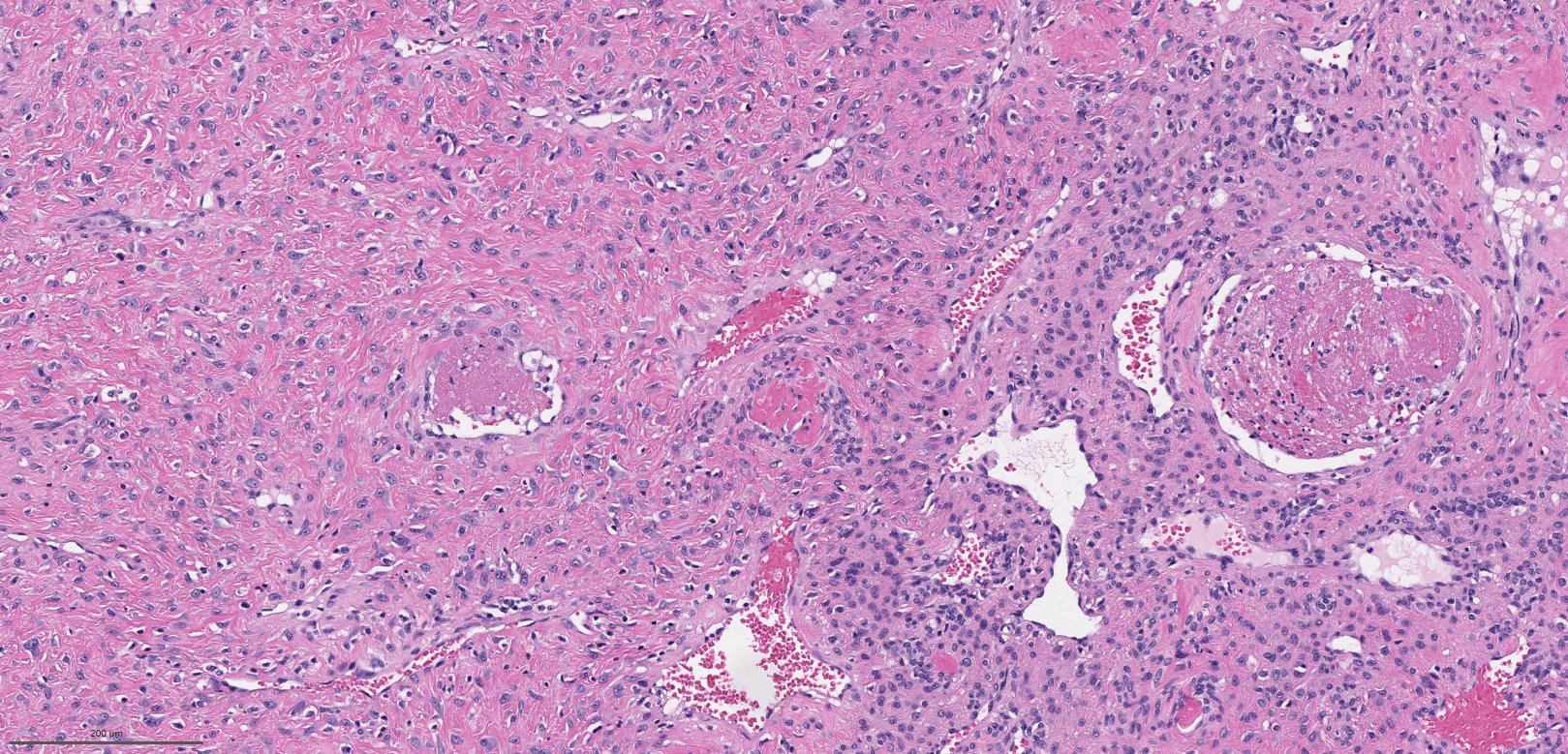
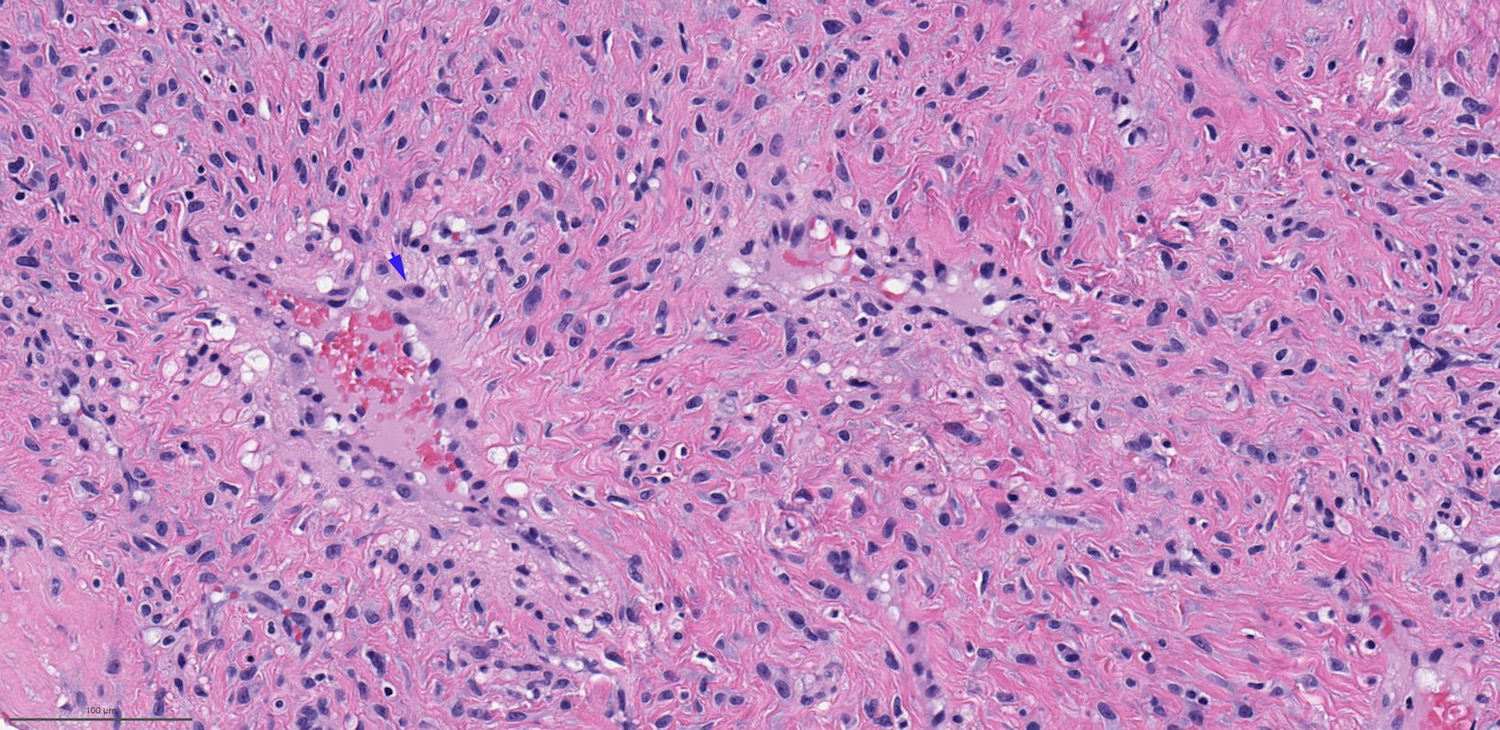
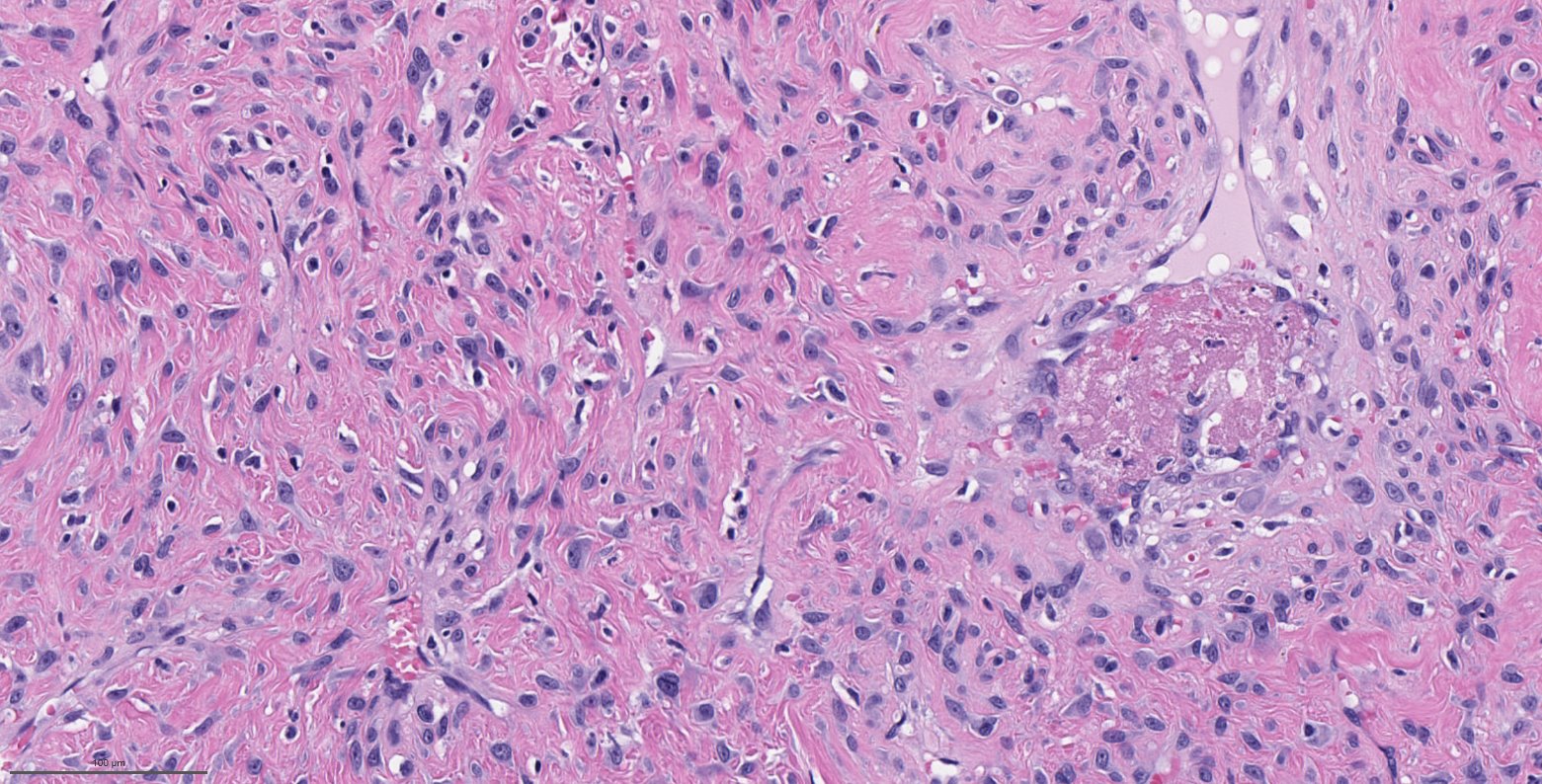
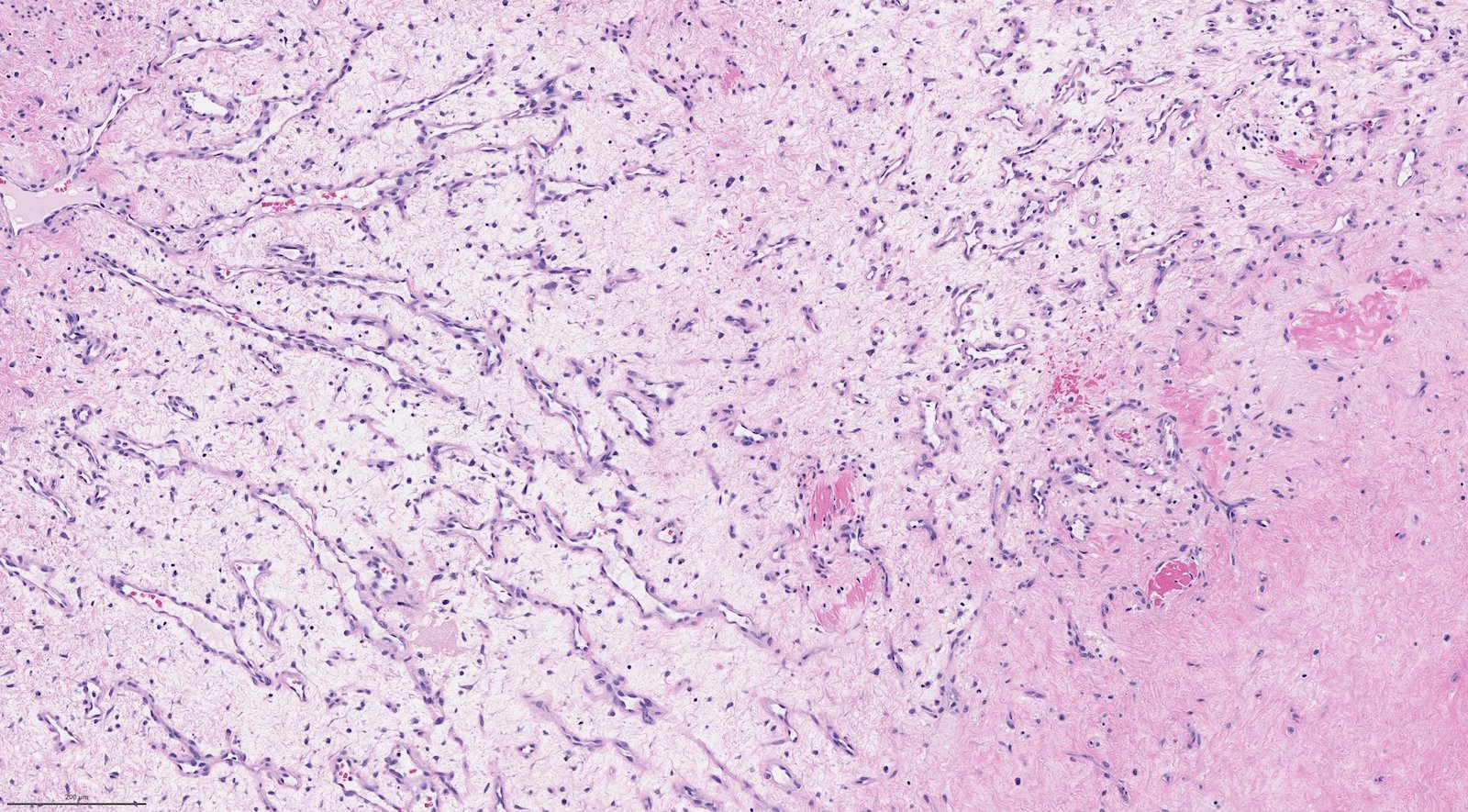
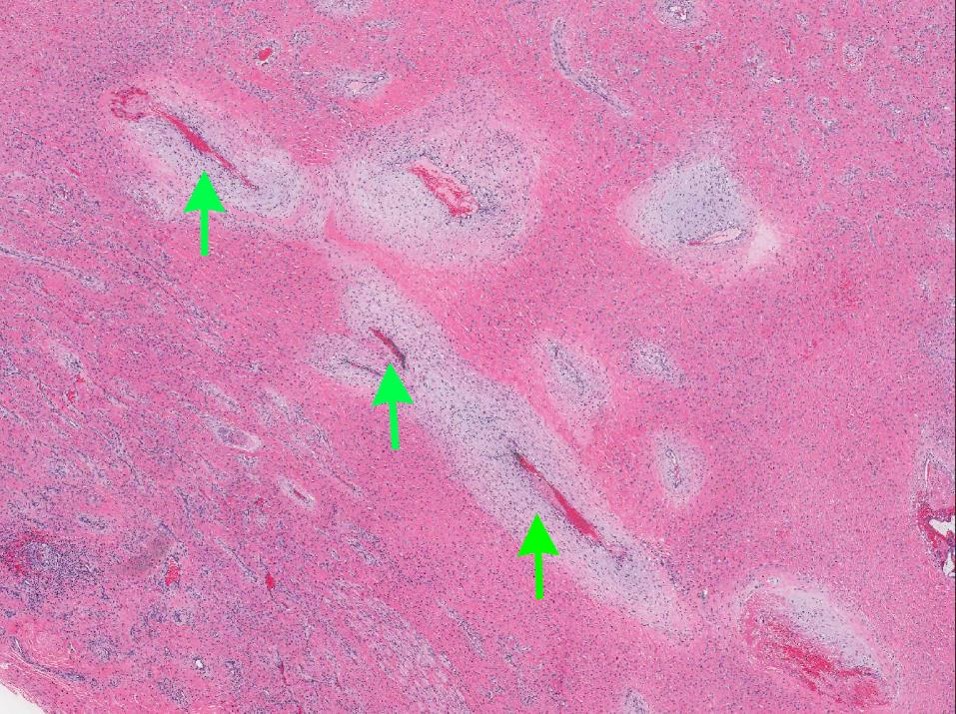
Microscopic (histologic) description
- Benign fibrovascular lesion composed of 2 components
- Vascular space of various sizes, ranging from dilated branching vessel of various thickness to slit-like capillaries
- Fibrous or collagenous stroma with fibroblasts
- Central area of the tumor is typically cellular, composed of fibroblasts or myofibroblasts with spindle, round or stellate morphology
- Stroma can be fibrous, edematous or collagenized
- Fibrinous thrombi may be seen in dilated vessels
- Frequently contain (abundant) mast cells
- Mitotic figures are usually absent
- Reference: Chan: WHO Classification of Head and Neck Tumours, 4th Edition, 2017
Microscopic (histologic) images
Contributed by Bin Xu, M.D., Ph.D.
Contributed by Kelly Magliocca, D.D.S., M.P.H.
Cytology description
- Given the nasopharyngeal location and the highly vascular nature of the lesion, fine needle aspiration should be avoided
Positive stains
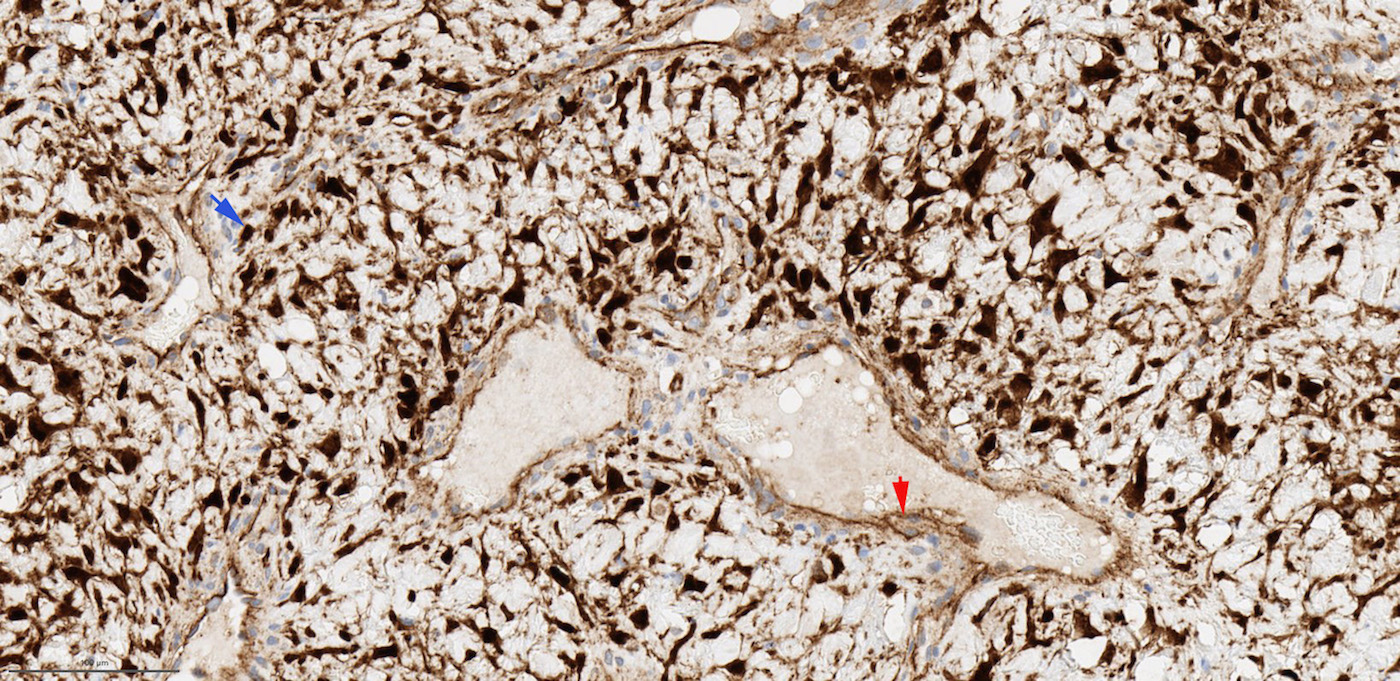
- SMA, HHF35 / h-caldesmon in smooth muscle wall of large vasculature (Pathology 2008;40:396, Head Neck Pathol 2018;12:52)
- CD31, CD34 and ERG highlight endothelial cells of vasculature
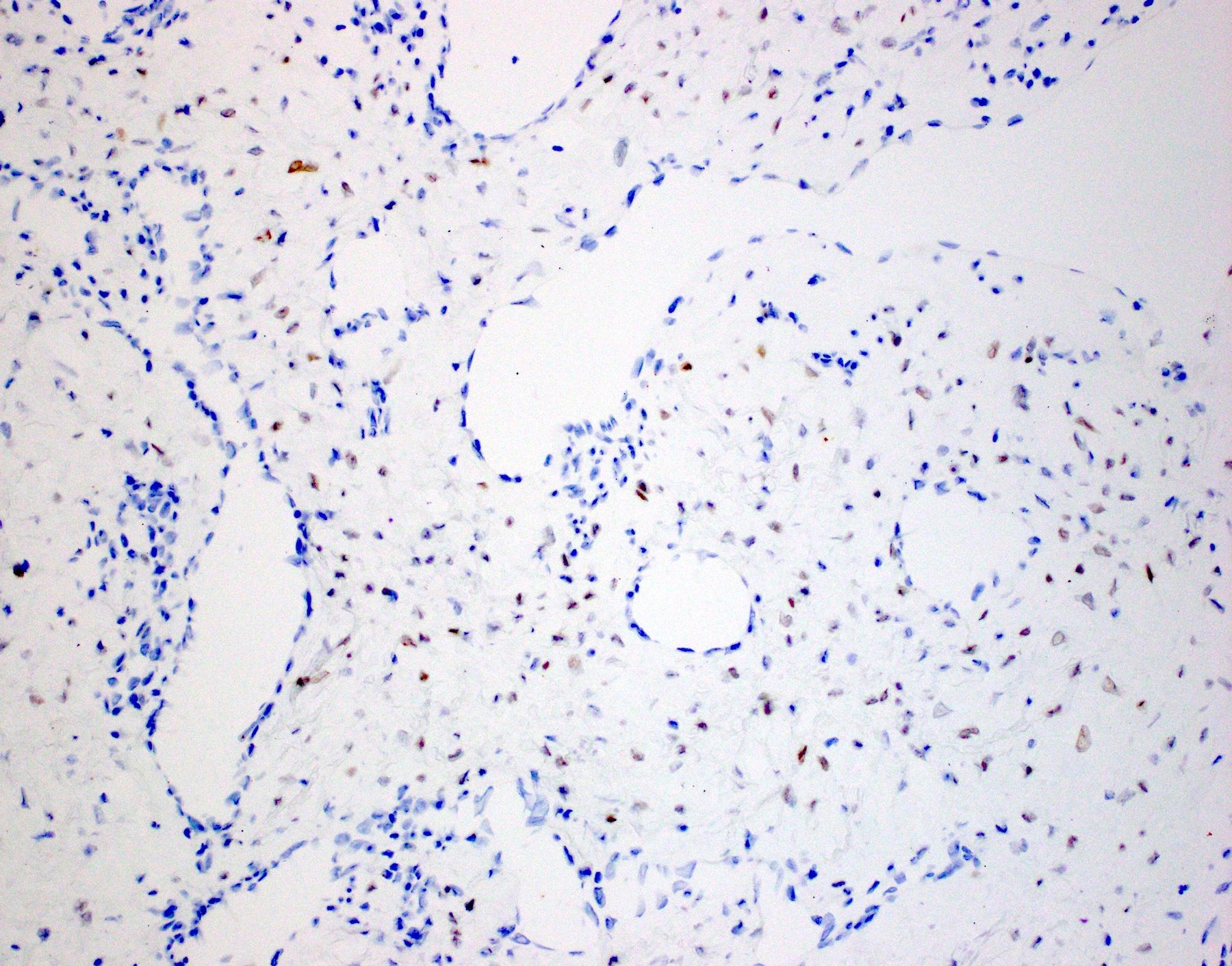
- AR is positive in stroma cells in 40 - 75% cases; the expression may be focal and weak (Acta Otolaryngol 2015;135:51, Am J Clin Pathol 2006;125:832, Mod Pathol 1998;11:1122)
- Reported positive rate of ER is highly variable, ranging from 0% to over 90% partially depending on the subunits stained (Acta Otolaryngol 2015;135:51, Am J Clin Pathol 2006;125:832)
- Beta catenin: nuclear staining in stromal cells (fibroblasts) in 70 - 90% of cases, membranous / cytoplasmic staining in endothelial cells (J Laryngol Otol 2016;130:907)
Negative stains
Molecular / cytogenetics description
- Somatic mutation of CTNNB1 (beta catenin) gene in 75% of cases (Ann Otol Rhinol Laryngol 2019;128:1061)
Sample pathology report
- Nasopharynx, resection:
- Nasopharyngeal angiofibroma, 1.8 cm, margin negative for tumor (see comment)
- Comment: Immunostain shows that the tumor is focally positive for AR. There is abnormal nuclear accumulation of beta catenin. The immunoprofile supports the diagnosis.
Differential diagnosis
- Hemangioma:
- May affect both genders, any age and is not limited to nasopharynx
- Lacks cellular stroma enriched with fibroblasts
- Vessels are typically uniform in size, whereas angiofibroma usually contains central large caliber vessels and peripheral slit-like vascular space
- Does not show AR immunopositivity or nuclear beta catenin
- Inflammatory sinonasal polyp:
- May contain fibrous to edematous stroma but usually hypocellular
- Lack rich vasculature seen in angiofibroma
- Does not show AR immunopositivity or nuclear beta catenin
- Occurs in nasal cavity or paranasal sinuses, rather than nasopharynx
- Nasal turbinate:
- Normal nasal turbinate is vascular rich, containing large caliber blood vessels with muscle wall
- Lacks hypercellular stroma and slit-like vasculatures of angiofibroma
Board review style question #1
Board review style answer #1
B. It is locally aggressive with 20% risk of local recurrence
Comment Here
Reference: Nasopharyngeal angiofibroma
Comment Here
Reference: Nasopharyngeal angiofibroma
Board review style question #2
- Which of the following statements of nasopharyngeal angiofibroma is true?
- It generally affects adolescent women
- It has a hormonal profile of ER+, PR+, AR+
- It is a benign lesion that can be safely managed by long term observation even when large
- The most frequent molecular alteration in this lesion is CTNNB1 somatic mutation
Board review style answer #2
D. The most frequent molecular alteration in this lesion is CTNNB1 somatic mutation
Comment Here
Reference: Nasopharyngeal angiofibroma
Comment Here
Reference: Nasopharyngeal angiofibroma