Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Smith MH. Lingual tonsil. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavitylingualtonsil.html. Accessed September 20th, 2025.
Definition / general
- Collection of reactive submucosal lymphoid nodules situated on the dorsal or lateral aspects of the tongue base, which presents clinically as red papules or nodules
- One of the three sets of tonsils present within Waldeyer ring, along with the pharyngeal and palatine tonsils
Essential features
- Clinically presents as red papules or nodules posterior to the circumvallate papillae
- Often clinically diagnostic, although asymmetric, hyperplastic nodules may warrant biopsy to rule out lymphoma, HPV-positive squamous cell carcinoma, or other pathology
- Hyperplastic lingual tonsil is associated with obesity, obstructive sleep apnea, acid reflux disease, younger age, allergic rhinitis and smoking (Am J Rhinol Allergy 2020;34:87)
Terminology
- Hyperplastic lingual tonsil
- Hyperplastic lymphoid aggregates
- Lingual tonsillar hypertrophy
ICD coding
- ICD-10: J35.1 - hyperplastic lingual tonsil
Epidemiology
- Normal anatomical structure
- Hyperplastic lingual tonsils demonstrate higher incidence in younger patients (Am J Rhinol Allergy 2020;34:87)
- Associated with obesity, obstructive sleep apnea, laryngopharyngeal reflux, younger age, allergic rhinitis and smoking (Am J Rhinol Allergy 2020;34:87)
Sites
- Base of tongue, dorsal or lateral aspects, posterior to the circumvallate papillae
- Anterior to the epiglottis
Clinical features
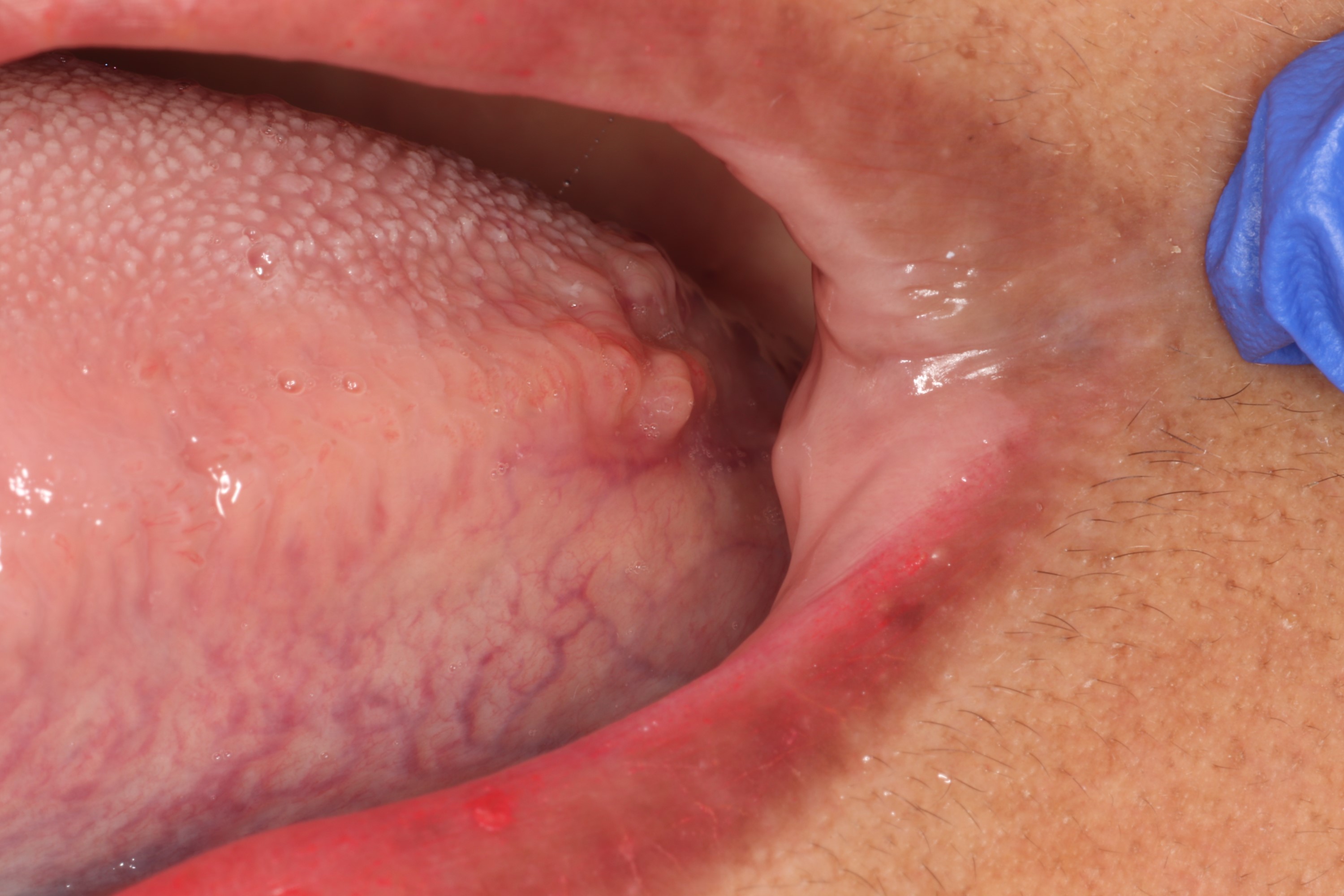
- Red papules or nodules on the dorsal or lateral aspects of the base of the tongue
- Size ranges from a small papule to a large mass (Clin Otolaryngol 2017;42:144)
- Patients with hyperplastic lingual tonsils may present with dysphagia, chronic cough, voice changes, globus sensation, snoring, lingual tonsillitis or rarely airway compromise (Am J Rhinol Allergy 2020;34:87, Cureus 2020;12:e8309, BMJ Case Rep 2019;12:e229555)
- May contribute to the pathogenesis of acid reflux or obstructive sleep apnea in children who are obese (J Otolaryngol Head Neck Surg 2017;46:32)
- Hyperplastic lingual tonsils may cause difficulty in face mask ventilation or tracheal intubation (Clin Otolaryngol 2017;42:144, Anesthesiology 2010;112:746)
Diagnosis
- Diagnosis is made upon clinical features or awake endoscopy (Otolaryngol Head Neck Surg 2018;158:391)
- Biopsy rarely is indicated to rule out other pathological causes of submusocal masses (e.g. lymphoma)
- Head and neck computed tomography (CT), magnetic resonance imaging (MRI), skull lateral radiographs may prove useful in diagnosis and staging of lingual tonsil hypertrophy (Otolaryngol Head Neck Surg 2017;157:898)
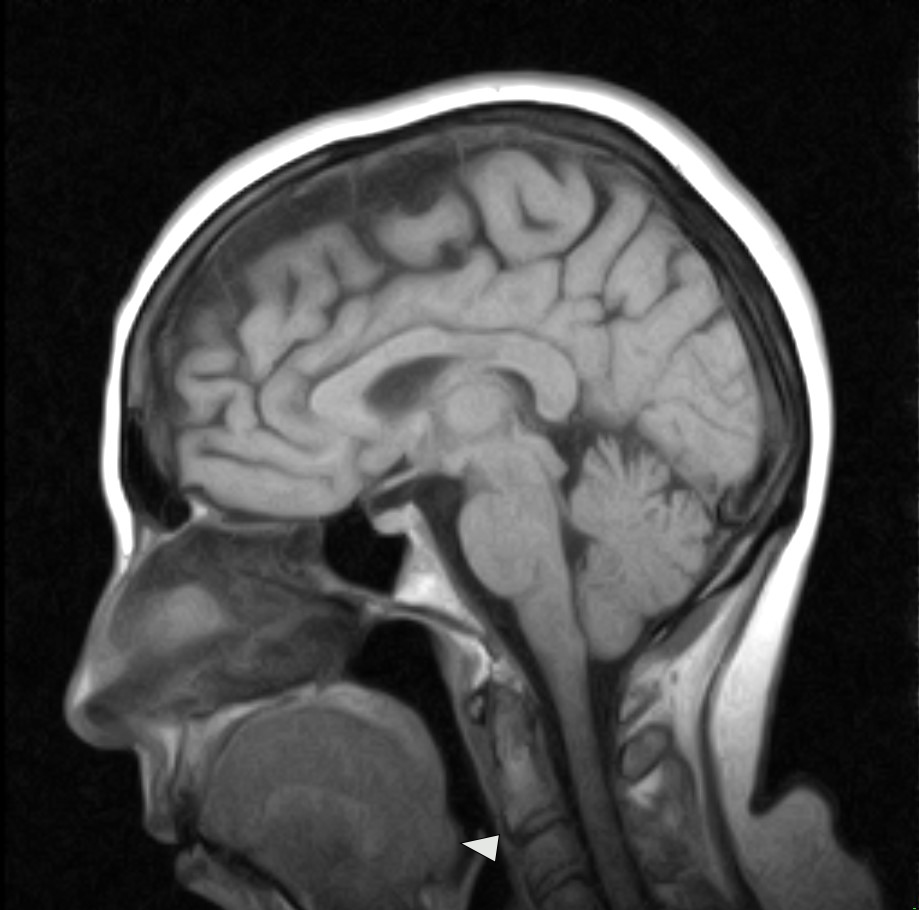
Radiology description
- Head and neck computed tomography (CT), magnetic resonance imaging (MRI) and skull lateral radiographs demonstrate lingual tonsils at the level of the epiglottis on the tongue base (Otolaryngol Head Neck Surg 2017;157:898)
Case reports
- 17 year old girl and 26 and 30 year old women present with eosinophilic lingual tonsillitis following sublingual immunotherapy for allergic rhinitis (Clin Case Rep 2020;8:2211)
- 48 year old woman with lingual tonsil abscess contributing to rapidly progressing sore throat (BMJ Case Rep 2019;12:e229555)
- 70 year old woman with hyperplastic lingual tonsil leading to partial airway obstruction (Cureus 2020;12:e8309)
Treatment
- Nonsurgical medical management or surgical debulking / removal may be indicated in cases of hyperplastic lingual tonsil contributing to sleep apnea (Clin Otolaryngol 2017;42:144)
- Nonsurgical management most often entails treating symptoms of acid reflux to prevent inflammation of the tonsil tissue (Clin Otolaryngol 2017;42:144)
- Surgical debulking or removal includes a number of different techniques including sharp dissection, coblation, cryotherapy, laser ablation, suction diathermy, ultrasonographic coagulating dissection and bipolar radiofrequency plasma excision (JAMA Otolaryngol Head Neck Surg 2013;139:1032, Clin Otolaryngol 2017;42:144)
Clinical images
Microscopic (histologic) description
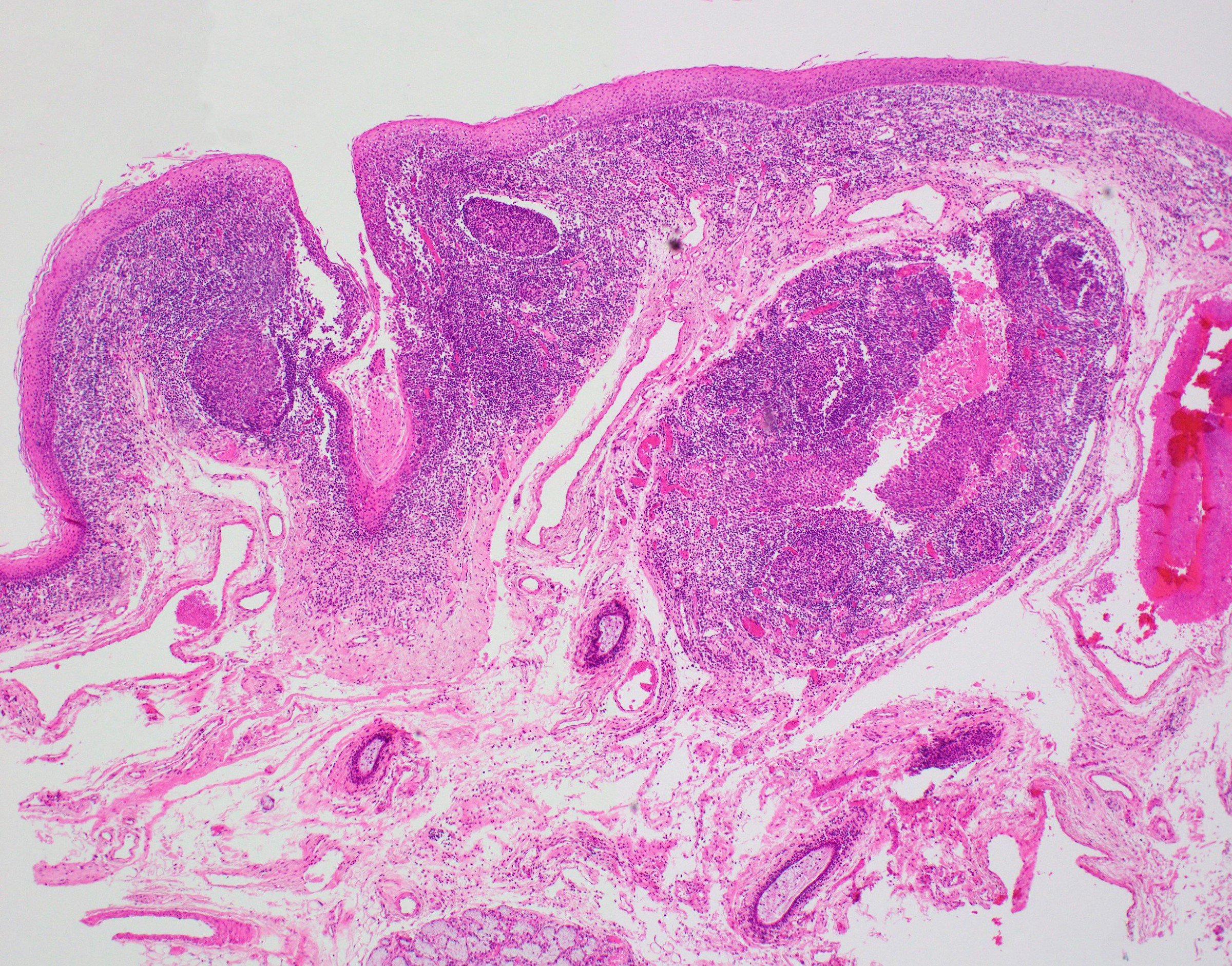
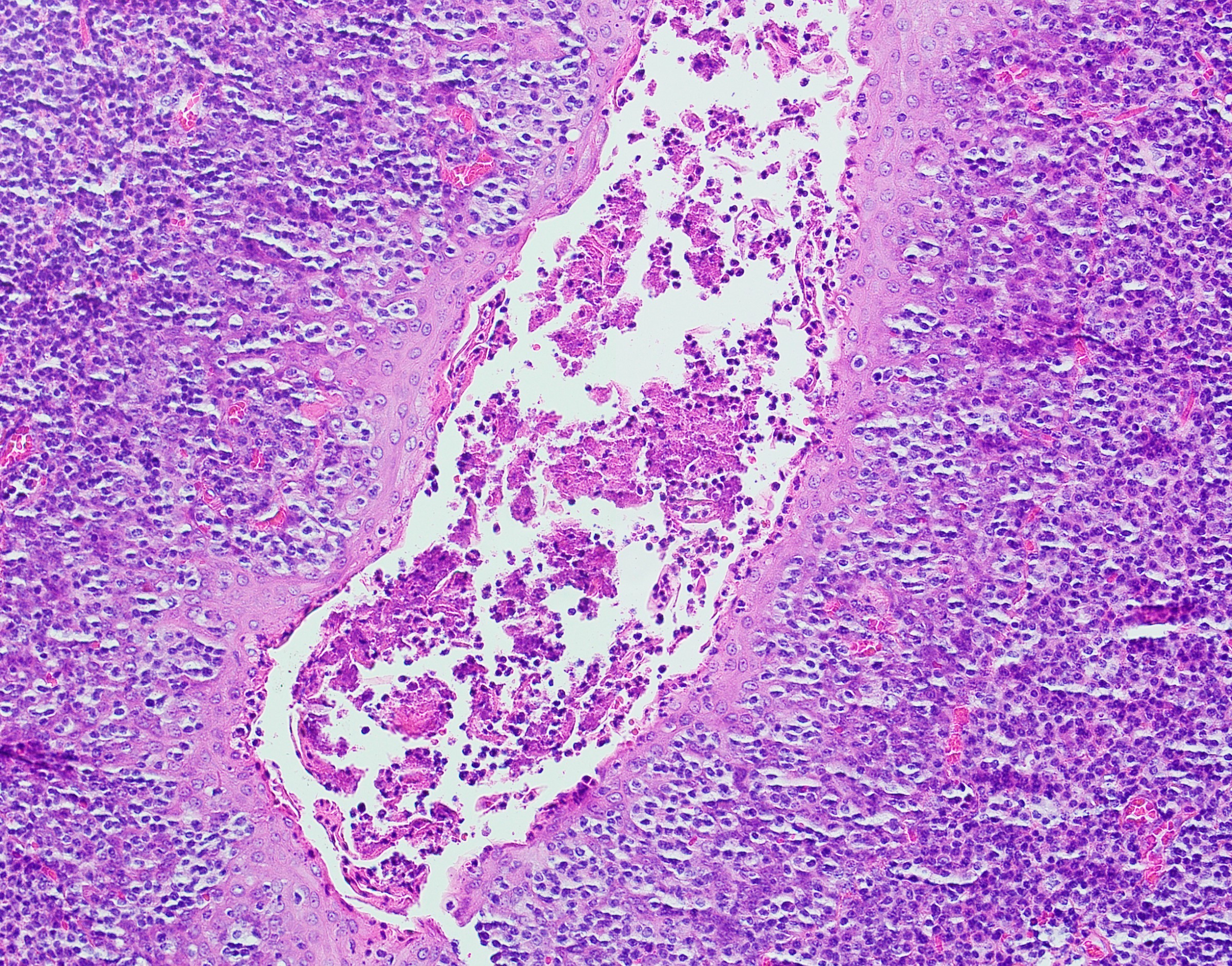
- Aggregates of benign lymphoid tissue, often with germinal center formation; germinal centers lack capsules and sinusoidal spaces
- May contain crypts lined by specialized keratinized stratified squamous epithelium (termed reticular epithelium) that invaginate from the surface; crypts are often filled with desquamated epithelial cells and bacteria, which may calcify
- Often surrounded by other normal structures of the tongue, including striated muscle, mucinous glands and serous glands
- Reference: Anat Histol Embryol 2005;34:27
Microscopic (histologic) images
Videos
Histology of the lingual tonsil
Lingual tonsillectomy for obstructive sleep apnea
Sample pathology report
- Tongue base, incisional biopsy:
- Hyperplastic lingual tonsil (see comment)
- Comment: Microscopic examination reveals surface stratified squamous epithelium and supporting connective tissue. The surface epithelium contains scattered taste buds and focally invaginates into the mesenchymal tissue forming deep crypts containing keratin flakes. Within the supporting connective tissue is a well defined area of lymphoid tissue. Germinal center formation is noted. Lobules of minor salivary glands and associated ductal structures are noted in the surrounding stroma.
Differential diagnosis
- Lymphoepithelial cyst:
- Often clinically presents as an opaque yellow-white nodule that easily ruptures upon manipulation
- Microscopically similar to lingual tonsil, although an enlarged cystic space is seen rather than an crypt-like invagination of surface epithelium (J Clin Exp Dent 2017;9:e1035)
- Human Papilloma Virus-Positive Squamous Cell Carcinoma (HPV-positive SCCa):
- Since HPV positive SCCa often originates deep within the tonsillar crypt epithelium, it may clinically present as an enlarged, smooth surfaced, red / pink nodule within the area of the lingual tonsils (Statpearls: Oropharyngeal Squamous Cell Carcinoma [Accessed 23 June 2021])
- Firm / indurated on palpation
- Typically larger in size when compared to the contralateral side of the tongue
- Microscopically, islands of epithelium arising from the tonsillar crypt epithelium are seen invading into the connective tissue in HPV-pos SCCa; P16ink4a or cytokeratin immunohistochemical markers may be used to highlight the invasive islands when dense inflammation obscures the presence of overt invasion
Additional references
Practice question #1
Oral examination of a patient reveals an asymmetric 4 mm red nodule at the dorsal tongue base. The patient is asymptomatic and was unaware of the finding. Biopsy of the lesion is shown. Which of the following is true regarding the diagnosis?
- Diagnosis of this entity relies heavily on immunohistochemical findings
- Diagnosis represents reactive hyperplasia of a normal structure
- Significant clinical follow up is recommended, since malignant transformation occurs in the majority of patients with this finding
- This entity is more commonly found in older adults
Practice answer #1
B. Diagnosis represents reactive hyperplasia of a normal structure
Comment Here
Reference: Lingual tonsil
Comment Here
Reference: Lingual tonsil
Practice question #2
A patient presents with a focal collection of red papules on the posterior lateral tongue. Biopsy demonstrates a well defined aggregate of lymphocytes showing germinal center formation. An epithelial lined crypt containing keratin is seen in the central aspects of the lymphocytic nodule. What is the most likely diagnosis?
- Fibroma
- HPV related squamous cell carcinoma
- Lingual tonsil
- Lymphoma
Practice answer #2