Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Glass SH. SCC-general. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityscc.html. Accessed October 5th, 2025.
Definition / general
- Squamous cell carcinoma (SCC) is a malignant neoplasm that arises from the mucosal epithelium of the oral cavity and shows variable squamous differentiation
Essential features
- Most common cancer of the oral cavity, with a variable clinical appearance and a predilection for the ventrolateral tongue
- Associated with tobacco, alcohol and betel quid
- Malignancy of squamous cells with varying degrees of keratinization
ICD coding
- ICD-10: C00 - C14 - malignant neoplasms of lip, oral cavity and pharynx
Epidemiology
- > 90% of cancers in the oral cavity are SCC
- Globally, the highest rates are seen in Melanesia and South Central Asia; it is the leading cause of cancer related death for men in India (CA Cancer J Clin 2021;71:209)
- For the United States, the American Cancer Society estimates ~58,000 new cases of oral and oropharyngeal cancers in 2024 with 12,230 deaths (American Cancer Society: Key Statistics for Oral Cavity and Oropharyngeal Cancers [Accessed 2 February 2024])
- M > F
- Average age is 63
- Can occur in younger patients, especially in the setting of dyskeratosis congenita or Fanconi anemia (J Pediatr Hematol Oncol 2019;41:501, Head Neck Pathol 2021;15:1099)
Sites
- Can occur at any oral mucosal site (mucosal lip, buccal mucosa, alveolar ridge, floor of the mouth, hard palate, mobile tongue)
- Classic high risk locations are ventrolateral tongue and floor of mouth
- Patients can develop second primaries, synchronous or metachronous, with field cancerization as a probable hypothesis (Head Neck 2020;42:1848, Oral Oncol 2015;51:643)
- Proliferative (verrucous) leukoplakia lesions have a high risk of malignant transformation, especially in locations such as the gingiva (Head Neck Pathol 2021;15:572)
- Spread typically occurs via the lymphatic system to cervical lymph nodes
Pathophysiology
- Multifactorial with accumulation of genetic alterations
- Loss of function of TP53 mutations and CDKN2A inactivation are frequently seen (Nature 2015;517:576)
- Oral potentially malignant disorders, many of which harbor some degree of epithelial dysplasia, are associated with a risk of malignant progression (Head Neck Pathol 2019;13:423)
Etiology
- Tobacco (Int J Cancer 2008;122:155)
- Alcohol (Lancet Oncol 2021;22:1071)
- Significantly higher risk with synergistic consumption of alcohol and tobacco (Clin Oral Investig 2019;23:2849)
- Betel quid, gutka, pan masala (Curr Oncol Rep 2019;21:53)
- Smokeless tobacco products (Nicotine Tob Res 2019;21:1162)
- Ultraviolet (UV) radiation for lip squamous cell carcinoma (Laryngoscope 2018;128:84)
- High risk human papillomavirus (HPV) is strongly associated with oropharyngeal squamous cell carcinoma; in contrast, 4.4% of oral squamous cell carcinoma cases are associated with high risk HPV (Braz J Otorhinolaryngol 2021;87:346)
- Controversy regarding oral lichen planus and malignant transformation is unresolved (Oral Surg Oral Med Oral Pathol Oral Radiol 2016;122:332)
- Due to confounding variables, chronic mechanical irritation has not been established as an independent risk factor (Bosn J Basic Med Sci 2021;21:647)
Clinical features
- Varied clinical presentation, including exophytic, endophytic, white (leukoplakia), red (erythroplakia), nonhealing ulceration
- May be preceded by or associated with an oral, potentially malignant disorder
- Clinical factors associated with malignancy include nonhomogenous leukoplakia, erythroplakia, induration, deep ulceration, exophytic component and pain (Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:264)
- Patient factors associated with malignant transformation include heavy tobacco smoking (> 20 pack years), heavy alcohol consumption (> 14 drinks/week for women and 21 drinks/week in men), immunosuppression (Head Neck 2021;43:3552)
- Firm, fixed, nontender cervical lymph nodes may indicate regional spread
Diagnosis
- U.S. Preventive Services Task Force concludes that for primary care providers, current evidence is insufficient to assess balance of benefits and harms of oral cancer screening in asymptomatic adults (Ann Intern Med 2014;160:55)
- Visual and tactile exams of the oral cavity are often performed by oral health care providers and otolaryngologists
- Immediate tissue biopsy with histopathologic examination for definitive diagnosis (J Am Dent Assoc 2017;148:712)
- 48.4% of cases are regional at diagnosis (NIH: Oral Cavity and Pharynx Stage Distribution of SEER Incidence Cases, 2011-2020 [Accessed 2 February 2024])
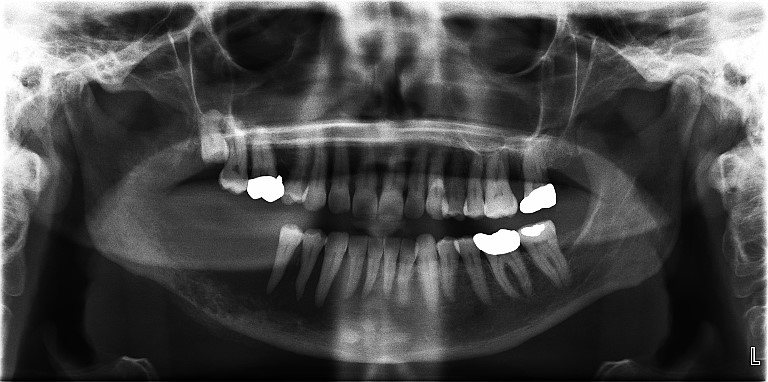
Radiology description
- Invasive, advanced tumors may be detected on dental radiographs as destruction of underlying bone producing an ill defined radiolucency
- Positron emission tomography (PET), computed tomography (CT) and magnetic resonance imaging (MRI) can be used to determine the presence and extent of disease
- Carcinomas arising in the jaw bones without a mucosal origin are primary intraosseous squamous cell carcinoma and are not discussed here (Head Neck Pathol 2021;15:608)
Prognostic factors
- 5 year survival rate of 68.5% (NIH: Cancer Stat Facts - Oral Cavity and Pharynx Cancer [Accessed 2 February 2024])
- Depth of invasion (DOI) and extranodal extension (ENE) were added to the AJCC staging 8th edition and are associated with upstaging (Oral Oncol 2018;85:82)
- Bone invasion is correlated with a worse prognosis (and invasion through cortical bone into medullary bone provides the tumor with AJCC stage T4a) (Arch Pathol Lab Med 2019;143:439)
- Noncohesive pattern of invasion is an adverse prognostic factor (Arch Pathol Lab Med 2019;143:439)
- Perineural invasion is associated with poor disease specific survival (J Oral Pathol Med 2020;49:994)
- Lymphovascular invasion may serve as a prognostic predictor of metastasis (Oral Surg Oral Med Oral Pathol Oral Radiol 2021;131:319)
- Margin of < 1 mm is associated with increased risk of local recurrence (JAMA Otolaryngol Head Neck Surg 2017;143:1166)
Case reports
- 28 year old woman with asymptomatic tumor of the left mandibular gingiva and Fanconi anemia (Case Rep Dent 2021;2021:5571649)
- 63 year old man with pain and swelling on the right lower jaw (Head Neck Pathol 2021;15:1313)
- 66 year old woman with fungating ulcerative mass on the left lateral tongue (Head Neck Pathol 2017;11:552)
- 70 year old woman with ulcerated mass on the lateral border of the tongue (Head Neck Pathol 2018;12:580)
Treatment
- Early staged lesions are often treated with surgery
- Patients with early stage cancer may benefit from elective neck dissection (N Engl J Med 2015;373:521)
- Moderate staged lesions are often treated with surgery, radiation therapy or chemotherapy
- Patients with recurrent or metastatic head and neck cancer may benefit from immunotherapeutic agents (J Immunother Cancer 2019;7:184)
Clinical images
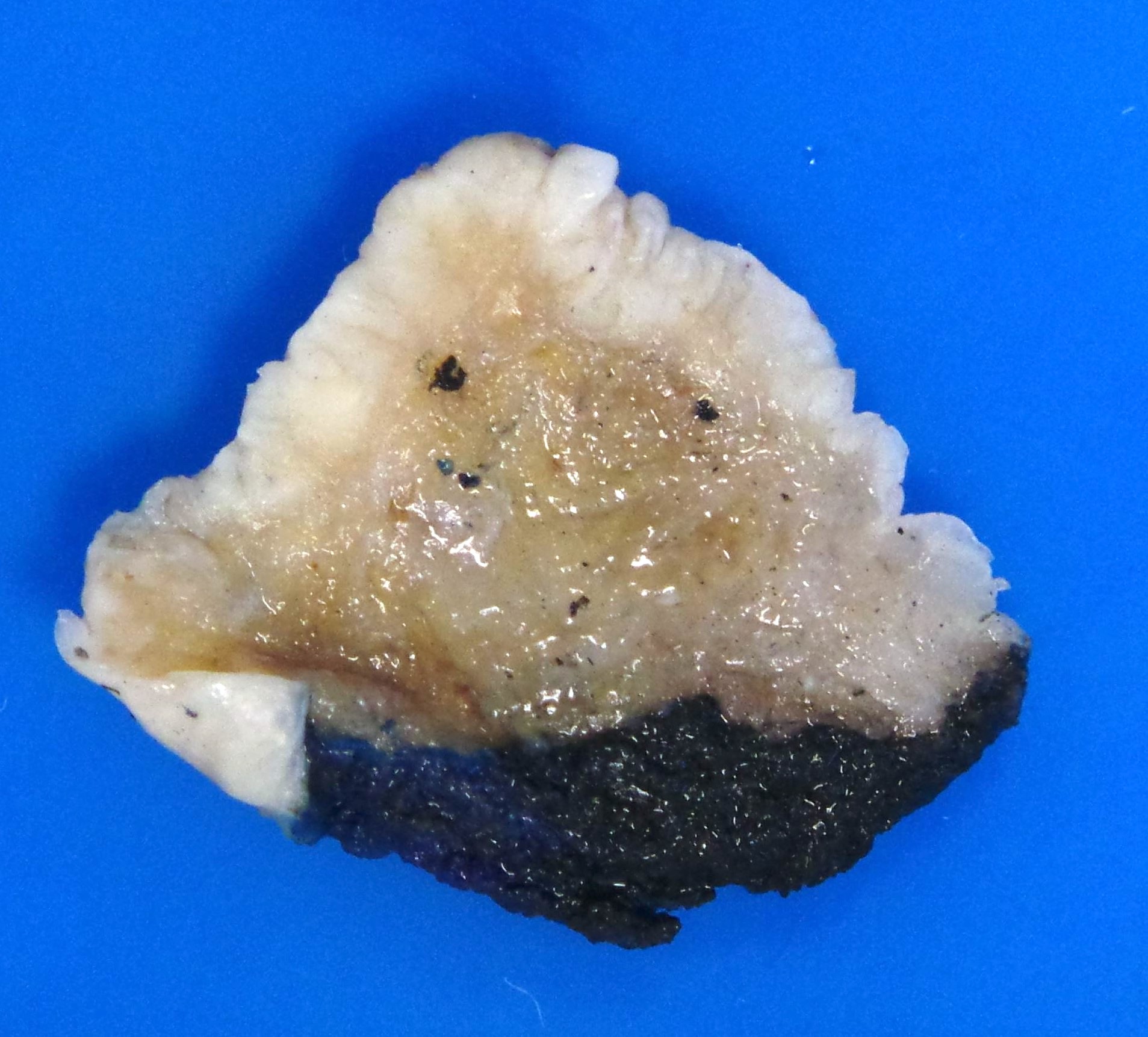
Gross description
- Site of involvement, tumor laterality and operative procedure should be communicated from the surgeon (Arch Pathol Lab Med 2019;143:439)
- Gross examination of a specimen may not entirely reflect microscopic tumor extent, as dysplasia, ulceration or inflammation may appear as tumor on macroscopic examination (Arch Pathol Lab Med 2019;143:439)
- White infiltrating tumor on cross section
Gross images
Frozen section description
- Frozen section analysis can be used to evaluate tumor diagnosis and margin status
- Results are highly specific but only moderately sensitive when compared with final margins (Laryngoscope 2000;110:1773)
Frozen section images
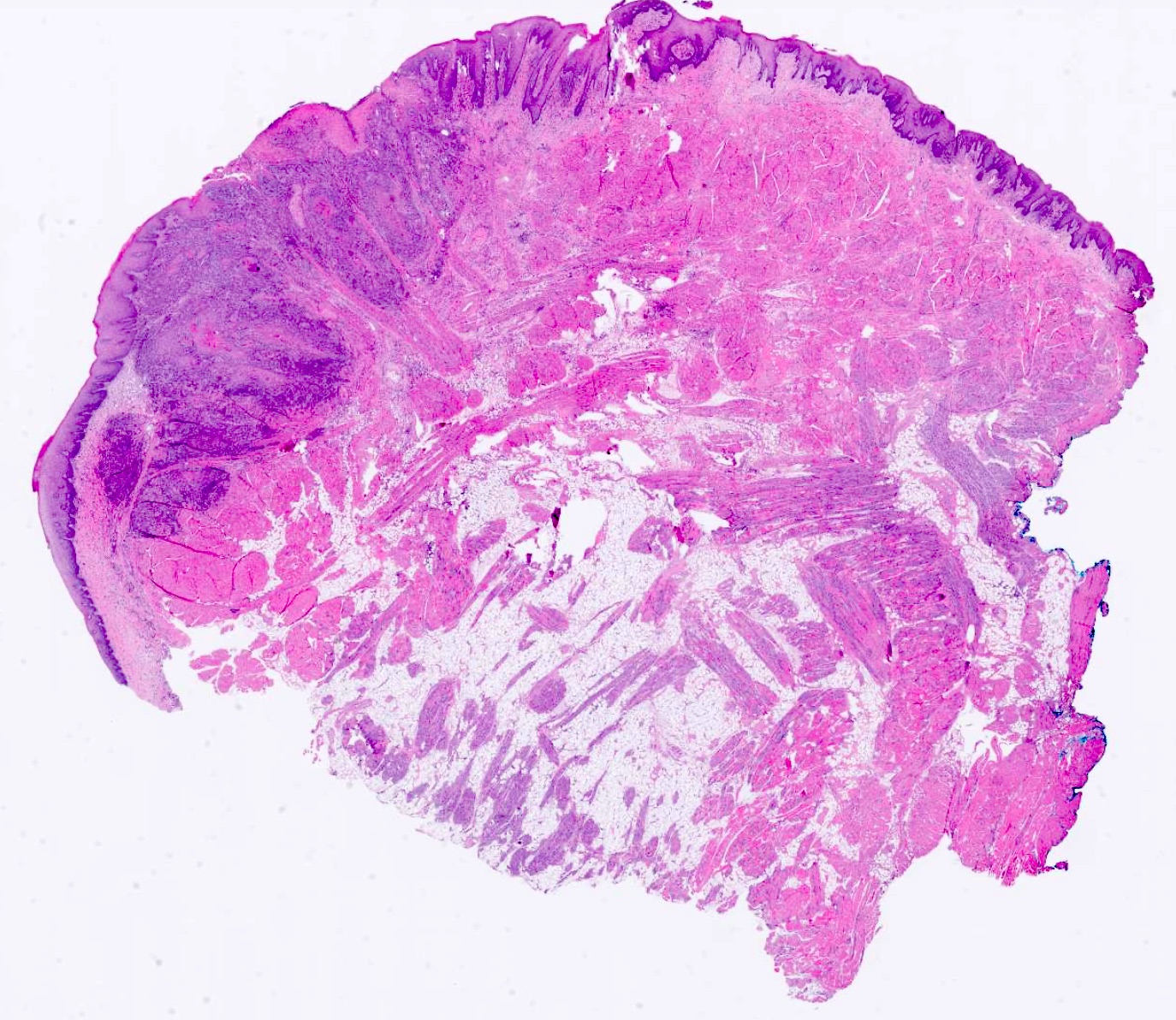
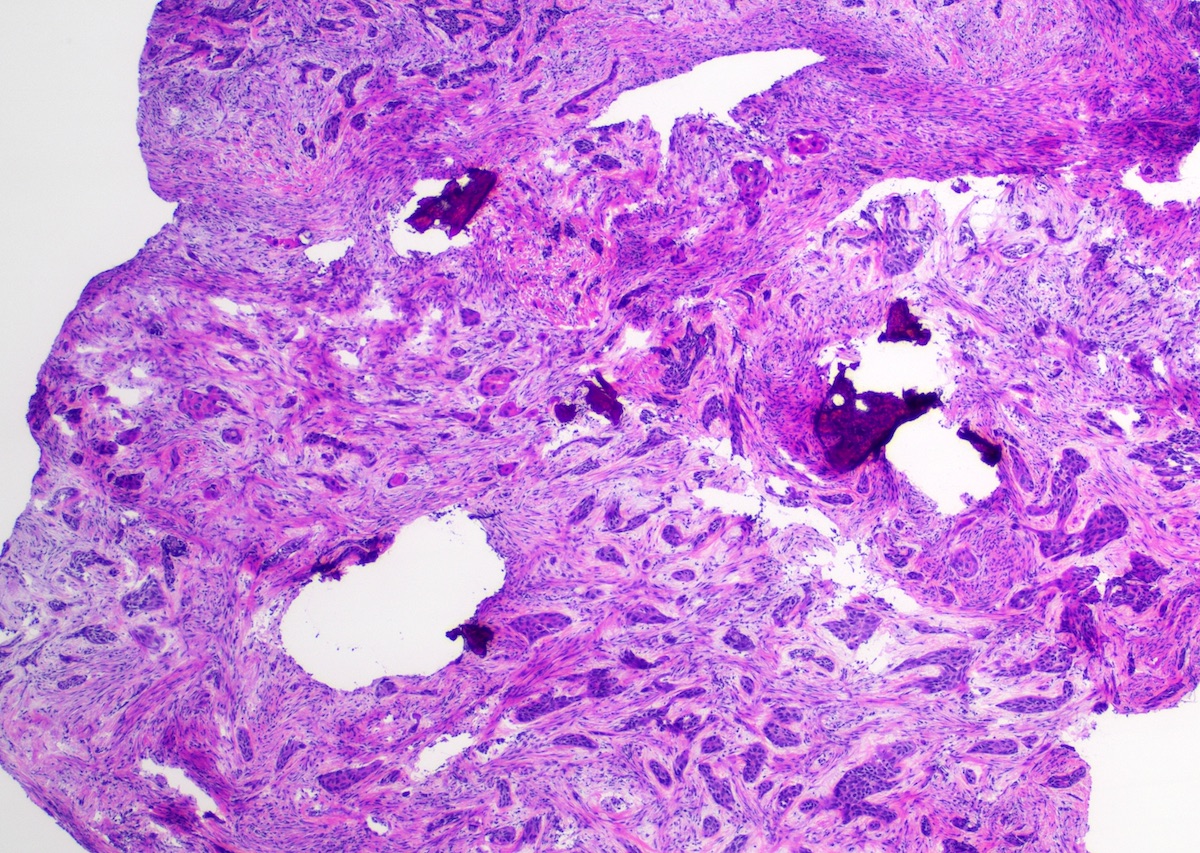
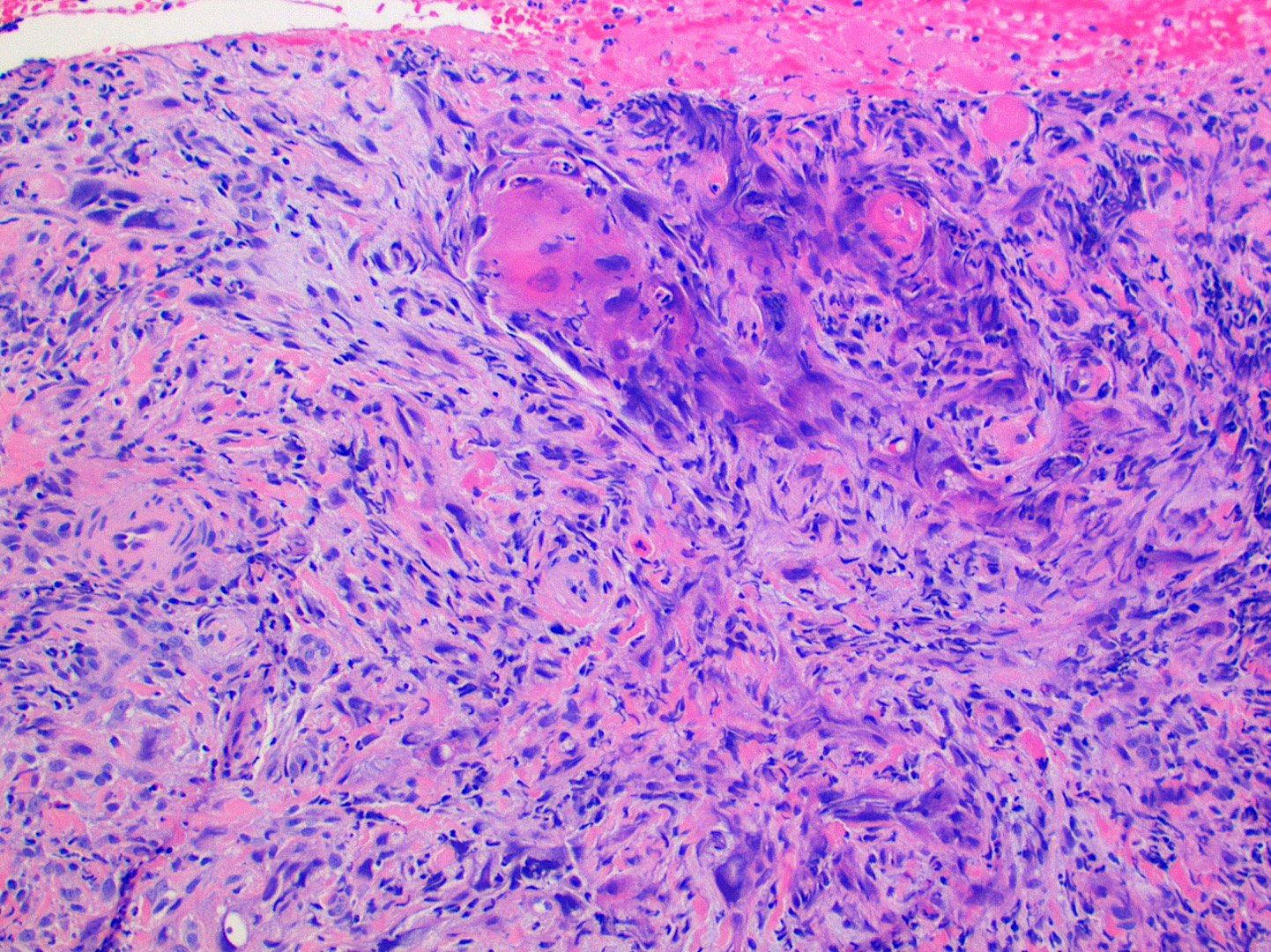
Microscopic (histologic) description
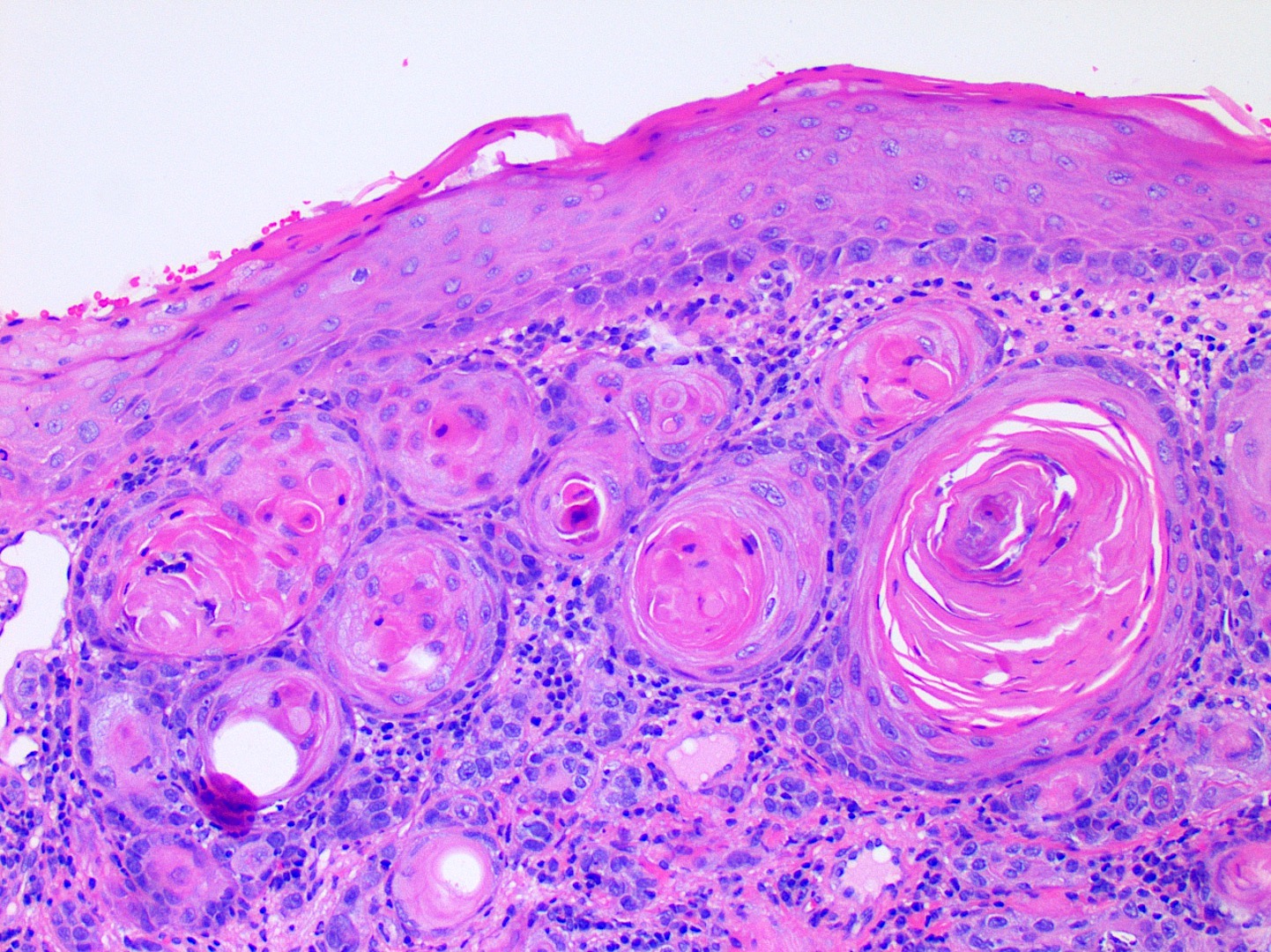
- Dysplastic stratified squamous epithelium that extends through the basement membrane and into the underlying fibrous connective tissue without attachment to the surface
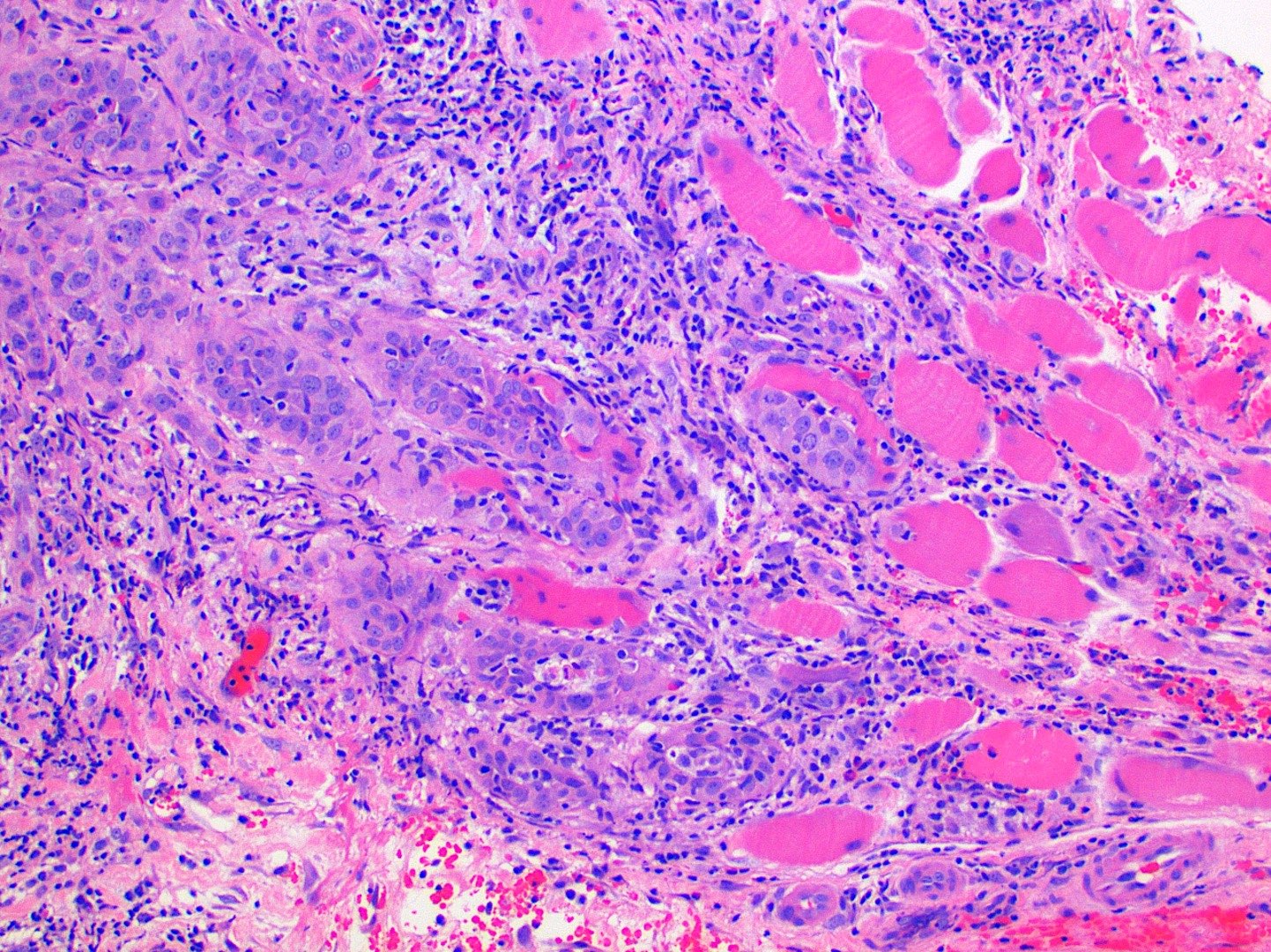
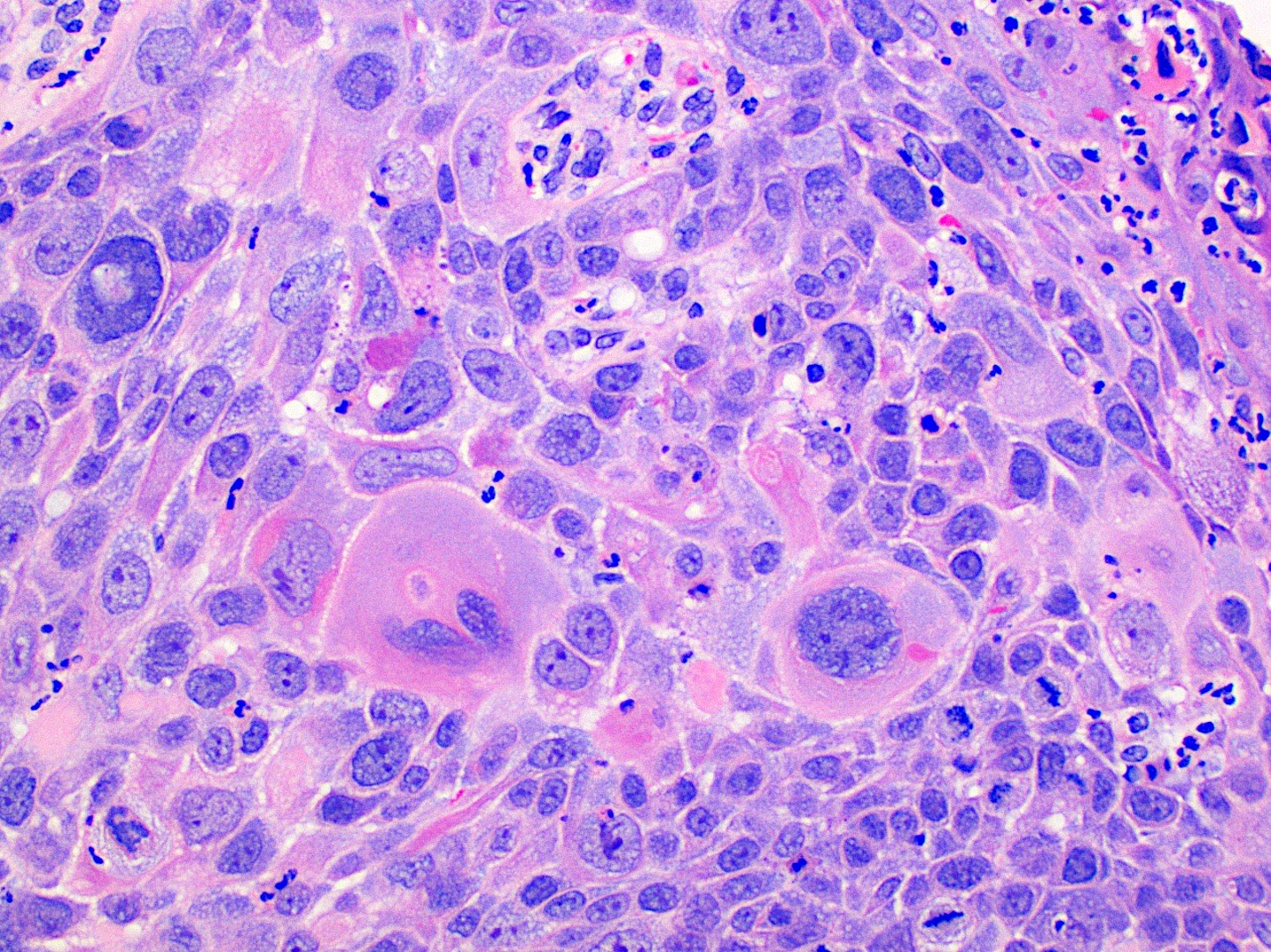
- Malignant epithelial cells show eosinophilic cytoplasm, hyperchromatic nuclei, pleomorphism, mitotic activity, individual cell keratinization and intercellular bridging
- Superficial or microinvasion can be used to describe the earliest moment of invasion
- Malignant epithelium can invade fibrous connective tissue in islands, cords or individual cells
- Keratin pearls of round, eosinophilic, concentric layers of keratin can be seen and are associated with well differentiated tumors
- 3 histologic grades for conventional squamous cell carcinoma include well, moderately and poorly differentiated based on amount of keratinization, mitotic activity, cellular and nuclear pleomorphism, pattern of invasion and host response (Arch Pathol Lab Med 2019;143:439)
- Histologic variants are listed below (Arch Pathol Lab Med 2019;143:439)
- Verrucous squamous cell carcinoma
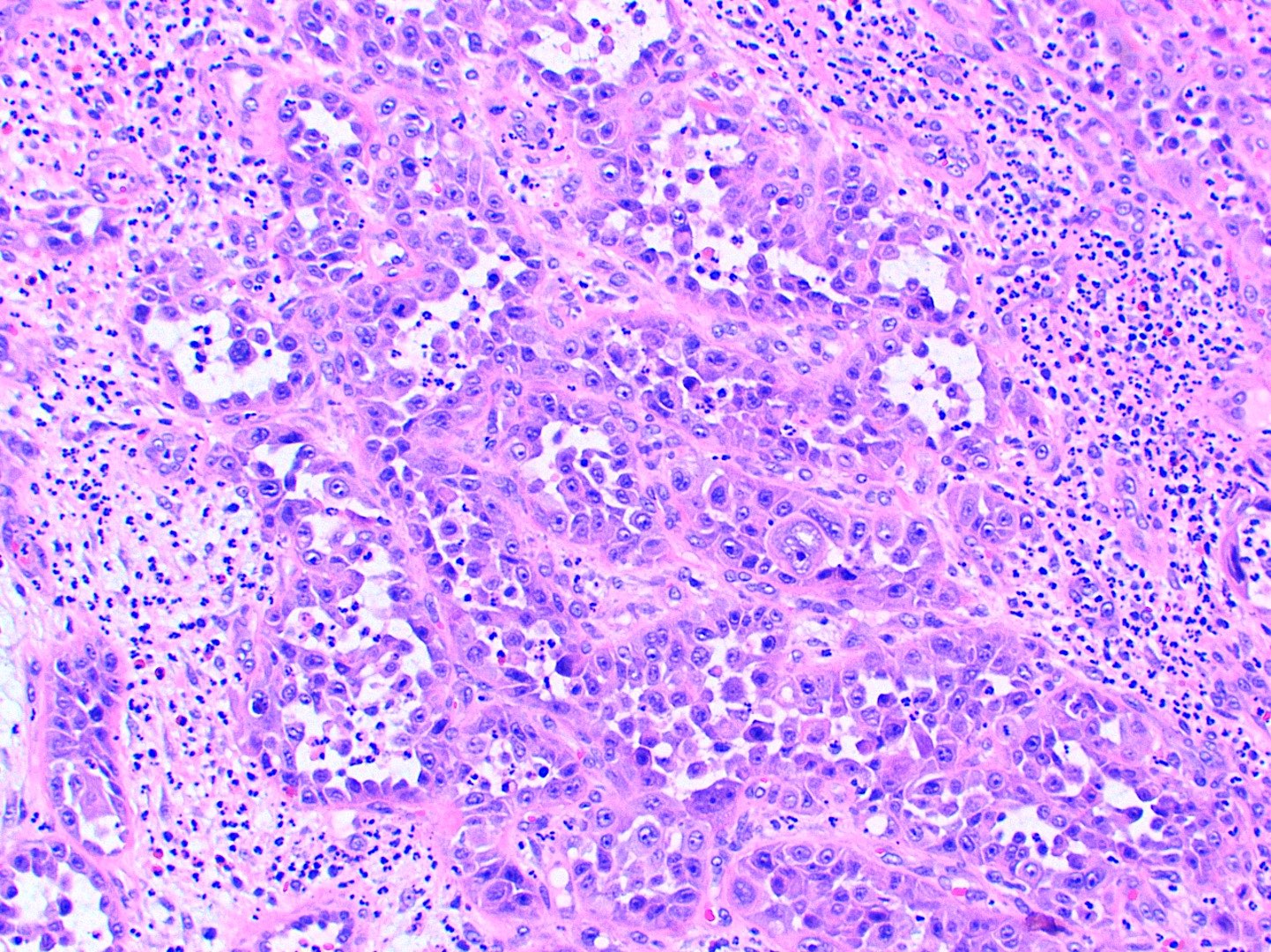
- Papillary squamous cell carcinoma
- Exophytic growth demonstrating multiple, thin keratinized papillary projections with fibrovascular cores or rounded, bulbous projections with nonkeratinized epithelium
- Malignant epithelial cells show an increased N:C ratio, prominent nucleoli and mitotic figures
- Obvious invasive components uncommon (Ann Diagn Pathol 2013;17:18)
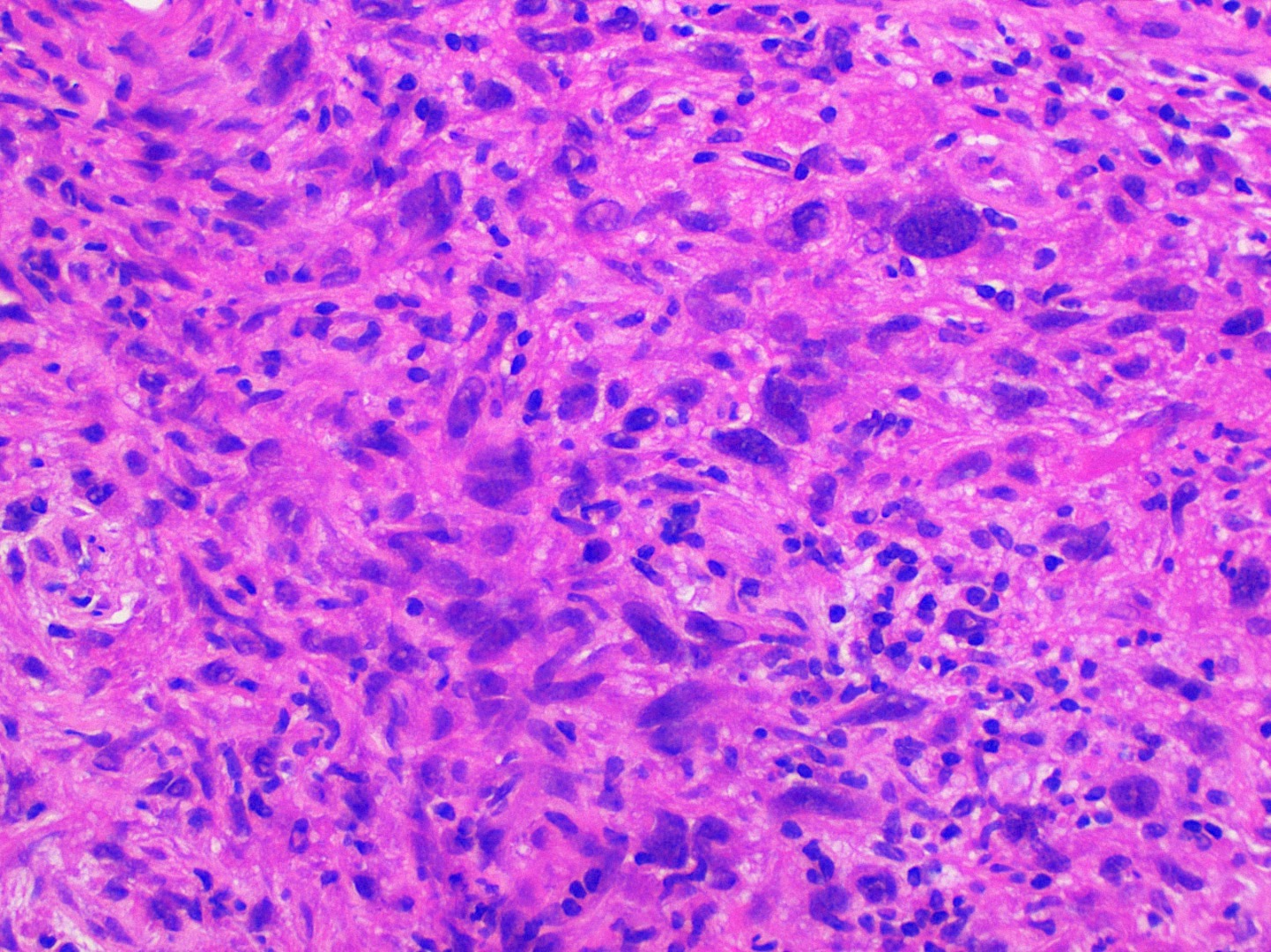
- Spindle cell squamous cell carcinoma
- Also called sarcomatoid
- Monoclonal, evolving from conventional squamous carcinoma with dedifferentiation (Head Neck Pathol 2010;4:265)
- Often polypoid configuration on biopsy; tumor may be ulcerated
- Overlying epithelium may show carcinoma in situ or dysplasia with elongation and spindling of the basal epithelial cells
- Nest of moderately or poorly differentiated conventional squamous cell carcinoma may be intricately mixed sarcomatoid component
- High mitotic count with bizarre, atypical mitotic figures
- Dense and eosinophilic cytoplasm
- Cells can be arranged in various patterns with variable amount of intervening matrix, which can mimic mesenchymal malignancies
- Metaplastic mesenchymal elements such as bone or cartilage not identified
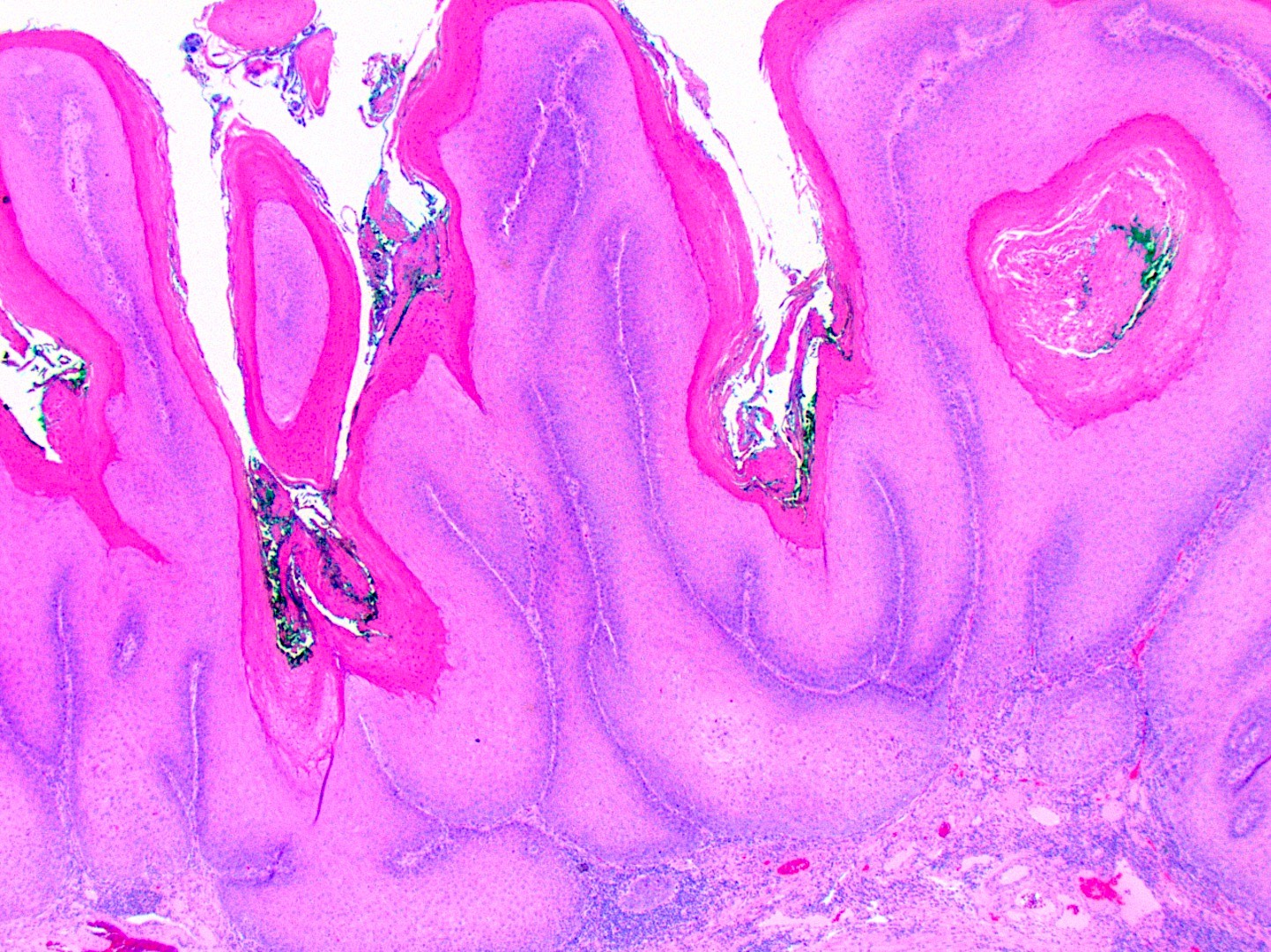
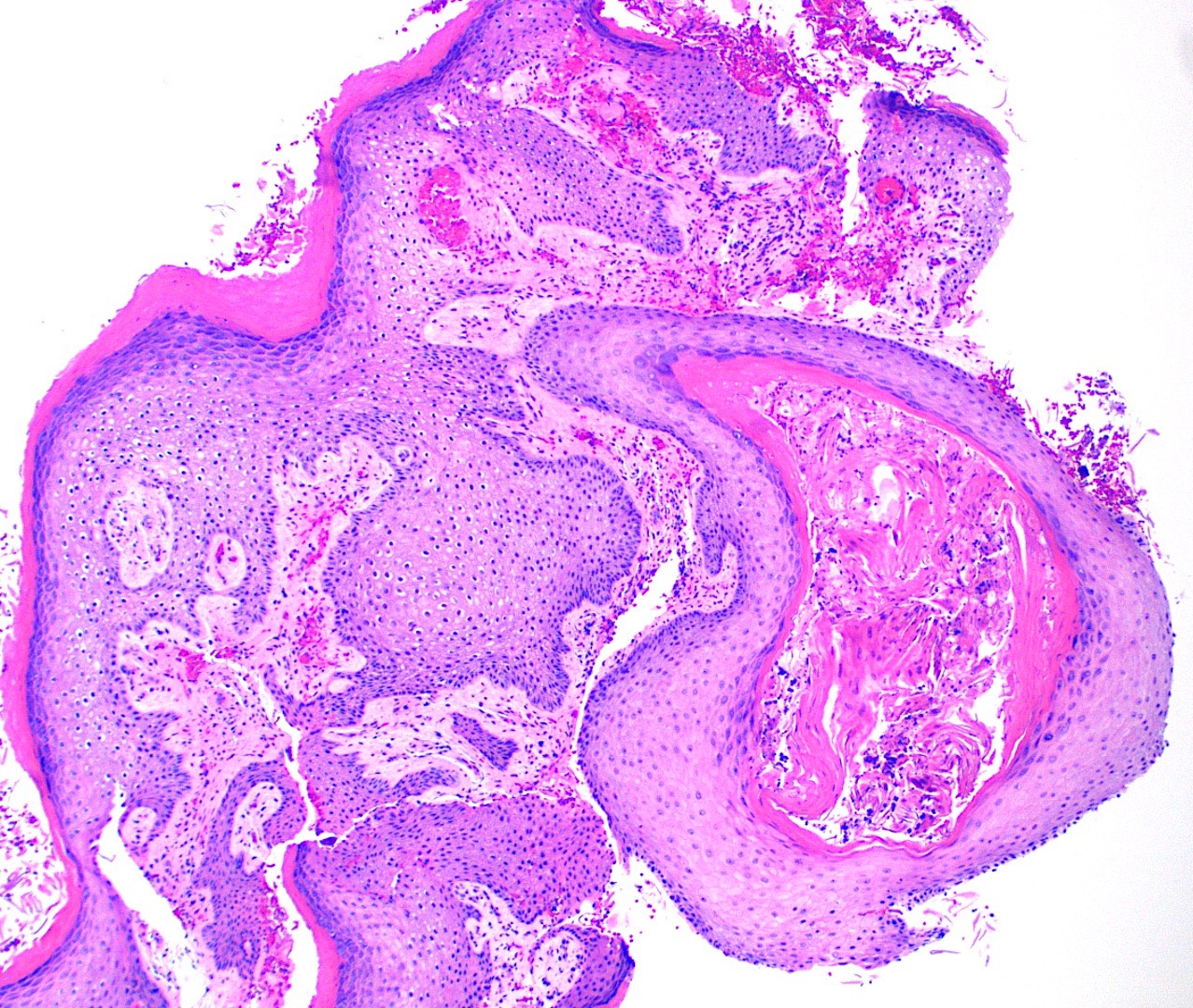
- Carcinoma cuniculatum
- Well differentiated squamous epithelium with minimal to no cytologic atypia
- Unique deeply infiltrative, large sized, branching, keratin filled cavities, resembling rabbit burrows (Head Neck Pathol 2022;16:213)
- Lymphocytic infiltrate surrounding epithelial tunnels and intraepithelial neutrophilic microabscesses
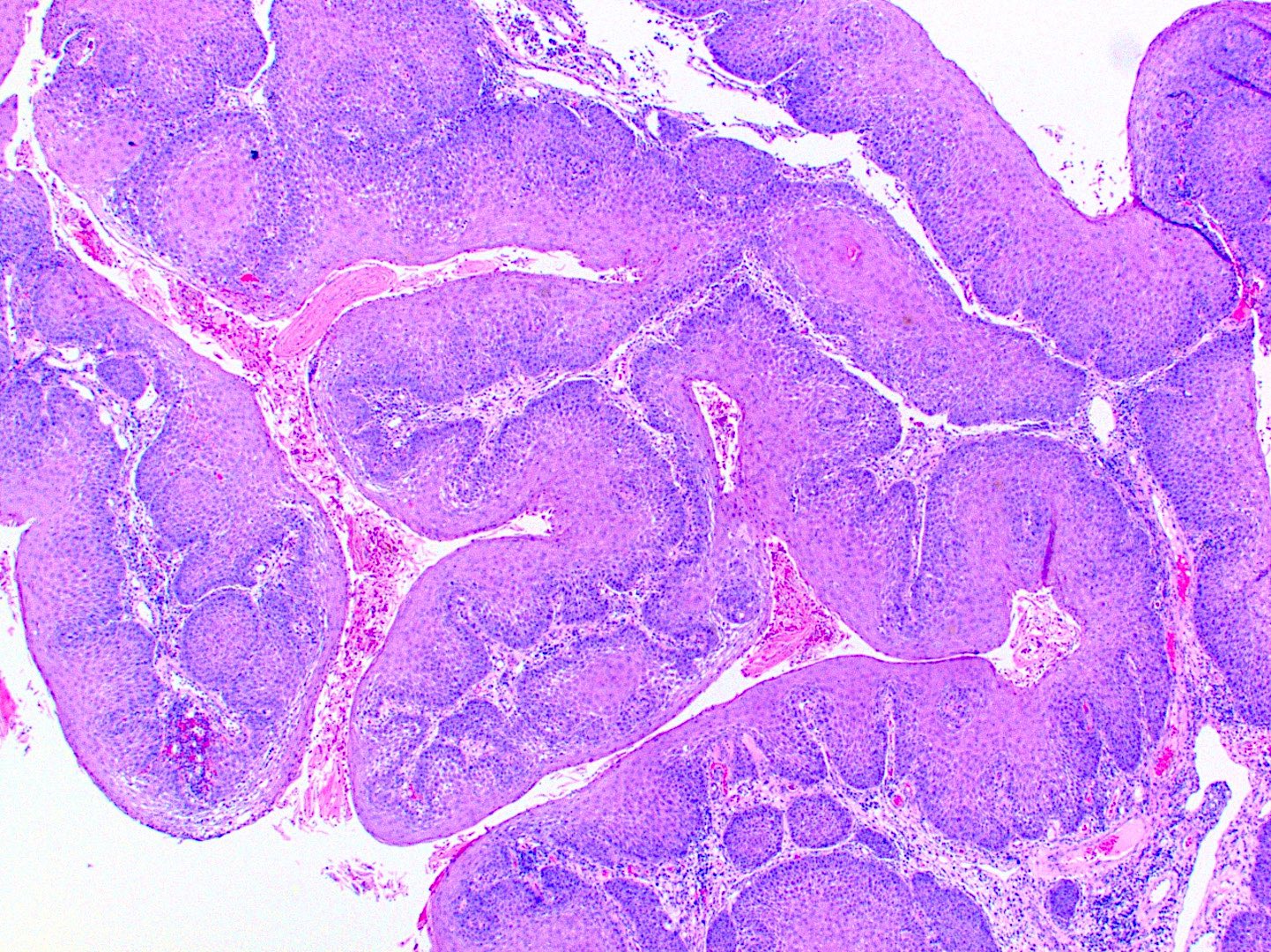
- Basaloid squamous cell carcinoma
- Lobules, nests or cribriform patterns of small basaloid cells with peripheral palisading and a thick basement membrane
- Cells have minimal cytoplasm, are moderately pleomorphic with hyperchromatic nuclei and often abruptly transition to squamous epithelium
- Single cell necrosis and comedonecrosis are common; often contiguous with carcinoma in situ in surface epithelium
- Frequent mitotic activity, stroma is often hyalinized or myxoid; variable pseudoglandular spaces resembling adenoid cystic carcinoma
- Rarely has a spindle cell component (Arch Pathol Lab Med 1995;119:181)
- Acantholytic squamous cell carcinoma
- Pseudoglandular structures, dyskeratotic cells and prominent acantholysis within tumor islands (Head Neck Pathol 2022;16:388)
- Adenosquamous cell carcinoma
- Distinct squamous and glandular differentiation in close proximity with blending and intermixing
- Typically presents as a superficial squamous cell carcinoma transitioning to a deeper adenocarcinoma (Head Neck Pathol 2018;12:576)
- Lymphoepithelial carcinoma
- Undifferentiated squamous cell carcinoma associated with a prominent, nonneoplastic lymphoplasmacytic cell infiltrate (Head Neck Pathol 2020;14:1001)
- Definitive squamous differentiation may be present but is usually limited, while a basaloid morphology can be identified (Head Neck Pathol 2012;6:445)
- Epstein-Barr virus (EBV) associated
- Morphologically indistinguishable from undifferentiated nasopharyngeal carcinoma (Head Neck Pathol 2020;14:1001)
- Although more often seen in salivary gland neoplasms and odontogenic tumors, oral squamous cell carcinoma may rarely show clear cell change (Cureus 2022;14:e25057)
- American Joint Committee on Cancer (AJCC) 8th edition is currently used for staging (see Staging - oral cavity)
- College of American Pathologists (CAP) protocol including TNM (CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 2 February 2024])
- Data set elements: operative procedure, specimens submitted, tumor dimensions, histologic tumor type, histologic tumor grade, pattern of invasive front, bone invasion, perineural invasion, lymphovascular invasion, margin status, pathologic staging (Arch Pathol Lab Med 2019;143:439)
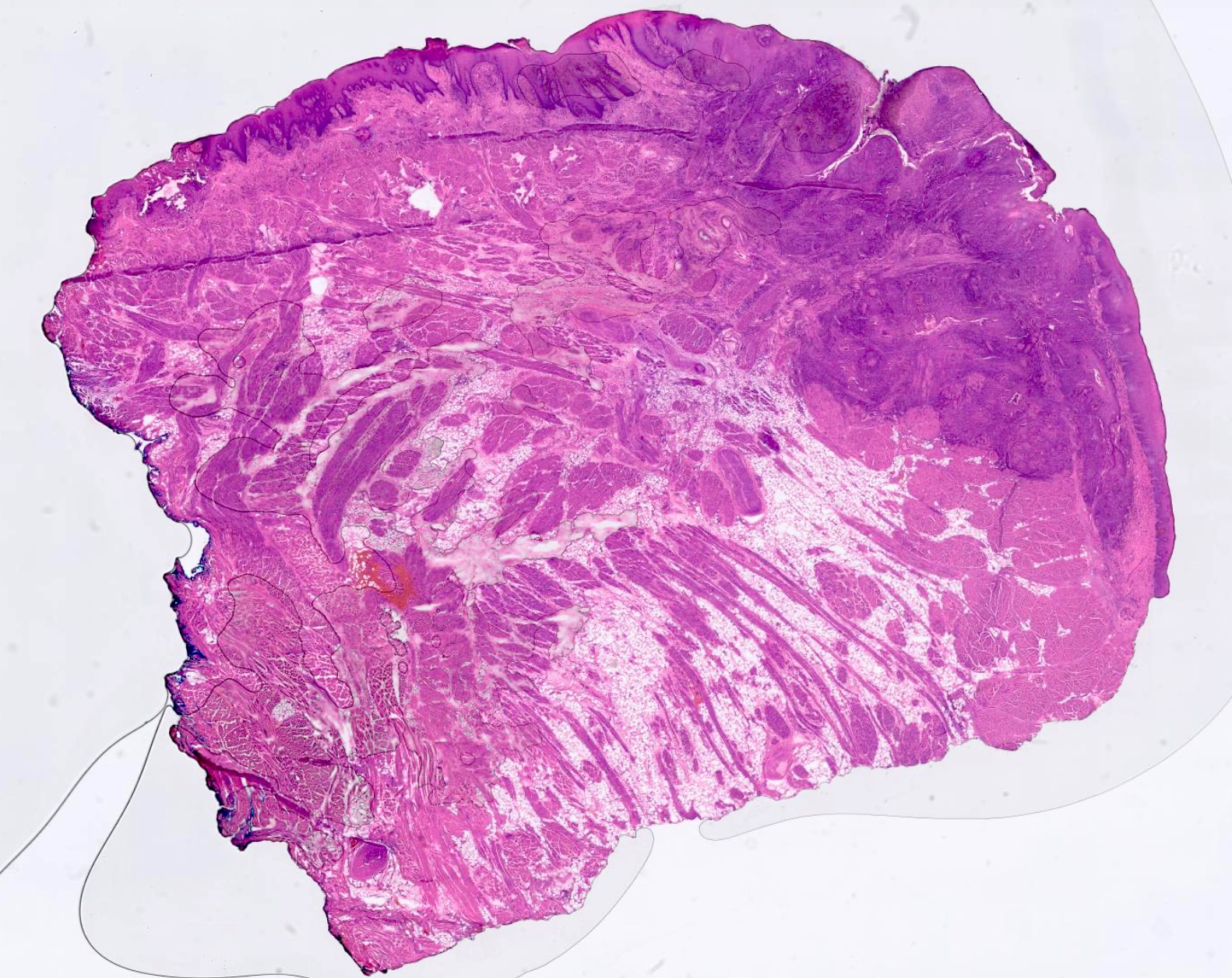
Microscopic (histologic) images
Contributed by Kathleen Higgins, D.D.S., M.S., Duane Schafer, D.D.S., M.S. and Sarah Glass, D.D.S.
Cytology description
- Cytology is not routinely recommended for evaluation of intraoral lesions suspicious for malignancy (J Am Dent Assoc 2017;148:712)
- Fine needle aspiration can identify regional spread to cervical lymph nodes
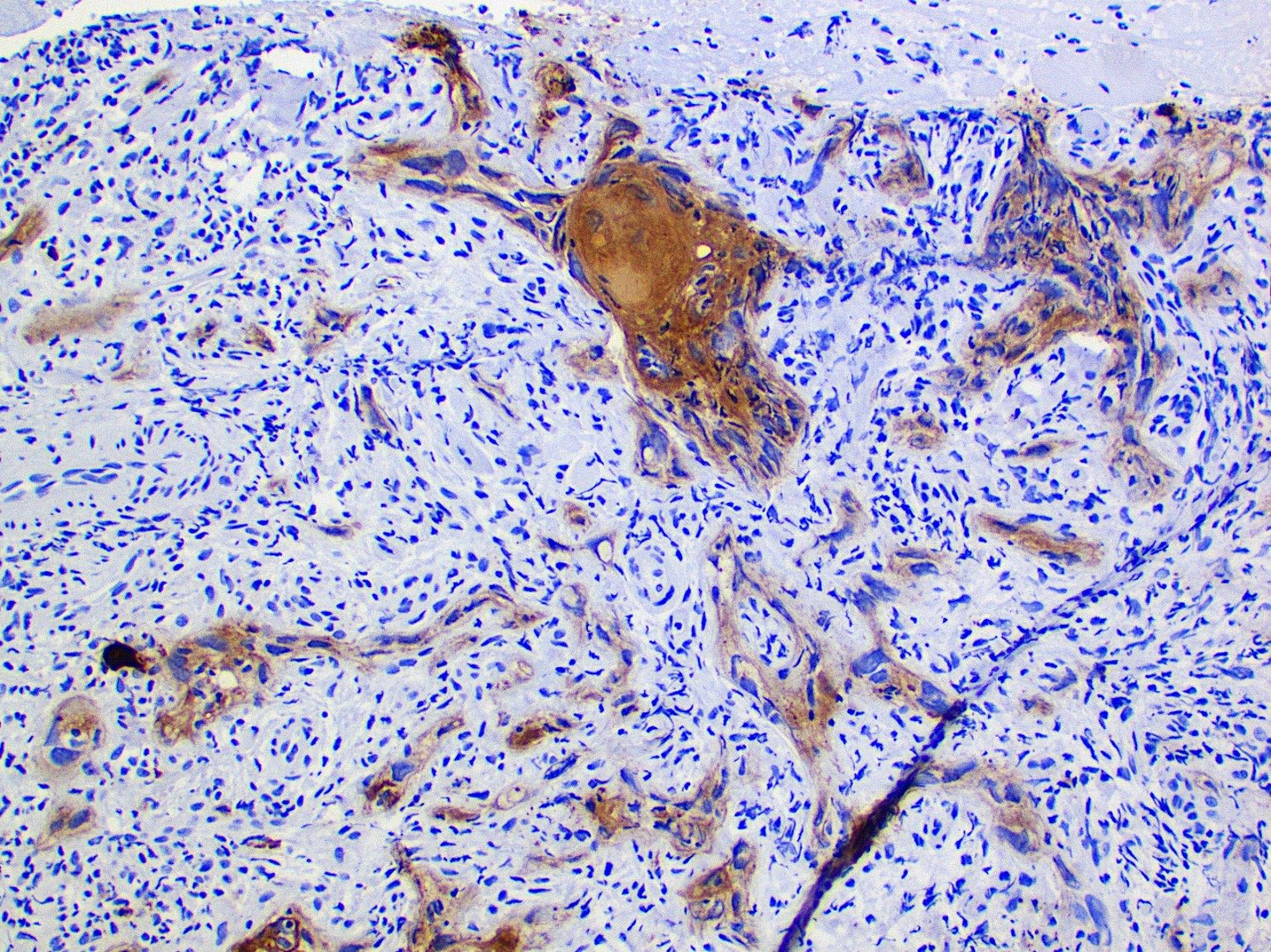
Positive stains
- Cytokeratin stains are positive: AE1 / AE3, CK5/6, p63, p40 (Arch Pathol Lab Med 2019;143:439)
- This can be helpful to support epithelial origin in poorly differentiated tumors
Negative stains
- Pathologists should not routinely perform high risk HPV testing on patients with nonoropharyngeal primary head and neck tumors (Arch Pathol Lab Med 2018;142:559)
Molecular / cytogenetics description
- Due to advances in targeted therapy, some centers are evaluating the mutational profiles of tumors (Nat Rev Dis Primers 2020;6:92)
Sample pathology report
- Right lateral tongue, incisional biopsy:
- Squamous cell carcinoma, well differentiated (see comment)
- Comment: Tumor islands are present at all surgical margins. Depth of invasion is at least 3 mm. Perineural and lymphovascular invasion are identified.
Differential diagnosis
- Pseudoepitheliomatous hyperplasia (Arch Otolaryngol Head Neck Surg 2003;129:127):
- Benign lesions in the oral cavity, such as granular cell tumor, may show pseudoepitheliomatous hyperplasia of the overlying squamous mucosa
- Granular cell tumors are S100 positive and occur on the dorsal tongue, an uncommon location for oral squamous cell carcinoma
- Mucoepidermoid carcinoma:
- May be difficult to distinguish high grade mucoepidermoid carcinoma from squamous cell carcinoma, adenosquamous variant
- High grade tumors may show predominantly squamous and intermediate cells with infrequent mucous cells
- Basaloid salivary gland tumors (Semin Diagn Pathol 2022;39:17):
- Oral malignant melanoma:
- Epithelioid sarcoma (Ann Otol Rhinol Laryngol 2021;130:416):
- Epithelioid sarcoma may express epithelial markers but most importantly does not express INI1
- Angiosarcoma (Head Face Med 2008;4:17):
- May be difficult to distinguish angiosarcoma from squamous cell carcinoma, acantholytic variant
- Expresses endothelial cell markers such as FLI1
- Metastatic squamous cell carcinoma to the oral cavity:
- Metastases may involve the soft tissue or bone
- First manifestation of disease in 25 - 30% of patients (Head Neck Pathol 2022;16:802)
- Histopathology is variable
- Patient history can be helpful, especially the ability to compare histopathology of known primary with current specimen
- Overlying mucosa uninvolved with lack of overt surface dysplasia
- Neuroepithelial structures, including the juxtaoral organ of Chievitz:
- Avoid misinterpretation as carcinoma showing neural invasion (Head Neck Pathol 2020;14:876)
- Located lingual to the mandible, buccal to the mandible and within the posterior tongue
- Smalls islands of squamoid epithelium in close association with small nerves or the taste buds
- Absence of keratinization, cytological atypia and mitotic activity
Additional references
Practice question #1
Practice answer #1
D. Squamous cell carcinoma. The histopathologic image shows well differentiated malignant squamous cells that have broken through the basement membrane and are invading the underlying connective tissue. Answer A is incorrect because the proliferation of abnormal squamous cells is not confined to the epithelium as seen in epithelial dysplasia. Answer B is incorrect because granular cells are not present in the connective tissue. Granular cell tumors may show pseudoepitheliomatous hyperplasia, which can be mistaken for squamous cell carcinoma. Answer C is incorrect because mucous cells and intermediate cells are not seen.
Comment Here
Reference: SCC-general
Comment Here
Reference: SCC-general
Practice question #2
Which oral squamous cell carcinoma histologic variant is the most likely to show minimal to no cytologic atypia?
- Adenosquamous cell carcinoma
- Basaloid squamous cell carcinoma
- Carcinoma cuniculatum
- Spindle cell squamous cell carcinoma
Practice answer #2
C. Carcinoma cuniculatum. This histologic variant shows minimal to no cytologic atypia. Architecturally, the tumor is described as resembling rabbit burrows. Answer B is incorrect because basaloid squamous cell carcinoma frequently demonstrates mitotic activity, pleomorphic nuclei and single cell necrosis. Answer D is incorrect because spindle cell squamous cell carcinoma frequently demonstrates bizarre, atypical mitotic figures. Answer A is incorrect because adenosquamous cell carcinoma typically displays classic features of both squamous cell carcinoma and adenocarcinoma.
Comment Here
Reference: SCC-general
Comment Here
Reference: SCC-general