Oral cavity & oropharynx
General
Staging-oral cavity
Last author update: 26 September 2018
Last staff update: 7 September 2022
Copyright: 2002-2024, PathologyOutlines.com, Inc.
PubMed Search: Staging oral cavity
Page views in 2023: 14,408
Page views in 2024 to date: 4,905
Cite this page: Magliocca KR. Staging-oral cavity. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavitytnm.html. Accessed April 23rd, 2024.
Definition / general
- Staging of definitive resections for carcinoma (squamous cell carcinoma, neuroendocrine carcinoma and minor salivary gland carcinoma) of the oral cavity should use this system (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- Oral cavity extends from the portion of the lip that contacts the opposed lip (wet mucosa) to the junction of the hard and soft palate above to the line of circumvallate papillae below and to the anterior tonsillar pillars laterally (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- Staging system name "oral cavity" reflects the focus on all of oral cavity, which includes mucosa of lip but not the external (dry) lip
- Staging protocols, such as those of CAP, are to document procedure, tumor site, tumor laterality, tumor focality, tumor size, histologic type, histologic grade where applicable, margin status, lymphovascular invasion, perineural invasion, regional lymph node findings and summarize these pathologic findings using TNM system (CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- See also Head and neck staging features
Terminology
- Anatomic boundaries and primary site(s): the oral cavity extends from the portion of the lip that contacts the opposed lip (wet mucosa) to the junction of the hard and soft palate above, to the line of circumvallate papillae below and to the anterior tonsillar pillars laterally; it is additionally divided into multiple specific sites listed below (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020], see figure 1 in Diagrams / tables)
- Mucosal lip:
- Begins at the junction of the wet and dry mucosa of the lip (the anterior border of the portion of the lip that comes into contact with the opposed lip) and extends posteriorly into the oral cavity to the attached gingiva of the alveolar ridge
- Dry vermilion lip and vermilion border are staged using the chapter on cutaneous carcinoma of the head and neck; this is a change from past AJCC editions where the dry vermilion was included in the lip and oral cavity chapter
- Buccal mucosa:
- Includes all the mucous membrane lining of the inner surface of the cheeks and lips from the line of contact of the opposing lips to the line of attachment of mucosa of the alveolar ridge (upper and lower) and pterygomandibular raphe
- Lower alveolar ridge:
- Refers to the mucosa overlying the alveolar process of the mandible, which extends from the line of attachment of mucosa in the lower gingivobuccal sulcus to the line of attachment of free mucosa of the floor of the mouth
- Posteriorly, it extends to the ascending ramus of the mandible
- Upper alveolar ridge:
- Refers to the mucosa overlying the alveolar process of the maxilla, which extends from the line of attachment of mucosa in the upper gingivobuccal sulcus to the junction of the hard palate
- Its posterior margin is the upper end of the pterygopalatine arch
- Retromolar gingiva (retromolar trigone):
- Attached mucosa overlying the ascending ramus of the mandible from the level of the posterior surface of the last lower molar tooth to the apex superiorly, adjacent to the tuberosity of the maxilla
- Floor of the mouth:
- Crescentic surface overlying the mylohyoid and hyoglossus muscles, extending from the inner surface of the lower alveolar ridge to the undersurface of the tongue
- Its posterior boundary is the base of the anterior pillar of the tonsil
- It is divided into 2 sides by the frenulum of the tongue and harbors the ostia of the submandibular and sublingual salivary glands
- Hard palate:
- Semilunar area between the upper alveolar ridge and the mucous membrane covering the palatine process of the maxillary palatine bones
- It extends from the inner surface of the superior alveolar ridge to the posterior edge of the palatine bone
- Anterior two - thirds of the tongue (oral tongue):
- Freely mobile portion of the tongue that extends anteriorly from the line of circumvallate papillae to the undersurface of the tongue at the junction with the floor of the mouth
- It is composed of 4 areas: the tip, the lateral borders, the dorsum and the undersurface (nonvillous ventral surface of the tongue)
- Undersurface of the tongue is considered a separate category by the World Health Organization (WHO)
- Tumor thickness (TT) versus depth of invasion (DOI) (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]):
- Tumor thickness is usually measured from the mucosal surface of the tumor to the deepest point of tissue invasion in a perpendicular fashion with a measuring instrument
- DOI is measured from the basement membrane of an adjacent normal to the deepest point of invasion of the tumor
- DOI assesses the invasiveness of a carcinoma, regardless of any exophytic component
- It is measured by first finding the "horizon" of the basement membrane of the adjacent squamous mucosa
- Perpendicular "plumb line" is established from this horizon to the deepest point of tumor invasion, which represents DOI
- DOI is recorded in millimeters
- See figures 2A and 2B in Microscopic (histologic) images
- Extrinsic tongue muscle (ETM) invasion (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]):
- No longer used as a component of pT4 staging because this is a feature of DOI
- No longer a staging criterion for T4 designation in oral cavity because depth of invasion supersedes it and extrinsic muscle invasion is difficult to assess (both clinically and pathologically)
- Surgical margins (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]):
- Definition of a positive margin is somewhat controversial given the varied results from prior studies
- However, overall, several studies support the definition of a positive margin to be invasive carcinoma or carcinoma in situ / high grade dysplasia present at margins (microscopic cut through of tumor)
- Furthermore, reporting of surgical margins should also include information regarding the distance of invasive carcinoma, carcinoma in situ or high grade dysplasia (moderate to severe) from the surgical margin
- Tumor bed versus specimen margins:
- Regarding what actually represents the relevant margin status, it becomes increasingly clear that margins obtained from the main resection specimen are of more reliable prognostic value
- Clinical value of tumor bed margins (i.e. margins taken separately) is often undermined by their uncertain origin with respect to the main resection, infrequent orientation as to the new margin surface and fragmentation
- Nonetheless, tumor bed margin status is still utilized in various practice settings for patient management
- However, the challenge for pathologists is to arrive at a "final" margin status, integrating both tumor bed and specimen margin status
- As it is in multipart resections, the pathologist's ability to confidently establish the relationship between the main resected specimen and additional, separately submitted parts and to assess the adequacy of excision is compromised
- To optimize reporting, both specimen margin and tumor bed margin status should thus be reported separately
- "Final" margin status then becomes a multidisciplinary integration of these findings
- For instance, in cases with differing margin statuses (i.e. resection specimen margin positive, corresponding tumor bed margin negative), the small size and lack of orientation of the tumor bed margin may preclude a reliable conversion to final negative margin
- Conversely, in some cases the tumor bed specimen (e.g. revision of margin) may be a reliable indicator of a true final margin
- This is a judgment call that requires close interaction between the surgeon and pathologist but generally, the following basic requirements are met:
- Tumor bed margins are quite large (i.e. thick enough to be readily processed as radial margins and large enough to match the corresponding aspect of the main specimen margin)
- Are oriented as to the new true margin surface (by ink or stitch)
- Physical relationship between the main resection specimen and additional tumor bed margins is confirmed by pathologist and surgeon (usually through unequivocal labeling and even fitting the tumor bed margin to the main specimen)
- In such a case, the tumor bed margin could be considered a final margin
- Worst pattern of invasion (WPOI) (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020]):
- Validated outcome predictor for oral cavity squamous carcinoma patients in multivariate analysis
- To simplify prognostication and enhance adaptation, the only cutpoint recommended for assessment is whether or not WPOI-5 is present
- WPOI-5 is defined as tumor dispersion of ≥ 1 mm between tumor satellites
- Tumor dispersion is assessed at the advancing tumor edge
- To some, WPOI can be viewed as redundant and only optional for reporting purposes, as extratumoral perineural invasion or extratumoral lymphovascular invasion also count as WPOI-5
ICD coding
- C00.3: Mucosa of upper lip
- C00.4: Mucosa of lower lip
- C00.5: Mucosa of lip, NOS
- C00.8: Overlapping lesion of lip
- C00.9: Lip, NOS
- C02.0: Dorsal surface of tongue, NOS
- C02.1: Border of tongue
- C02.2: Ventral surface of tongue, NOS
- C02.3: Anterior 2/3 of tongue, NOS
- C02.8: Overlapping lesion of tongue
- C02.9: Tongue, NOS
- C03.0: Upper gum
- C03.1: Lower gum
- C03.9: Gum, NOS
- C04.0: Anterior floor of mouth
- C04.1: Lateral floor of mouth
- C04.8: Overlapping lesion of floor of mouth
- C04.9: Floor of mouth, NOS
- C05.0: Hard palate
- C05.8: Overlapping lesion of palate
- C05.9: Palate, NOS
- C06.0: Cheek mucosa
- C06.1: Vestibule of mouth
- C06.2: Retromolar area
- C06.8: Overlapping lesion of other and unspecified parts of mouth
- C06.9: Mouth, NOS
Primary tumor (pT)
- TX: Primary tumor cannot be assessed
- Tis: Carcinoma in situ
- T1: Tumor ≤ 2 cm with depth of invasion (DOI)* ≤ 5 mm
- T2: Tumor ≤ 2 cm with DOI* > 5 mm and ≤ 10 mm or tumor > 2 cm and ≤ 4 cm with DOI* ≤ 10 mm
- T3: Tumor > 2 cm and ≤ 4 cm with DOI* > 10 mm or tumor > 4 cm with DOI* ≤ 10 mm or any tumor
- T4: Moderately advanced or very advanced local disease
- T4a: Moderately advanced disease
- Tumor > 4 cm with DOI* > 10 mm or
- Tumor invades adjacent structures only (e.g. through cortical bone of the mandible or maxilla or involves the maxillary sinus or skin of the face)
- T4b: Very advanced disease
- Tumor invades masticator space, pterygoid plates or skull base or encases the internal carotid artery
Notes:
- *DOI is depth of invasion and not tumor thickness, see above Terminology section for definition
- Superficial erosion of bone / tooth socket alone by a gingival primary is not sufficient to classify a tumor as T4
Pathological regional lymph nodes (pN)
- NX: Regional lymph nodes cannot be assessed
- N0: No regional lymph node metastasis
- N1: Metastasis in a single ipsilateral lymph node, ≤ 3 cm in greatest dimension and extranodal extension (ENE)-
- N2: Metastasis in a single ipsilateral lymph node, ≤ 3 cm in greatest dimension and ENE+ or > 3 cm but ≤ 6 cm in greatest dimension and ENE-; or metastases in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-; or in bilateral or contralateral lymph nodes(s), none > 6 cm in greatest dimension and ENE-
- N2a: Metastasis in either
- Single ipsilateral lymph node that is ≤ 3 cm and ENE+ or
- Single ipsilateral lymph node that is > 3 cm but ≤ 6 cm in greatest dimension and ENE-
- N2b: Metastasis in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-
- N2c: Metastasis in bilateral or contralateral lymph node(s), none > 6 cm in greatest dimension and ENE-
- N3: Metastasis in a lymph node > 6 cm in greatest dimension and ENE-; or in a single ipsilateral node > 3 cm in greatest dimension and ENE+; or multiple ipsilateral, contralateral or bilateral nodes, any with ENE+; or a single contralateral node of any size and ENE+
- N3a: Metastasis in a lymph node that is > 6 cm in greatest dimension and ENE-
- N3b: Metastasis in either
- Single ipsilateral lymph node, > 3 cm and ENE+ or
- Multiple ipsilateral, contralateral or bilateral lymph nodes, any with ENE+ or
- Single contralateral lymph node of any size and ENE+
Notes:
- Designation of "U" or "L" may be used for any N category to indicate metastasis above the lower border of the cricoid (U) or below the lower border of the cricoid (L)
- Per AJCC 8th edition, for pN, a selective neck dissection ordinarly will include 10+ lymph nodes and a comprehensive neck dissection (radical or modified radical neck dissection) ordinarily will include 15+ lymph nodes
- Negative pathologic examination of a smaller number of nodes still mandates a pN0 designation
- Midline nodes are considered ipsilateral nodes
AJCC prognostic stage grouping for oral cavity
| Stage 0:
| Tis
| N0
| M0
|
| Stage I:
| T1
| N0
| M0
|
| Stage II:
| T2
| N0
| M0
|
| Stage III:
| T3
| N0
| M0
|
|
| T1 - 3
| N1
| M0
|
| Stage IVA:
| T4a
| N0 - 1
| M0
|
|
| T1 - 4a
| N2
| M0
|
| Stage IVB:
| Any T
| N3
| M0
|
|
| T4b
| Any N
| M0
|
| Stage IVC:
| Any T
| Any N
| M1
|
Registry data collection variables
- Extranodal extension (ENE) clinical (present versus absent)
- ENE pathological (present versus absent)
- Extent of microscopic ENE (distance of extension from the native lymph node capsule to the farthest point of invasion in extranodal tissue)
- Perineural invasion
- Lymphovascular invasion
- p16 / HPV status
- Performance status
- Tobacco use and pack year
- Alcohol use
- Depression diagnosis
- Depth of invasion (mm)
- Margin status (grossly involved, microscopic involvement)
- Distance of tumor (or moderate / severe dysplasia) from closest margin
- Distance of moderate / severe dysplasia from closest margin
- Worst pattern of invasion - 5
Histologic grade
- Gx: Cannot be assessed
- G1: Well differentiated
- G2: Moderately differentiated
- G3: Poorly differentiated
Notes:
- For histologic types of carcinomas that are amenable to grading, 3 histologic grades are suggested, as shown below (AJCC: Cancer Staging [Accessed 21 September 2018], CAP: Protocol for the Examination of Specimens from Patients with Cancers of the Lip and Oral Cavity [Accessed 29 December 2020])
- For conventional squamous cell carcinoma, histologic grading as a whole does not perform well as a prognosticator
- Nonetheless, it should be recorded when applicable, as it is a basic tumor characteristic
- Selecting either the most prevalent grade or the highest grade for this synoptic protocol is acceptable
- Variants of squamous cell carcinoma (i.e. verrucous, basaloid, etc.) have an intrinsic biologic potential and currently do not appear to require grading
- Histologic (microscopic) grading of salivary gland carcinomas has been shown to be an independent predictor of behavior and plays a role in optimizing therapy
- However, most salivary gland carcinoma types have an intrinsic biologic behavior and attempted application of a universal grading scheme is merely a crude surrogate
- Thus a generic grading scheme is no longer recommended for salivary gland carcinomas
- Carcinoma types for which grading systems exist and are relevant are incorporated into histologic type
- 3 major categories that are amenable to grading include adenoid cystic carcinoma, mucoepidermoid carcinoma and adenocarcinoma, not otherwise specified
- In some carcinomas, histologic grading may be based on growth pattern, such as in adenoid cystic carcinoma, for which a histologic high grade variant has been recognized based on the percentage of solid growth
- Those adenoid cystic carcinomas showing ≥ 30% of solid growth pattern are considered to be histologically high grade carcinomas
- Histologic grading of mucoepidermoid carcinoma includes a combination of growth pattern characteristics (e.g. cystic, solid, neurotropism) and cytomorphologic findings (e.g. anaplasia, mitoses, necrosis)
- Adenocarcinomas, not otherwise specified do not have a formalized grading scheme and are graded intuitively based on cytomorphologic features
Histopathologic type
- Carcinoma of the oral cavity
- Squamous cell carcinoma (conventional)
- Verrucous squamous cell carcinoma
- Papillary squamous cell carcinoma
- Spindle cell squamous cell carcinoma
- Acantholytic squamous cell carcinoma
- Lymphoepithelial carcinoma
- Basaloid squamous carcinoma
- Adenosquamous carcinoma
- Carcinoma cuniculatum
- Carcinoma of minor salivary gland
- Acinic cell
- Adenoid cystic
- Adenocarcinoma, NOS
- Basal cell adenocarcinoma
- Carcinoma ex pleomorphic adenoma
- Carcinoma type cannot be determined
- Carcinosarcoma
- Clear cell adenocarcinoma
- Cystadenocarcinoma
- Epithelial myoepithelial carcinoma
- Mammary analogue secretory carcinoma
- Mucoepidermoid carcinoma
- Mucinous carcinoma
- Myoepithelial carcinoma
- Oncocytic carcinoma
- Polymorphous adenocarcinoma
- Salivary duct carcinoma
- Neuroendocrine carcinoma
- Well differentiated neuroendocrine carcinoma (typical carcinoid tumor)
- Moderately differentiated neuroendocrine carcinoma (atypical carcinoid tumor)
- Poorly differentiated neuroendocrine carcinoma, small cell type
- Poorly differentiated neuroendocrine carcinoma, large cell type
- Combined (or composite) neuroendocrine carcinoma (specify types)
- Carcinoma type cannot be determined
- Mucosal melanoma
Diagrams / tables
Images hosted on other servers:

Figure 1
Microscopic (histologic) images
Images hosted on other servers:

Figure 2A

Figure 2B
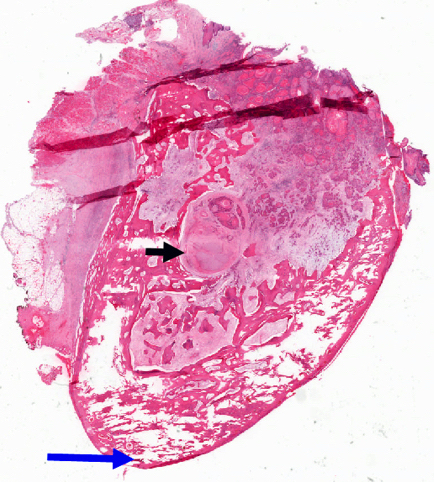
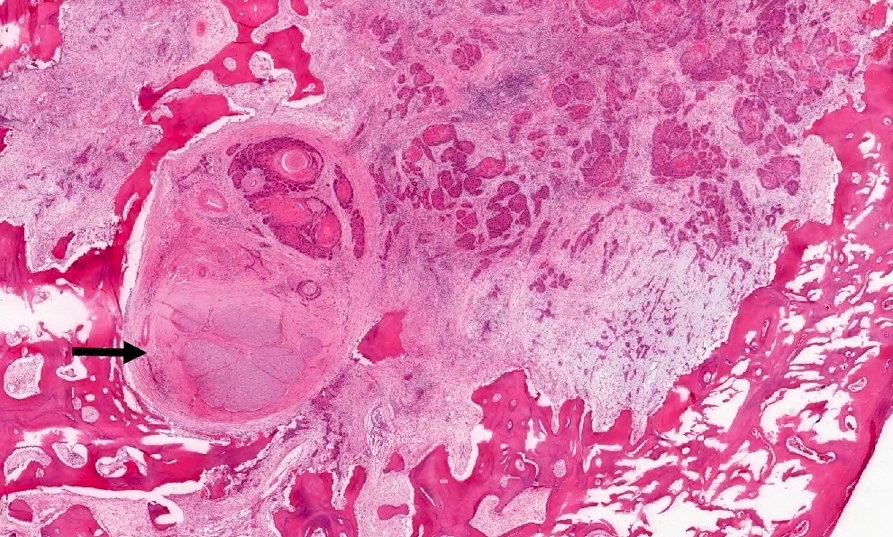
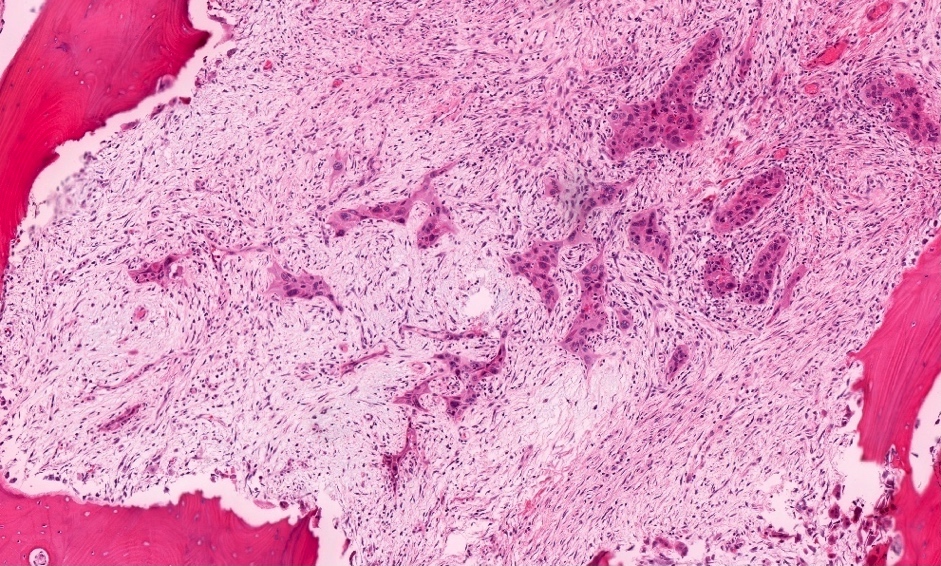
Board review style question #1
A 2.4 cm primary gingival carcinoma was resected in continuity with the underlying posterior mandible. Which of the T category criteria in the 8th edition AJCC staging guide is satisfied by the examination of the microscopic sections above?
- T1 by depth of invasion
- T2 by depth of invasion
- T3 by mandibular medullary bone invasion
- T4 by mandibular medullary bone invasion
Board review style answer #1
Back to top