Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Lucas E, Zheng W. Wolffian tumor / Female adnexal tumor of probable Wolffian origin. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorfatwo.html. Accessed September 9th, 2025.
Definition / general
- Adnexal tumor arising from remnants of Wolffian (mesonephric) duct
Essential features
- Adnexal tumor arising from mesonephric (Wolffian duct) remnants
- Heterogeneous histologic appearance
- Diagnosis based predominantly on the anatomical site and morphology
Terminology
- Wolffian tumor
- Female adnexal tumor of probable Wolffian origin (FATWO)
- Wolffian adnexal tumor (WAT)
- Wolffian adenoma
- Retiform Wolffian adenoma
- Mesonephric tumor, NOS
ICD coding
- ICD-O: 9110/1 - mesonephric tumor, NOS
- ICD-11: 2F33.Y & XH2WJ5 - benign neoplasm of other or unspecified female genital organs & Wolffian tumor
Epidemiology
- Rare, approximately 130 cases reported (Oncol Lett 2017;14:5167)
- Median age 50 years, range 15 - 87 years (Int J Surg Pathol 2008;16:222)
Sites
- Broad ligament (most common site) (Hum Pathol 1999;30:856)
- Ovaries (Am J Surg Pathol 1983;7:125)
- Mesosalpinx, fallopian tubes
- Paravaginal (Am J Clin Pathol 1994;101:275)
- Peritoneum
Pathophysiology
- Believed to originate from mesonephric (Wolffian) duct remnants
- Arises along the trajectory of the Wolffian duct: from the ovarian hilum, along mesosalpinx, broad ligament, lateral aspects of the uterus and cervix, to the outer third of the vagina (Hum Pathol 1999;30:856)
Etiology
- Unknown
Clinical features
- Adnexal mass with nonspecific symptoms or an incidental finding
- Complaints include lower abdominal pain / distention, pelvic mass, abnormal vaginal bleeding or ascites
- Most tumors are hormonally inert; rare tumors are hormonally active, causing endometrial hyperplasia (Gynecol Oncol 1995;59:304)
- Most tumors are unilateral; rarely bilateral
Diagnosis
- Tumor location
- Surgical specimen: gross and microscopic examination
Radiology description
- Well defined, encapsulated, lobulated or ovoid mass, often separate from ovaries, tubes and uterus
- May demonstrate solid and cystic areas
- Low signal intensity rim around the tumor on T2 weighted MRI images; might be a characteristic feature (J Obstet Gynaecol Res 2016;42:1046)
Prognostic factors
- Low malignant potential; most tumors behave in a benign fashion
- Recurrence or metastases occur in 11 - 20% of cases; median of 48 months to recurrence (range 13 - 96 months) (Gynecol Oncol 2002;86:225)
- Adverse prognostic factors: large size (> 10 cm), capsular invasion and rupture with tumor implants (Histopathology 2005;46:716)
- Aggressive behavior includes intra-abdominal spread, recurrence or distant metastasis, typically to the liver and lungs (Gynecol Oncol 2002;86:225)
- High cellularity, nuclear pleomorphism and high mitotic activity are associated with worse prognosis but tumors with minimal nuclear atypia and low mitotic rate may recur; no single feature is predictive of malignant behavior (Tohoku J Exp Med 1997;181:371)
Case reports
- 28 year old woman with left paratubal cyst (Gynecol Oncol Rep 2021;36:100726)
- 30 year old woman with an incidental ovarian mass (Gynecol Oncol Rep 2014;10:22)
- 37 year old woman with abdominal pain and adnexal mass (Oncol Lett 2017;13:3403)
- 50 year old woman with bilateral adnexal masses (Int J Gynecol Pathol 2018;37:331)
- 70 year old woman with an abdominal mass (Indian J Pathol Microbiol 2014;57:620)
- Series of 11 cases of FATWO (Arch Pathol Lab Med 2022;146:166)
- Series of 15 tumors of FATWO (Mod Pathol 2020;33:734)
Treatment
- Hysterectomy and bilateral salpingo-oophorectomy; tumor debulking
- Role of adjuvant chemotherapy or radiation therapy is unknown
- For recurrent / metastatic KIT (CD117) expressing tumors, tyrosine kinase inhibitor Gleevac (STI571) is a treatment option (Int J Gynecol Cancer 2004;14:546)
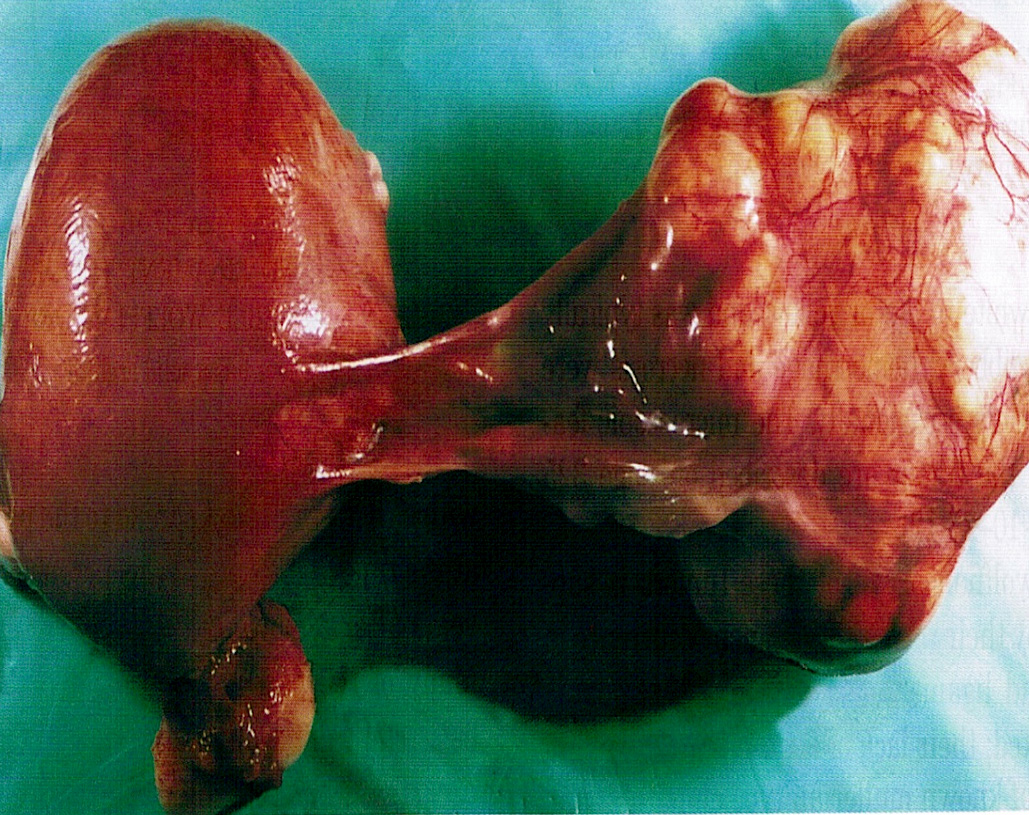
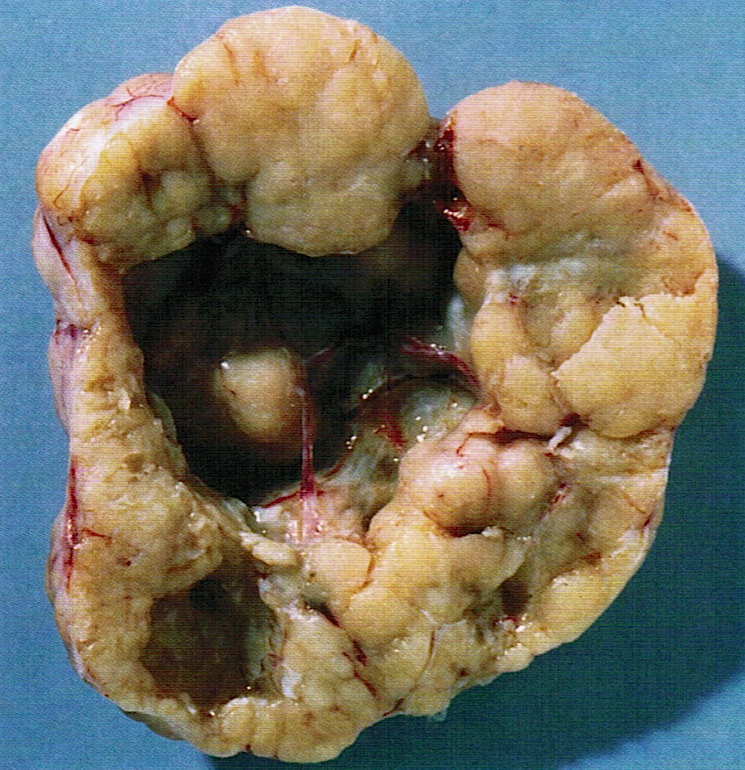
Gross description
- Size from < 1 cm to 30 cm
- Encapsulated mass, often nodular, lobulated appearance
- Often centered within or hanging from broad ligament or fallopian tube by a pedicle
- Solid or partially cystic; may have spongy appearance
- Cut surface is rubbery, variegated, pale yellow, gray-white or tan
- May be hemorrhagic or necrotic
- References: Cancer 1973;31:671, Am J Surg Pathol 1983;7:125, Hum Pathol 1999;30:856
Gross images
Frozen section description
- May be mistaken for adenocarcinoma, sex cord stromal tumor or mesonephric carcinoma
- If the tumor is extraovarian, the tumor location (e.g., broad ligament, mesosalpinx) may help to include FATWO in the differential diagnosis during intraoperative consultation
- Variety of patterns may aid with a differential diagnosis, although this may be difficult to appreciate during frozen section due to limited sampling
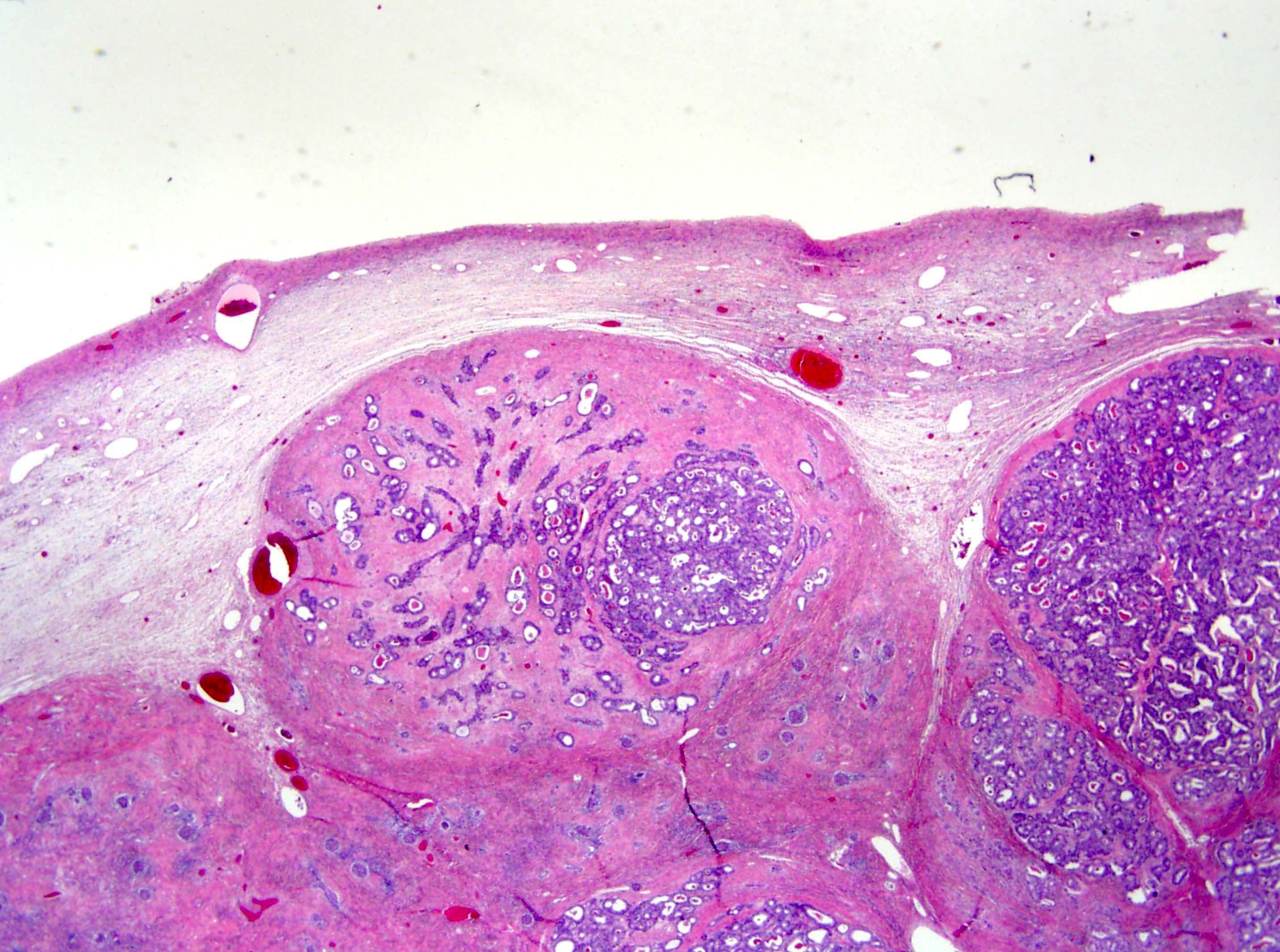
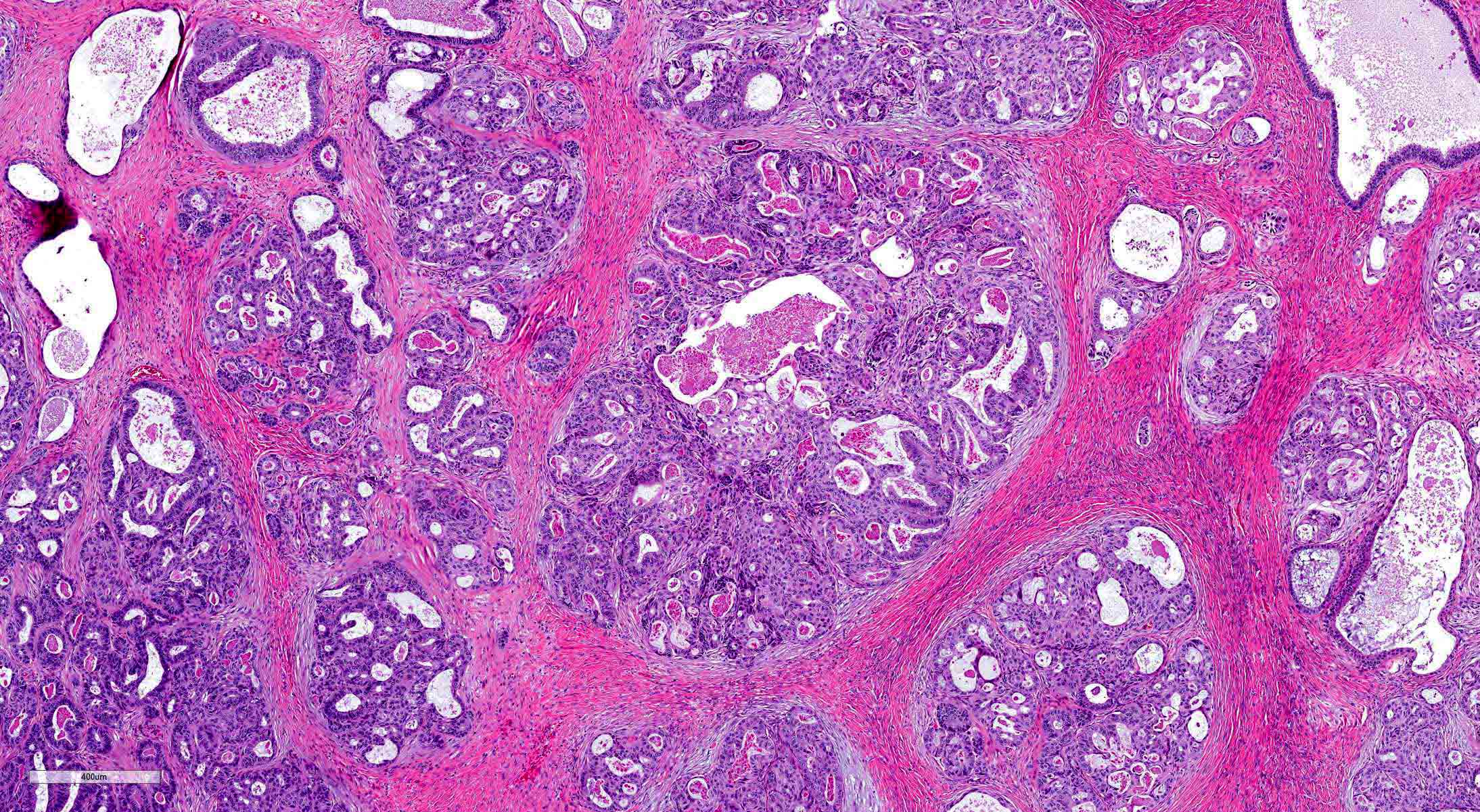
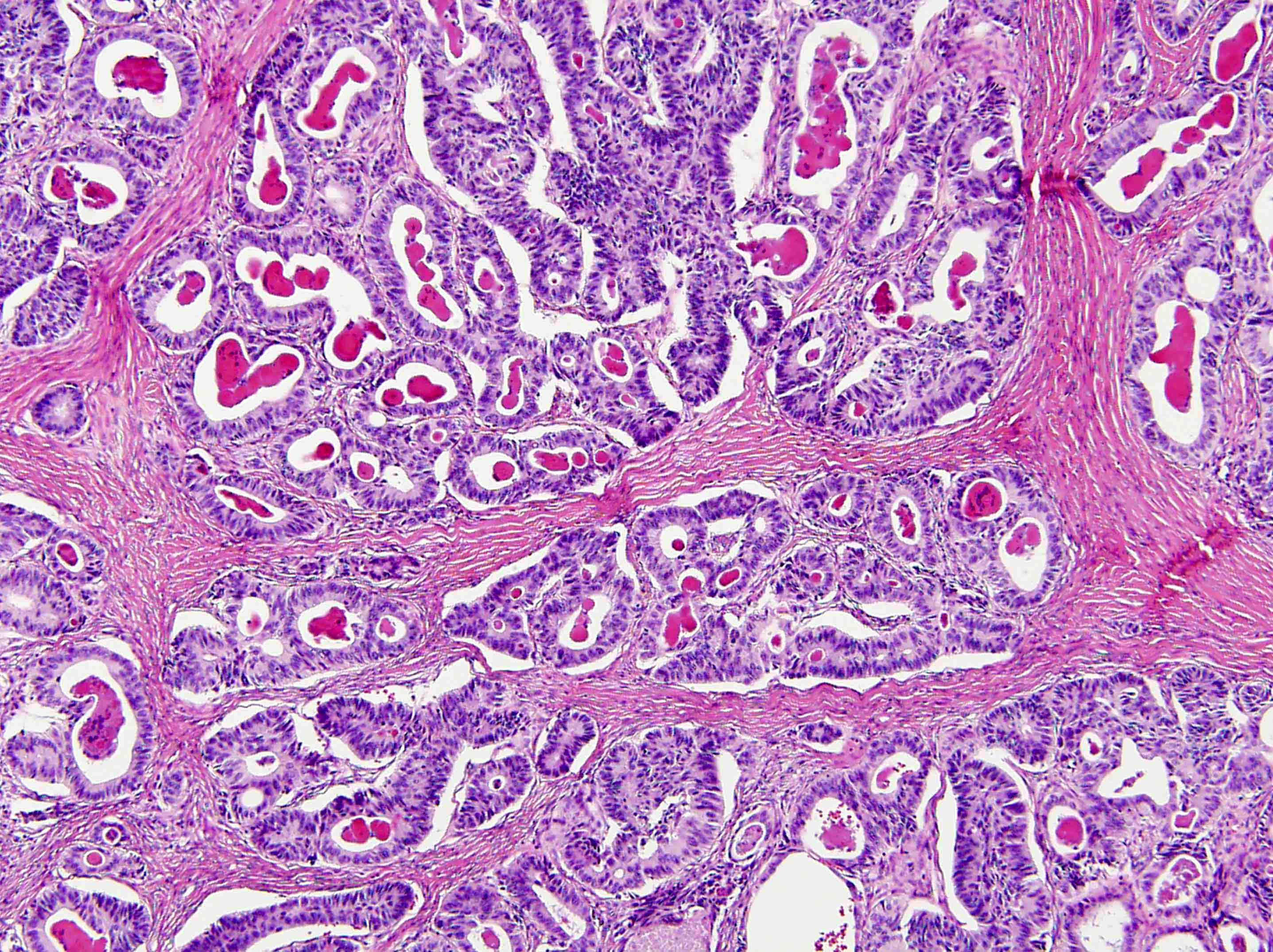
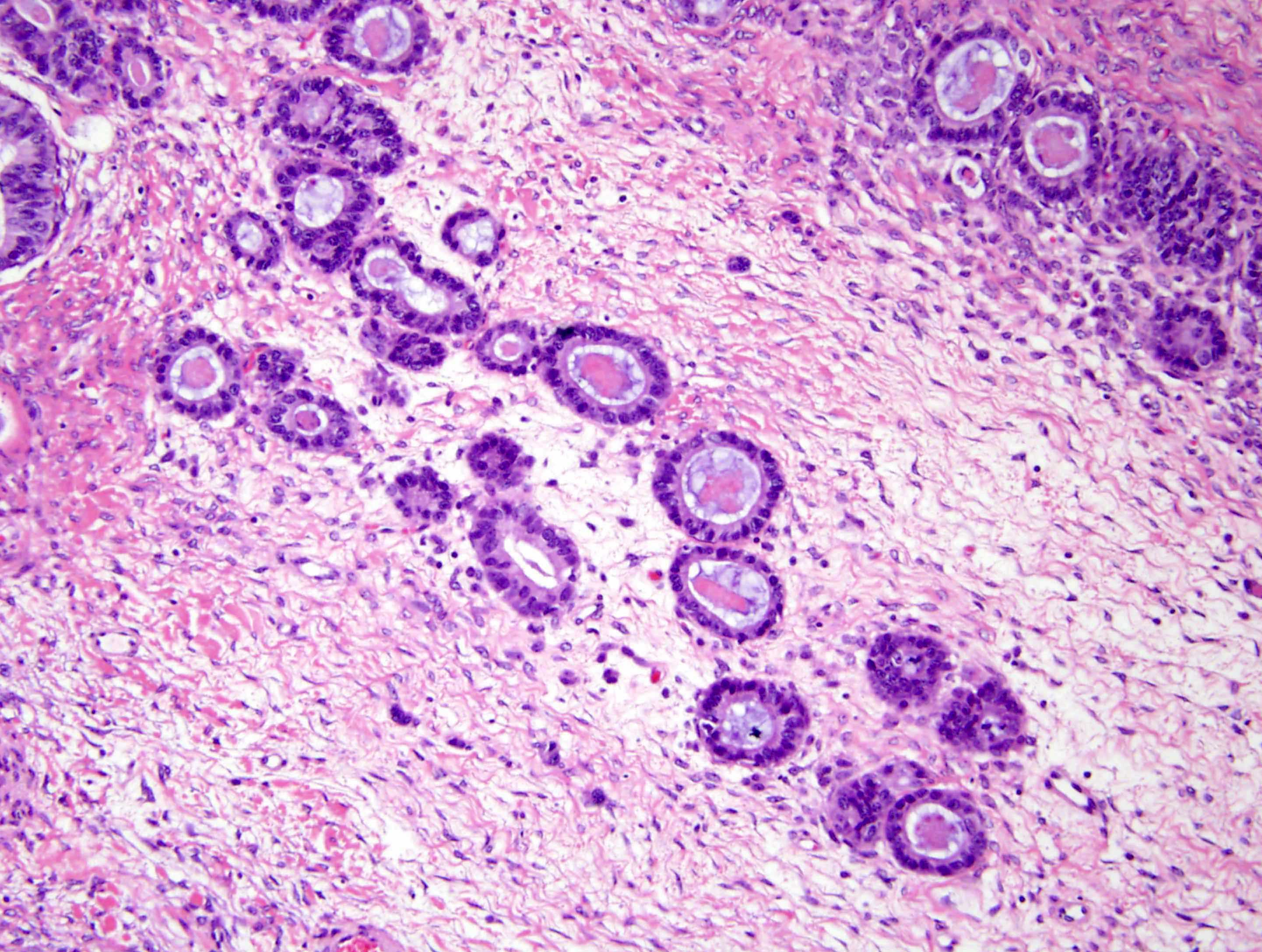
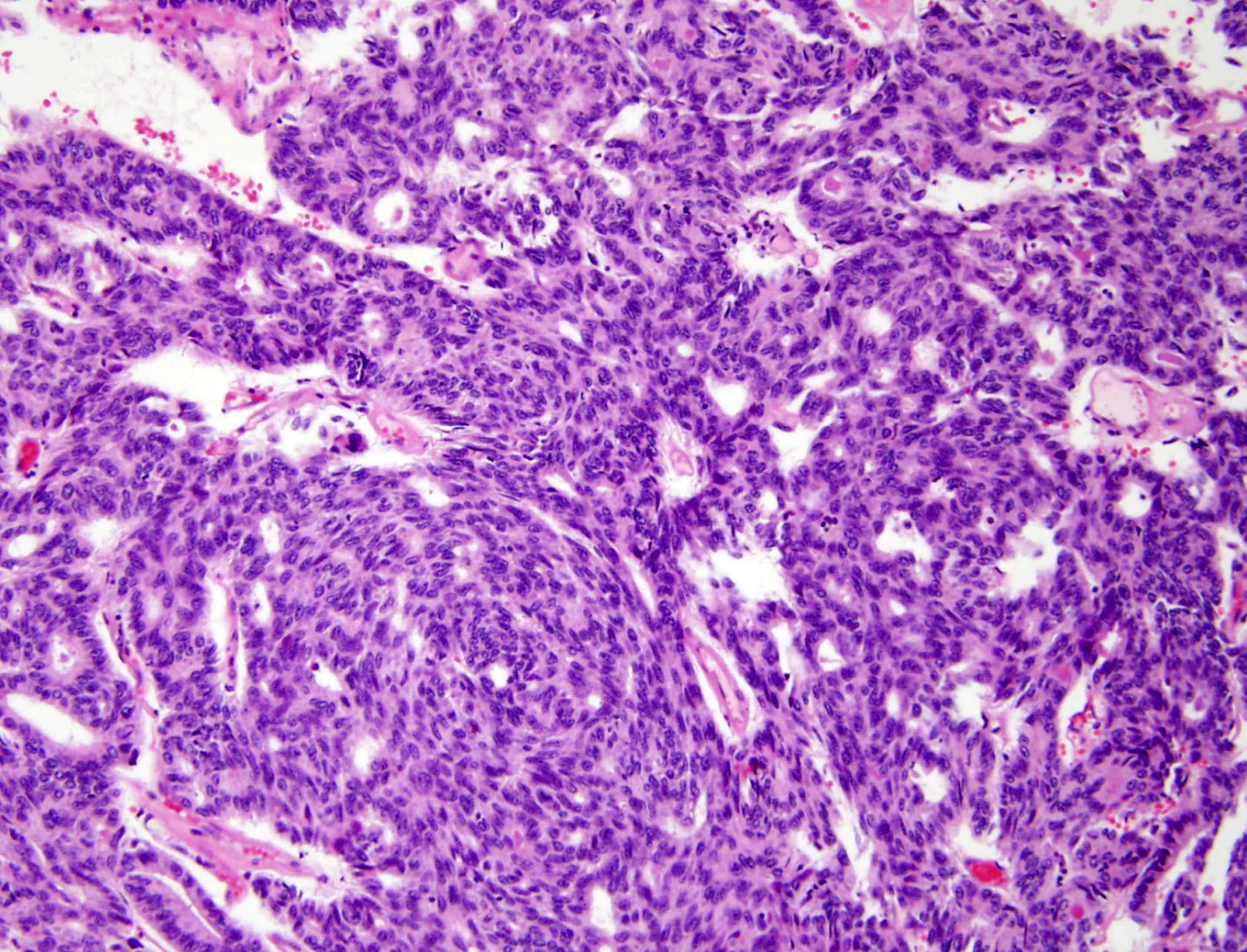
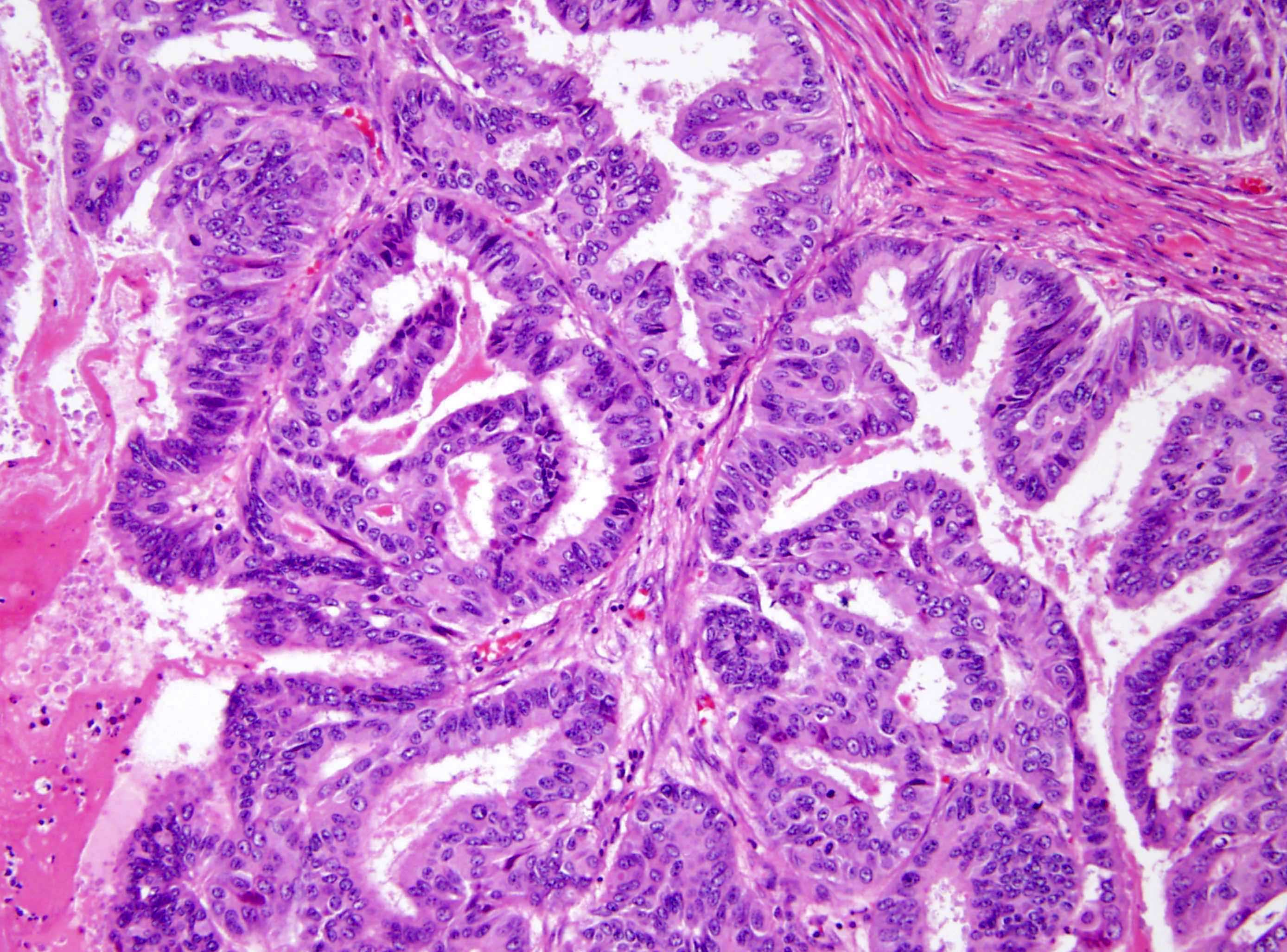
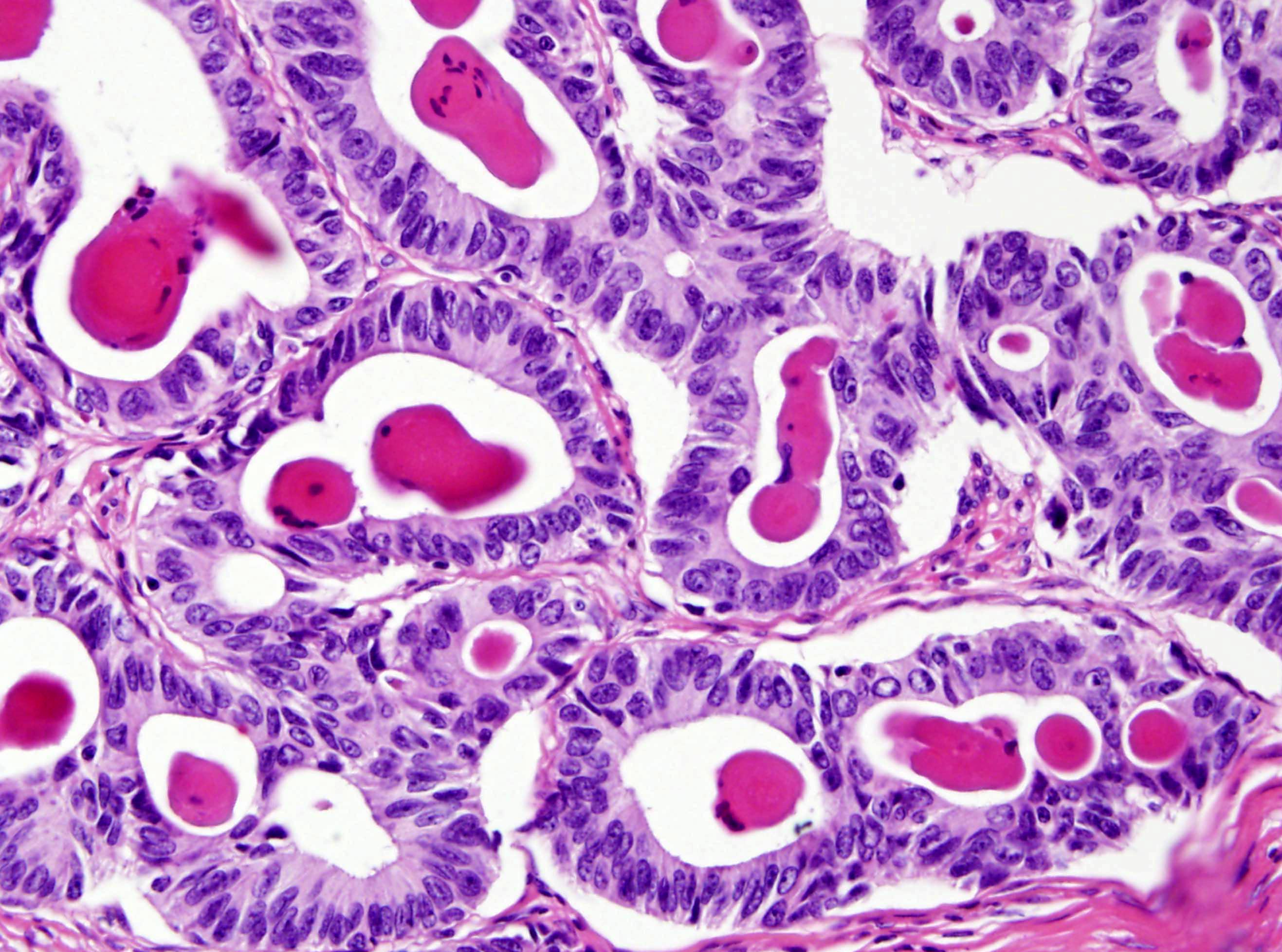
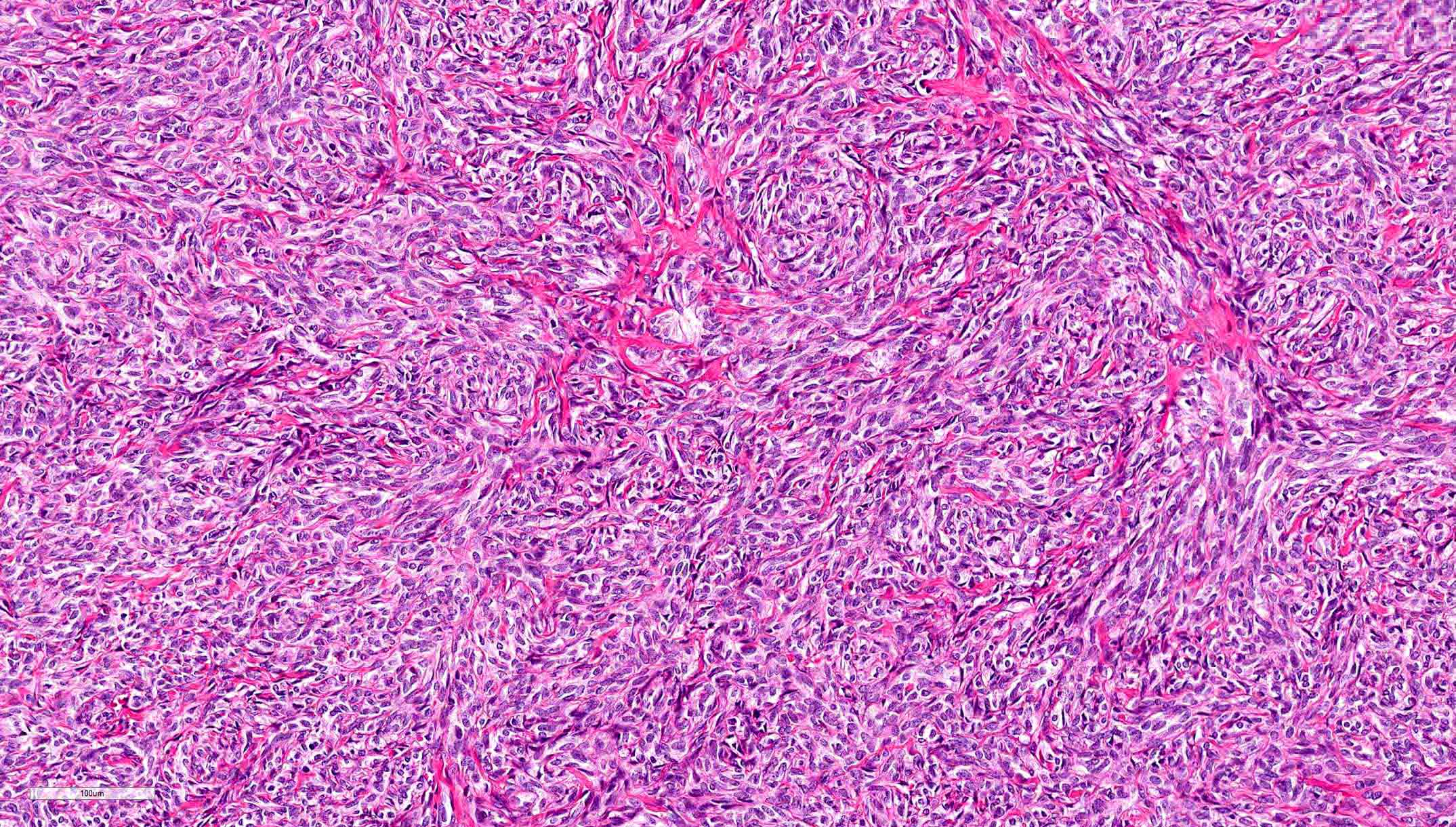
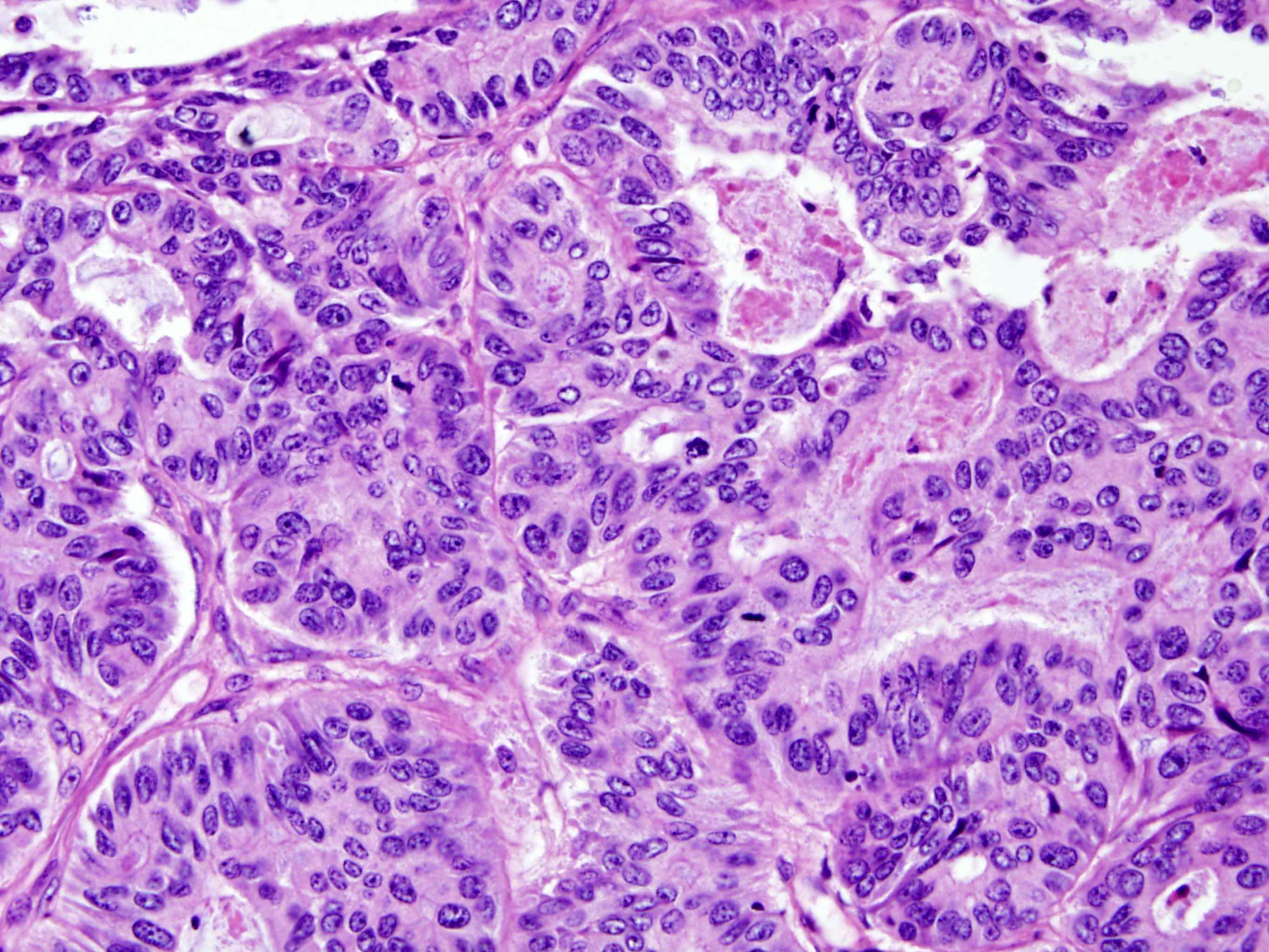
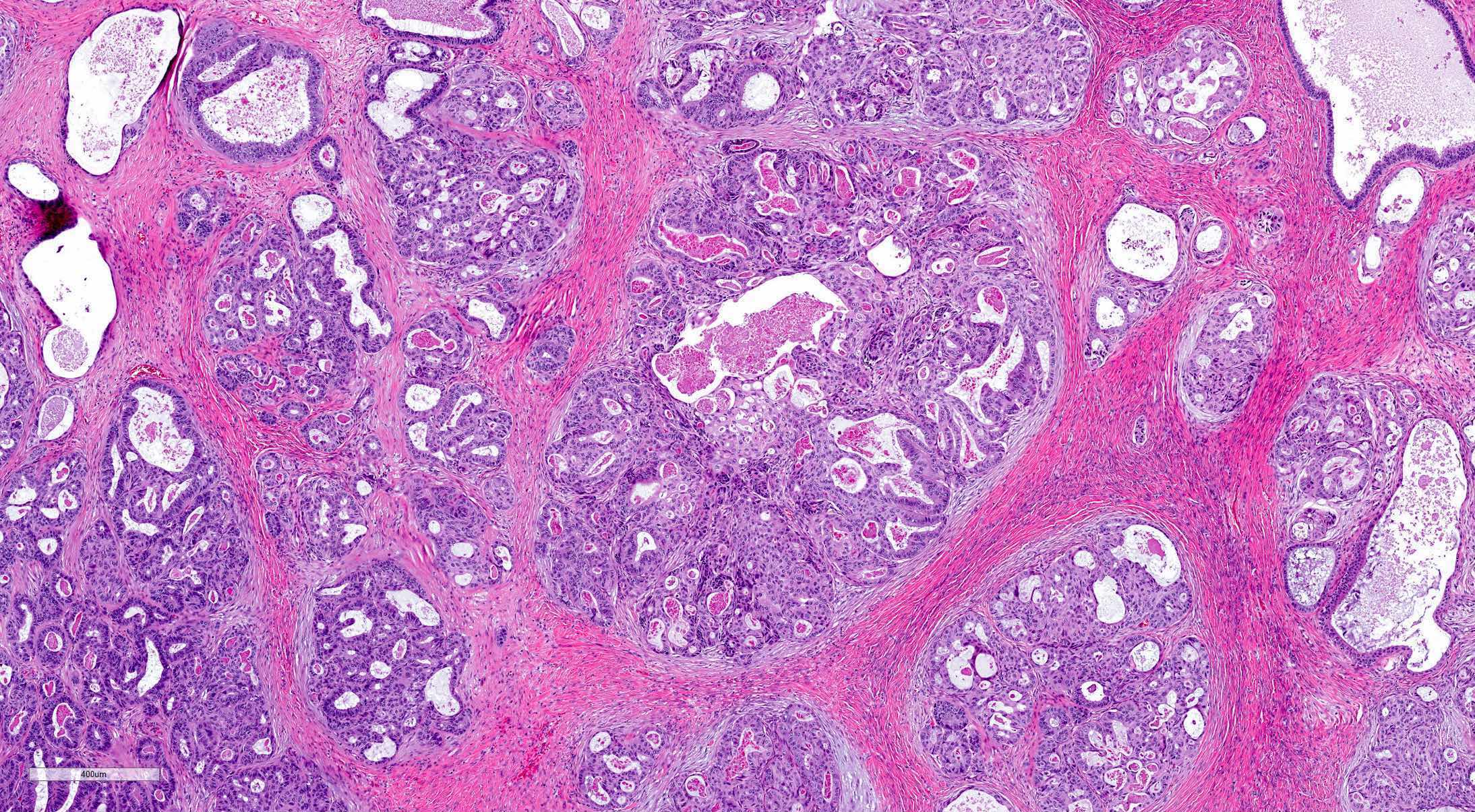
Microscopic (histologic) description
- Cribriform, tubular, cystic, tubulocystic, sieve-like, solid cords and diffuse growth patterns
- Usually a single pattern predominates but several architectural patterns may coexist (Am J Surg Pathol 1983;7:125)
- Solid sheets of spindle or polygonal cells may be the dominant morphology
- Fibrous stroma varies from scant to large areas of hyalinization
- Intraluminal, bright eosinophilic secretions are often present
- Cells are columnar or cuboidal, may have scant clear cytoplasm, flat or hobnail appearance
- Large cytoplasmic vacuoles and signet ring cell-like forms may be seen (Int J Surg Pathol 2008;16:222)
- Uniform, round or oval nuclei with pale, evenly dispersed chromatin; may have nuclear grooves
- Nuclear atypia is mild to moderate
- Mitotic activity is typically low (up to 1/10 - 3/10 high power fields)
- Malignant tumors have been suggested to present as undifferentiated carcinoma with high cellularity, pleomorphic nuclei or increased mitoses (up to 16/10 high power fields); however, a recent literature review of tumors classified as malignant FATWO indicates that many represent STK11 adnexal tumor or endometrioid carcinoma with unusual features (Am J Surg Pathol 1983;7:125, Histopathology 2022;81:280)
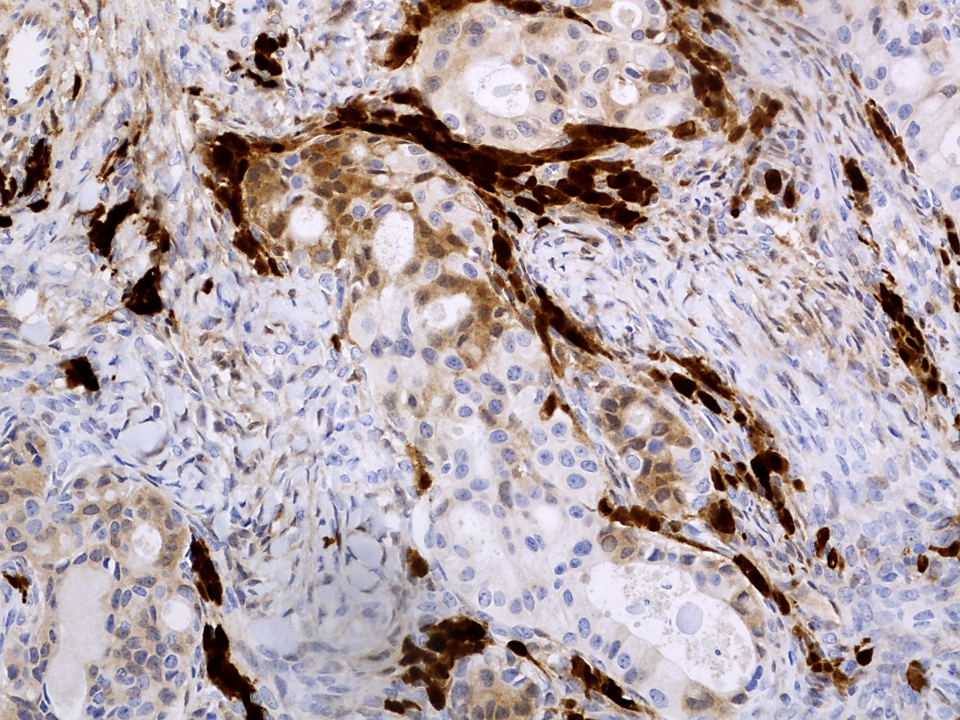
Microscopic (histologic) images
Contributed by Elena Lucas, M.D. and Wenxin Zheng, M.D.
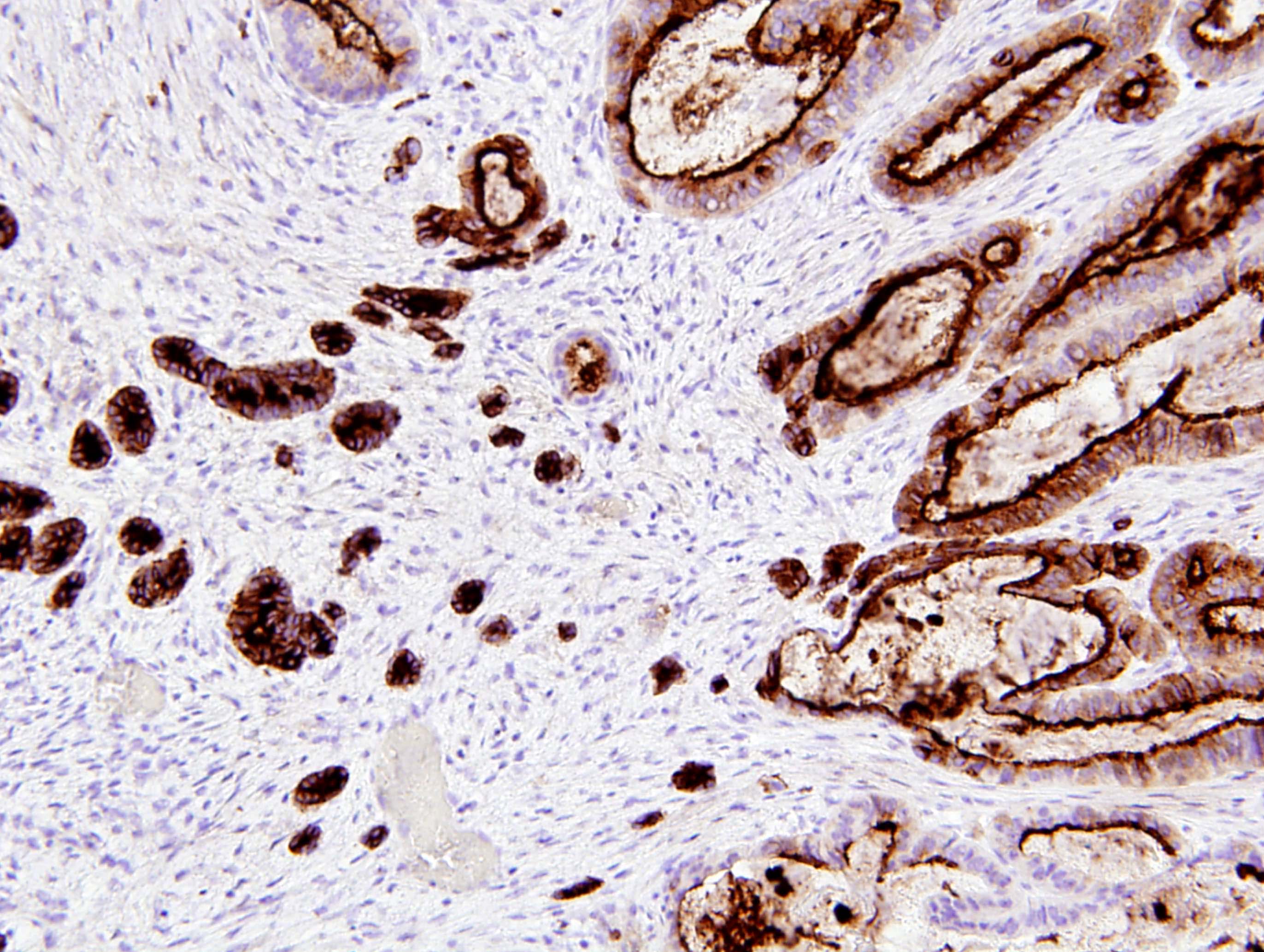
Positive stains
- Pancytokeratin (AE1 / AE3, CAM5.2), CK7, CK19
- Variable: CD10 (50 - 100%), calretinin, inhibin, MelanA, CD99, WT1, ER, PR, androgen receptor, EMA, GATA3, CD117 (KIT), vimentin, SMA (in spindle cell areas)
- References: Hum Pathol 1999;30:856, Int J Gynecol Pathol 2019;38:543, Mod Pathol 2020;33:734, Am J Surg Pathol 2015;39:1411, Arch Pathol Lab Med 2022;146:166
Negative stains
- PAX8 (negative in majority of cases, although focal positivity has been rarely reported) (Mod Pathol 2020;33:734)
- EMA (typically negative; may show focal weak staining)
- CK20, CEA, TTF1, SF1 (Int J Gynecol Pathol 2016;35:167)
Electron microscopy description
- Distinct basal laminae, desmosomal junctions and poorly developed cytoplasmic organelles (Pathol Int 2006;56:95)
- No / minimal cilia, no secretory granules (Pathol Int 2006;56:95)
Molecular / cytogenetics description
- No disease defining molecular alterations identified
- Rare tumors harbor APC and MBD4 mutations; KMT2D mutations (Mod Pathol 2020;33:734, Int J Gynecol Pathol 2019;38:543)
- Tumors previously classified as FATWOs with recurring STK11 mutations are now known to represent STK11 adnexal tumors (Histopathology 2022;81:280)
- Despite CD117 positivity in some tumors, no KIT mutations have been detected (Pathol Int 2006;56:95)
Sample pathology report
- Right adnexal mass, right salpingo-oophorectomy:
- Female adnexal tumor of probable Wolffian origin (FATWO), 6.0 cm (see synoptic report and comment)
- Comment: FATWO (also known as Wolffian tumor) is a rare tumor of low malignant potential. These tumors are thought to arise from mesonephric remnants. Most tumors behave in a benign fashion, although some tumors exhibit aggressive behavior. Although features known to be associated with adverse prognosis (e.g., large size, capsular invasion, rupture, high cellularity, nuclear pleomorphism, high mitotic activity) are absent in this case, cases without these features may also recur. Clinical correlation and follow up are recommended.
Differential diagnosis
- Endometrioid carcinoma:
- Glandular pattern with variable squamous differentiation
- Nuclear atypia
- May show intraluminal mucin
- Positive for PAX8
- High grade serous carcinoma:
- Clear cell carcinoma:
- High grade nuclear features
- Typical architectural patterns (papillary, tubulocystic, solid)
- Positive for PAX8
- Sertoli cell tumor (SCT) and Sertoli-Leydig cell tumors (SLCT):
- Androgenic or estrogenic manifestations; presence of Leydig cells (in SLCT)
- Negative for CD10
- Positive for SF1 and FOXL2
- DICER1 mutation in moderately and poorly differentiated SLCT (Am J Surg Pathol 2017;41:1178)
- Adult granulosa cell tumor:
- Typically solid pattern
- Pale, angulated cells with nuclear grooves
- Hyperestrogenism
- Negative for CD10
- FOXL2 mutation (FOXL2 immunohistochemistry is not specific for mutation status) (N Engl J Med 2009;360:2719)
- STK11 tumors:
- Interanastomosing cords and trabeculae, salivary gland tumor-like growth, tubular, cystic, cribriform, microacinar, nested, nodular, papillary, follicular and solid
- Myxoid, collagenous or hyalinized stroma
- Nuclear atypia with prominent nucleoli, variable mitoses
- Basophilic intraluminal secretions
- Association with Peutz-Jeghers syndrome in ~50%
- Recurrent STK11 alterations (Histopathology 2022;81:280)
- Mesonephric carcinoma:
- Predominantly in the cervix
- May arise in a background of mesonephric hyperplasia
- Mesonephric-like carcinoma:
- Adenomatoid tumor:
- Small, unencapsulated tumor
- Lacks variety of patterns within the same tumor
- Negative for CD10
- Mesothelioma:
- Metastatic carcinoma:
- Higher nuclear grade
- Typically lacks variety of patterns
- Often shows necrosis
- Often positive for CEA
Additional references
Practice question #1
A 48 year old woman is diagnosed with a 6 cm adnexal mass arising from the broad ligament. She undergoes salpingo-oophorectomy. Microscopically, the tumor has a nodular appearance with low grade cells arranged in a sieve-like pattern and tightly packed tubules with eosinophilic secretions. No necrosis is seen. Mitotic activity is 1/10 high power fields. The tumor cells are negative for PAX8 and positive for CD10. Which of the following is likely to be true?
- Final diagnosis is based on ancillary studies
- Minimal nuclear atypia and low mitotic rate are predictive of benign behavior
- Patients often have virilizing symptoms
- Tumor likely originated from mesonephric embryological remnants
- Tumor originated from paramesonephric embryological remnants
Practice answer #1
D. Tumor likely originated from mesonephric embryological remnants
Comment Here
Reference: Female adnexal tumor of probable Wolffian origin
Comment Here
Reference: Female adnexal tumor of probable Wolffian origin
Practice question #2
This image is from a 50 year old woman with an encapsulated adnexal mass, found incidentally. Which of the following statements is true?
- Calretinin and inhibin immunostains help to differentiate it from sex cord stromal tumors
- CD117+ tumors harbor KIT mutation
- ER and PR immunostains help to differentiate it from endometrioid carcinoma
- FOXL2 mutation is present in the majority of tumors
- Tumor is typically positive for pancytokeratin and CD10
Practice answer #2
E. Tumor is typically positive for pancytokeratin and CD10. This is a female adnexal tumor of probable Wolffian origin (FATWO), which is typically positive for pancytokeratin and CD10.
Comment Here
Reference: Female adnexal tumor of probable Wolffian origin
Comment Here
Reference: Female adnexal tumor of probable Wolffian origin