Ovary
General
Staging
Editorial Board Member: Gulisa Turashvili, M.D., Ph.D.
Editor-in-Chief: Debra L. Zynger, M.D.
Last author update: 8 August 2022
Last staff update: 8 August 2022
Copyright: 2002-2025, PathologyOutlines.com, Inc.
PubMed Search: Staging ovary
Page views in 2024: 18,136
Page views in 2025 to date: 12,432
Cite this page: Buza N. Staging. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorstage.html. Accessed September 17th, 2025.
Definition / general
- All primary tumors (malignant or potentially malignant [borderline] of the ovary and fallopian tube) and primary peritoneal carcinoma are covered by this staging system
- The following topics are not covered: metastatic tumors to the ovary and fallopian tube, hematopoietic malignancies, peritoneal primaries other than primary peritoneal carcinoma (i.e., mesothelioma, gastrointestinal stromal tumor)
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
ICD coding
- ICD-10:
- D39.10 - neoplasm of uncertain behavior of unspecified ovary
- D39.11 - neoplasm of uncertain behavior of right ovary
- D39.12 - neoplasm of uncertain behavior of left ovary
- C56.1 - malignant neoplasm of right ovary
- C56.2 - malignant neoplasm of left ovary
- C56.9 - malignant neoplasm of unspecified ovary
- C57.00 - malignant neoplasm of unspecified fallopian tube
- C57.01 - malignant neoplasm of right fallopian tube
- C57.02 - malignant neoplasm of left fallopian tube
- C48.1 - malignant neoplasm of specified parts of peritoneum
- C48.2 - malignant neoplasm of peritoneum, unspecified
- C48.8 - malignant neoplasm of overlapping sites of retroperitoneum and peritoneum
Primary tumor (pT) and FIGO stages in ( )
- pTX: primary tumor cannot be assessed
- pT0: no evidence of primary tumor
- pT1a (IA): tumor limited to 1 ovary (capsule intact) or fallopian tube; no tumor on ovarian or fallopian tube surface; no malignant cells in ascites or peritoneal washings
- pT1b (IB): tumor limited to both ovaries (capsules intact) or fallopian tubes; no tumor on ovarian or fallopian tube surface; no malignant cells in ascites or peritoneal washings
- pT1c (IC): tumor limited to 1 or both ovaries or fallopian tubes, with any of following:
- pT1c1 (IC1): surgical spill
- pT1c2 (IC2): capsule ruptured before surgery or tumor on ovarian or fallopian tube surface
- pT1c3 (IC3): malignant cells in ascites or peritoneal washings
- pT2a (IIA): extension or implants on the uterus or fallopian tube(s) or ovaries
- pT2b (IIB): extension to or implants on other pelvic tissues
- pT3a (IIIA2): microscopic extrapelvic (above the pelvic brim) peritoneal involvement with or without positive retroperitoneal lymph nodes
- pT3b (IIIB): macroscopic peritoneal metastasis beyond pelvis ≤ 2 cm with or without retroperitoneal lymph node metastasis
- pT3c (IIIC): macroscopic peritoneal metastasis beyond pelvis > 2 cm with or without retroperitoneal lymph node metastasis (includes extension of tumor to capsule of liver and spleen without parenchymal involvement of either organ)
Regional lymph nodes (pN) and FIGO stages in ( )
- pNX: regional lymph nodes cannot be assessed
- pN0: no regional lymph node metastasis
- pN0(i+): isolated tumor cells in regional lymph node(s) ≤ 0.2 mm
- pN1a (IIIA1i): lymph node metastatic deposit > 0.2 mm to ≤ 10 mm
- pN1b (IIIA1ii): lymph node metastatic deposit > 10 mm
Note:
- Regional lymph nodes include the following: external iliac, internal iliac (hypogastric), obturator, common iliac, para-aortic, pelvic NOS and retroperitoneal NOS lymph nodes
Prefixes
- cTNM: clinical classification
- pTNM: pathological classification
- ypTNM: post therapy pathological classification
- rTNM: recurrence or retreatment classification
- aTNM: autopsy classification
AJCC prognostic stage groups
|
| Stage I: |
pT1 |
N0 |
M0 |
|
|
|
|
| Stage IA: |
pT1a |
N0 |
M0 |
|
|
|
|
| Stage IB: |
pT1b |
N0 |
M0 |
|
|
|
|
| Stage IC: |
pT1c |
N0 |
M0 |
|
|
|
|
| Stage II: |
pT2 |
N0 |
M0 |
|
|
|
|
| Stage IIA: |
pT2a |
N0 |
M0 |
|
|
|
|
| Stage IIB: |
pT2b |
N0 |
M0 |
|
|
|
|
| Stage IIIA1: |
pT1/2 |
N1 |
M0 |
|
|
|
|
| Stage IIIA2: |
pT3a |
any N |
M0 |
|
|
|
|
| Stage IIIB: |
pT3b |
any N |
M0 |
|
|
|
|
| Stage IIIC: |
pT3c |
any N |
M0 |
|
|
|
|
| Stage IV: |
any T |
any N |
M1 |
|
|
|
|
| Stage IVA: |
any T |
any N |
M1a |
|
|
|
|
| Stage IVB: |
any T |
any N |
M1b |
|
|
|
|
Registry data collection variables
- FIGO stage
- Preoperative CA125 level
- Gross residual tumor after primary cytoreductive surgery
- Residual tumor volume after primary cytoreductive surgery
- Residual tumor location following primary cytoreductive surgery
Histologic grade (G)
- GX: grade cannot be assessed
- GB: borderline tumor
- G1: well differentiated
- G2: moderately differentiated
- G3: poorly differentiated
Histopathologic type
- Epithelial tumors (borderline or malignant)
- Serous tumors
- Serous borderline tumor
- Low grade serous carcinoma
- High grade serous carcinoma
- Mucinous tumors
- Mucinous borderline tumor
- Mucinous carcinoma
- Endometrioid tumors
- Endometrioid borderline tumor
- Endometrioid carcinoma
- Clear cell tumors
- Clear cell borderline tumor
- Clear cell carcinoma
- Seromucinous tumors
- Seromucinous borderline tumor
- (Seromucinous carcinoma - now considered a subtype of endometrioid carcinoma, according to WHO 5th edition)
- Brenner tumors
- Borderline Brenner tumor
- Malignant Brenner tumor
- Other carcinomas
- Mesonephric-like adenocarcinoma
- Undifferentiated and dedifferentiated carcinoma
- Carcinosarcoma
- Mixed carcinoma
- Sex cord - stromal tumors (malignant or potentially malignant)
- Adult granulosa cell tumor
- Juvenile granulosa cell tumor
- Sertoli-Leydig cell tumor
- Gynandroblastoma
- Steroid cell tumor, NOS
- Fibrosarcoma
- Germ cell tumors (malignant)
- Dysgerminoma
- Yolk sac tumor
- Immature teratoma
- Choriocarcinoma (nongestational)
- Embryonal carcinoma
- Mixed germ cell tumor
- Somatic neoplasms arising from teratomas
- Miscellaneous tumors
- Small cell carcinoma, hypercalcemic type
- Adenocarcinoma of rete ovarii
Gross images
Contributed by Natalia Buza, M.D.
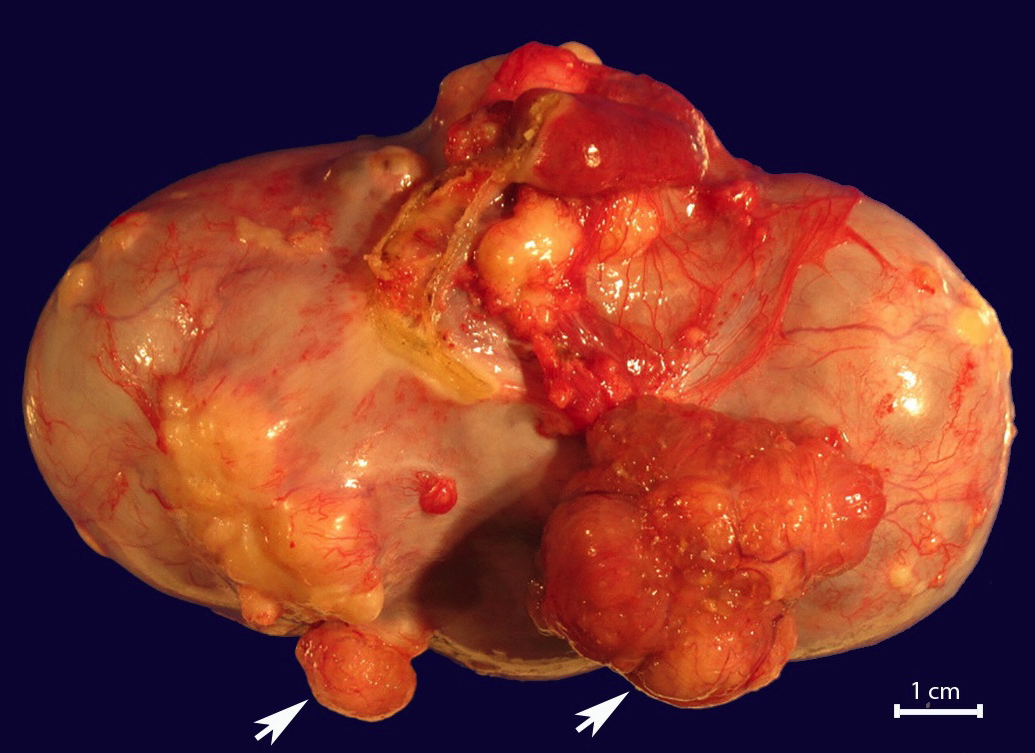
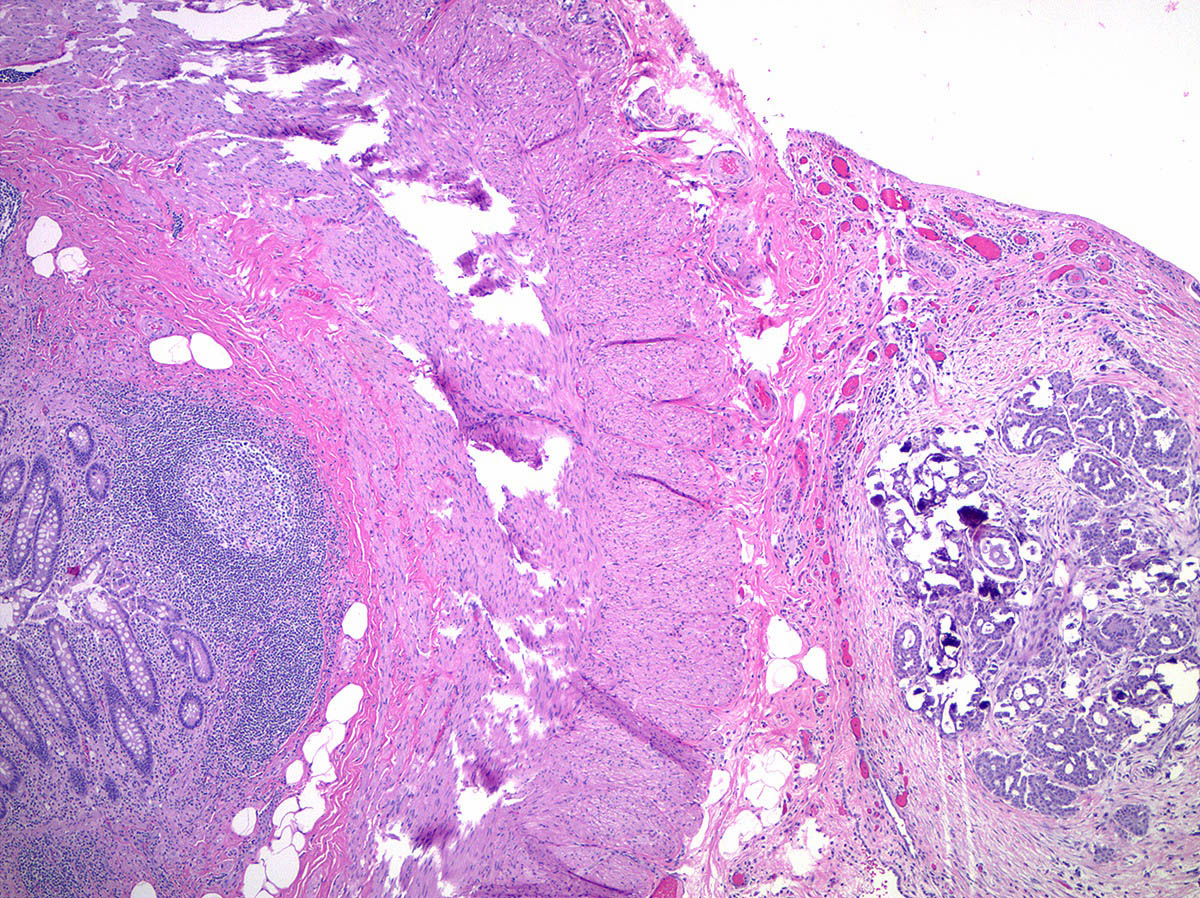
Ovarian surface involvement (pT1c2)

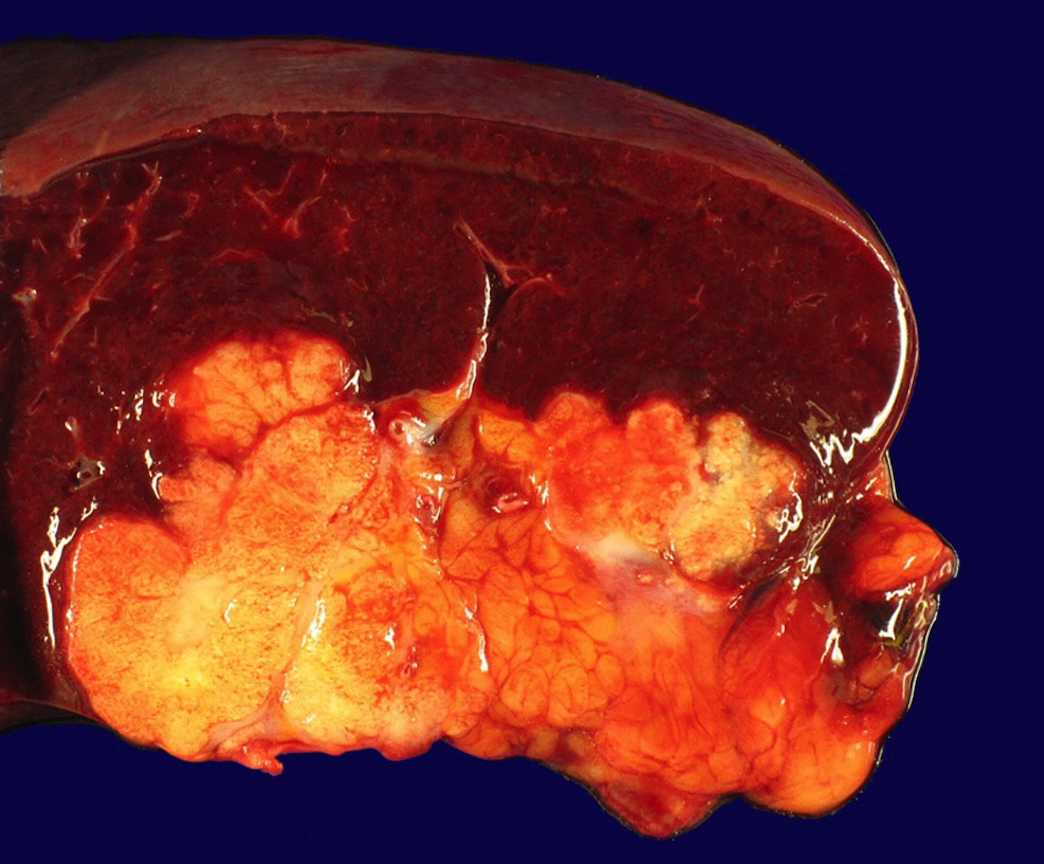
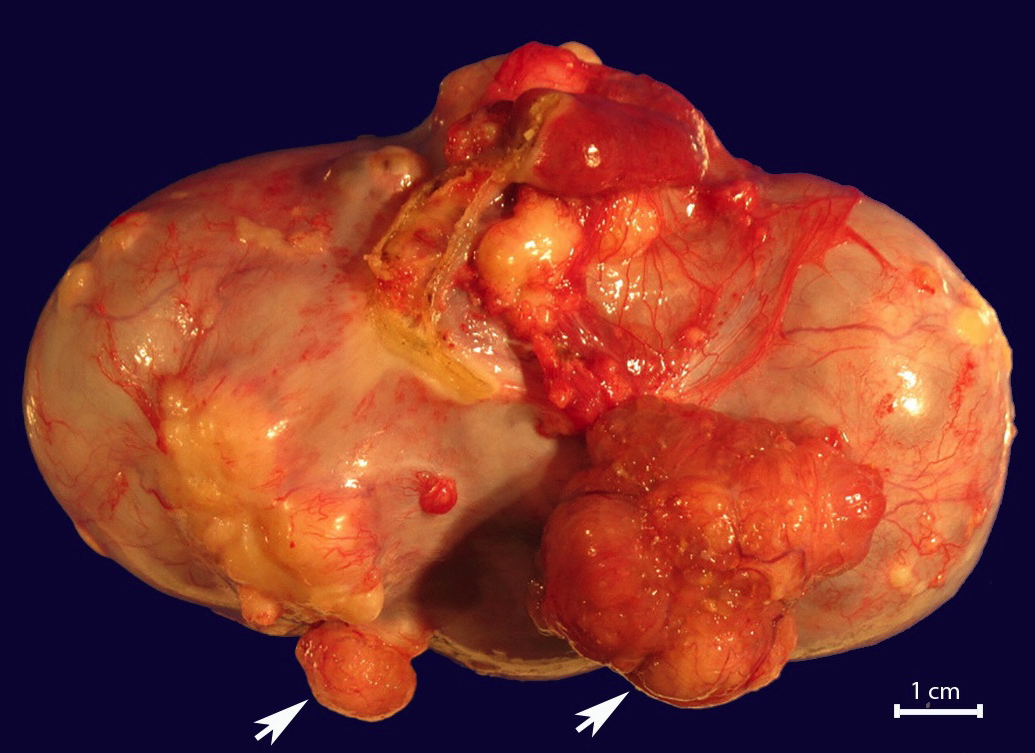
Rectosigmoid colon (pT2b)
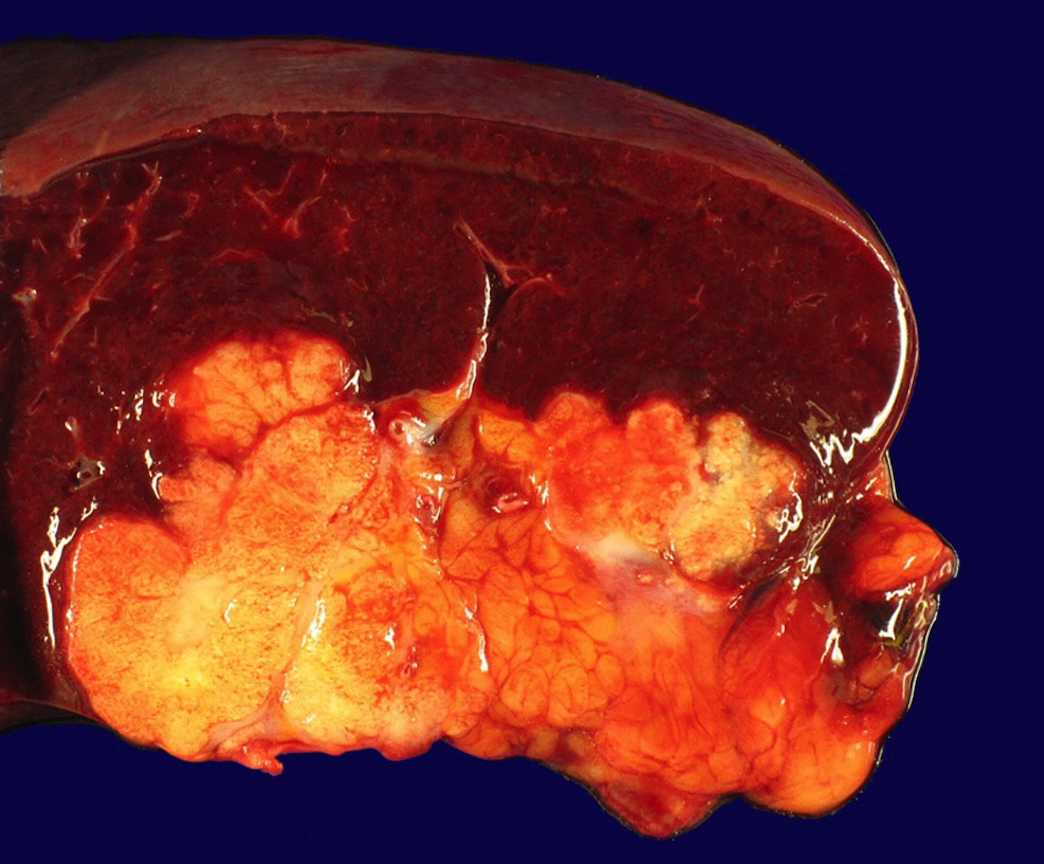
Splenic hilum and parenchyma (pM1b)
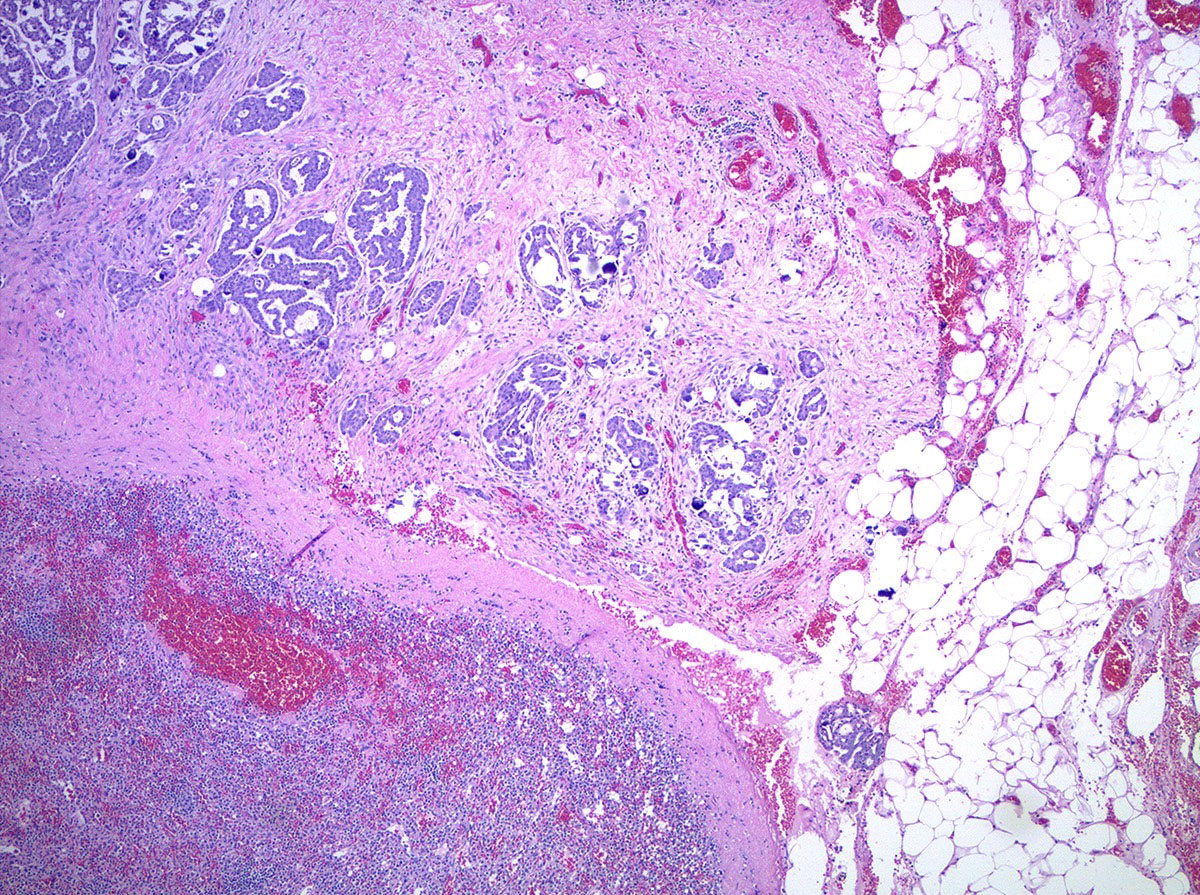
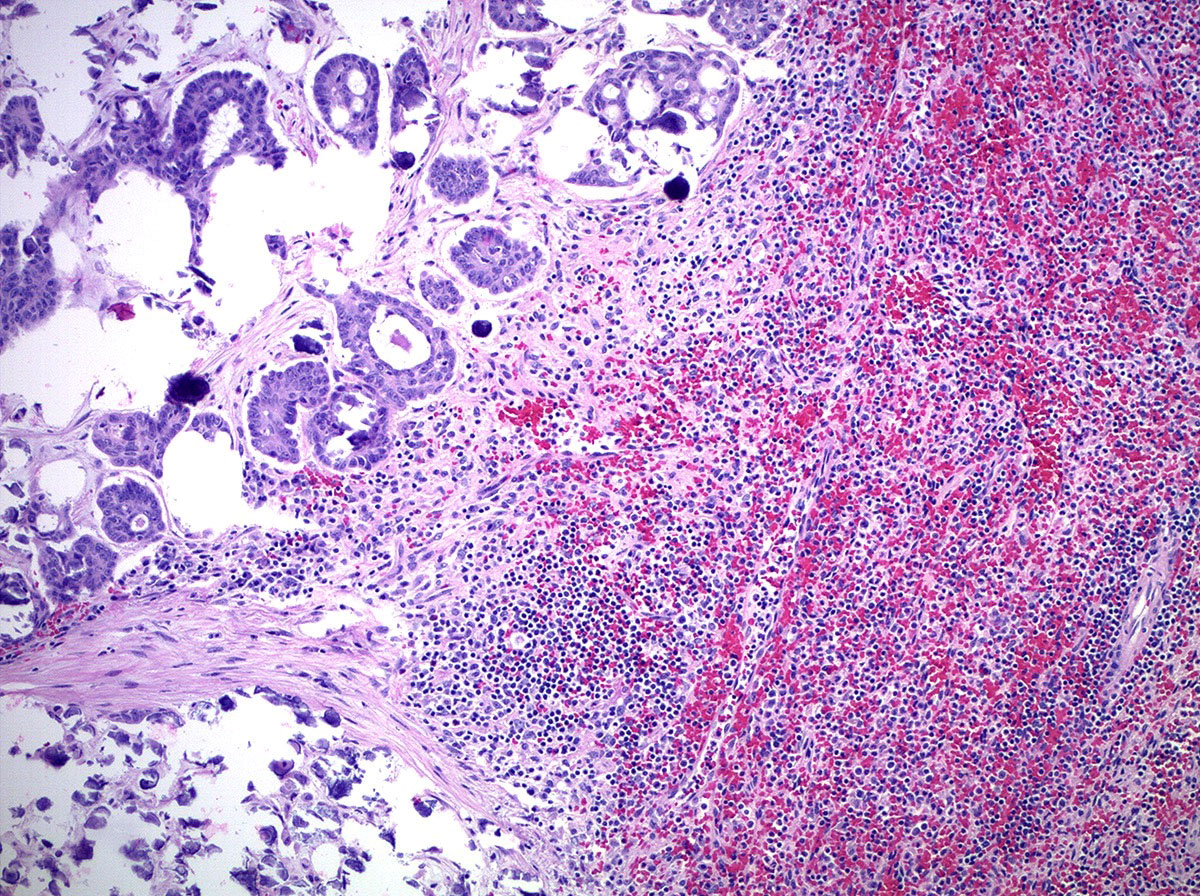
Microscopic (histologic) images
Contributed by Natalia Buza, M.D.
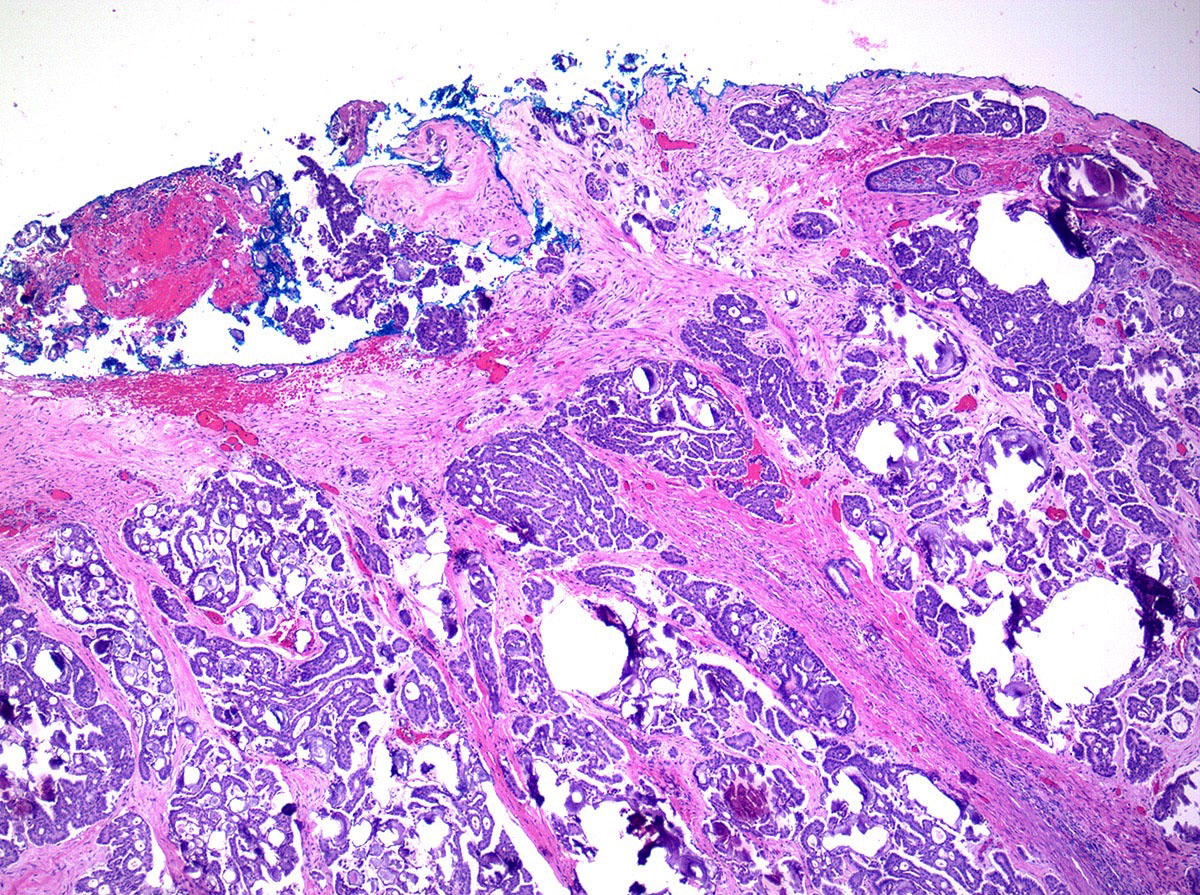
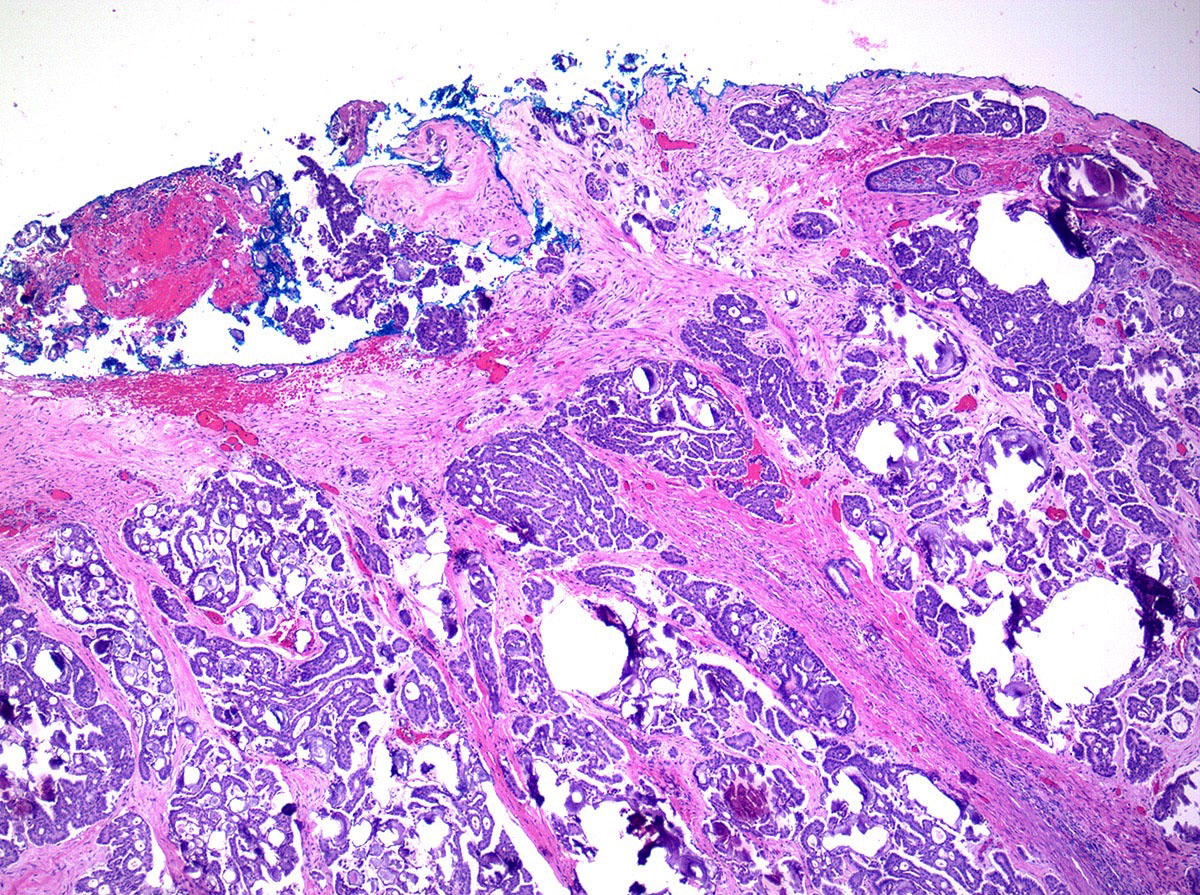
Ovarian surface involvement (pT1c2)
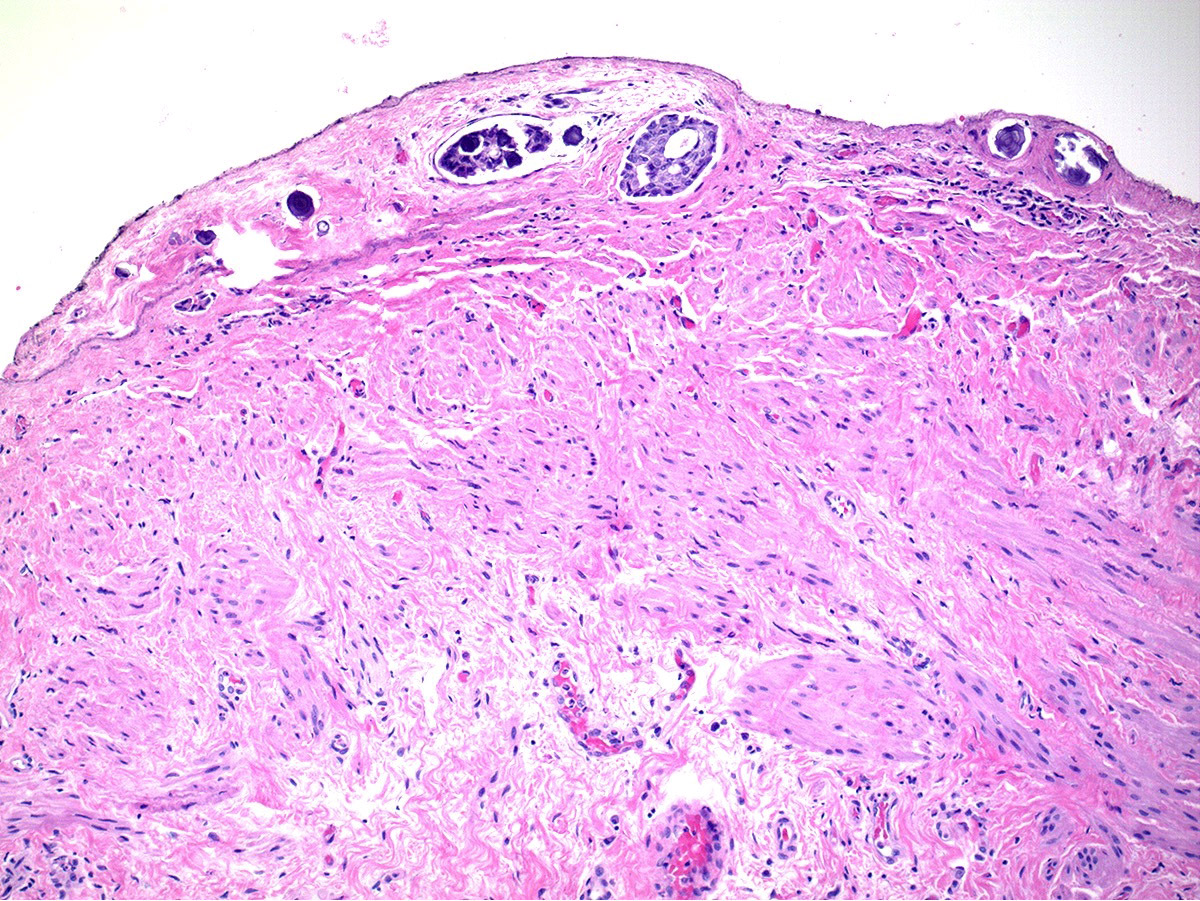
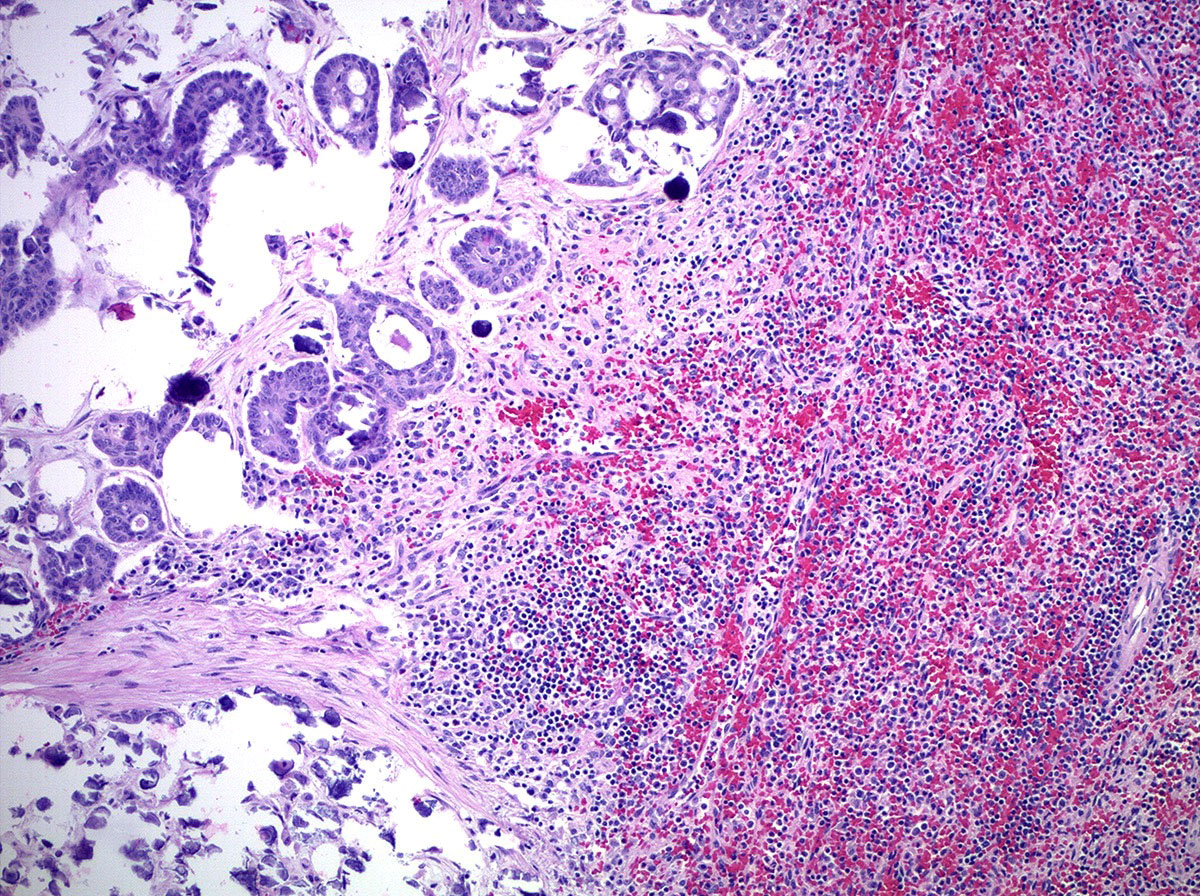
Uterine serosal (pT2a)
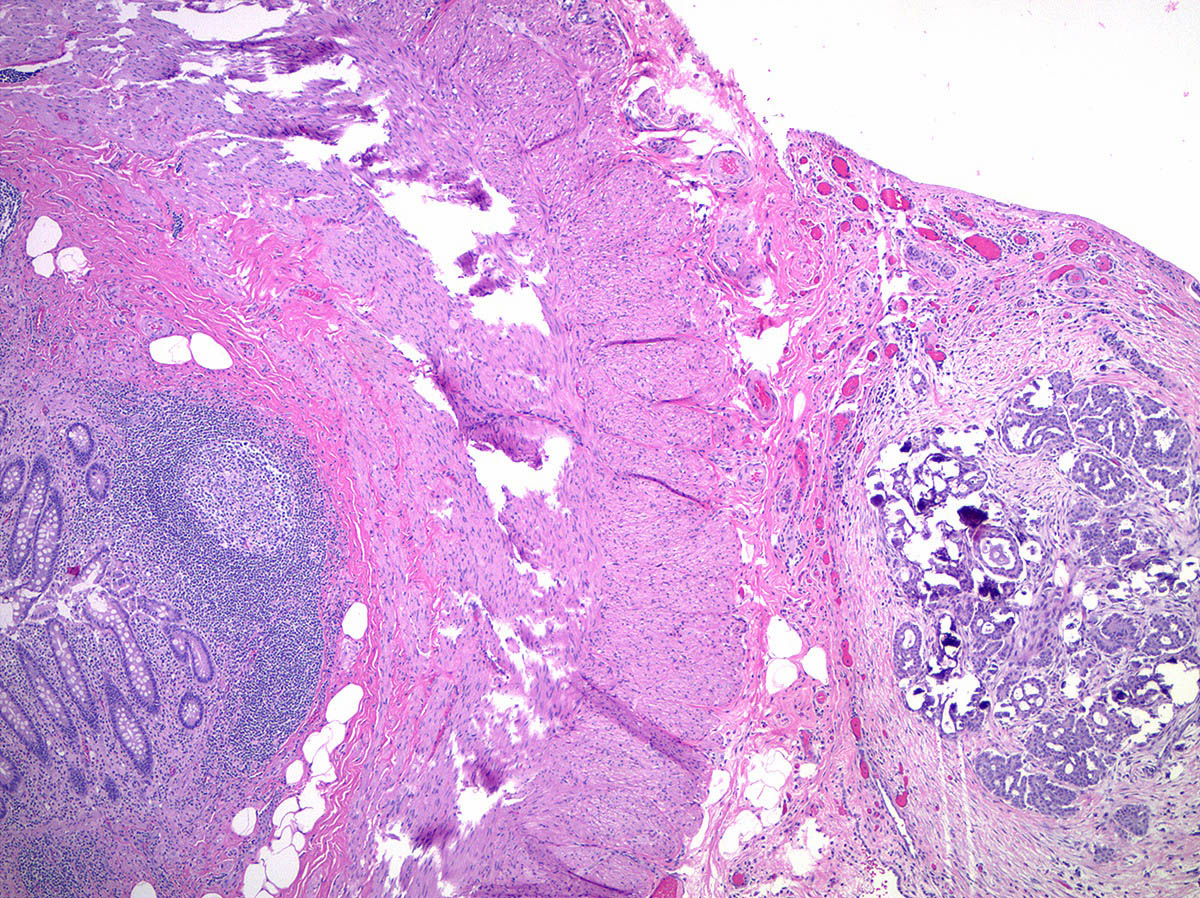
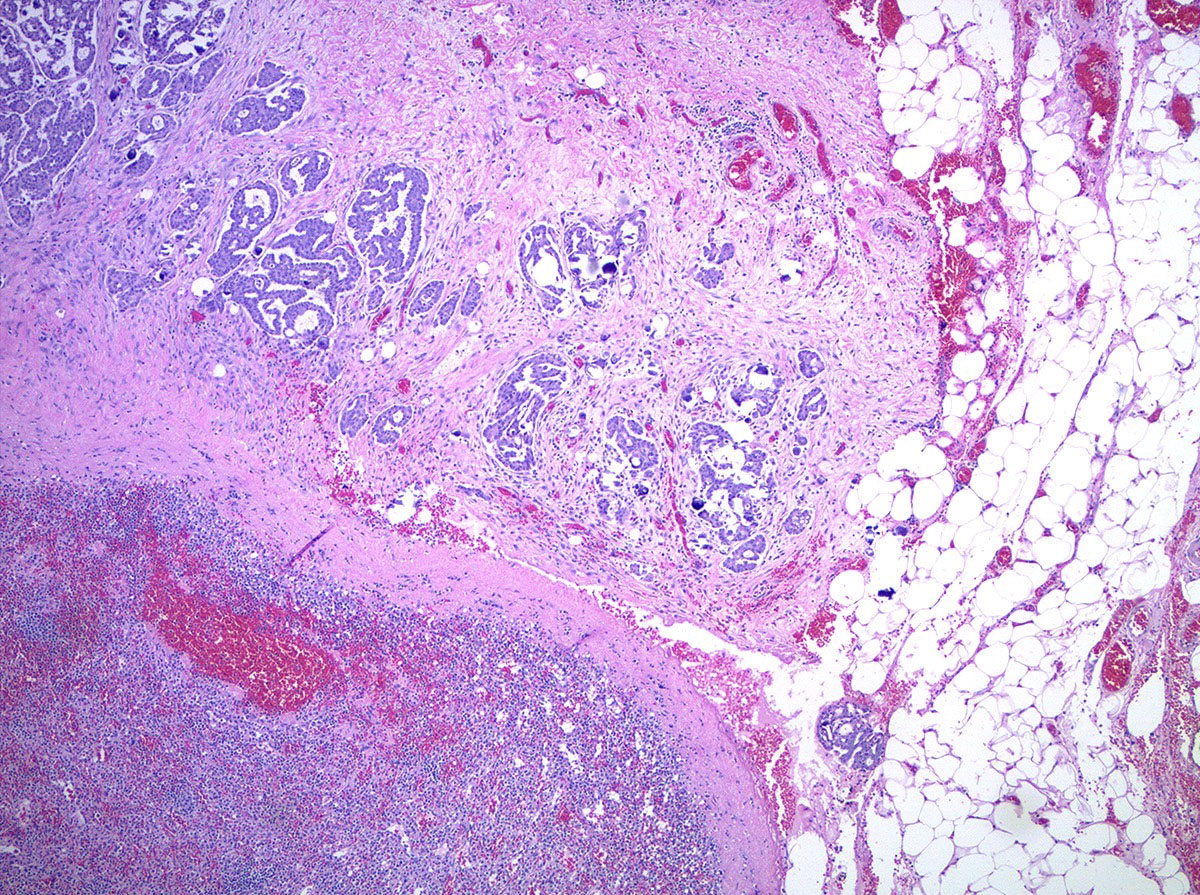
Appendiceal serosal (pT3b)
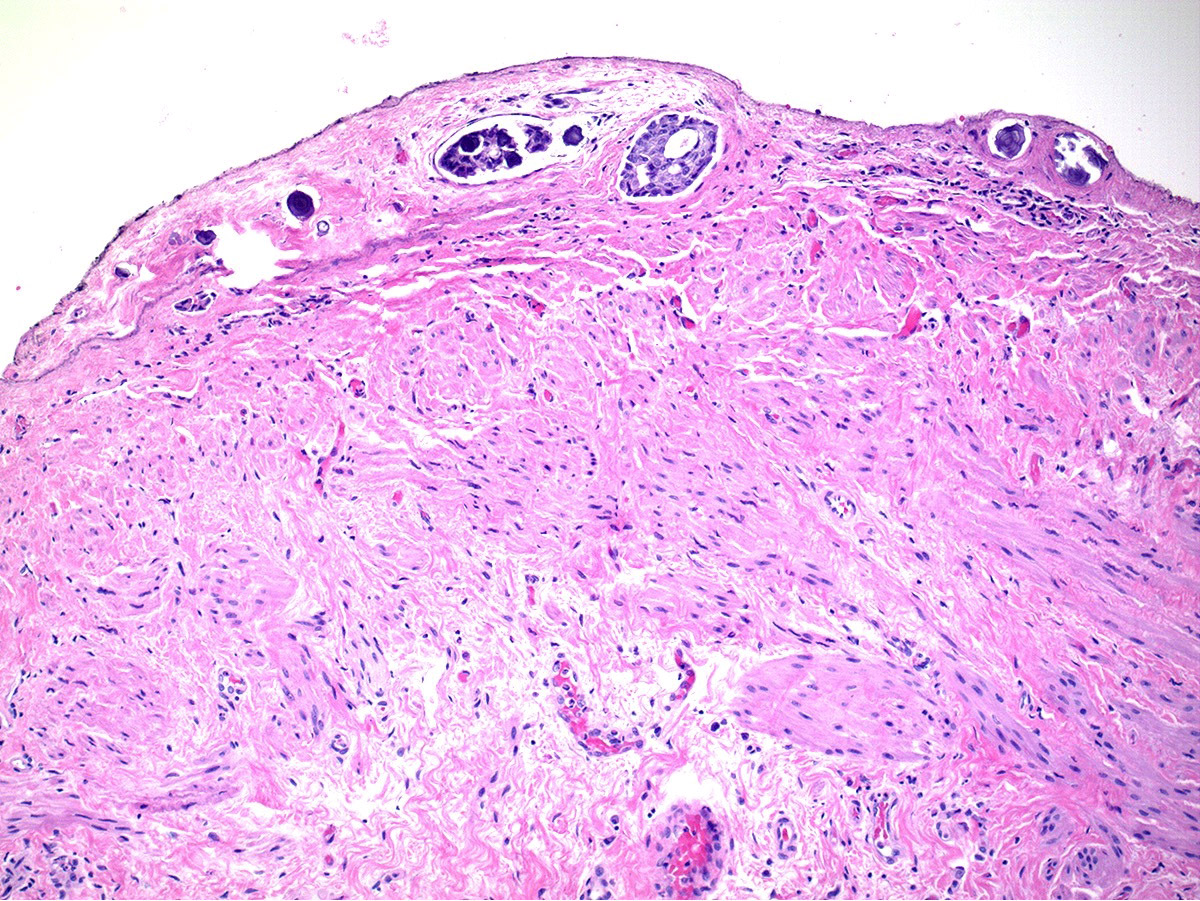
Splenic capsule (pT3c)
Splenic parenchyma (pM1b)
Practice question #1
Which of the following is the pTNM stage (per the AJCC 8th edition) of a malignant ovarian tumor involving the right ovarian parenchyma and surface, omentum and splenic capsule (for which the largest tumor focus in the omentum and splenic capsule exceeds 2 cm) and no lymph node or parenchymal spleen metastases?
- pT1c N0 M0, stage IC
- pT1c N0 M1b, stage IVB
- pT3b N0 M0, stage IIIB
- pT3c N0 M1b, stage IVB
- pT3c N0 M0, stage IIIC
Practice answer #1
E. pT3c N0 M0, stage IIIC. Macroscopic peritoneal metastasis beyond the pelvis (including capsule of liver and spleen without parenchymal involvement) measuring more than 2 cm in greatest dimension is pT3c. Parenchymal metastasis to the liver or spleen is pM1b, which would yield stage IVB.
Comment Here
Reference:
Staging - ovary

Back to top