Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mathison BA, Pritt BS. Amebic colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonamebic.html. Accessed April 20th, 2024.
Definition / general
- Disease caused by infection of the large intestine with the protozoan parasite, Entamoeba histolytica
- Several protozoan species in the genus Entamoeba colonize humans but not all of them are associated with amebiasis (Centers for Disease Control and Prevention: Amebiasis [Accessed 13 October 2023])
Essential features
- Due to invasive infection with Entamoeba histolytica
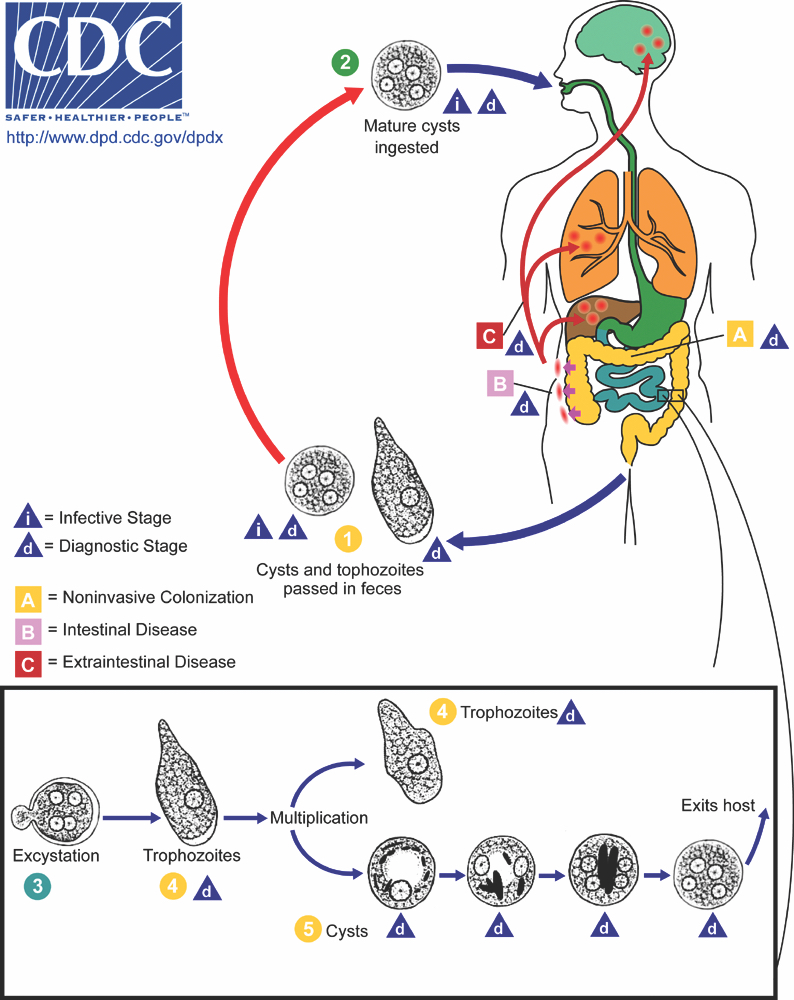
- Transmission primarily by ingestion of E. histolytica cysts in fecally contaminated food or water (fecal - oral); also by sexual contact (oral - anal)
- Associated with fever, abdominal pain, tenesmus, diarrhea (with or without blood), dysentery
- Amebae may disseminate to the liver and other organs (see Entamoeba histolytica abscess)
- See flask shaped ulcers; rarely inflammatory mass (ameboma), perforation
- Amebic trophozoites invade the submucosa, undermining the overlying mucosa; no amebic cysts in tissue
- Trophozoites with pseudopod projections, ingested RBCs in cytoplasm, small round nucleus with dot-like karyosome and peripheral rim of condensed chromatin
- Trophozoites are CD68 negative, strongly PAS positive
- Treat invasive disease with metronidazole or tinidazole; also use paromomycin to eradicate luminal cysts
Terminology
- Amebiasis, amoebiasis
ICD coding
- ICD-10:
- ICD-11:
Epidemiology
- Occurs worldwide but more common in tropical and subtropical regions (Open Forum Infect Dis 2018;5:ofy161)
- In developed countries, affected patients are usually immigrants, travelers, men who have sex with men (MSM) or institutionalized individuals
- Microscopy based detection methods overestimate the prevalence of E. histolytica due to the presence of the morphologically identical amebae, E. dispar, E. moshkovskii, E. bangladeshi and E. nuttalli (CDC: Amebiasis [Accessed 22 April 2022])
- 1 of the top 15 causes of diarrhea in children; diarrhea is a leading cause of death in children < 5 years of age (Lancet Infect Dis 2017;17:909)
- Millions of cases are estimated to occur worldwide each year; estimated 67,900 deaths in 2015 with 15,500 deaths in children < 5 years of age (Lancet 2016;388:1459)
- < 5 deaths per year reported in the United States from 1990 - 2007 (Am J Trop Med Hyg 2011;85:1038)
Sites
- Colon; cecum is the most common, followed by right colon, rectum, sigmoid and appendix (BMC Gastroenterol 2021;21:367)
- Terminal ileum is usually spared
- Skip lesions are common
- Hematogenous dissemination may occur, usually to the liver (see Entamoeba histolytica abscess); also lungs, brain
- Rectovesical fistula and fistulous involvement of the skin may also occur
Pathophysiology
- Entamoeba histolytica cysts are ingested from fecally contaminated food or water; sexual transmission also occurs (see Diagrams / tables)
- Cysts are resistant to gastric acid (and chlorine in water supplies)
- Excystation occurs in the small intestine to release trophozoites
- Trophozoites are invasive and multiply by binary fission
- Estimated that 20% of infections are associated with intestinal wall invasion
- Susceptibility to invasive infection appears to be host dependent (Trends Parasitol 2011;27:254):
- Polymorphisms in leptin receptor affect susceptibility
- Risk factors for severe disease: malnutrition, malignancy, alcoholism, immunocompromised state, pregnancy, young age
- Cell adhesion and killing by E. histolytica trophozoites (Trends Parasitol 2011;27:254):
- Gal / GalNAc lectin on E. histolytica's surface binds galactose and N-acetyle-D-galactosamine residues found on O linked sugar side chains of host colonic mucin; degrades intestinal protective mucous barrier and allows penetration of epithelium
- Parasite secretion of proteinases, contact dependent cell lysis and apoptosis and the formation of amebapores result in host cell death
- E. histolytica ingests remnant erythrocytes (hemophagocytosis)
- Some trophozoites undergo encystation through signaling pathways, completing the cycle
Etiology
- Due to E. histolytica infection
Diagrams / tables
Clinical features
- 80 - 90% of individuals with E. histolytica infection are asymptomatic (Can J Gastroenterol Hepatol 2018;2018:4601420)
- Symptoms range from mild diarrhea (most common) to severe dysentery
- Subacute onset; develops over 3 - 4 weeks with worsening diarrhea and abdominal pain
- Symptoms may also develop acutely and mimic acute abdomen
- Cases may occur where symptoms develop months after infection
- Young children may develop intussusception or necrotizing colitis, that may lead to perforation
- Rare complications are toxic megacolon, fulminant necrotizing colitis, colonic amebomas, perianal fistulas
- 50% mortality rate with fulminant necrotizing colitis (Pathog Glob Health 2012;106:245)
- Disseminated disease is more common in men (see Entamoeba histolytica abscess)
- Morphologically similar species E. dispar is nonpathogenic (does not invade); the pathogenic potential of E. bangladeshi, E. moshkovskii and E. nuttalli is not fully understood
Diagnosis
- May be suspected based on epidemiologic factors, patient symptoms, radiologic or colonoscopic findings (Open Forum Infect Dis 2018;5:ofy161)
- Definitive diagnosis of amebic colitis is made by finding trophozoites that have invaded the intestinal mucosa
- Patients with amebic liver abscesses usually have antiamebic antibodies (see Entamoeba histolytica abscess)
- Cyst aspiration is sometimes performed; although it is unusual to see parasites, the absence of other microorganisms supports evidence of amebic liver abscess
Laboratory
- E. histolytica infection is usually detected via stool microscopy (ova and parasite examination), stool antigen or stool nucleic acid testing (Open Forum Infect Dis 2018;5:ofy161)
- Positive stool exam is not definitive for amebic colitis, since 80 - 90% of infections do not cause symptoms
- Stool microscopy detects cysts or trophozoites that are morphologically consistent with E. histolytica and other morphologically identical species, but cannot usually differentiate them
- Some antigen detection or nucleic acid amplification tests (NAATs) can distinguish E. histolytica from similar appearing amebae
- NAATs are the most sensitive detection methods performed on stool
- Stool microscopy findings:
- Trophozoites measure 10 - 60 micrometers and possess a single nucleus with even peripheral chromatin and a pinpoint, often centrally located karyosome
- Ingested erythrocytes pathognomonic for E. histolytica infection; otherwise, needs to be distinguished from nonpathogenic species (e.g., E. dispar)
- Cysts are spherical, 10 - 20 micrometers in diameter; mature cysts have 4 nuclei and chromatoid bodies with bluntly rounded ends
- Serologic testing for E. histolytica antibodies supports the diagnosis of amebiasis but cannot differentiate current from past infection
- Most useful for diagnosing disseminated disease
Radiology description
- Evidence of colitis may be seen on CT (Jpn J Radiol 2021;39:558):
- Acute colitis: nonspecific diffuse wall thickening, submucosal edema with stratified or target patterns (contrast enhanced CT)
- Chronic colitis: prominent thickened wall; may mimic malignancy
- Most common pattern: involvement of cecum and rectum with sparing of the terminal ileum
- Plain film radiographs using barium may reveal ulcerative changes
- Ameboma: localized wall thickening with minimal contrast enhancement on CT
- Fulminant necrotizing colitis:
- Prominent thickened wall on contrast enhanced CT with a thin enhancing rim
- Contiguous involvement or skip lesions
- Ultrasonography and CT can be used for detection of liver abscess
Case reports
- 40 year old man with fulminant necrotizing amebic colitis following receipt of corticosteroids for severe COVID-19 (BMJ Case Rep 2021;14:e246110)
- 43 year old married couple with amebic colitis treated with paromomycin monotherapy (PLoS Negl Trop Dis 2020;14:e0008013)
- 54 year old man with cecal amebiasis mimicking inflammatory bowel disease (J Int Med Res 2020;48:300060520922379)
- 56 year old man with advanced HIV infection requiring emergent subtotal colectomy of invasive intestinal amebiasis (J Clin Microbiol 2018;56:e01703)
- 67 year old man with sexually acquired amebiasis (BMJ Case Rep 2019;12:e228942)
- Patient with 2 different types of objects seen in a trichrome stained stool specimen (Pritt: Creepy Dreadful Wonderful Parasites Blog - Case of the Week 546 [Accessed 13 October 2023])
Treatment
- Amebic colitis is treated with both an amebicidal and luminal agent (Open Forum Infect Dis 2018;5:ofy161)
- Metronidazole or tinidazole amebicides, to target invading trophozoites
- Paromomycin to eradicate luminal cysts and prevent relapse / transmission to others
- Complicated disease may also require surgical resection of perforated / necrotic bowel, fluid resuscitation, broad spectrum antimicrobials for peritonitis
Gross description
- Discrete, sharply defined ulcers and erosions with smooth, irregularly shaped borders (BMC Gastroenterol 2021;21:367, AFIP: Topics on the Pathology of Protozoan and Invasive Arthropod Diseases [Accessed 22 April 2022])
- Ulcers with white or yellow exudates, bloody exudates
- Normal intervening mucosa
- Ulcers may coalesce, resulting in larger lesions that may be necrotic in the center
- May show areas of colitis or inflammatory polyps
- Ameboma (amebic pseudotumor) presents as firm, well defined, annular inflammatory thickening of the colon wall, usually in the cecum or ascending colon; commonly causes a napkin ring deformity
Gross images
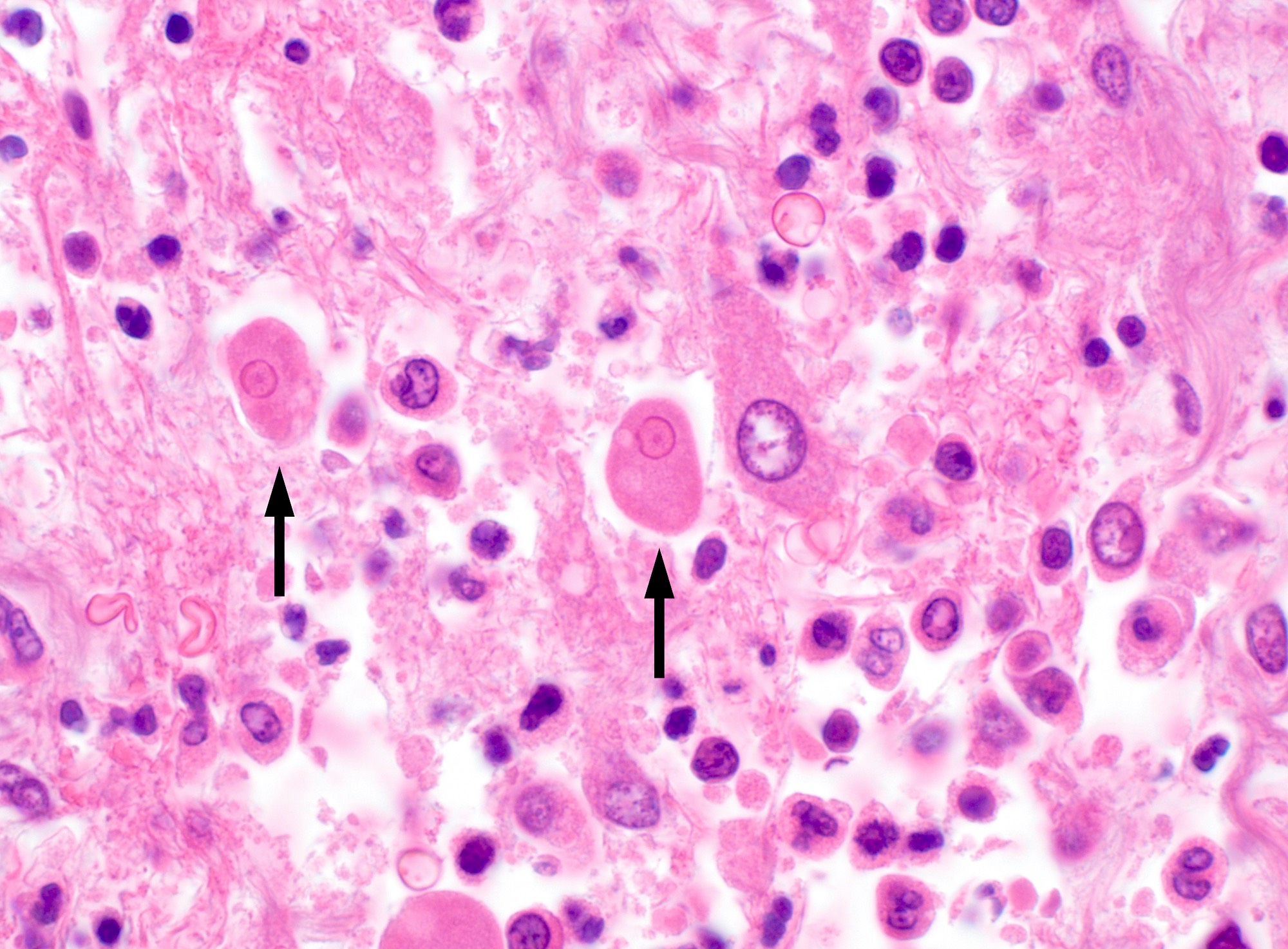
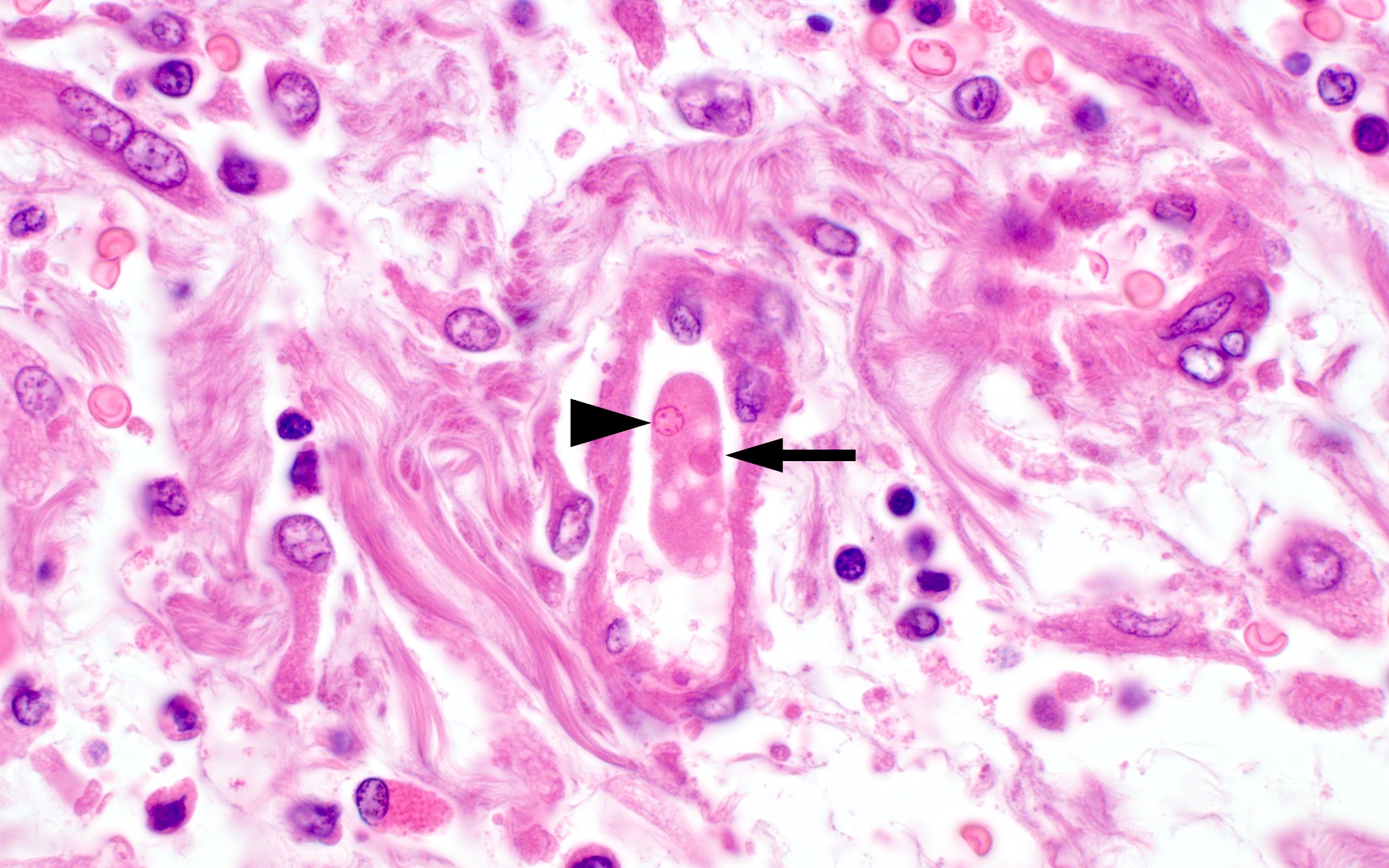
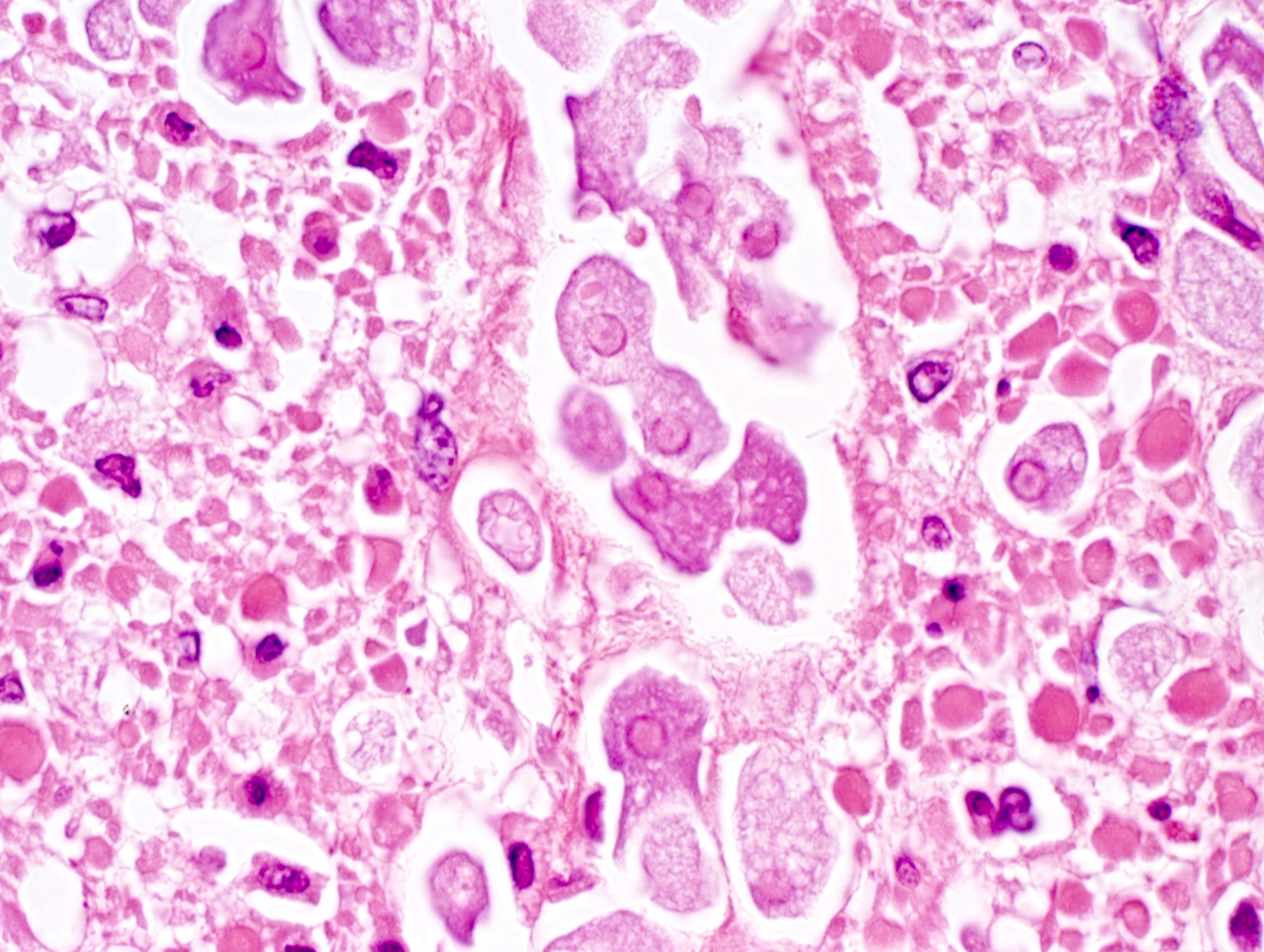
Microscopic (histologic) description
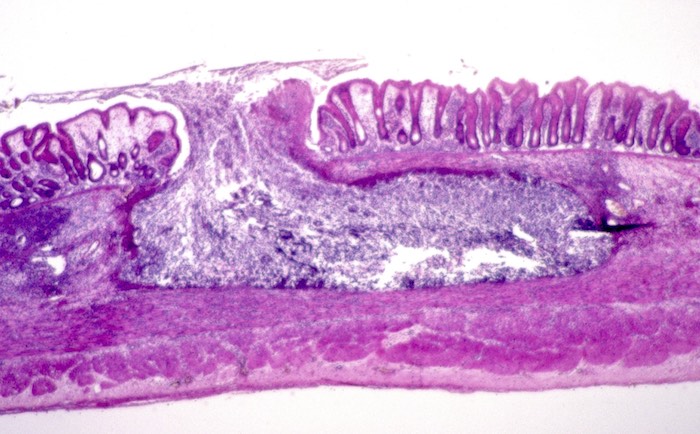
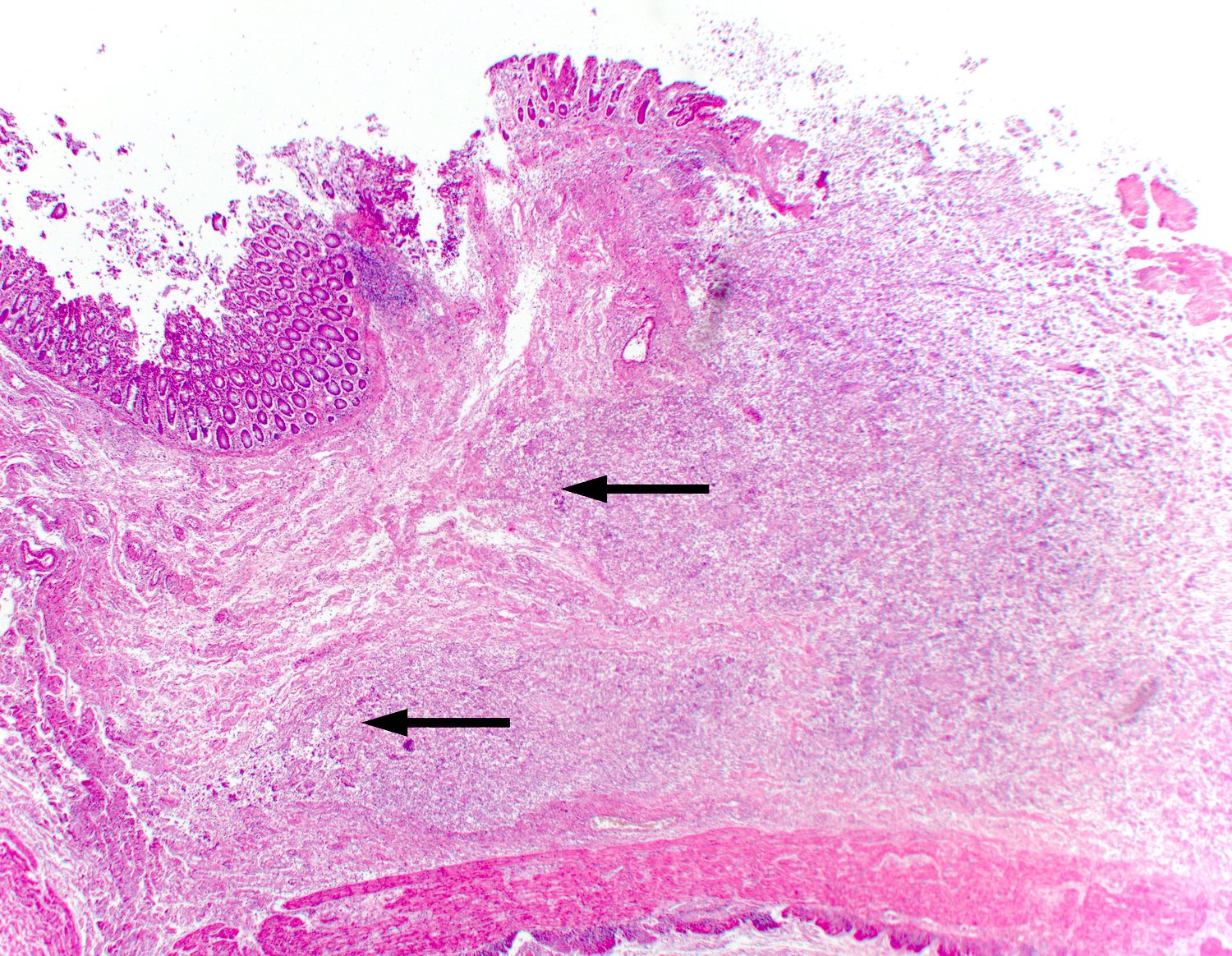
- Lesions begin with superficial mucosal necrosis and progress to erosions and ulcers (AFIP: Topics on the Pathology of Protozoan and Invasive Arthropod Diseases [Accessed 22 April 2022])
- Overlying inflammatory exudates consist of necrotic material, fibrin and inflammatory cells, and often contain E. histolytica trophozoites
- Chronic cryptitis and crypt architectural distortion may be seen
- Mature ulcers are flask shaped, with a base that is broader than the apex; undermines the overlying mucosa
- Ulcer crater is composed of cellular debris, fibrin and trophozoites
- Minimal inflammation initially; later includes neutrophils, histiocytes, lymphocytes, plasma cells and occasionally eosinophils within and around the ulcer
- Amebic trophozoites are best appreciated at the border of viable and necrotic tissue
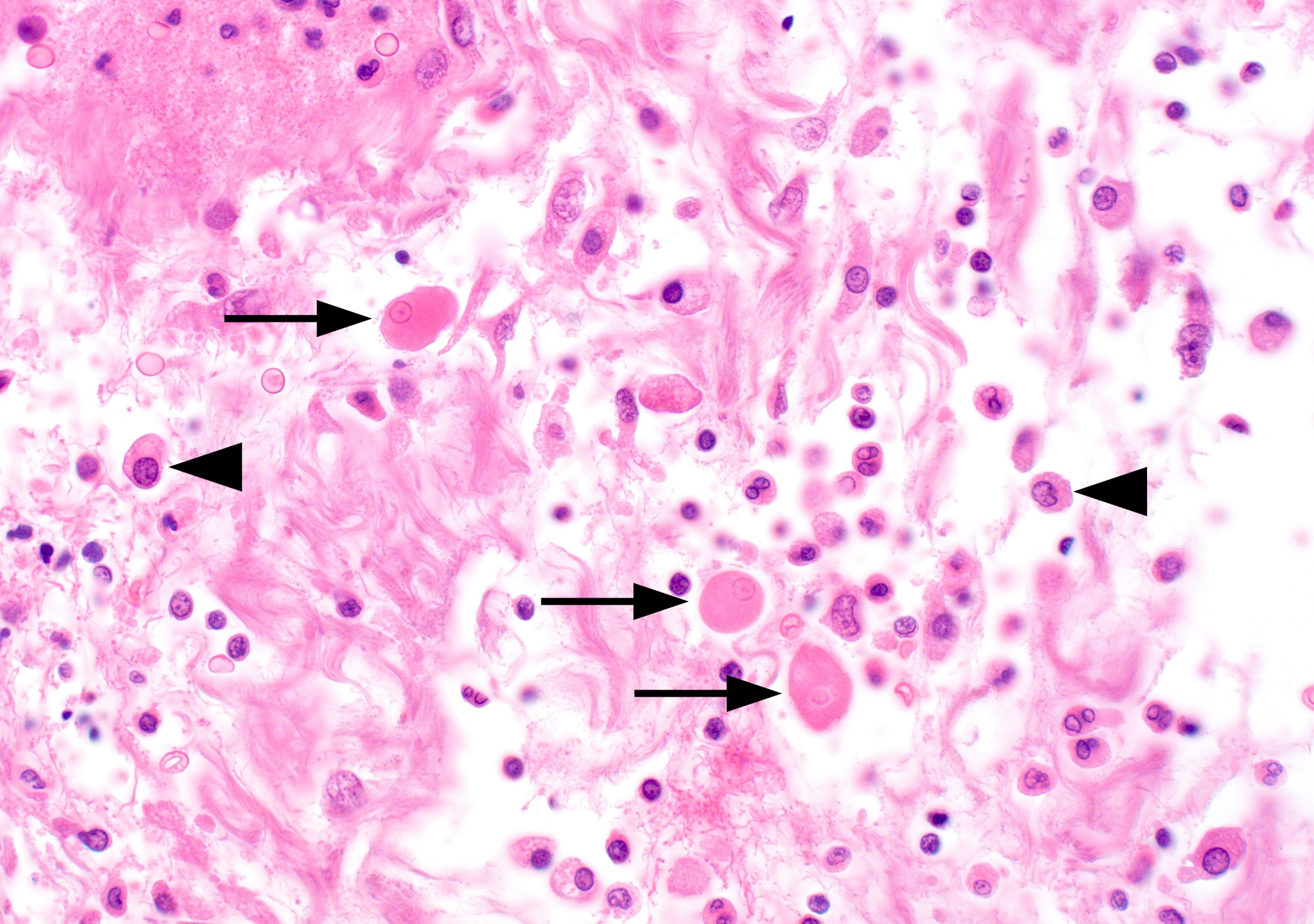
- Trophozoites of Entamoeba histolytica are 10 - 60 micrometers and may resemble macrophages
- Round to oval with pseudopod projections
- Commonly surrounded by a halo in FFPE tissue preparations; caused by retraction during fixation or by parasite toxins
- Cytoplasm is abundant, vacuolated, pink-purple on H&E, and may contain ingested red blood cells
- Nuclei are small and round with a prominent rim of peripheral chromatin and a small, dot-like central karyosome
- Amebomas are comprised of granulation tissue, chronic inflammatory cells and fibrosis
- Clusters of trophozoites are usually seen near submucosa ulcerations
- In trichrome stained stool specimens, peripheral chromatin and discrete karyosome are supportive of E. histolytica / E. dispar (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 546 [Accessed 13 October 2023])
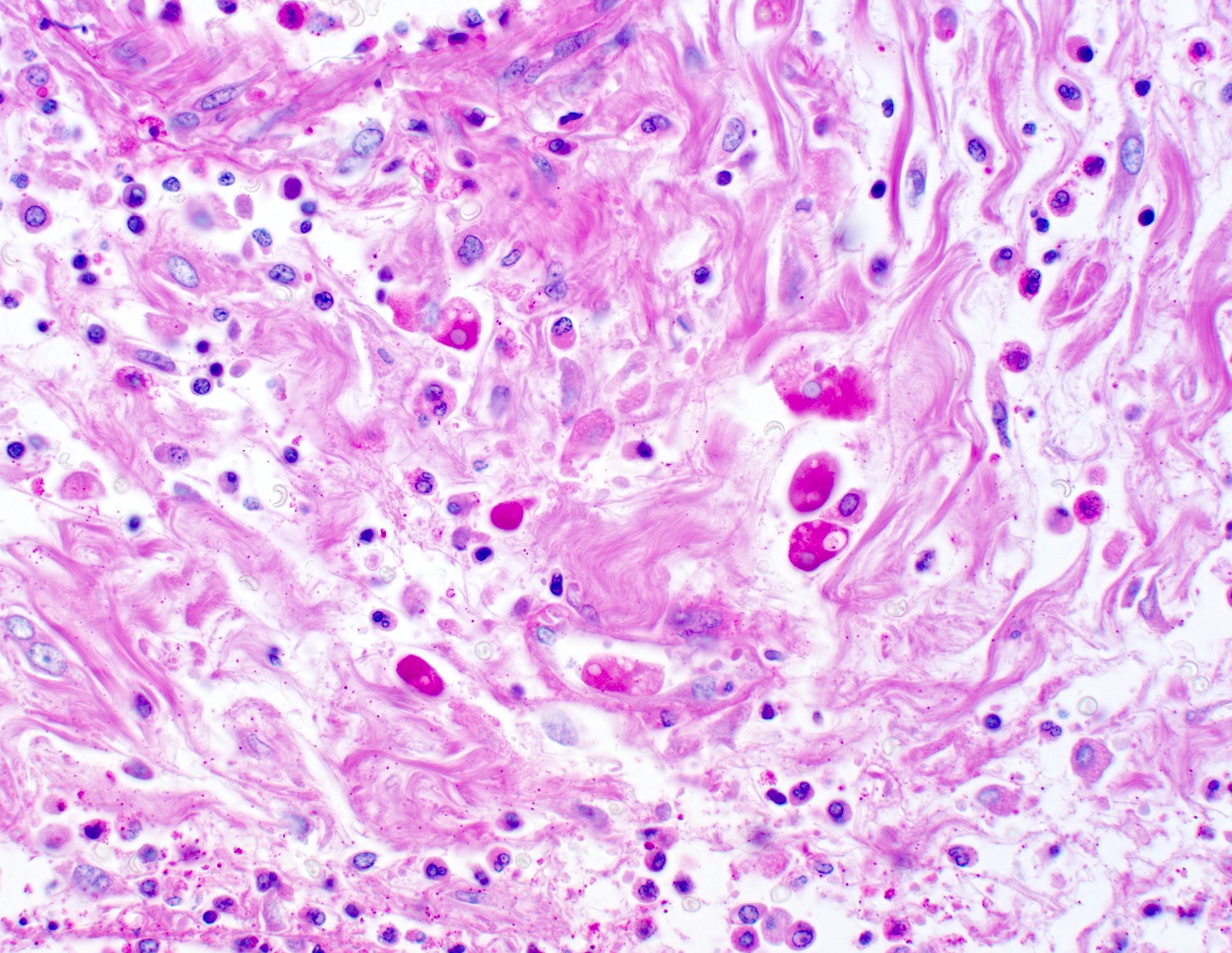
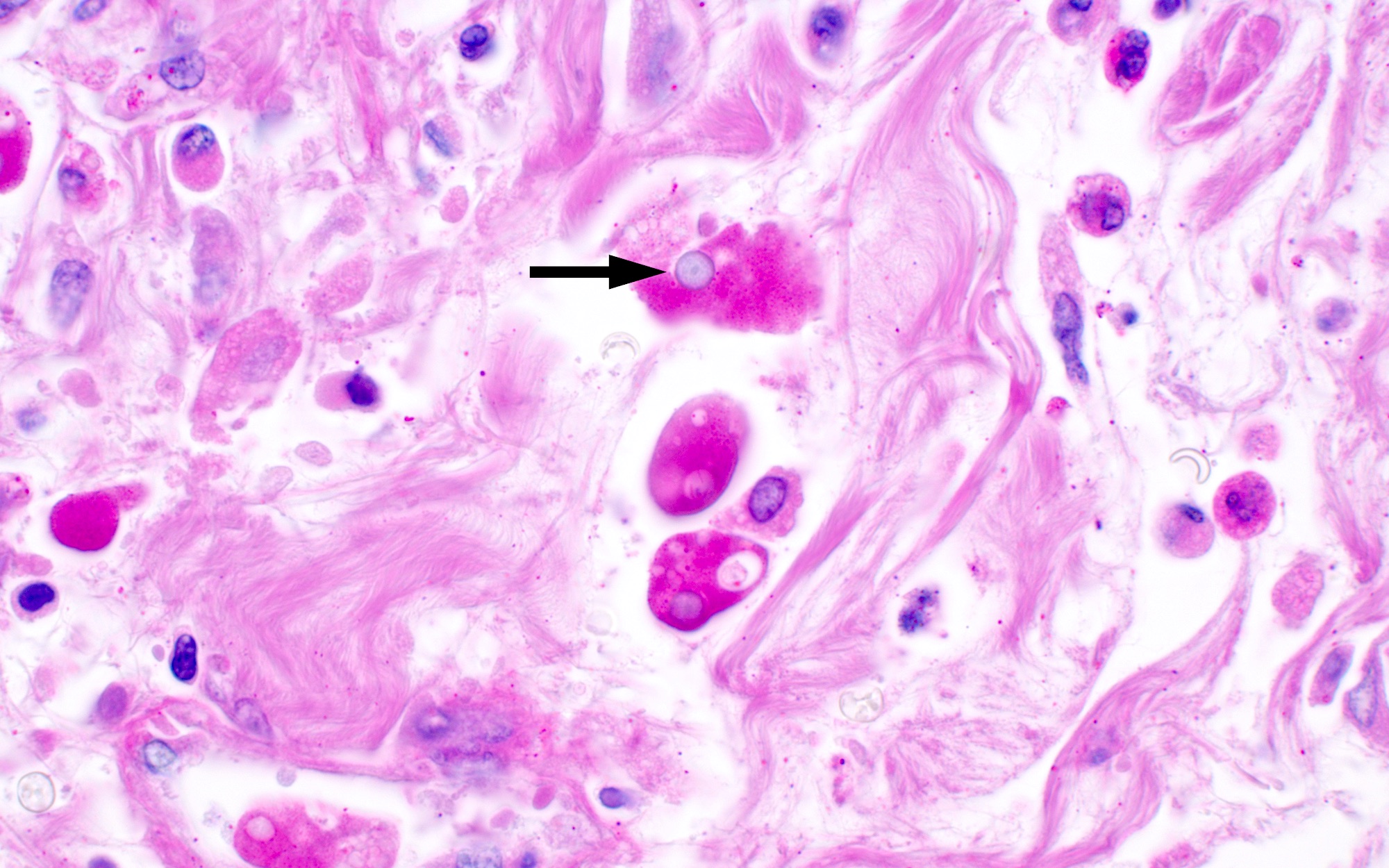
Microscopic (histologic) images
Positive stains
- Periodic acid Schiff (PAS) highlights amebic trophozoites by staining them deep pink / magenta
- There are no commercially available IHC stains for E. histolytica
- Reference: AFIP: Topics on the Pathology of Protozoan and Invasive Arthropod Diseases [Accessed 22 April 2022]
Negative stains
- CD68 is negative in amebae, allowing for differentiation from macrophages (AFIP: Topics on the Pathology of Protozoan and Invasive Arthropod Diseases [Accessed 22 April 2022])
Sample pathology report
- Colon, cecum, biopsy:
- Intestinal amebiasis (see comment)
- Comment: The biopsy shows mucosal ulceration with an overlying fibrinous exudate. Within the ulcer bed and exudate are numerous trophozoites of the protozoan pathogen, Entamoeba histolytica, which extend into the submucosa but not into the underlying muscular layer. The trophozoites are readily identified by their abundant dense bubbly cytoplasm and small round nucleus with peripheral rim of condensed chromatin and central dot-like karyosome. Some trophozoites contain ingested erythrocytes. The trophozoites are highlighted with PAS, which stains their cytoplasm deep magenta.
Differential diagnosis
- Appendicitis:
- Acute inflammation
- No infiltrating trophozoites
- Balantidium coli (Balantioides coli):
- Flask shaped ulcers resembling amebiasis
- Large (40 - 200 micrometers) ciliated trophozoites invading the mucosa and submucosa
- Crohn's disease:
- Active chronic colitis
- No infiltrating trophozoites
- Histiocytes (also known as tissue macrophages):
- Present in various inflammatory and infectious conditions
- Similar size to Entamoeba histolytica trophozoites
- Large, often reniform nucleus (versus small round nucleus of E. histolytica)
- CD68+
- Nonpathogenic ameba
- Pseudomembranous colitis:
- Mucopurulent exudate erupts out of crypts to form a mushroom-like layer of karyorrhectic debris and neutrophils that adheres to the epithelial surface
- Crypt necrosis
- Superficial lamina propria with neutrophilic inflammation and some capillary fibrin thrombi
- No infiltrating trophozoites
- Pyogenic abscess (in liver)
- Tuberculosis
- Ulcerative colitis:
- Active chronic colitis
- No infiltrating trophozoites
Additional references
Board review style question #1
A 47 year old man living in Mexico presented with 3 months of gradually increasing abdominal pain and diarrhea. The initial diagnostic workup was unrevealing, so a colonoscopy was performed, which revealed several well demarcated ulcers in the cecum and ascending colon. Biopsies of the ulcers were obtained and above is a representative image of the histopathologic findings. What is the diagnosis?
- Amebiasis
- Balantiosis
- Signet ring carcinoma
- Toxic drug injury
Board review style answer #1
Board review style question #2
Which of the following histochemical stains is useful for highlighting invasive trophozoites of Entamoeba histolytica?
- Alcian blue
- Giemsa
- Masson trichrome
- Mucicarmine
- Periodic acid Schiff
Board review style answer #2