Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Prosser N, Gupta R. Basal cell adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsbasalcelladenocarcinoma.html. Accessed August 29th, 2025.
Definition / general
- Primary biphasic carcinoma of the salivary glands; composed of basal and ductal cells (Surg Pathol Clin 2021;14:25)
Essential features
- Biphasic, low grade malignancy of salivary gland
- Parotid is the most common location; rare in other salivary glands and minor salivary gland tissue
- Histologic features similar to basal cell adenoma but with evidence of invasive growth pattern
- Diagnosis based on demonstration of a dual cell population of centrally located ductal cells and abluminal basal cells with peripheral palisading of nuclei
- Squamous and sebaceous differentiation may be seen
- Surgery with clear margins is the mainstay of treatment
Terminology
- Basal cell adenocarcinoma (BCAC)
- Use of other terminology is not recommended
ICD coding
- ICD-O: 8147/3 - basal cell adenocarcinoma
Epidemiology
- Rare primary salivary gland tumor, accounting for < 1 - 2% of salivary gland malignancies
- Wide age range (40 - 90)
- Most frequent in adults in seventh to eighth decade; exceedingly rare in children
- Slight female predominance (F:M = 1.2:1) (Surg Pathol Clin 2021;14:25)
Sites
- Parotid (75 - 90%), submandibular, minor salivary gland of oral cavity
Etiology
- Arises from pluripotential, ductal and myoepithelial cells
- Majority arise de novo; approximately 25% of cases arise from basal cell adenoma (Cancer 1996;78:2471)
- Rare examples may occur in the context of familial cylindromatosis syndromes, such as Brooke-Spiegler syndrome (Surg Pathol Clin 2021;14:25)
Clinical features
- Slow growing, painless mass; often present for many years
- Rare association with dermal cylindromas (Case Rep Radiol 2012;2012:249583)
- ~50% recur locally; 15% metastasize to lymph nodes, rarely to lungs (Head Neck Pathol 2015;9:205, Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
Diagnosis
- Imaging modalities for workup of salivary gland neoplasms include ultrasonography, CT and MRI (Otolaryngol Head Neck Surg 2021;164:27)
- Cytologic diagnosis exceedingly difficult due to morphologic overlap with other more common biphasic salivary gland neoplasms, including pleomorphic adenoma and adenoid cystic carcinoma (Diagn Pathol 2013;8:171)
Radiology description
- No specific radiological findings
Prognostic factors
- BCAC is a low grade malignant tumor with good long term prognosis; death from disease is rarely reported (Head Neck Pathol 2015;9:205, Head Neck Pathol 2009;3:69)
- May be locally destructive and recurrences are seen in 50%, up to 10 years later (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
- Poorer prognostic features include location in minor salivary gland, advanced stage, incomplete excision and recurrence (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
Case reports
- 57 year old man with epistaxis and decreased hearing for 1 month duration, found to have a nasopharyngeal tumor (BMC Cancer 2018;18:878)
- 66 year old woman with 2 year history of slow growing painless mass in parotid (Turk Arch Otorhinolaryngol 2017;55:187)
- 86 year old man with diplopia, epistaxis and buccal swelling (SAGE Open Med Case Rep 2021;9:2050313X211048041)
Treatment
- Surgical resection of tumor with clear margins is first line treatment (Oncotarget 2017;8:3946)
- Neck dissection if evidence of lymph node metastases present (Oncotarget 2017;8:3946)
- Postoperative radiotherapy if adverse prognostic features present or lesion originating in minor salivary gland (Arch Pathol Lab Med 2007;131:1602)
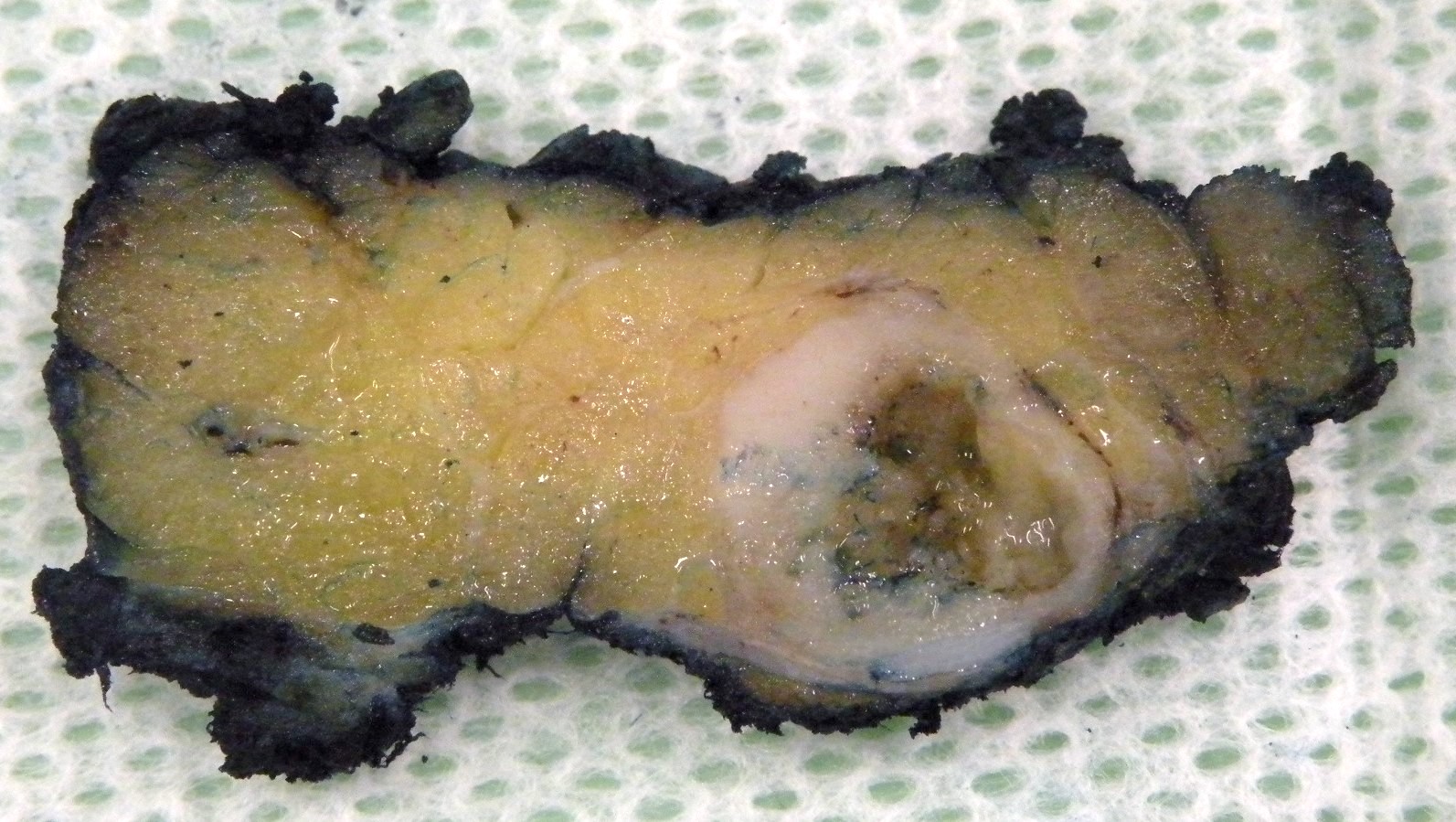
Gross description
- Typically presents as a well circumscribed, unencapsulated lesion
- Solid to focally cystic with white / cream to tan cut surface
- Size usually < 5 cm (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
Gross images
Frozen section description
- Should not be used; diagnosis may not be possible on frozen section
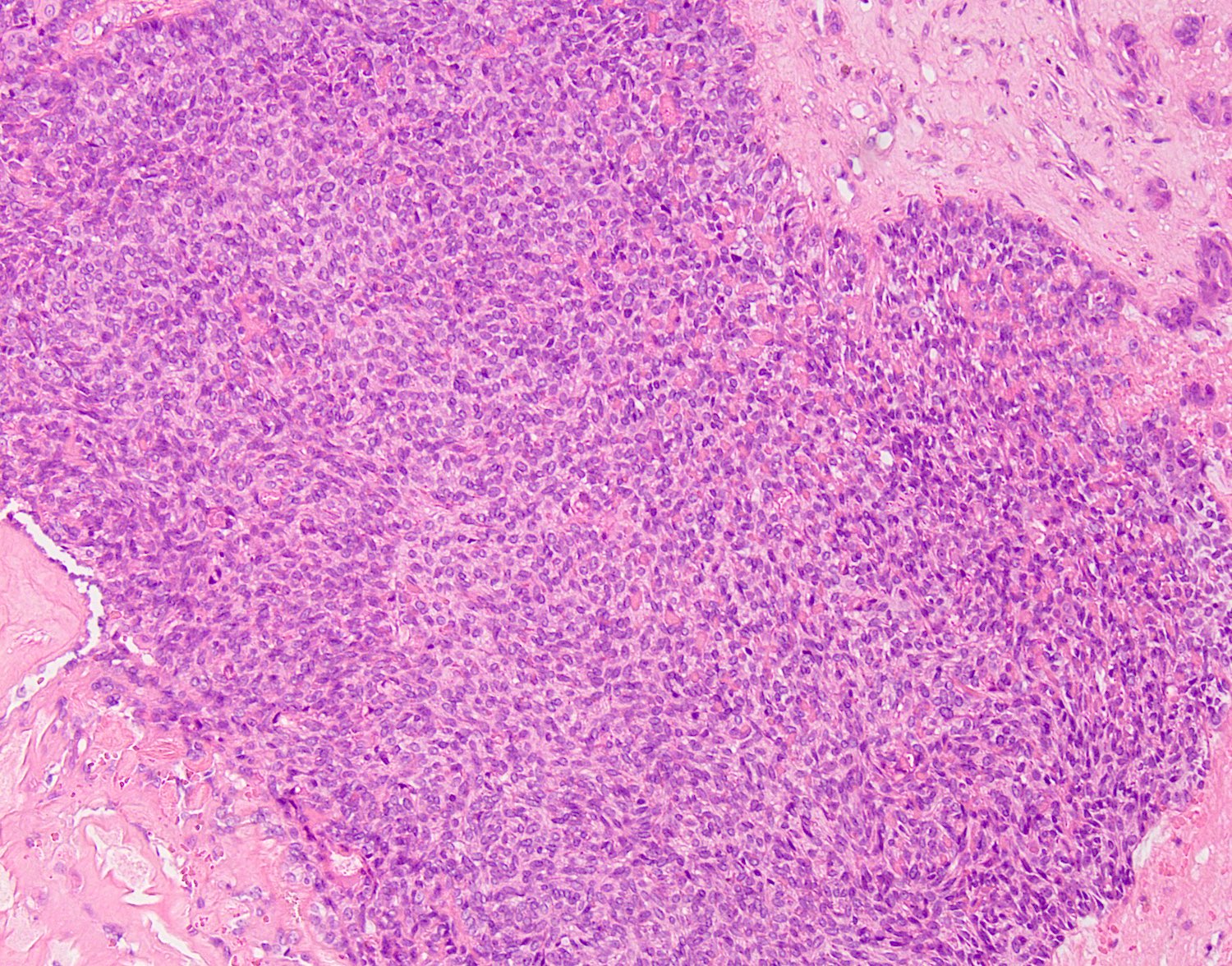
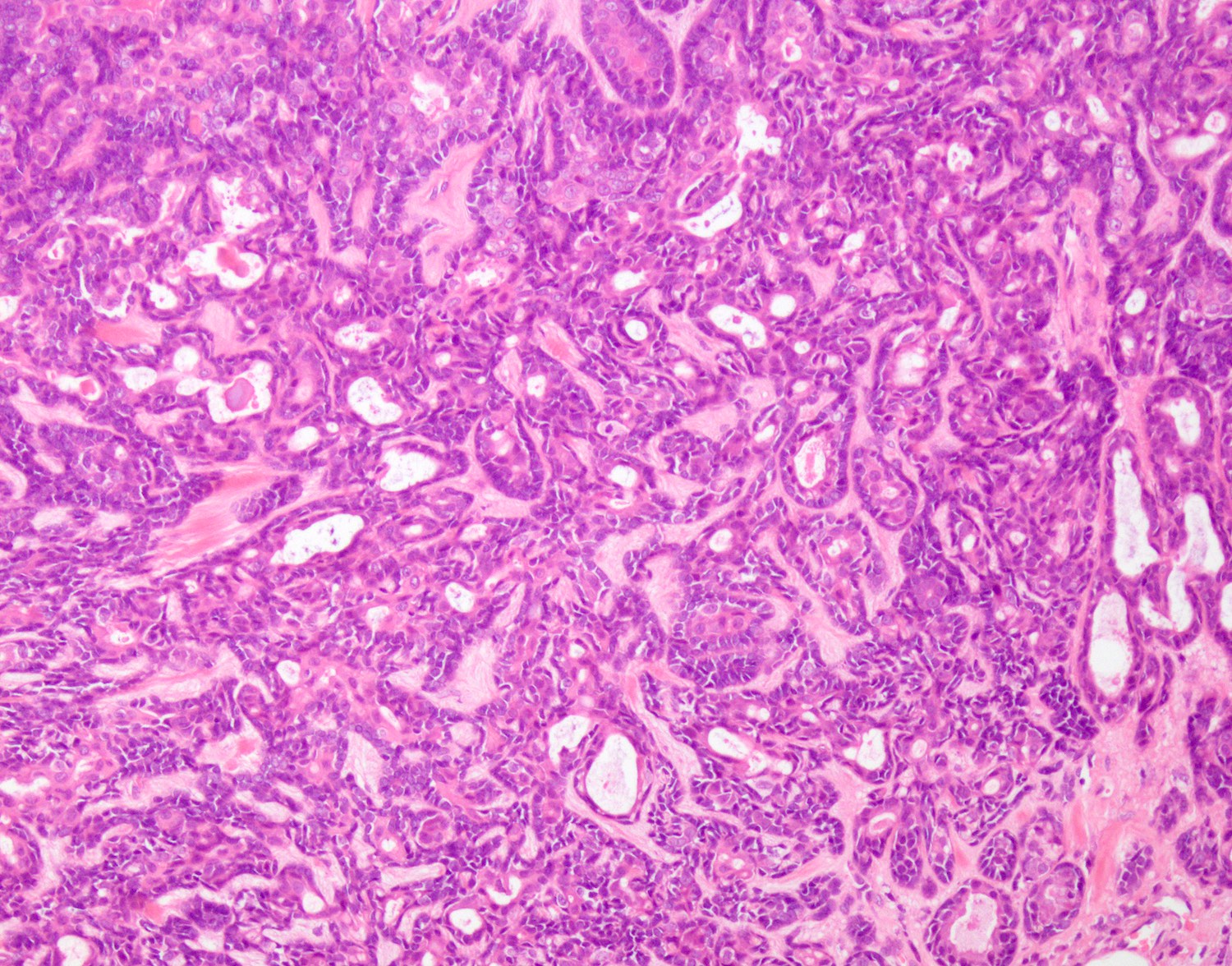
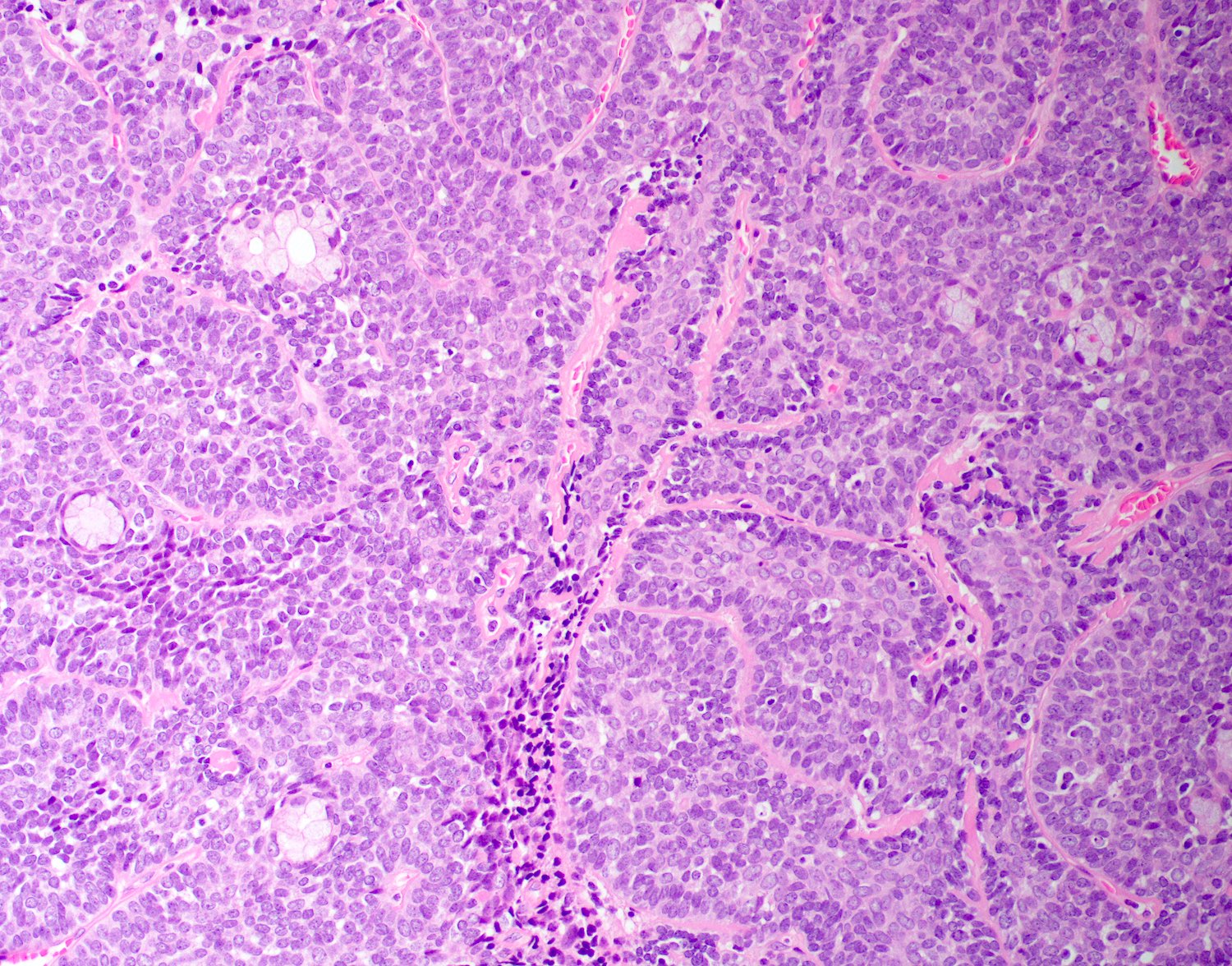
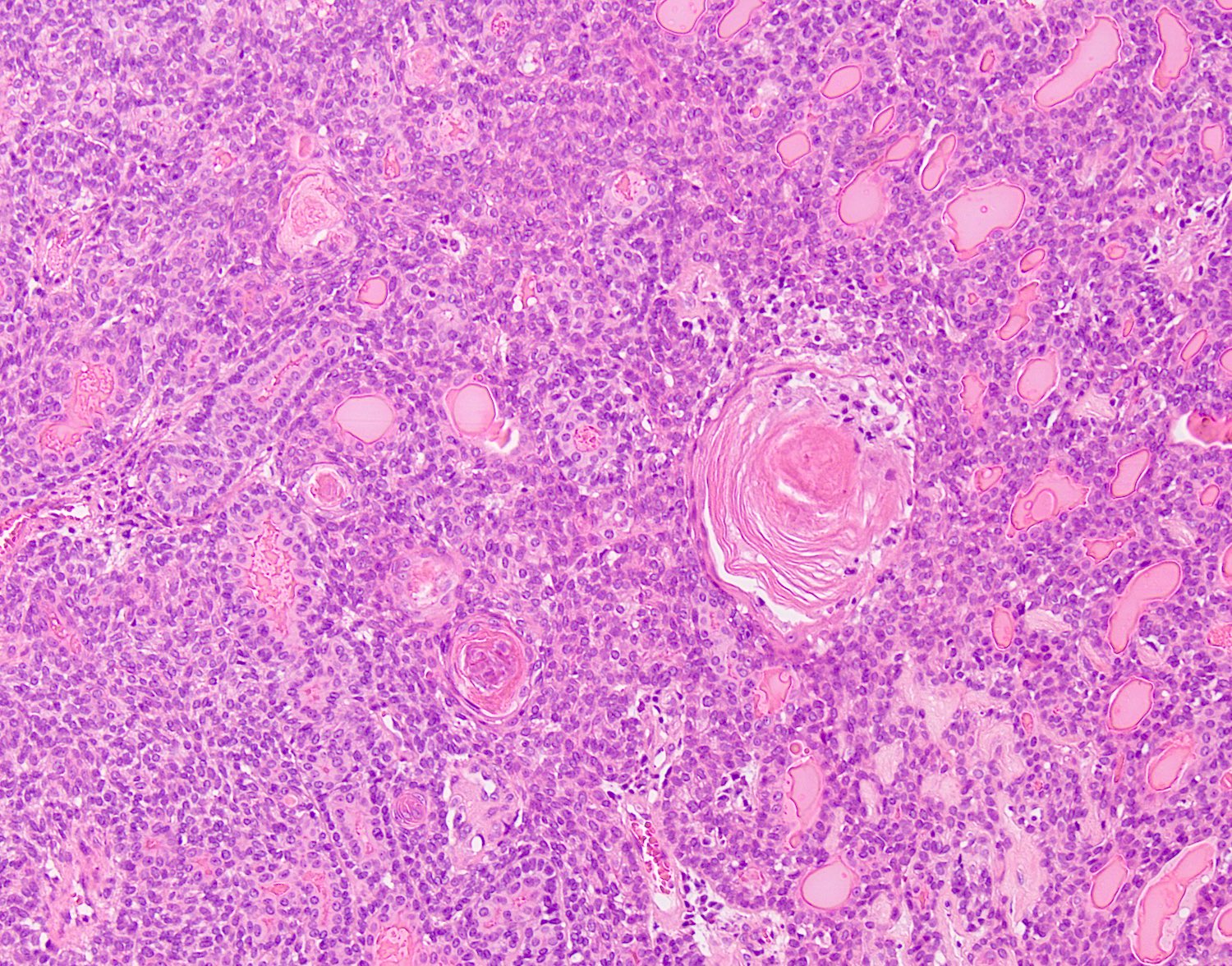
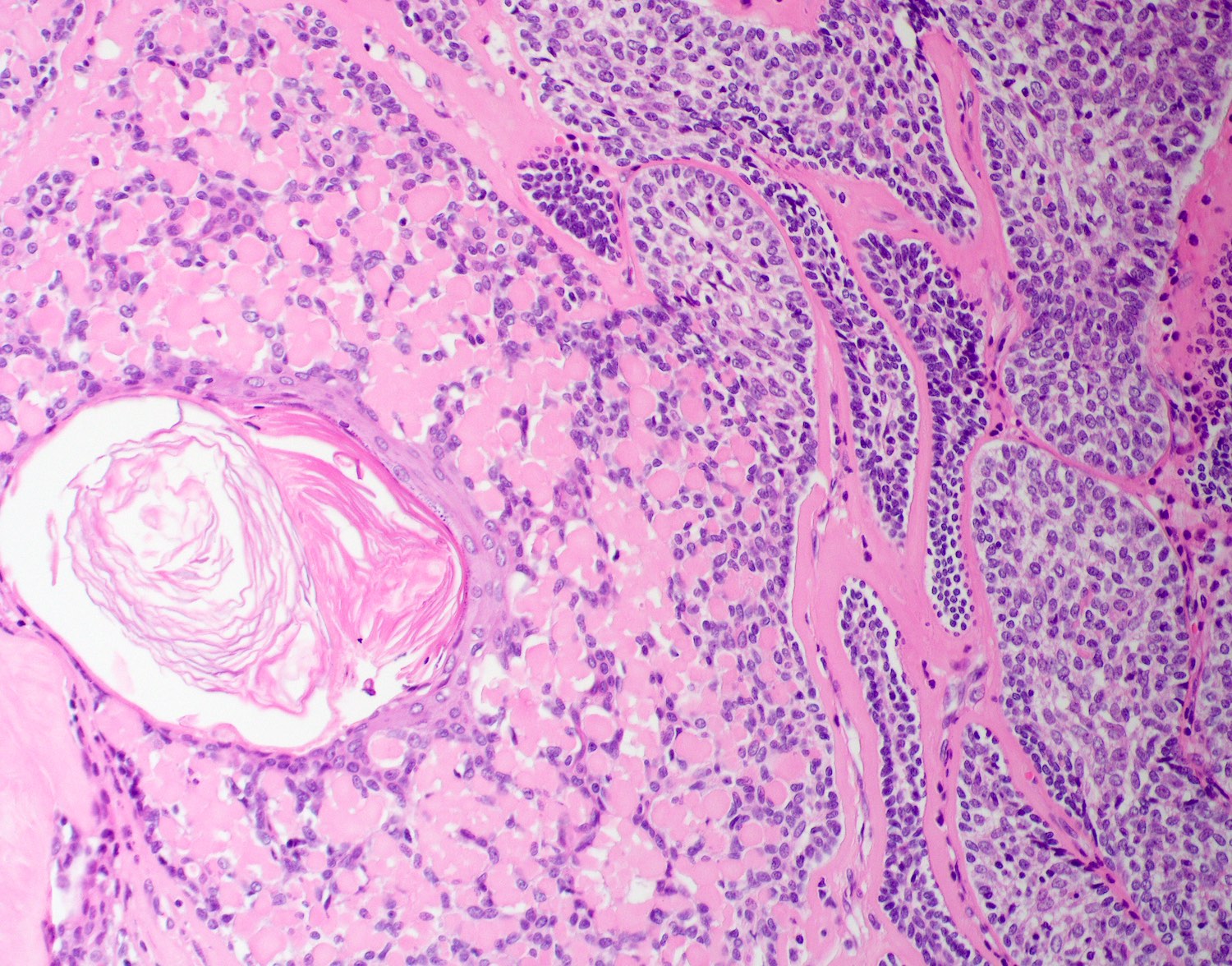
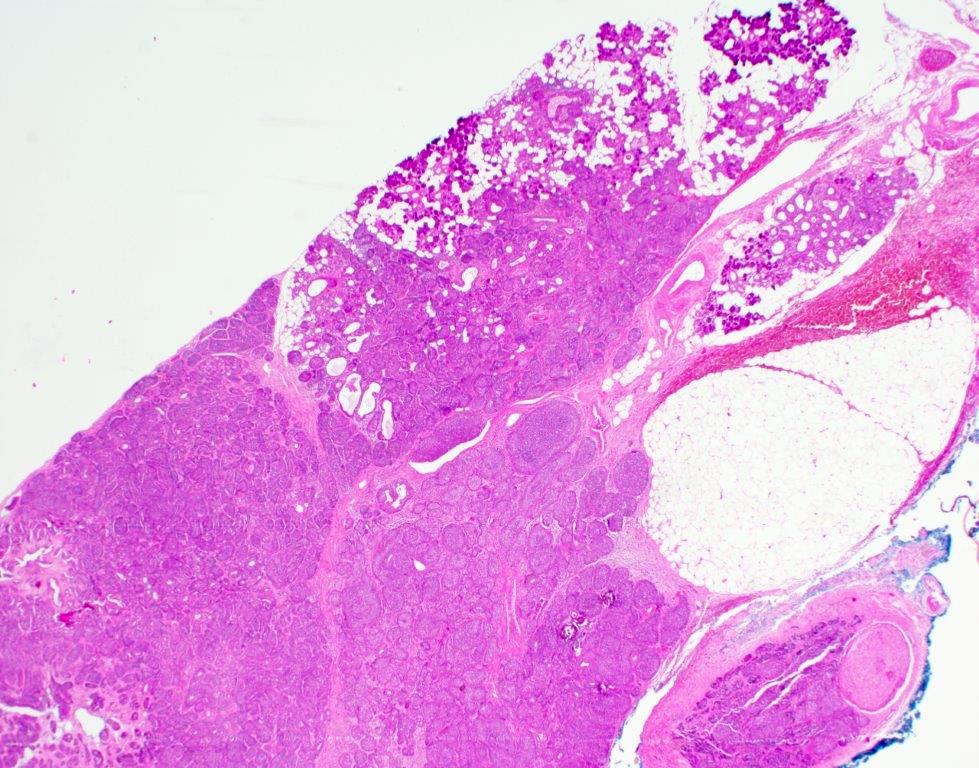
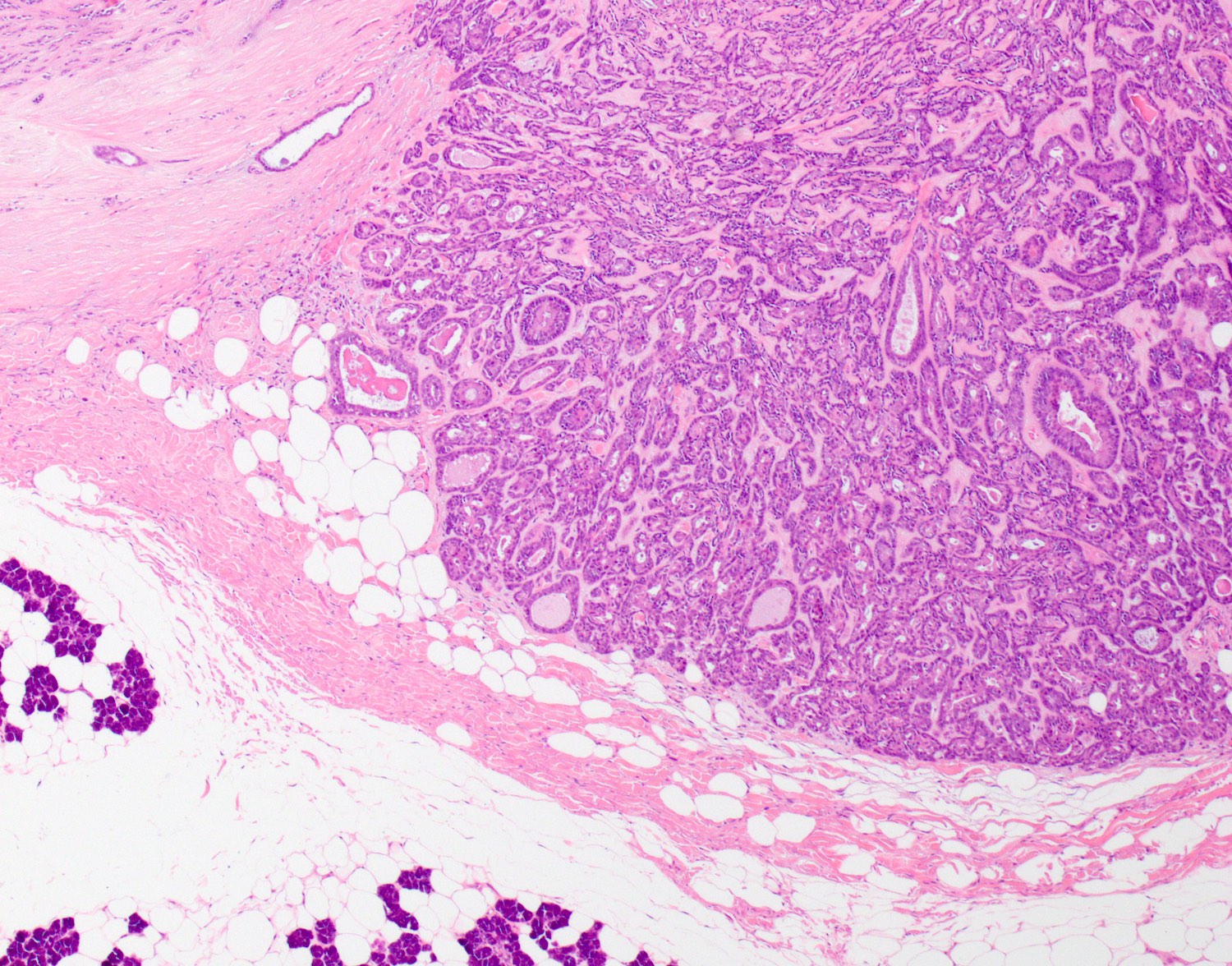
Microscopic (histologic) description
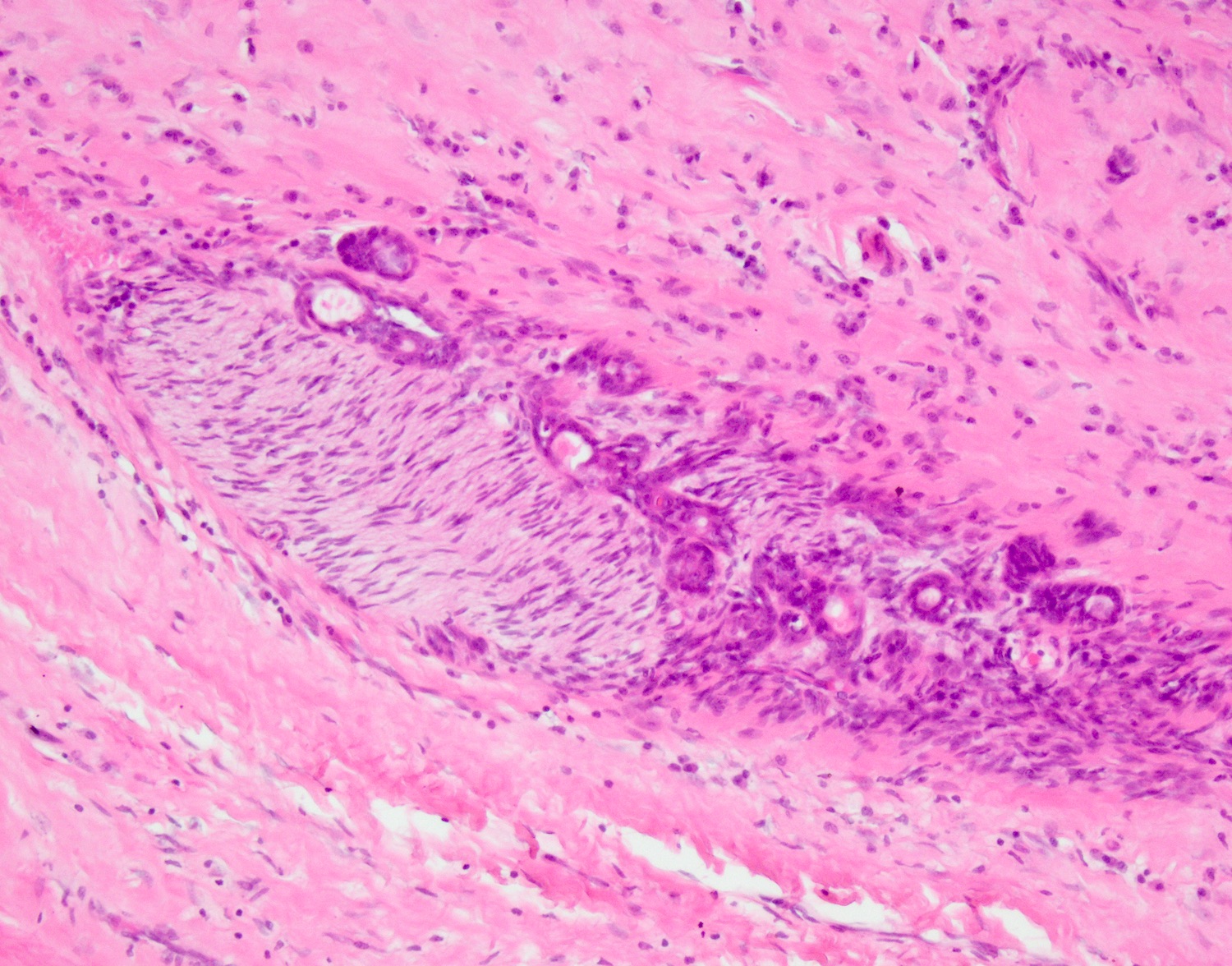
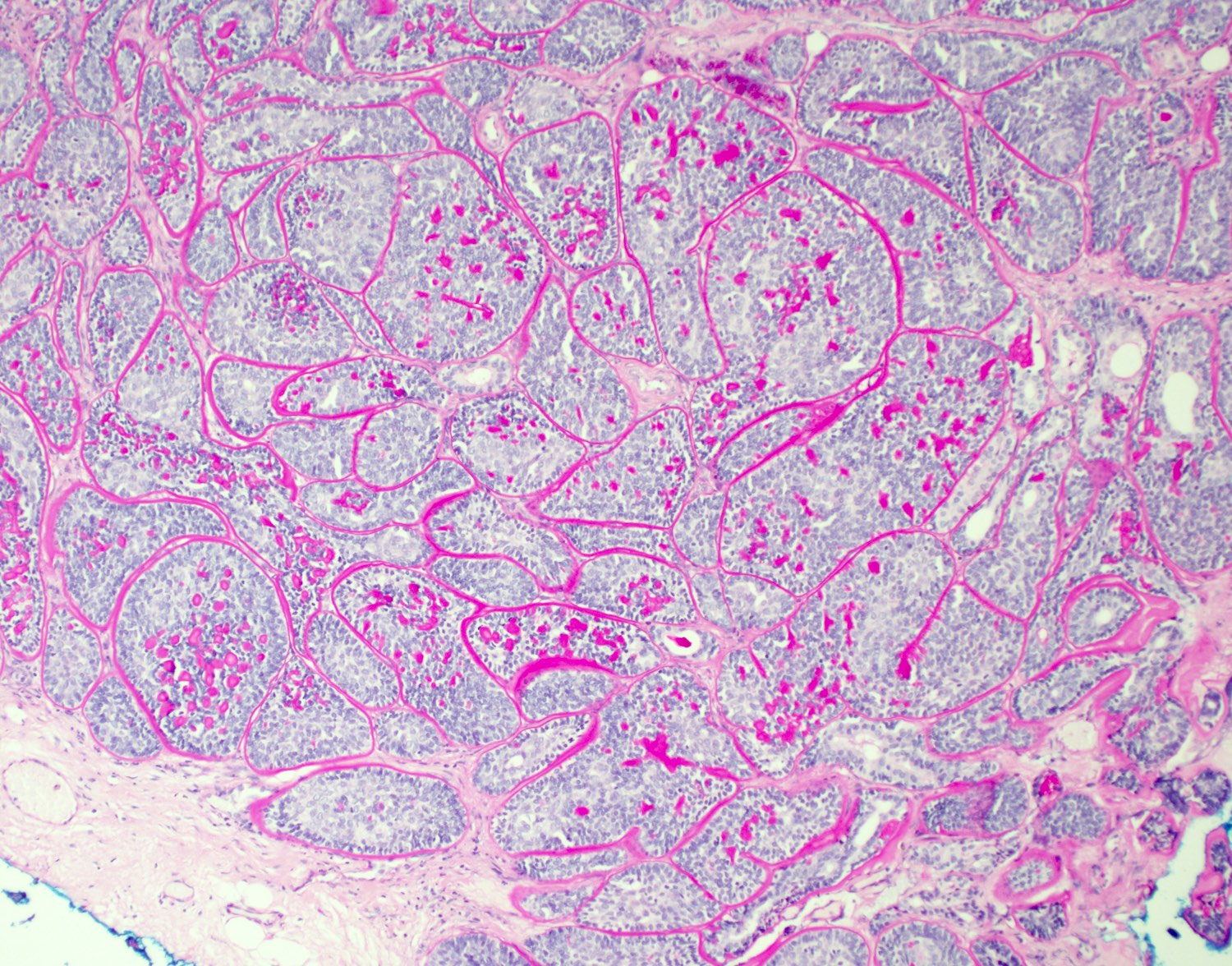
- Unencapsulated, with circumscribed to infiltrative edges with infiltration into salivary gland parenchyma, fat, nerve or lymphovascular spaces (Head Neck Pathol 2015;9:205, Diagn Pathol 2013;8:171)
- Solid, trabecular, tubular and membraneous growth patterns (Head Neck Pathol 2015;9:205)
- Biphasic tumors with central ductal cells and abluminal basal cells (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
- Ductal cells appear cuboidal, with moderate amounts of eosinophilic cytoplasm and round to ovoid nuclei (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
- Basal cells show scanty cytoplasm and hyperchromatic ovoid nuclei (Head Neck Pathol 2015;9:205)
- Nuclear palisading of the peripheral basal cells is seen (Head Neck Pathol 2015;9:205)
- Basement membrane-like eosinophilic material separates nests (Head Neck Pathol 2015;9:205)
- Squamous and sebaceous differentiation may be present (J Clin Pathol 2000;53:153)
- Necrosis may be seen in 45% of tumors, with an increase in mitoses (Thompson: Diagnostic Pathology - Head and Neck, 2nd Edition, 2016)
Microscopic (histologic) images
Contributed by Natasha Prosser, B.Sc., M.B.B.S. and Ruta Gupta, M.D.
Cytology description
- Cytologic diagnosis of basal cell adenocarcinoma is exceedingly difficult as the smears show a dual cell population and are rich in stroma, similar to several biphasic salivary gland neoplasms:
- Cellular smears with irregular cohesive cell clusters
- Small and intermediate sized basaloid cells with peripheral palisading
- Dense, nonfibrillary stroma at the periphery of cell groups
- Malignant features with nuclear atypia, mitotic activity or necrosis are rare
- References: Diagn Cytopathol 2015;43:432, Acta Cytol 2018;62:346, Cibas: Cytology - Diagnostic Principles and Clinical Correlates, 5th Edition, 2020
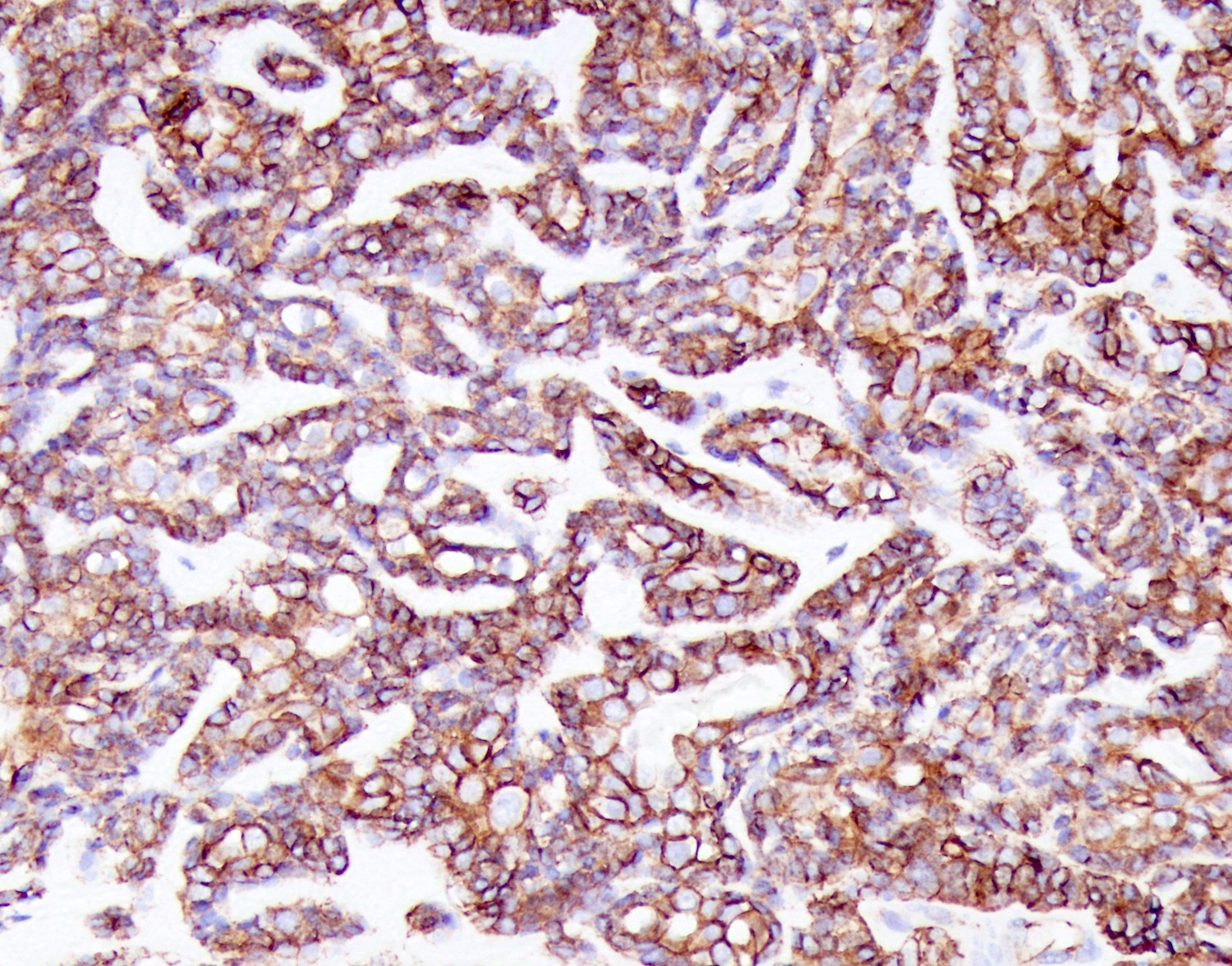
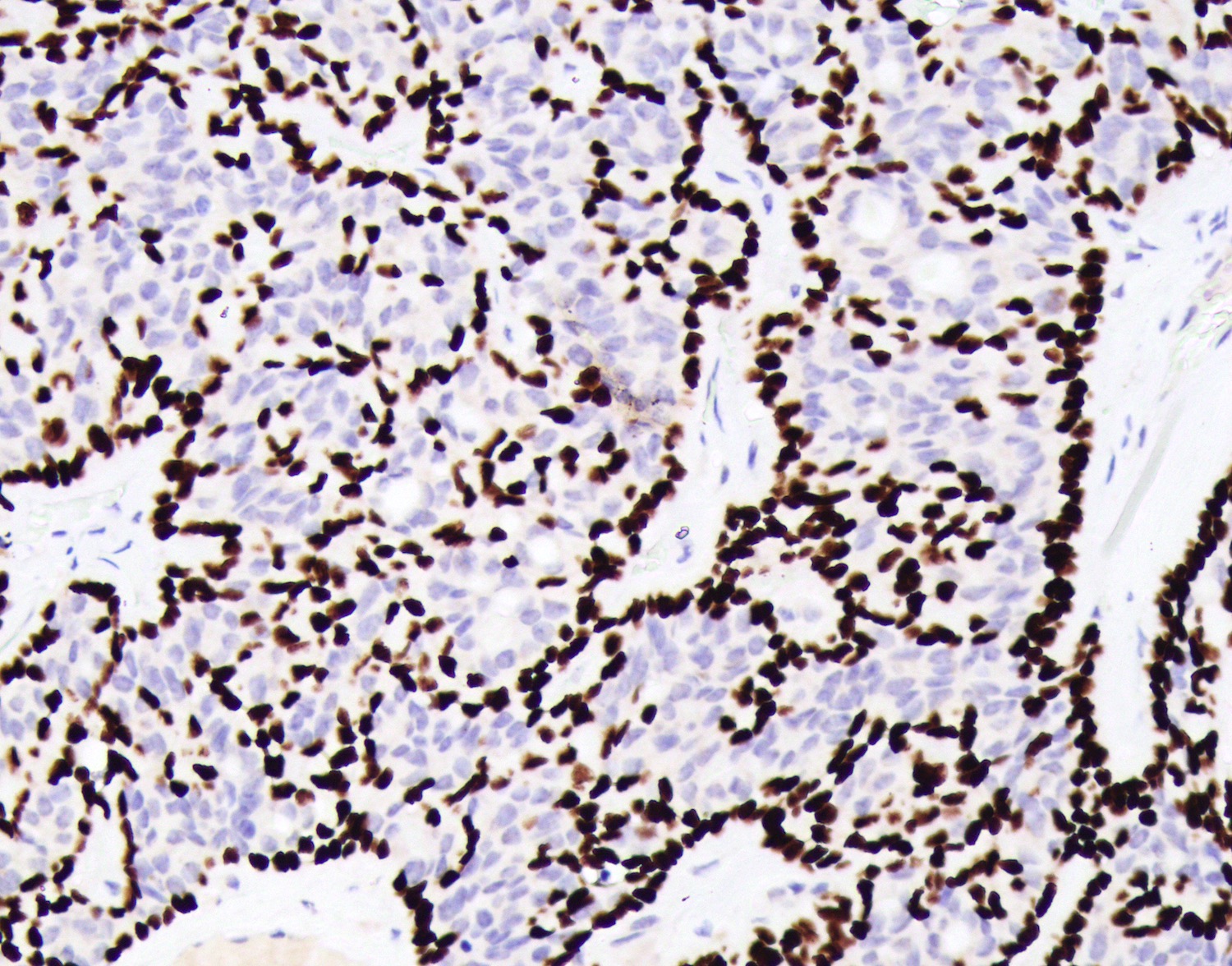
Positive stains
- Pancytokeratin, CK7
- CEA-M luminal cells
- p63, p40, S100, calponin in basal / myoepithelial cell
- CK5/6 highlighting areas of squamous differentiation (Surg Pathol Clin 2021;14:25)
Negative stains
Electron microscopy description
- Not used in routine practice
- Ultrastructural features identical for basal cell adenoma and BCAC
- Cells show basal, myoepithelial and ductal differentiation
- Excess basal lamina, marginally and intercellularly seen around nonluminal cells
- Reference: Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:485
Molecular / cytogenetics description
- CYLD alterations, usually in membranous type (Mod Pathol 2018;31:1064)
Sample pathology report
- Left superficial parotid, excision:
- Basal cell adenocarcinoma (see comment)
- Comment: The sections show a partly encapsulated tumor composed of anastomosing tubules and ductules with a prominent hyaline stroma. In most areas, there appears to be a double cell layer, with CK7 positive pale cells surrounded by SMA positive darker cells abutting the hyaline stroma. There is invasion of adipose tissue with an extension close to the parotid gland. No perineural invasion was found. The tumor is 0.8 mm from the nearest inked margin of excision. Mitoses are sparse.
Differential diagnosis
- Basal cell adenoma:
- Well circumscribed, no invasion / infiltration into adjacent tissues
- Multifocal or membranous type can simulate invasion
- Nuclear beta catenin+
- Pleomorphic adenoma:
- Presence of myxoid / chondromyxoid matrix
- Plasmacytoid and spindled cells frequent
- Epithelial / myoepithelial cells blend into stroma; BCAC has abrupt border with matrix
- Multinodular growth may simulate invasion
- Canalicular adenoma:
- Adenoid cystic carcinoma:
- Cribriform patterns and punched out spaces surrounded by small cells with minimal cytoplasm
- Palisading not prominent
- Lacks large pale and small dark cells common in BCAC
- Coarse nuclear chromatin, high mitotic rate
- Of note: basal cell adenocarcinoma may occasionally show MYB overexpression (J Oral Pathol Med 2017;46:798)
- Basaloid squamous cell carcinoma:
- High grade neoplasm, usually oral or sinonasal tract rather than salivary glands
- Basaloid, comedonecrosis and hyaline type material seen in both
- Abrupt squamous differentiation
- Polymorphous adenocarcinoma:
- Occurs in minor salivary glands only
- Polymorphous architectural patterns
- Monotonous population of single cell type neoplastic proliferation
- Cells have open, vesicular nuclear chromatin with small nucleoli (not basaloid cells)
- Perineural invasion
- Immunohistochemistry highlights only single cell population (not biphasic)
- Skin basal cell carcinoma:
- Skin tumors may metastasize to intraparotid lymph nodes or directly invade parotid
- Palisading, basaloid architecture, necrosis and increased mitotic figures
- Lacks biphasic appearance and myoepithelial cells
- BerEP4+
Additional references
Practice question #1
A 70 year old man presents with a slow growing, painless lesion in the parotid. On gross examination, the lesion is well circumscribed, with a cream, partly cystic lesion. Which of the following is correct?
- Cytology is helpful in the diagnosis of this lesion
- Invasion distinguishes this lesion from its benign counterpart
- Molecular features are often used to differentiate this tumor from mimics
- This low grade neoplasm frequently metastasizes to the lung
Practice answer #1
B. Invasion distinguishes this lesion from its benign counterpart. The tumor is a basal cell adenocarcinoma, a rare, indolent malignant counterpart to basal cell adenoma. Evidence of invasion is essential for diagnosis.
Comment Here
Reference: Basal cell adenocarcinoma
Comment Here
Reference: Basal cell adenocarcinoma