Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Smith MH. Necrotizing sialometaplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsnecrotizingsialo.html. Accessed August 29th, 2025.
Definition / general
- Reactive, self resolving inflammatory condition of the salivary glands that most often affects the palate and is known to mimic malignancy both clinically and histopathologically
Essential features
- Classically begins as a swelling that evolves into a crater-like ulceration, which resolves within 3 - 12 weeks
- Most commonly affects the palate
- Necrosis or disruption of salivary acini with squamous metaplasia of ductal structures
- Etiology is thought to be a reaction to trauma or smoking in a setting of vascular compromise / tissue ischemia
- Mimics malignancy both clinically and histopathologically
Terminology
- Not recommended: adenometaplasia
ICD coding
Epidemiology
- Slight female predominance, although older studies cite a male prominence (Dermatol Online J 2020;26:13030, Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
- Wide age range; mean age of 35 (Dermatol Online J 2020;26:13030)
Sites
- Hard palate is the most common site
- Other sites include buccal mucosa, floor of mouth, nasal cavity, trachea, parotid gland, sublingual gland, submandibular gland, larynx, maxillary sinus, tongue, tonsil and retromolar trigone (Arch Pathol Lab Med 2009;133:692)
Pathophysiology
- Unknown pathogenesis; thought to be caused by vascular ischemia that interrupts the blood supply to the underlying salivary glands (Stomatologija 2022;24:56)
Etiology
- Smoking / vaping
- Trauma, including
- Nonspecific mechanical trauma
- Trauma from dental procedures or anesthetic, especially with vasoconstrictors
- Trauma from an ill fitting denture or orthodontic appliances
- Trauma from intubation or extubation (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
- Bulimia or frequent episodes of vomiting may be an underreported cause (Arch Pathol Lab Med 2009;133:692, Quintessence Int 2016;47:147, Stomatologija 2022;24:56)
- Alcohol, anabolic steroid and cocaine use (Stomatologija 2022;24:56)
Clinical features
- Acute onset, erythematous or mucosal colored swelling often precedes development of crater-like ulceration, which measures 1 - 3 cm (Arch Pathol Lab Med 2009;133:692)
- Borders of the ulcer may be raised
- Swelling may be fluctuant, mimicking an abscess (Arch Pathol Lab Med 2009;133:692)
- Pain and rapid progression are almost universal (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
- Sensations of itching, burning and paresthesia have also been reported (Oral Surg Oral Med Oral Pathol 1991;72:317, Dermatol Online J 2020;26:13030, Cureus 2023;15:e42825, Autops Case Rep 2021;11:e2021244)
- Often unilateral but bilateral and metachronous cases are seen
- May be mistaken for malignancy (Arch Pathol Lab Med 2009;133:692)
- Typically heals within 3 - 12 weeks (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
- Uncommon; < 1% of oral biopsies (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
Diagnosis
- Abrupt, rapidly progressing swelling with subsequent formation of a crateriform ulceration and spontaneous healing over a span of 3 - 12 weeks is clinically diagnostic for necrotizing sialometaplasia (NSM); however, the aggressive clinical behavior / appearance may prompt biopsy to rule out malignancy prior to regression (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
- Close clinical follow up is imperative; if lesional tissue does not heal, biopsy is advised to rule out neoplasia
- NSM has been reported to occur alongside malignancies (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
- Biopsies of lesional tissue should be ample and should avoid particularly necrotic areas (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
Radiology description
- Absent radiologic findings or rare bony erosion (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577, Cureus 2023;15:e42825)
Prognostic factors
- Heals spontaneously within 3 - 12 weeks, although uncommon cases persist for up to 6 months (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577, Dermatol Online J 2020;26:13030)
Case reports
- 26 year old man presented with an ulcer on the palate (Clin Case Rep 2021;9:2019)
- 27 year old woman presented with severe pain and a swelling on the palate (Dermatol Online J 2020;26:13030)
- 32 year old man presented with a 1 month history of palatal swelling (Autops Case Rep 2021;11:e2021244)
- 50 year old woman presented with bony erosion and swelling of the palate (Cureus 2023;15:e42825)
Treatment
- Self resolving within 3 - 12 weeks, although surgical debridement with fabrication of a palatal guard may be considered in abnormally slow healing lesions (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577, Arch Pathol Lab Med 2009;133:692)
- Diagnostic biopsy or rebiopsy is recommended in nonhealing lesions
Clinical images
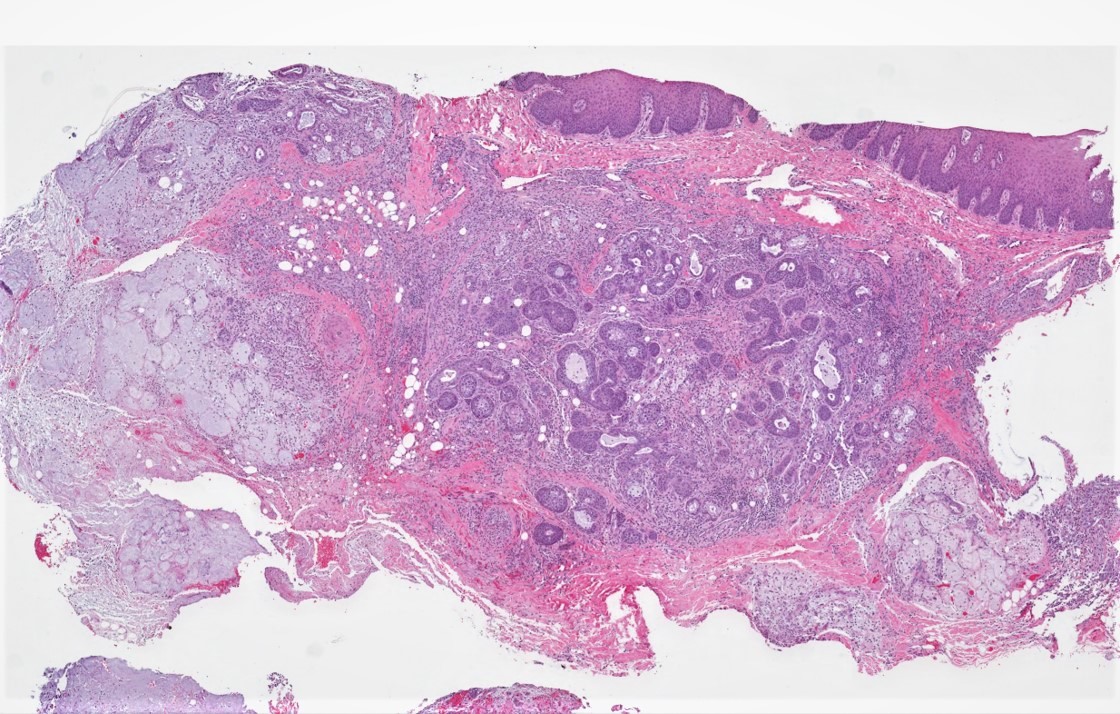
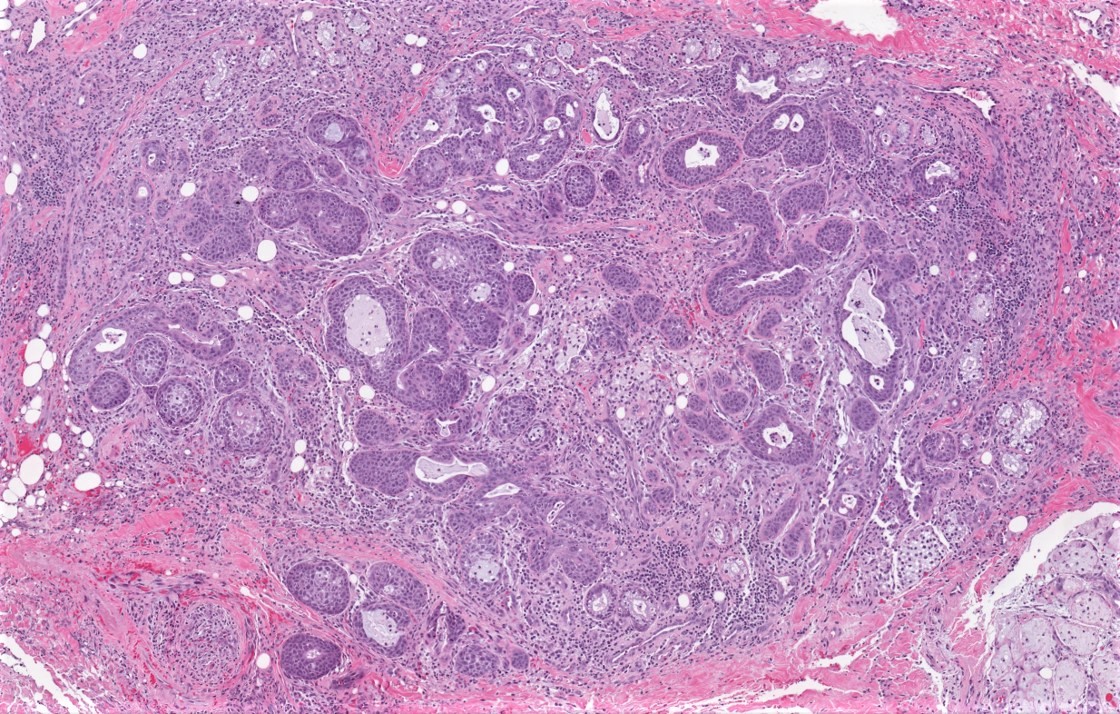
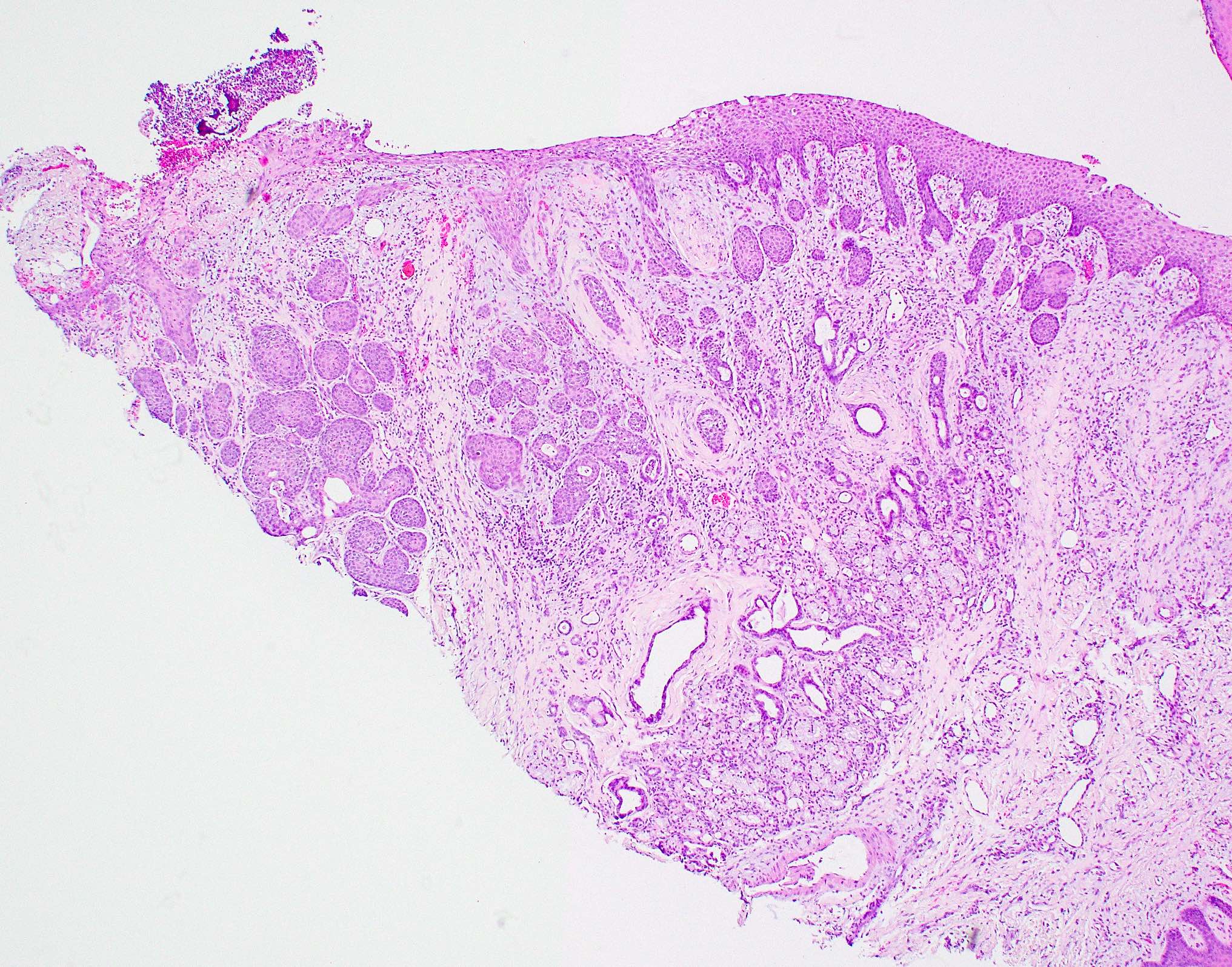
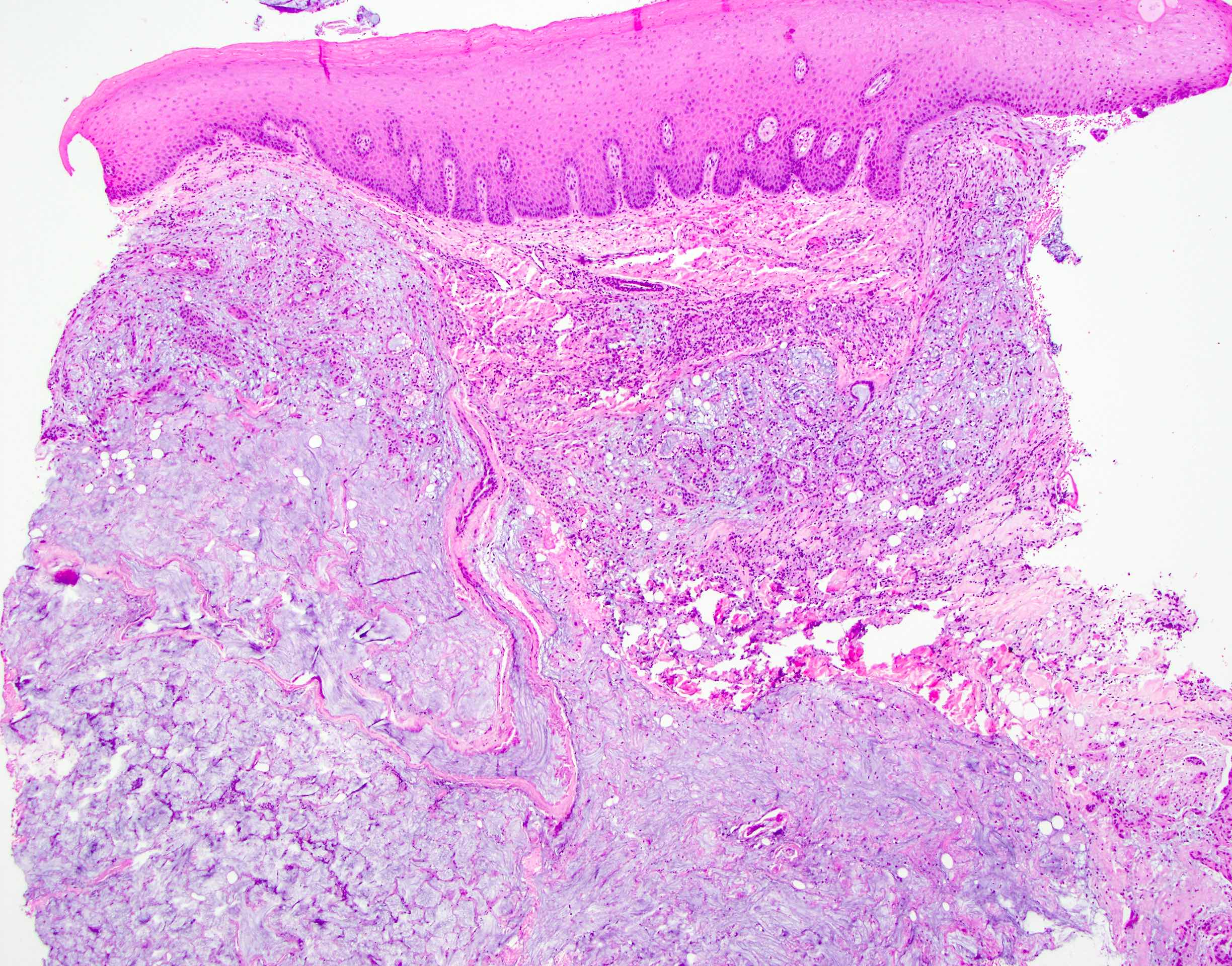
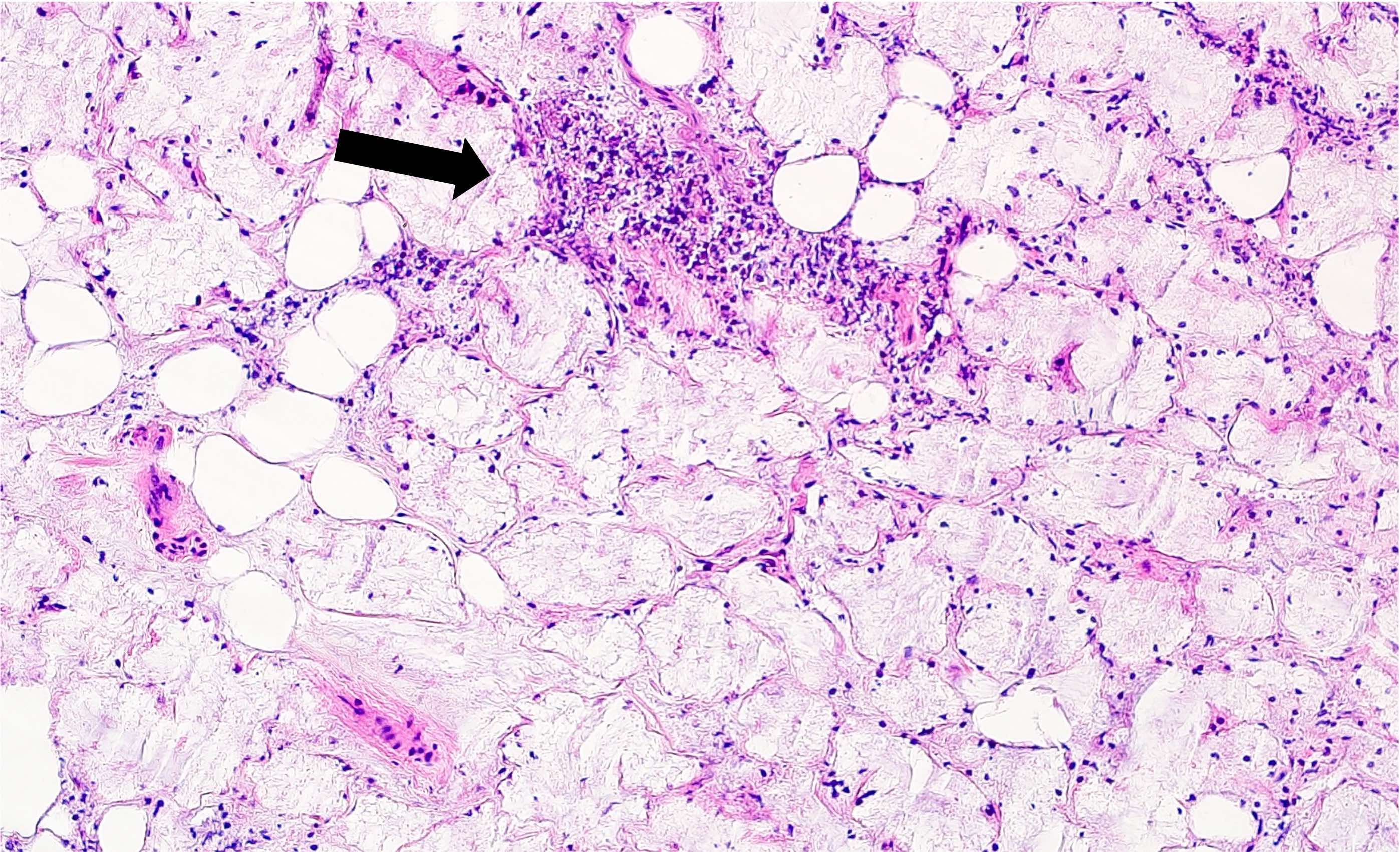
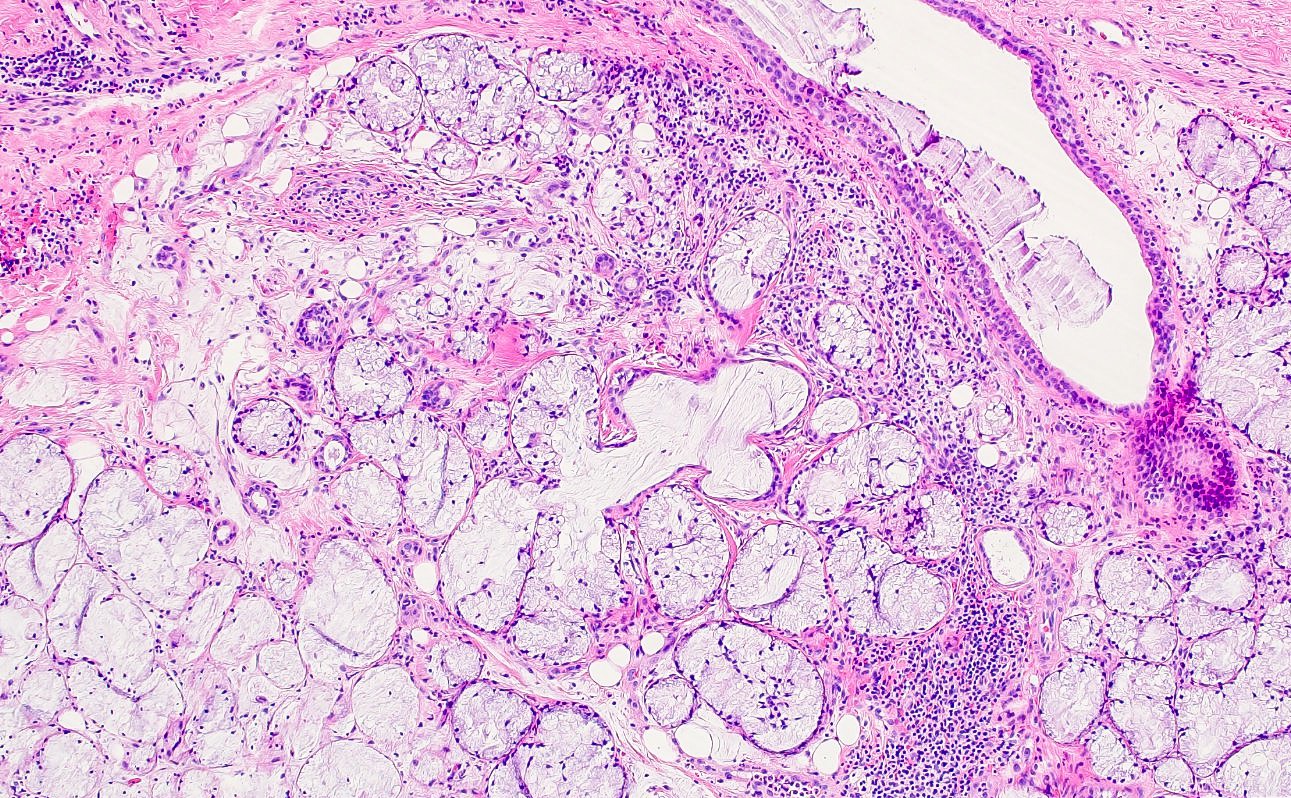
Microscopic (histologic) description
- Squamous metaplasia of ductal structures and acini with preservation of the salivary lobular architecture is an essential feature, according to World Health Organization (see WHO classification-oral cavity & oropharynx)
- Necrosis / infarction of acini characterized by loss of nuclei and cell borders with or without zones of spilled mucin
- Pseudoepitheliomatous hyperplasia with generally bland cytology or keratinocytic regenerative atypia
- Reactive, myxocollagenous background stroma
- Surface ulceration, granulation tissue and subacute inflammation may be present
- Has been conceptualized by 5 histologic stages of development and evolution: infarction, sequestration, ulceration, repair and healing (Int J Oral Surg 1982;11:283)
Microscopic (histologic) images
Positive stains
- Immunohistochemistry is often not necessary for diagnosis
- Generally low p53 and Ki67 index (Dermatol Online J 2020;26:13030)
- Epithelial (CK5, CK6, CK7, CAM5.2, etc.) and myoepithelial (SMA, calponin, p63, S100, etc.) markers may be used to highlight metaplastic ductal epithelium / lobular architecture (Dermatol Online J 2020;26:13030, Arch Pathol Lab Med 2009;133:692)
Sample pathology report
- Hard palate, incisional biopsy:
- Necrotizing sialometaplasia (see comment)
- Comment: The microscopic sections show ulcerated mucosa with zones of pseudoepitheliomatous hyperplasia without prominent cytologic atypia. Squamous metaplasia of ductal structures with preservation of lobular architecture is appreciated along with necrosis of salivary acini and extravasated mucin. No evidence of a neoplasm is identified upon review of multiple deeper levels. Clinical follow up to ensure complete resolution of the lesional tissue is recommended.
Differential diagnosis
- Although the clinical differential diagnosis for an ulceration or swelling on the palate may include a variety of entities (e.g., salivary gland neoplasm, T cell lymphoma, granulomatosis with polyangiitis, deep fungal or bacterial infection), the main histopathological differential diagnosis includes mucoepidermoid carcinoma, squamous cell carcinoma or subacute necrotizing sialadenitis
- Mucoepidermoid carcinoma (MEC):
- Can be challenging to differentiate NSM from MEC on fragmented biopsies or in the later stages of NSM (Head Neck Pathol 2022;16:54)
- Lobular architecture is not preserved
- S100 negative
- Depending on the grade of MEC, the following features may be seen in MEC but not in NSM (Arch Pathol Lab Med 2009;133:692)
- Cystic spaces
- Cellular pleomorphism / atypical mitotic figures
- Presence of perineural / lymphovascular invasion
- Proliferation of apparently neoplastic goblet cells
- Lack of intact lobular architecture
- May show t(11;19)(q14-21;p12-13) with CRTC1(MECT1)::MAML2 fusion
- Squamous cell carcinoma (SCCa):
- Exhibits pleomorphism / abnormal mitotic figures, as compared with NSM which often shows pseudoepitheliomatous hyperplasia with bland cytology (Head Neck Pathol 2022;16:54)
- Myoepithelial markers (e.g., p63, SMA, calponin, S100, etc.) should be absent in SCCa (Arch Pathol Lab Med 2009;133:692)
- SCCa is usually negative for CK7 (Arch Pathol Lab Med 2009;133:692)
- Subacute necrotizing sialadenitis (SNS):
- Debate exists on whether SNS should be considered a separate entity from NSM (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
- Rapid onset of a painful swelling, typically on the palate, which is characterized by necrosis of salivary glands and mixed inflammation but lacks surface ulceration and shows minimal to no squamous metaplasia of ductal epithelium (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:577)
- Heals within 2 - 3 weeks
Additional references
Practice question #1
Practice answer #1
B. Minor salivary glands of the palate. Although necrotizing sialometaplasia can affect any of the given answer choices, it classically involves the minor salivary glands of the hard palate. Answers A, C and D are incorrect because necrotizing sialometaplasia occurs at these sites less frequently than in the minor salivary glands of the palate.
Comment Here
Reference: Necrotizing sialometaplasia
Comment Here
Reference: Necrotizing sialometaplasia
Practice question #2
A patient presents to clinic with severe pain and an ulceration on the hard palate. She states that the lesion began after a dental procedure as a swelling that rapidly progressed to an ulceration over the course of a couple weeks. What is the diagnosis?
- Mucoepidermoid carcinoma
- Necrotizing sialometaplasia
- Squamous cell carcinoma
- T cell lymphoma
Practice answer #2
B. Necrotizing sialometaplasia. The patient presented with the classic clinical history of acute onset of a rapidly progressing lesion on the hard palate, which began as a swelling that subsequently ulcerated. Biopsy revealed large zones of pseudoepitheliomatous hyperplasia, squamous metaplasia of ducts, lack of overt pleomorphism and areas of acinar necrosis and mucin spillage. Answer A (mucoepidermoid carcinoma) is incorrect because the lobular architecture of the gland is preserved and there is no proliferation of cystic spaces or neoplastic goblet cells. Although T cell lymphomas classically may affect the hard palate, answer D is incorrect because the biopsy did not show an atypical lymphoid infiltrate. Answer C (squamous cell carcinoma) is incorrect as the proliferation of squamous epithelium classically forms the pseudoepitheliomatous hyperplasia type pattern and lacks cellular pleomorphism.
Comment Here
Reference: Necrotizing sialometaplasia
Comment Here
Reference: Necrotizing sialometaplasia