Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aghighi M, Motaparthi K. Atrophic papulosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumoratrophicpapulosis.html. Accessed April 18th, 2024.
Definition / general
- Rare vasculopathy with benign skin limited form and frequently lethal systemic variant with intestinal involvement
Essential features
- All ages, mostly in young adults
- Typically affects proximal extremities and trunk
- Papules with porcelain white centers and erythematous peripheral rims
- Wedge shaped dermal necrosis with mucin deposition
- Vessels with endothelial swelling, luminal obliteration, thrombosis
Terminology
- Köhlmeier-Degos disease
- Degos disease
- Malignant atrophic papulosis
- Lethal intestinocutaneous syndrome
ICD coding
- ICD-10: L90.9 - atrophic disorders of skin
Epidemiology
- All ages but mostly in young adults, with mean age of 33 years
- M:F = 3:1 (Br J Dermatol 2014;170:110)
Sites
- More commonly affects proximal extremities and trunk (Clin Exp Gastroenterol 2015;141:147)
- Less commonly affects genital, buccal and conjunctival sites
- GI tract involvement, specifically small intestine
- CNS, hepatorenal and cardiopulmonary system involvement
Pathophysiology
- High interferon alpha expression and accumulation of late stage complements (C5b9) in diseased vessels (Pediatrics 2018;S481:S484)
Clinical features
- Early disease: up to 5 mm in diameter, skin colored papules on proximal extremities and trunk
- Established disease: atrophic papules with porcelain white centers and erythematous peripheral rims, surrounded by telangiectasia
- Late disease: atrophic scars
- May be associated with factor V Leiden or parvovirus B19 infection or autoimmune connective tissue diseases, including systemic lupus erythematosus, antiphospholipid syndrome, dermatomyositis or systemic sclerosis (JAMA Dermatol 2014;150:96)
Diagnosis
- Biopsy from skin, intestines or other involved organs
- Complete blood count
- Stool guaiac test
- Antinuclear antibody titer
- Factor V Leiden, protein C and S, antithrombin III and homocysteine levels
- Anticardiolipin antibody titer
- Antiphospholipid antibody titer
- Endoscopy
- Laparotomy (Orphanet J Rare Dis 2013;8:10)
Laboratory
- In association with systemic lupus erythematosus: antinuclear antibody titer, anti-dsDNA, Coombs test, complement protein C3, C4, CH50 or immune complex assays (C1q or C3d)
- May be differentiated from other associated autoimmune disorders by antiphospholipid and anticardiolipin antibodies, rheumatoid factor, anti-Mi2, antitopoisomerase I and anti-Saccharomyces cerevisiae antibodies (Ann Dermatol 2017;29:215)
Prognostic factors
- Benign atrophic papulosis
- Normal life expectancy
- No systemic involvement
- Represents 70% of cases of atrophic papulosis
- Retrospective diagnosis that requires longterm followup
- Malignant atrophic papulosis
- Onset of systemic disease approximately 1 year after cutaneous findings
- Average 2 year survival in untreated patients with systemic disease
- Peritonitis secondary to intestinal perforation is the leading cause of death (Orphanet J Rare Dis 2013;8:10)
- Cerebral infarction is a less common cause of death
- Patients with underlying autoimmune connective tissue diseases have a better prognosis
Case reports
- 4 year old girl with systemic malignant atrophic papulosis and CNS involvement (Pediatrics 2018;141:S481)
- 30 year old man with multiple ulcerations of the digestive tract (JAMA Dermatol 2020;156:204)
- 30 year old woman with advanced neurologic and GI disease (J Dermatol 2018;45:723)
- 55 year old woman with malignant atrophic papulosis (J Am Acad Dermatol 2016;1274:1277)
Treatment
- Monotherapy or combination therapy
- Eculizumab: monoclonal antibody directed against the complement protein C5 (Orphanet J Rare Dis 2013;8:185)
- Treprostinil: synthetic analog of prostacyclin (Orphanet J Rare Dis 2013;8:52)
- Anticoagulants including heparin
- Aspirin
- Intravenous immunoglobulin
- Systemic corticosteroids
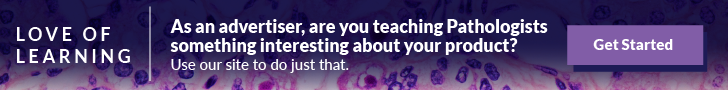
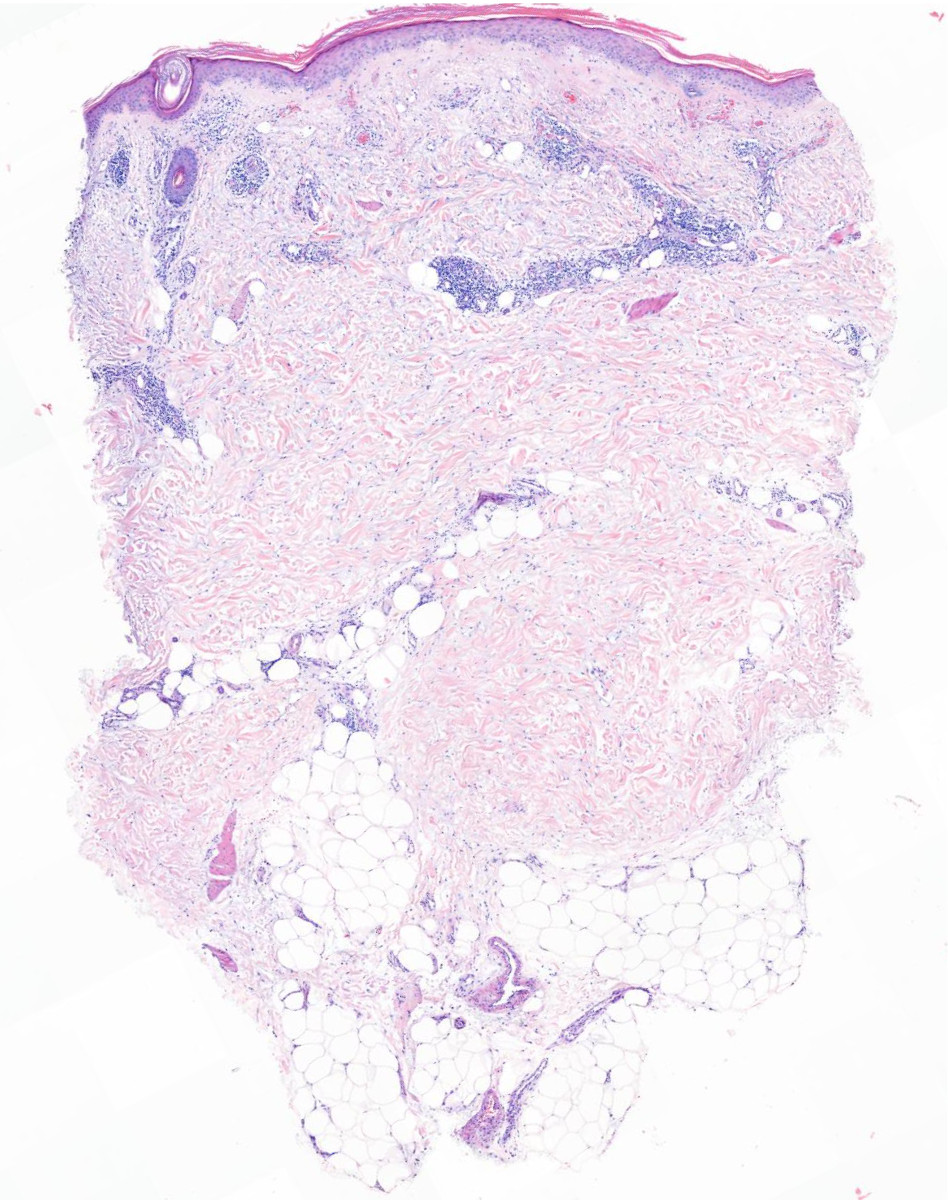
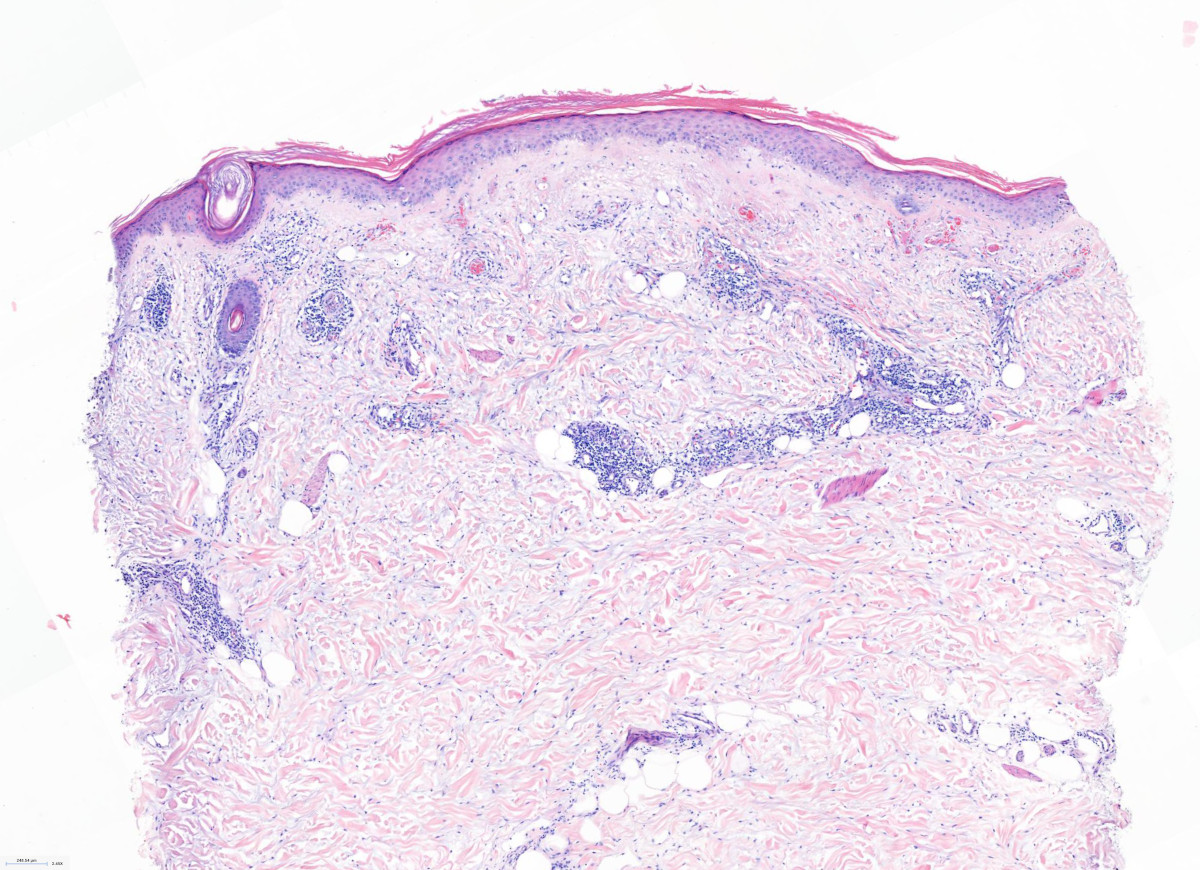
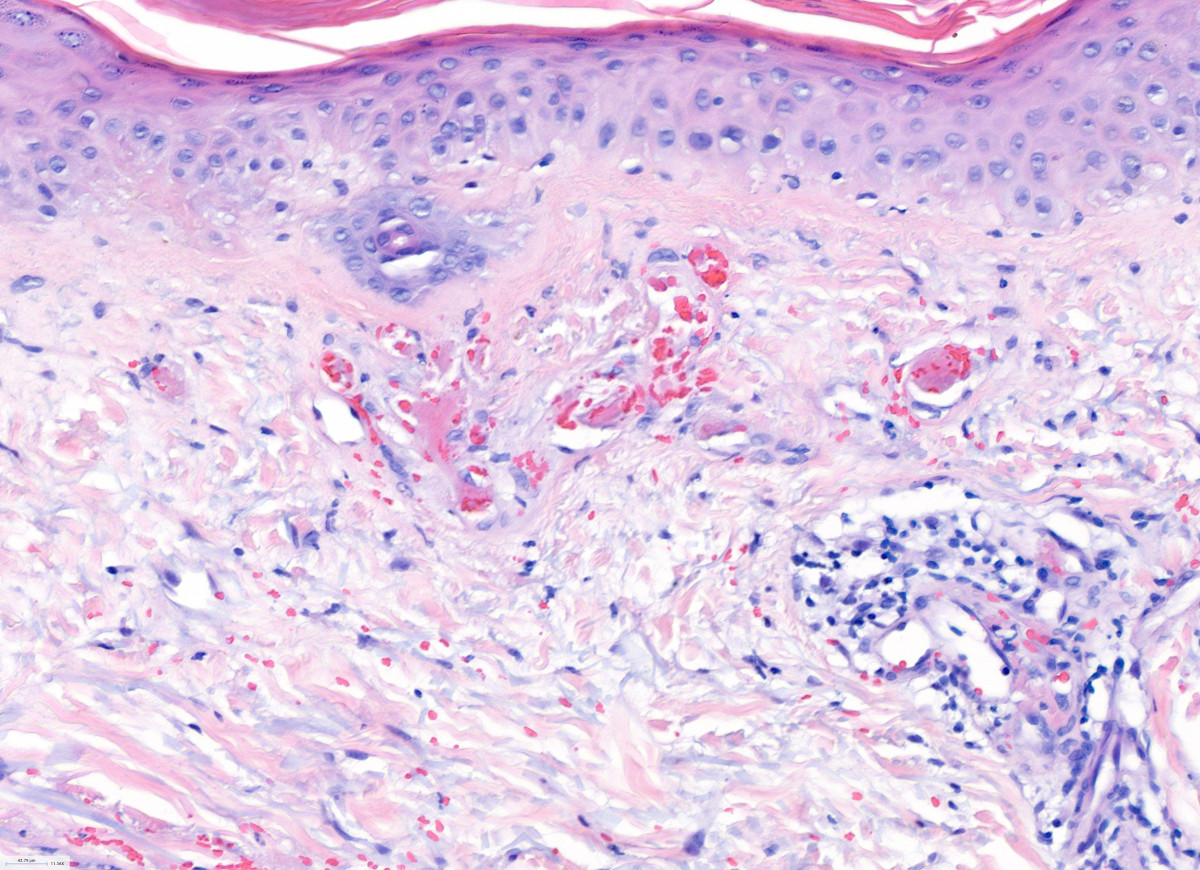
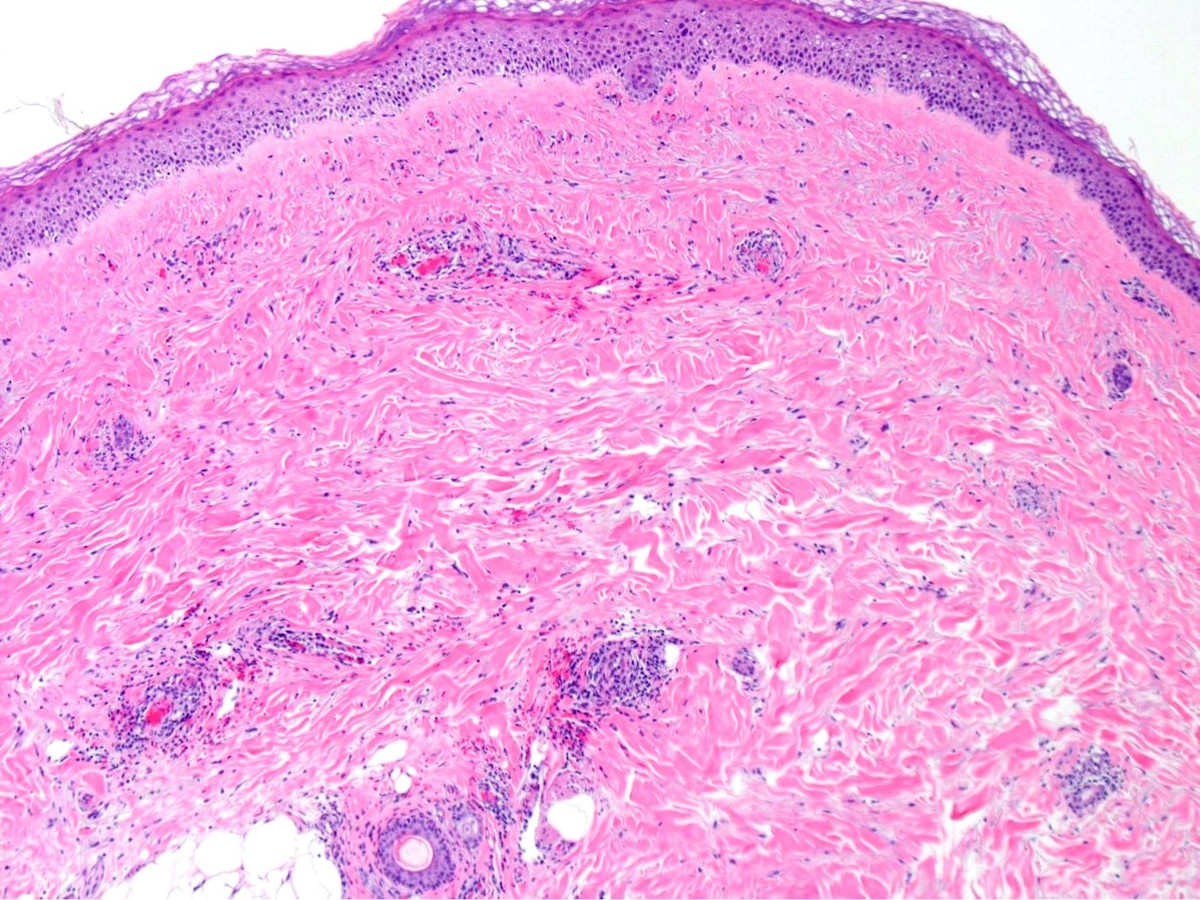
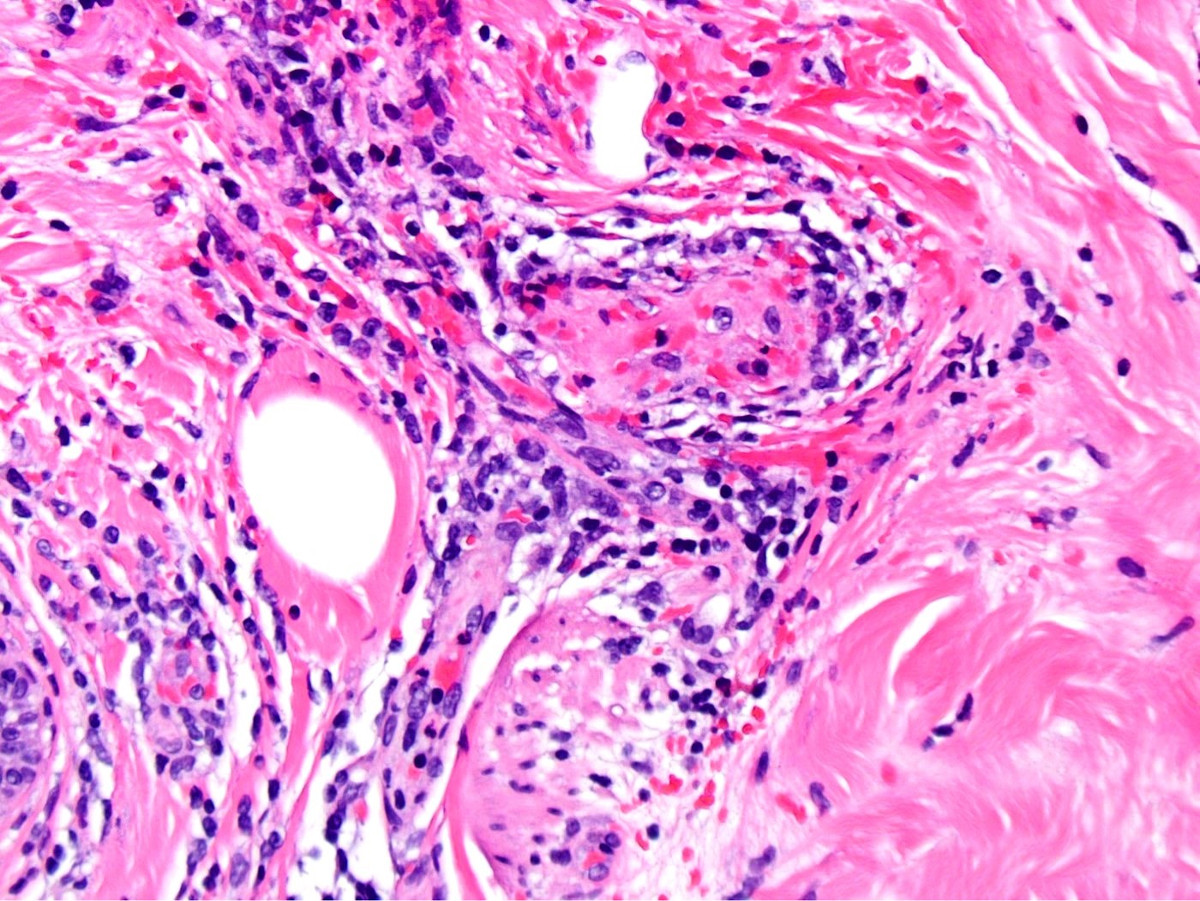
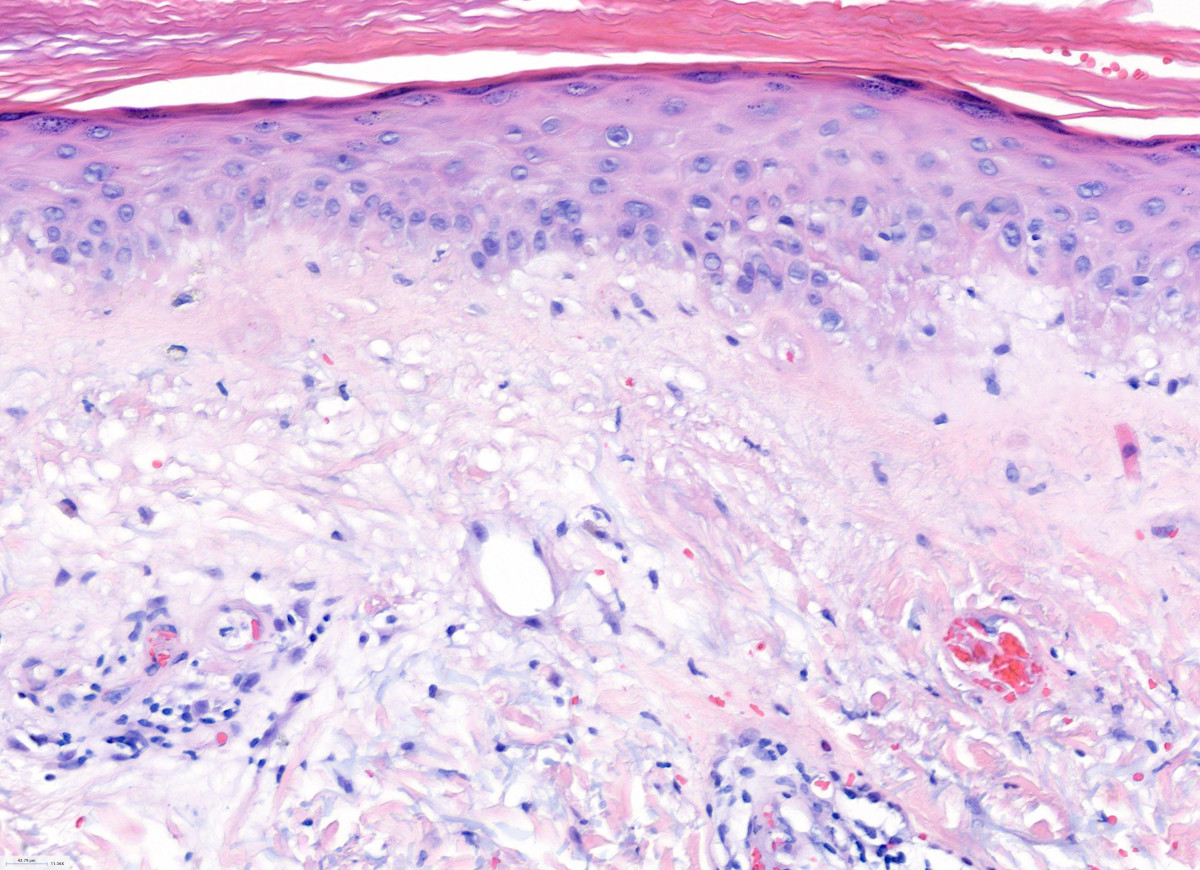
Microscopic (histologic) description
- Early disease:
- Superficial and deep perivascular and periadnexal lymphocytic infiltrate
- Established disease:
- Features of lichen sclerosus: epidermal atrophy, hyperkeratosis and edema with homogenization of the superficial dermis
- Lymphocytic vasculitis
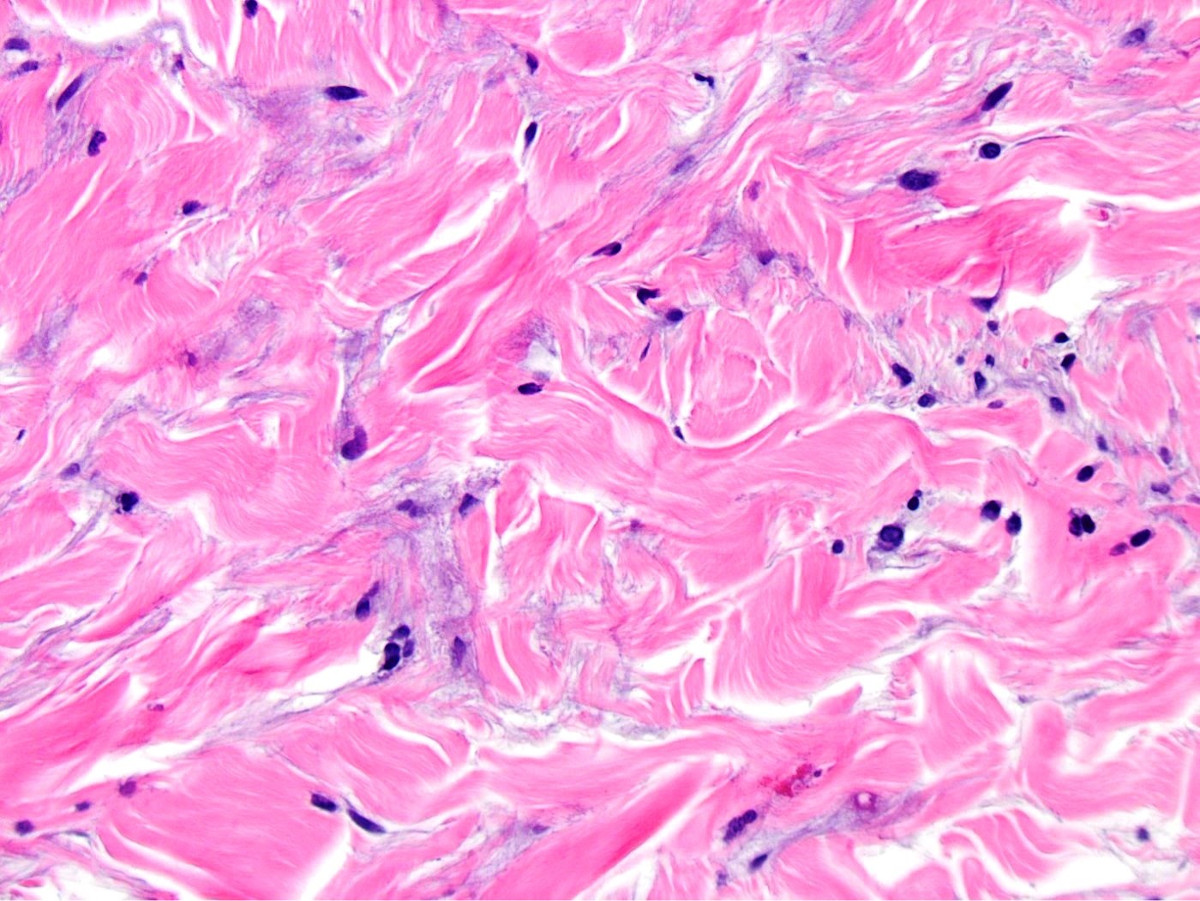
- Late disease (classic features):
- Thrombotic vasculopathy
- Wedge shaped dermal necrosis with mucin deposition (Cutis 1985;35:131)
Microscopic (histologic) images
Immunofluorescence description
- Deposits of C5b9 in vessels (Dermatol Online J 2011;17:6)
Positive stains
- Toluidine blue and hyaluronidase sensitive Alcian blue highlight mucin
- C5b9 stain show substantial deposition of C5b9 in vessels, interstitium and inflammatory cells (Pediatrics 2018;141:S481)
Electron microscopy description
- Endothelial cells with interwoven tubular structures and atrophy with loss of cell to vessel lumen attachment
- Reproduced vascular basement membrane with collagen deposition (Am J Clin Pathol 2011;135:599, Dermatol Online J 2011;17:6)
Sample pathology report
- Right upper arm, biopsy:
- Atrophic papulosis (Degos disease) (see comment)
- Comment: There is a wedge shaped scar, along with a perivascular lymphocytic infiltrate. Dermal vessels have hyaline walls and contain fibrin thrombi. There is also overlying epidermal atrophy and hyperkeratosis.
Differential diagnosis
- Autoimmune connective tissue disease:
- Similar clinicopathologic findings may be observed in systemic lupus erythematosus, systemic sclerosis, dermatomyositis, rheumatoid arthritis and Crohn's disease
- Thrombotic vasculopathy including livedoid vasculopathy:
- Thrombi in vessels may cause epidermal and dermal necrosis
- Lymphocytic infiltrates, mucin deposition, superficial lichen sclerosus-like changes and clinical features permit distinction
- Leukocytoclastic vasculitis:
- Perivascular and interstitial neutrophils, leukocytoclasia and fibrinoid necrosis of vessel walls without significant thrombosis
- Scar:
- Absence of wedge shaped silhouette, mucin or dermal necrosis
- Cutaneous lupus erythematosus:
- Absence of thrombotic vasculopathy
- Lichen sclerosus:
- Absence of thrombotic vasculopathy
Additional references
Board review style question #1
A 35 year old woman presents with white, atrophic papules on her proximal extremities and trunk, malar rash, Raynaud phenomenon, malaise, arthritis and anemia. Laboratory evaluation is significant for thrombocytopenia, leukopenia and high titer ANA and anti-dsDNA. Skin biopsy was performed, shown above. Which of the following statements is correct?
- A poor prognosis is anticipated, with significant neurologic or gastrointestinal involvement
- Late histopathologic findings include dermal necrosis and scar
- The cutaneous findings are most likely idiopathic
- The cutaneous findings represent extragenital lichen sclerosus
- The cutaneous findings represent lupus erythematosus
Board review style answer #1
B. Late histopathologic findings include dermal necrosis and scar. The diagnosis is malignant atrophic papulosis.
Comment Here
Reference: Atrophic papulosis
Comment Here
Reference: Atrophic papulosis
Board review style question #2
A 30 year old man presents with porcelain white papules on his left arm and abdominal discomfort. Skin biopsy showed vacuolar interface dermatitis, hyperkeratosis, perivascular lymphocytic infiltrates, thrombi, mucin and wedge shaped necrosis. Which of the following is the best diagnosis?
- Dermatomyositis
- Leukocytoclastic vasculitis
- Livedoid vasculopathy
- Malignant atrophic papulosis
- Systemic lupus erythematosus
Board review style answer #2