Table of Contents
Definition / general | Diagnosis | Clinical images | Case reports | Treatment | Microscopic (histologic) images | Differential diagnosis | Additional referencesCite this page: Soni A, Slominski A. Impetigo. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorimpetigo.html. Accessed April 26th, 2024.
Definition / general
- Contagious infection; either nonbullous (70%) or bullous (30%)
- Usually affects hands and face of normal children or adults in poor health
- Commonly due to Staphylococcus or Streptococcus infection (Cutis 2010;85:65)
- Methicillin resistant Staph aureus (MRSA) is becoming a new etiology (MedlinePlus: Impetigo [Accessed 27 August 2018])
- Rarely progresses to systemic infection, cellulitis, osteomyelitis, lymphangitis, post-infectious glomerulonephritis (most serious) or staphylococcal scalded skin syndrome (Am Fam Physician 2014;90:229)
Diagnosis
- Skin examination
- Culture of pus from skin lesions may help with pathogen identification and antimicrobial susceptibility testing
Clinical images
Case reports
- Newborn with impetigo contagiosa (BMJ Case Rep 2014;2014:bcr2014204639)
- 35 year old man with acute necrotizing swelling of lower lip (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;113:e22)
Treatment
- Prevention through proper hygiene (washing affected areas and not sharing personal items with others)
- Topical antibiotics such as mupirocin, retapamulin, fusidic acid
- Oral antibiotics if topical therapy is impractical (amoxicillin / calvulanate, dicloaxacillin, clindamycin, doxycycline, macrolides)
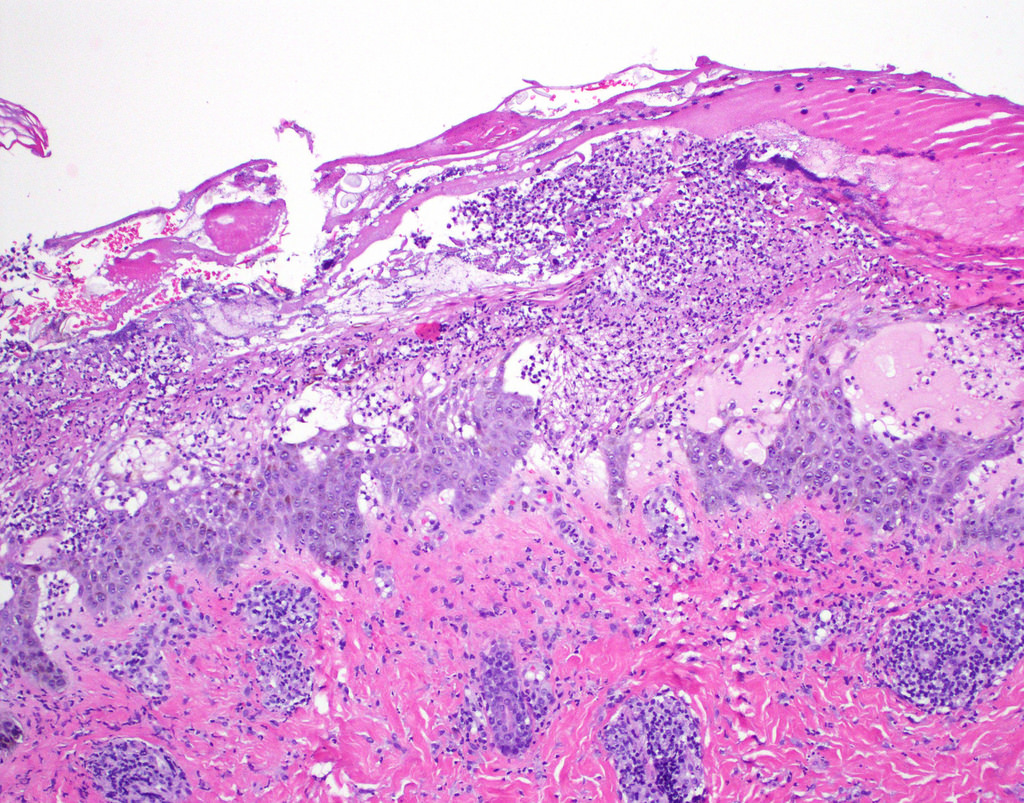
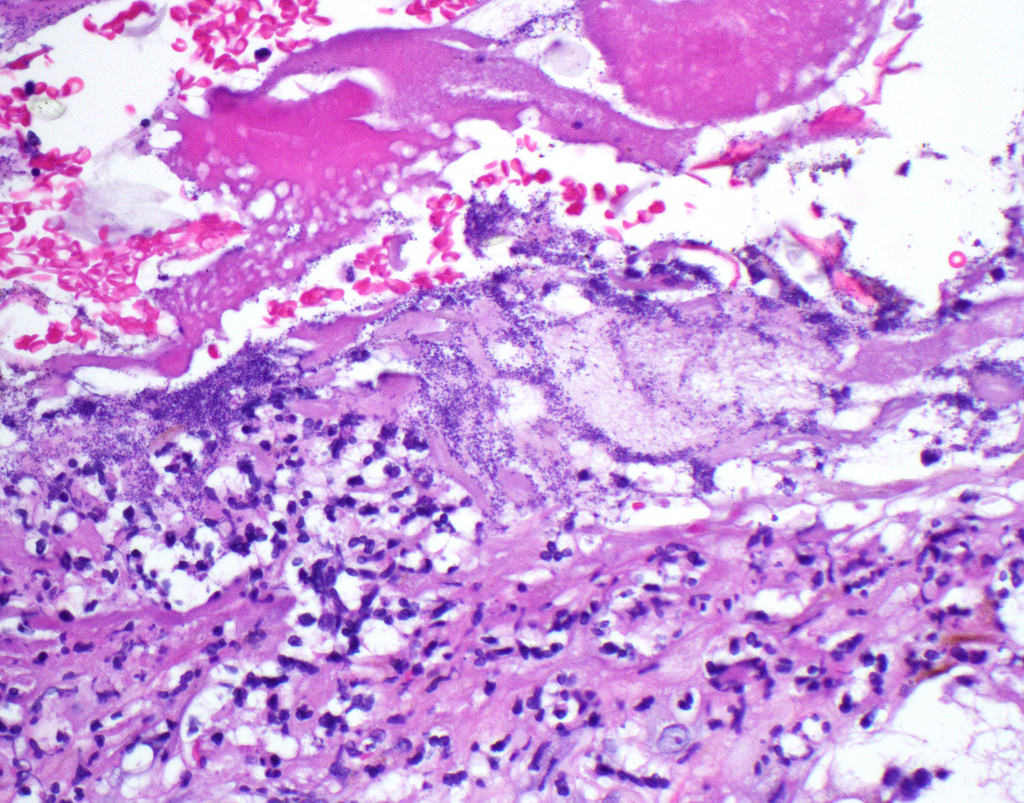
Microscopic (histologic) images
Differential diagnosis