Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Franklin M, Somach S. Foreign body reaction. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorforeignbodyreaction.html. Accessed September 16th, 2025.
Definition / general
- Inflammatory response, most often granulomatous, to an exogenous or endogenous substance that is regarded as foreign material by the cutaneous immune system
Essential features
- Foreign body reaction refers to the inflammatory response of the cutaneous immune system to either exogenous material or an endogenous substance that is altered in some way so that it is regarded as nonself / foreign
- Foreign material may be introduced intentionally (such as tattoos of cosmetic fillers) or accidentally (such as metals or minerals at sites of trauma) (Dermatol Clin 2015;33:497)
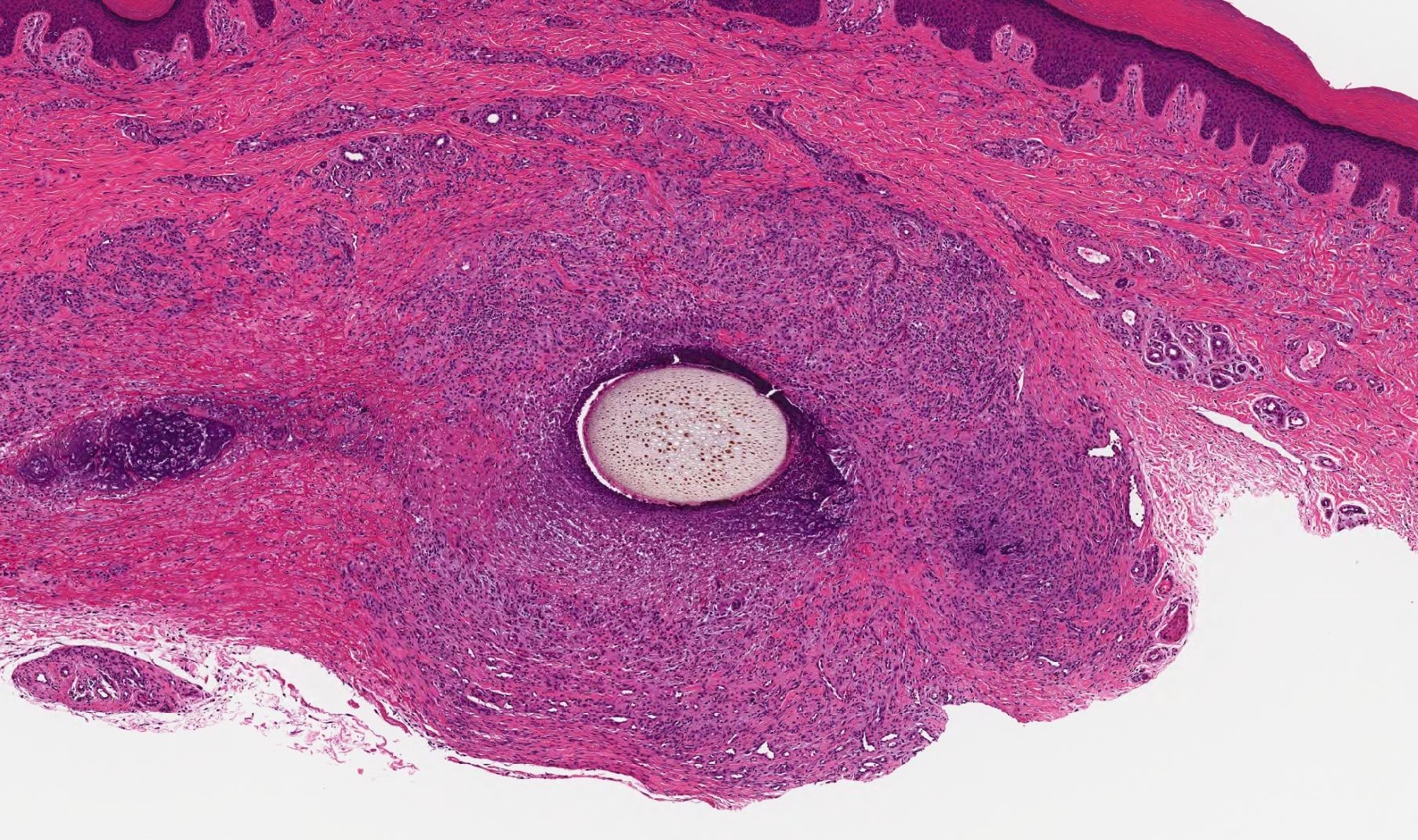
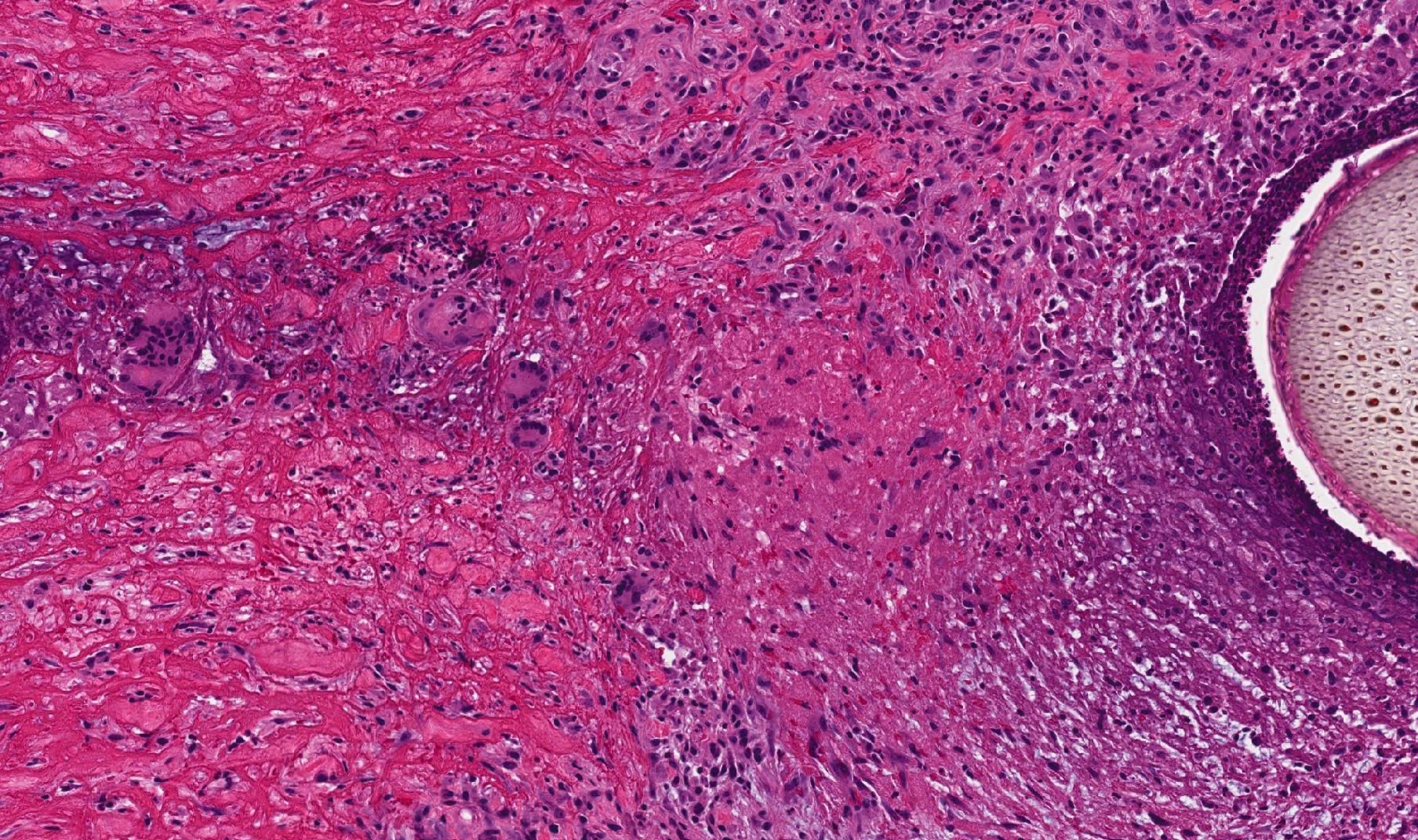
- Keratin is one of the most common substances to elicit a foreign body reaction, as it is typically confined to immune privileged sites
- Though other reaction patterns to foreign material can be seen, granulomatous is the most common (Int J Dermatol 1984;23:531)
Terminology
- Foreign body granuloma refers to foreign body reaction with granulomatous inflammation, which is the most common pattern
ICD coding
- ICD-10: L92.3 - foreign body granuloma of the skin and subcutaneous tissue
Epidemiology
- Given the myriad substances capable of inducing a foreign body reaction, the demographic spectrum of those affected spans all ages and geographic locations
- Specific associations:
- Silica
- Traumatic inoculation following motor vehicle accidents, land mines or sports injuries (Cutis 1987;40:41, Br J Dermatol 1997;137:477)
- Beryllium
- Industrial exposure, fluorescent lamps (J Am Acad Dermatol 2003;49:939)
- Zirconium
- Antiperspirant application (Br J Dermatol 1958;70:75)
- Mercury
- Skin trauma secondary to broken thermometers, self injection or temporary henna tattoos (Br J Dermatol 1997;137:477)
- Nickel
- Ear piercing (Am J Dermatopathol 2004;26:59)
- Titanium
- Ear piercing (J Am Acad Dermatol 2006;55:716)
- Aluminum
- Tattoos, injection sites (J Am Acad Dermatol 1989;20:903, J Cutan Pathol 1993;20:326, J Dermatol 2017;44:e332, Arch Dermatol 1984;120:1318)
- Palladium
- Ear piercing (Contact Dermatitis 2006;55:338)
- Silicone
- Cosmetic procedures / tissue augmentation (Arch Dermatol 2005;141:13, J Cutan Pathol 2007;34:281)
- Paraffin
- Cosmetic procedures / tissue augmentation (J Am Acad Dermatol 2001;45:S222, J Eur Acad Dermatol Venereol 2003;17:583)
- Soft tissue / dermal fillers (J Cutan Pathol 2008;35:536, Am J Dermatopathol 2006;28:173, J Am Acad Dermatol 2001;45:930, Arch Dermatol 2008;144:637)
- Gelfoam (Am J Dermatopathol 2005;27:259)
- Cotton gauze (Joint Bone Spine 2010;77:486)
- Suture material (Ann Surg 1975;181:144)
- Collagen injection (J Am Acad Dermatol 1982;6:867, J Dermatol Surg Oncol 1982;8:111)
- Antiretroviral therapy (Br J Dermatol 2008;158:145)
- Topical medications (e.g. hydroquinone) (J Cutan Pathol 1990;17:236)
- Starch (Arch Dermatol 1973;107:101)
- Talc
- Surgical procedures, drug injection (JAMA 1966;198:1370)
- Tattoo (J Eur Acad Dermatol Venereol 2006;20:349)
- Cactus bristles (Arch Dermatol 1983;119:152)
- Animals
- Arthropods, sea urchins (Am J Pathol 1948;24:367, Arch Dermatol 1962;85:406, J Cutan Pathol 2001;28:223)
- Zinc
- Insulin therapy (Clin Exp Dermatol 1989;14:227)
- Keratin
- Rupture of follicular structures or cysts or in the setting of cutaneous squamous cell carcinoma (Int J Dermatol 1984;23:531, Arch Dermatol 1992;128:649)
- Oxalate
- In the setting of hemodialysis (Br J Dermatol 1993;128:690, J Laryngol Otol 2001;115:514)
- Gunpowder (Clin Imaging 2020;68:197)
- Can be ignited during laser tattoo removal (Dermatol Surg 2000;26:1057)
- Graphite
- Silica
Sites
- Any site can be affected but sites of cutaneous injury most commonly affected
Pathophysiology
- Exogenous material or endogenous material typically hidden from the immune system (e.g. follicular keratin) becomes exposed to innate immune system through trauma (e.g. accidental injury, injection, surgery, tattooing), topical application or systemic exposure
- Initial response is a neutrophilic infiltrate, which typically fails to deal with the foreign material (Dermatol Clin 2015;33:497)
- Local tissue reactions may be lichenoid, eczematous or pseudolymphomatous; however, granulomatous is the most common reaction pattern seen with foreign bodies (Br J Dermatol 1995;133:665, Biomed Res Int 2014;2014:354608, Int J Dermatol 1984;23:531)
- Granuloma formation:
- Monocytes migrate to affected tissue, becoming macrophages and recruit other immune cells (Front Immunol 2014;5:491)
- Macrophages release IL1, IL6, IL12, IL23 and TNG alpha, promoting leukocytes infiltration and T cell activation (Front Immunol 2014;5:491)
- Macrophages primarily adopt an M1 functionality via activation of Toll-like receptors and interferon-gamma from Th1 cells (Nat Rev Immunol 2008;8:958)
- Shift toward epithelioid histiocytes with more secretory capacities and multinucleated giant cell formation may occur (Ann N Y Acad Sci 1976;278:3, Clin Exp Immunol 2009;155:476)
Etiology
- Exposure of immune system to exogenous material or an endogenous substance that is typically protected from the immune system
Clinical features
- Varies with the nature of the exposure to the foreign body and specifics of the host response
- Typically, an acute inflammatory response with erythema and pain is the earliest finding
- Resolves over weeks, months or even years
- Subsequently, a chronic inflammatory response may develop if the acute response did not entirely clear the foreign material
- Red to brown papules, plaques and nodules, along with variable ulceration, may be seen
- Fibrosis may result in tissue induration
- Configuration of lesion(s) may a be clue to causative agent
- Pyogenic granuloma-like lesions (Cases J 2009;2:7354)
- Pseudofolliculitis barbae (Dermatol Clin 1988;6:407)
- Foreign material may contain microorganisms (Arch Dermatol 1984;120:1209, Cutis 1995;56:41)
- Associated lymphadenopathy may secondary to granulomatous inflammation and foreign material in lymph node (Oral Surg Oral Med Oral Pathol 1985;59:449, J Clin Pathol 2000;53:549)
Diagnosis
- Careful history and examination correlated with tissue sampling and exclusion of other diagnoses (e.g. granulomatous disease, infection)
- Ultrasound can quantify the severity of tattoo reactions (Skin Res Technol 2014;20:257)
- Identification of foreign substance can be ascertained using ultrastructural analytic techniques such as energy dispersive Xray spectroscopy / analysis (Clin Dermatol 1991;9:157)
Radiology description
- Ultrasound
- Prominent echolucent band, the thickness of which correlates with thickness of cellular infiltration on histology (Skin Res Technol 2014;20:257)
Case reports
- 48 year old and 80 year old women with oral foreign body granuloma related to soft tissue fillers (J Clin Exp Dent 2018;10:e177)
- 67 year old woman with a forehead nodule secondary to a foreign body reaction to pencil core material (An Bras Dermatol 2017;92:578)
- 76 year old man with a foreign body granuloma of the tongue due to a pequi spine (Case Rep Dent 2020;2020:8838250)
- 83 year old woman with foreign body reaction to dermal filler treated with allopurinol (Actas Dermosifiliogr (Engl Ed) 2020;111:439)
Treatment
- Nonablative quality switched lasers may be used to obliterate unwanted tattoo ink (Dermatol Clin 2014;32:91)
- Etanercept has been used to successfully treat a granulomatous tattoo reaction (J Eur Acad Dermatol Venereol 2007;21:550)
- Surgical techniques (Malays J Med Sci 2019;26:137, Chin J Dent Res 2020;23:289)
- Minocycline for silicone granulomas (J Am Acad Dermatol 2005;52:53)
- Allopurinol (Case Rep Dermatol Med 2012;2012:945205)
- Colchicine (J Dermatolog Treat 2007;18:112)
- Cyclosporine (Dermatol Surg 1999;25:247)
- Dermal filler foreign body reaction treatments:
- Intralesional corticosteroids (Aesthetic Plast Surg 2012;36:421)
- Intralesional 5-fluorouracil (Aesthetic Plast Surg 2012;36:421)
- Oral corticosteroids (Arch Plast Surg 2015;42:232)
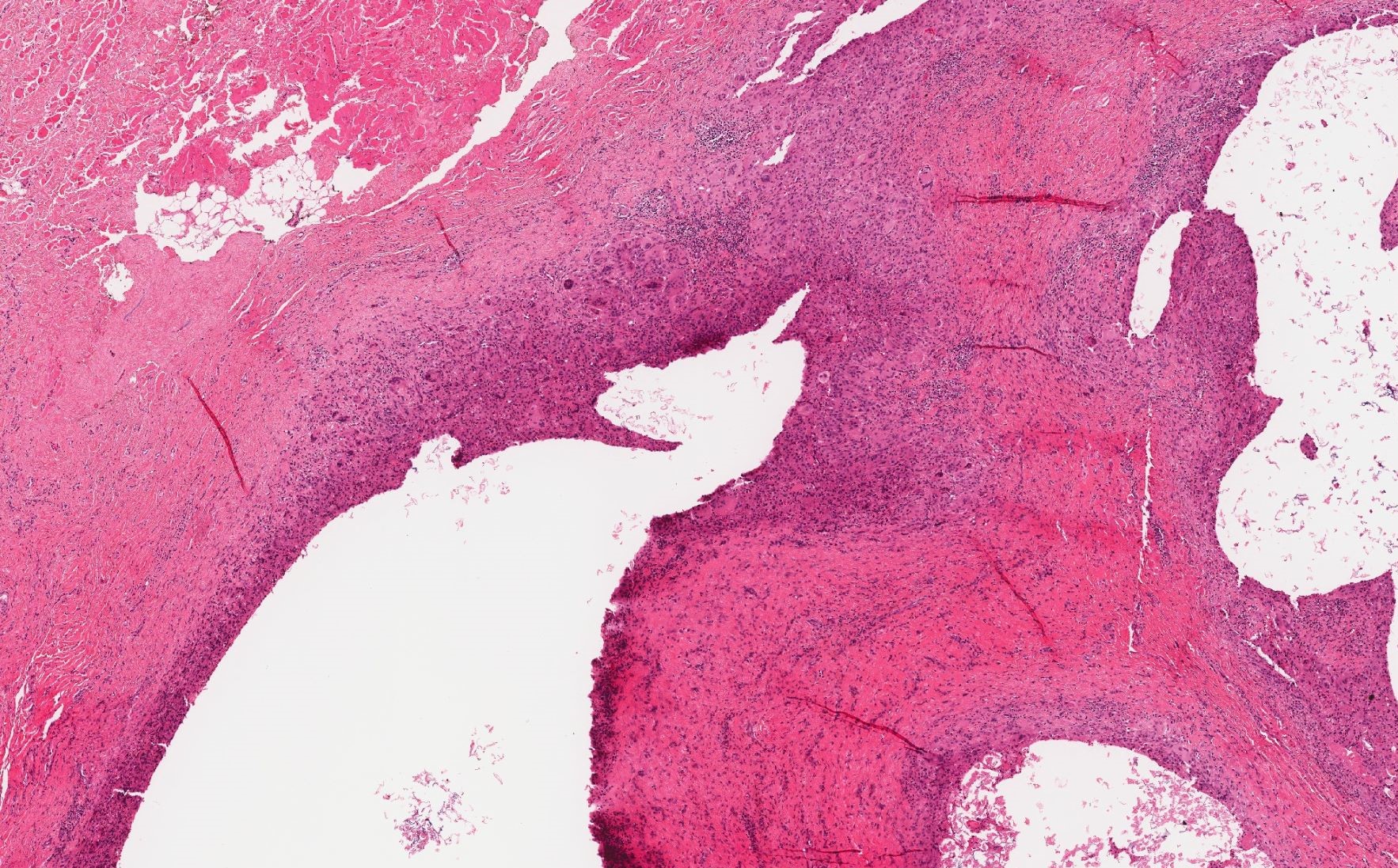
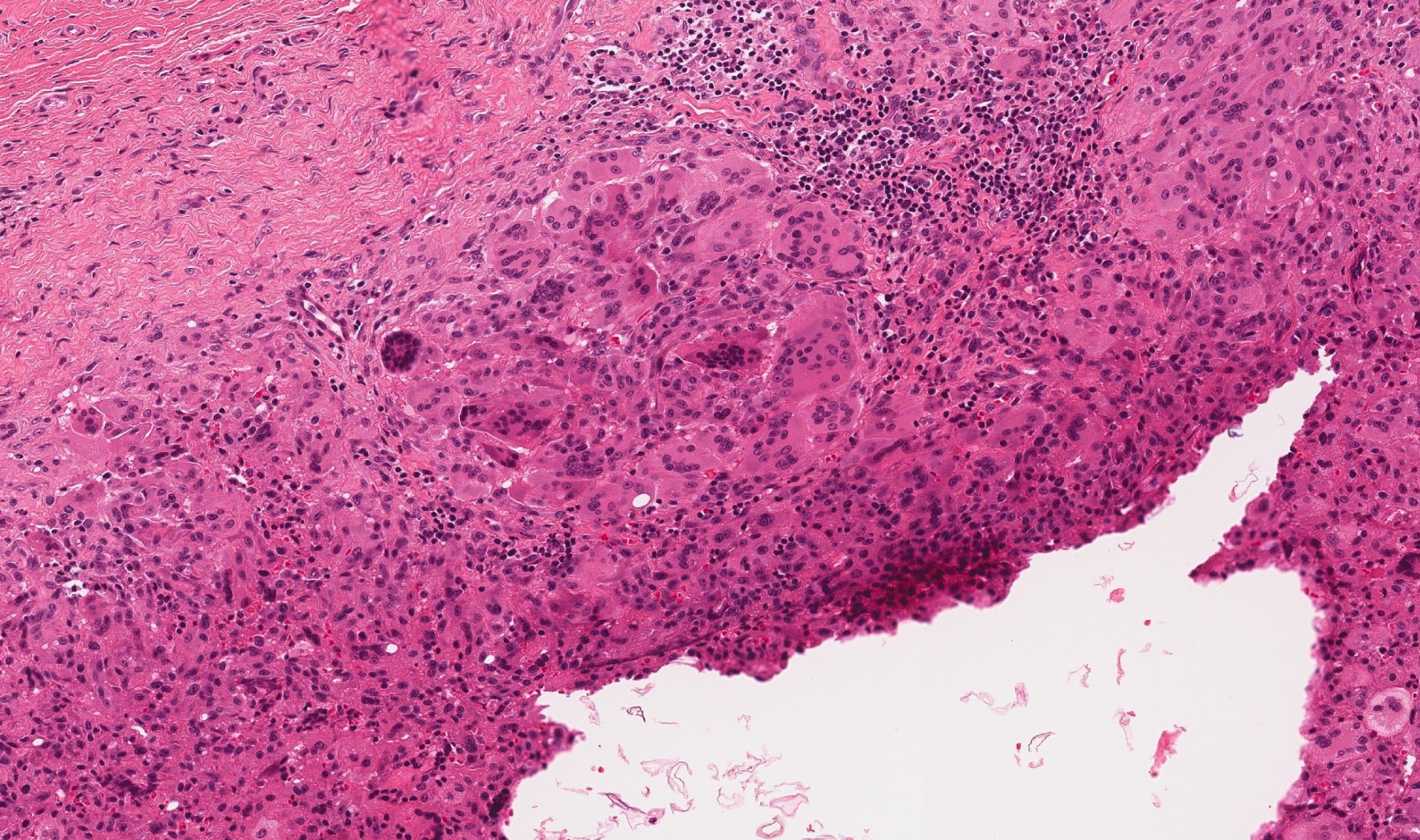
Microscopic (histologic) description
- Varies depending on the specific response but many materials (e.g. silica, tattoo pigments, zinc, keratin, zirconium, silicone etc.) produce sarcoidal granulomas (Int J Dermatol 1984;23:531):
- Discrete aggregates of epithelioid histiocytes and multinucleate giant cells (Langhans or foreign body type)
- Sparse rim of surrounding lymphocytes and plasma cells
- Specific patterns (Clin Dermatol 1991;9:157, Int J Dermatol 1984;23:531):
- Tattoo: may see pigment within macrophages and in interstitium
- Paraffin: cystic spaces of varying size (swiss cheese), which stain with oil red O on fresh tissue
- Silicone: cystic spaces of varying size (swiss cheese), which do not stain with oil red O on fresh tissue
- Silica: crystalline particles that are birefringent on polarized light
- Talc: birefringent particles with polarized light
- Starch: birefringent particles with Maltese cross shape on polarized light; stains with PAS
- Zinc: birefringent particles with polarized light
- Bovine collagen: stains pale gray-violet (rather than blue-green) with Masson trichrome
- Hyaluronic acid: stains blue with high pH Alcian blue
- Wood splinter: regularly sized cells on cross section
- Keratin: potato chip bodies that are variably birefringent
Microscopic (histologic) images
Positive stains
- CD68 stains multinucleate giant cells
Videos
Histopathology of breast foreign body reaction
Sample pathology report
- Skin, left dorsal forearm, punch biopsy:
- Tattoo with foreign body reaction (see comment)
- Comment: Sections show a bisected punch specimen with an unremarkable epidermis with subjacent dermal scar. Underlying the dermal scar, there is a broad, well demarcated zone of granulomatous inflammation with numerous multinucleate giant cells and scattered lymphocytes. Black pigment is identified within histiocytes and in the surrounding interstitium. The findings are those of a granulomatous foreign body reaction and could be consistent with a prior traumatic tattoo. Clinical correlation is recommended.
Differential diagnosis
- Sarcoidosis:
- Exclude foreign material and infection (e.g. with microscopic examination with polarized light and stains for microorganisms)
- Infection (e.g. abscess):
- Exclude with tissue cultures and stains for microorganisms (e.g. Fite, GMS, PAS, Gram stain)
- Pyogenic granuloma:
- May arise in the setting of a foreign body reaction
- Exclude an underlying foreign body reaction (e.g. with careful history and microscopic examination with polarized light)
Practice question #1
Practice answer #1
Practice question #2
Which inflammatory pattern is most commonly seen in a foreign body reaction?
- Eczematous
- Granulomatous
- Lichenoid
- Psoriasiform
Practice answer #2