Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zhovta N, Kazlouskaya V. Pityriasis rosea. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorpityriasisrosea.html. Accessed May 6th, 2024.
Definition / general
- Pityriasis rosea is a self limited viral exanthem usually seen in young patients that starts with a herald patch, followed by similar lesions on the trunk
Essential features
- Pityriasis rosea is a viral exanthem, commonly caused by reactivation of human herpesvirus 6 and human herpesvirus 7
- Clinically presents with the herald patch manifesting first, followed by disseminated similar patches on the upper trunk
- Histopathology of pityriasis rosea demonstrates spongiotic pattern
ICD coding
- ICD-10: L42 - pityriasis rosea
Epidemiology
- Incidence 0.68 per 100 clinic visits (Acta Dermatovenerol Alp Pannonica Adriat 2019;28:15)
- Usually happens in young patients, with the peak incidence in the 20 - 24 year old age groups (Eur J Epidemiol 1998;14:495)
- Average age of pediatric pityriasis rosea onset is 12 years (Turk J Med Sci 2016;46:1740)
- Some studies notice seasonal variation and predominance during colder months (Turk J Med Sci 2016;46:1740, Acta Dermatovenerol Alp Pannonica Adriat 2019;28:15)
- There may be a slight female predominance
Sites
- Skin (usually trunk and extremities), lymphadenopathy
Pathophysiology
- Elevated levels of Toll-like receptors 3, 7, 8, 9 (J Pathol Transl Med 2017;51:148)
- Elevated levels of IL22 (Clin Exp Dermatol 2017;42:30)
- Upregulation of IL17, IFNγ, VEGF and IP10 (Mediators Inflamm 2015;2015:438963)
Etiology
- Reactivation of latent human herpesvirus 6 and human herpesvirus 7 (Am J Emerg Med 2020;38:1969.e1)
- Triggered by infections, especially of upper respiratory tract (Australas J Dermatol 2021;62:e333)
Clinical features
- Large, scaly patch with slightly raised margins appears first on the trunk in most cases or more rarely on the extremities (herald patch)
- Rarely, multiple herald patches may appear
- Prodrome symptoms with malaise, fever, arthralgias or headaches may precede the development of skin lesions
- Disseminated lesions are slightly oval in shape and follow Langer lines, forming a so called Christmas tree pattern on the back
- Face, palms and soles are usually but not always spared
- Disease is usually self limiting and resolves in a few weeks; some durations of several months have been reported
- Recurrences are rare but have been reported
- Atypical clinical variants include:
- Acral pityriasis rosea: may be isolated or accompanied by classic lesions on the trunk (Dermatol Reports 2021;13:9081, Indian Dermatol Online J 2020;11:823)
- Blaschkoid variant: distribution along Blaschko lines (Pediatr Dermatol 2021;38:701)
- Unilateral pityriasis rosea (Indian Dermatol Online J 2020;11:823)
- Inverse variant: located in the larger body folds (Indian Pediatr 2019;56:981)
- Urticarial: annular, wheal-like lesions (World J Clin Cases 2017;5:203)
- Erythema multiforme-like: annular lesions resembling erythema multiforme (World J Clin Cases 2017;5:203)
- Vesicular / pustular: vesicular or pustular lesions surrounding the pityriasis rosea patches (World J Clin Cases 2017;5:203)
- Purpuric: purpuric macular eruptions, usually on the lower extremities (J Eur Acad Dermatol Venereol 2005;19:120)
- Papular / follicular: 1 - 3 mm papules, sometimes follicular, with scaling; common in darker skin types (World J Clin Cases 2017;5:203)
- Oral involvement: petechiae, erosions, geographic tongue, erythema, white palate (Pediatr Dermatol 2018;35:e124, J Am Acad Dermatol 2017;77:833)
Diagnosis
- Clinical examination
- Skin biopsy
Laboratory
- Usually not needed to establish the diagnosis
Prognostic factors
- Increased rate of complications in pregnant females was reported, especially in the first 15 weeks, associated with high HHV6 viral load and increased body area involvement (J Am Acad Dermatol 2021 Jan 8 [Epub ahead of print])
Case reports
- 7 year old girl and 30 year old woman, a mother and daughter, presenting with pityriasis rosea (Indian Dermatol Online J 2018;9:131)
- 11 year old boy with an inverse pityriasis rosea (Indian Pediatr 2019;56:981)
- 15 year old boy with unilateral pityriasis rosea (Turk J Pediatr 2017;59:214)
- 29 year old woman with pityriasis rosea with classical and acral lesions (Dermatol Reports 2021;13:9081)
- 54 year old woman with pityriasis rosea triggered by COVID-19 infection (Medicine (Baltimore) 2021;100:e25352)
Treatment
- Treatment is not necessary if subject is asymptomatic
- In symptomatic, topical or oral corticosteroids, oral antihistamines, ultraviolet B therapy may be used (Cochrane Database Syst Rev 2019;2019:CD005068)
- Antibiotics (erythromycin) and antiviral (acyclovir) were reported to shorten the course of the disease but the results are controversial and their use is not widespread (Cochrane Database Syst Rev 2019;2019:CD005068, J Dermatolog Treat 2019;30:288)
Clinical images
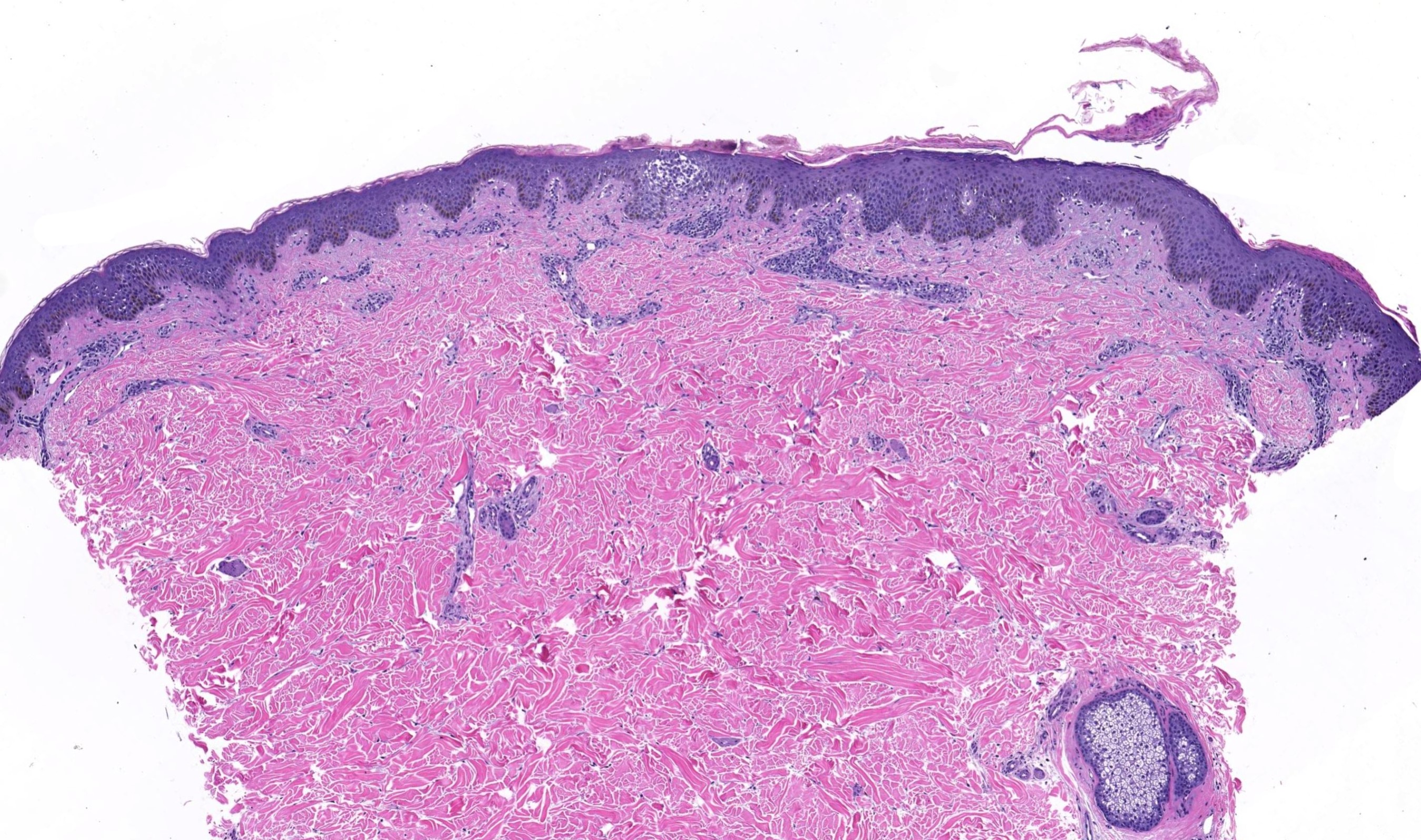
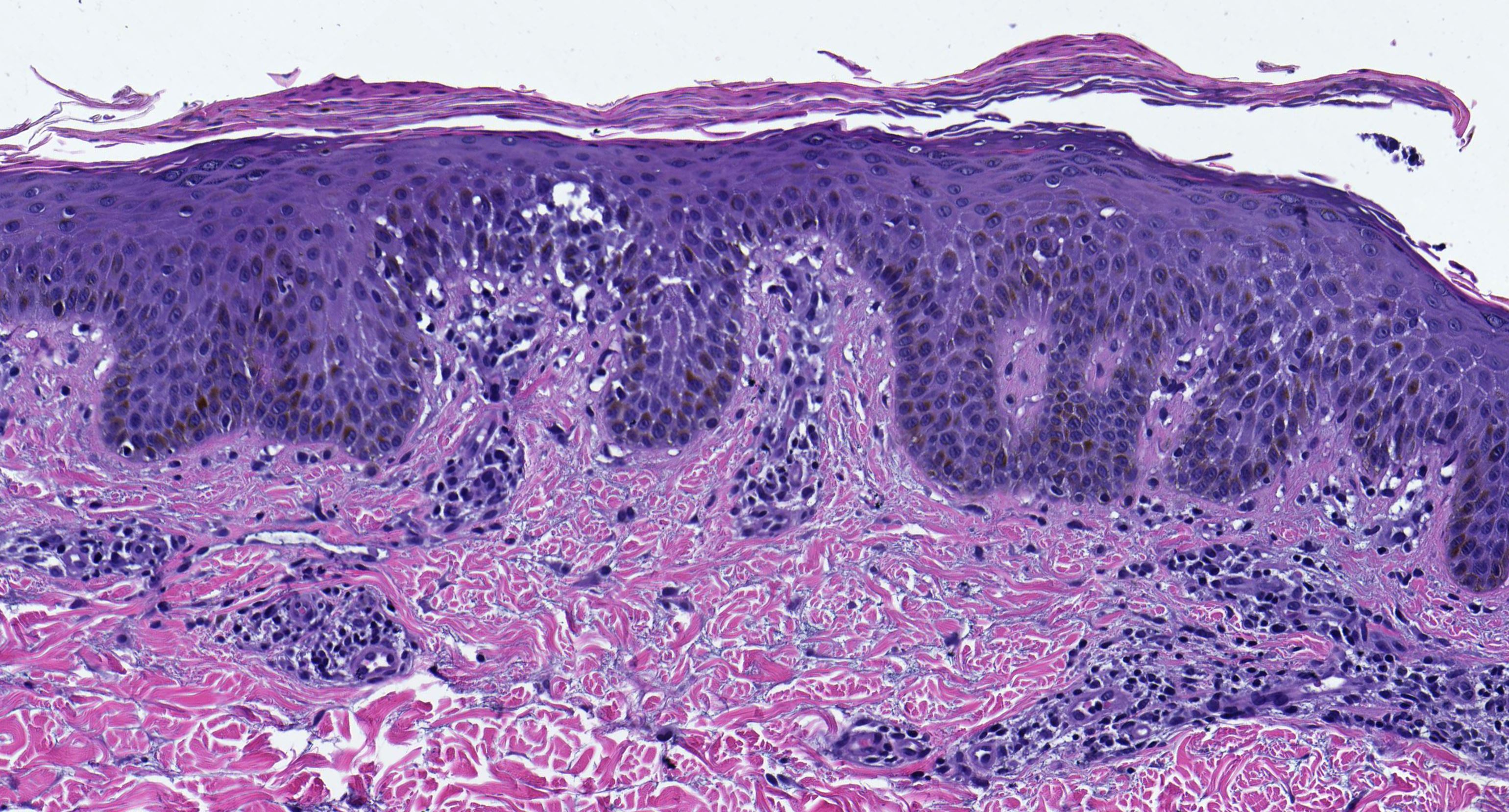
Microscopic (histologic) description
- Subacute spongiotic dermatitis with perivascular lymphocytic infiltrate (Dermatologica 1982;165:551)
- Mild acanthosis of the epidermis may be present, especially in herald patch
- Foci of parakeratosis overlying spongiosis
- Granular layer may be diminished or absent under area of parakeratosis (Indian J Dermatol Venereol Leprol 2000;66:244)
- Erythrocyte extravasates may be focally present in the superficial dermis
- Rare presence of dyskeratotic cells and eosinophils may be observed
Microscopic (histologic) images
Sample pathology report
- Skin, biopsy:
- Subacute spongiotic dermatitis, suggestive for / consistent with pityriasis rosea (see comment)
- Comment: Biopsy examination demonstrates subacute spongiosis with overlying mounds of parakeratosis. There is a mild inflammatory perivascular infiltrate composed predominantly of lymphocytes with erythrocyte extravasates. No fungal elements were identified with PAS stain. Clinical image was reviewed. Overall, the histopathological features and clinical presentation are consistent with pityriasis rosea or a pityriasis rosea-like drug reaction but only in an appropriate clinical setting. (If clinical images and history are not present, the report may be more descriptive and include differential diagnosis of other spongiotic conditions.)
Differential diagnosis
- Pityriasis rosea-like eruptions:
- Triggered by medications or vaccinations
- Clinically, may be itchier, often display peripheral eosinophilia and tend to persist unless the drug is stopped
- Histopathologically: often indistinguishable; may have interface and eosinophilia (JAAD Case Rep 2018;4:800)
- Guttate / eruptive psoriasis:
- May be very similar clinically and histopathologically
- Herald patch is usually not present in psoriasis
- Histopathologically: neutrophils present in the parakeratosis; dilated vessels in the papillary plates are more common (Australas J Dermatol 2020;61:e481)
- Secondary syphilis:
- Clinically, may be similar but no herald patch seen
- Histopathologically: psoriasiform and lichenoid dermatitis with perivascular and interstitial infiltrate with lymphocytes, histocytes and plasma cells
- Sometimes, the infiltrate may be granulomatous
- Swollen, prominent endothelial cells are common (J Am Acad Dermatol 2020;82:156)
- Other eczematous eruptions (contact dermatitis, nummular dermatitis, seborrheic dermatitis):
- May be indistinguishable histopathologically and clinical correlation is required
- Although a few eosinophils may be present in pityriasis rosea, large numbers are uncommon
- Drug eruptions:
- Variable clinical presentation
- Histopathology is variable; combination of interface pattern with spongiosis and eosinophil rich infiltrates are common
- Pityriasis lichenoides:
- Clinically, may have similar features; however, tends to have a chronic course, no herald patch present
- Histopathologically: an interface dermatitis and perivascular lymphocytic infiltrate is present with erythrocyte extravasates
- Presence of neutrophils in the parakeratosis
Board review style question #1
What are the expected histopathological features of this condition?
- Spongiosis, mixed perivascular infiltrate with lymphocytes and neutrophils, neutrophils in the stratum corneum and positive PAS stain
- Regular psoriasiform acanthosis, perivascular lymphocytic infiltrate, parakeratosis with neutrophils and negative PAS stain
- Acute spongiosis, wedge shaped perivascular and interstitial infiltrate with numerous eosinophils
- Subacute spongiosis, perivascular superficial lymphocytic infiltrate with erythrocyte exocytosis and mounds of parakeratosis overlying spongiosis
- Interface dermatitis, perivascular superficial lymphocytic infiltrate with erythrocyte exocytosis and parakeratosis with neutrophils
Board review style answer #1
D. The condition demonstrated in the picture is pityriasis rosea. The patient has scaly, slightly oval patches localized along Langer lines. Classical histopathological features of this condition are subacute spongiosis, superficial perivascular lymphocytic infiltrate (often with erythrocyte exocytosis) and small mounds of parakeratosis overlying spongiotic areas. The description from choice A corresponds to tinea infection; B) psoriasis; C) arthropod reaction; E) pityriasis lichenoides.
Comment Here
Reference: Pityriasis rosea
Comment Here
Reference: Pityriasis rosea
Board review style question #2
What virus plays the most significant role in the pathogenesis of pityriasis rosea?
- EBV
- HHV6
- HIV
- HSV1
- HSV2
Board review style answer #2
B. HHV6. Although the exact etiology of pityriasis rosea is unknown, the reactivation of HHV6 and HHV7 was reported to play a role.
Comment Here
Reference: Pityriasis rosea
Comment Here
Reference: Pityriasis rosea