Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Şimşek G. Pityriasis lichenoides. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorPLC.html. Accessed April 18th, 2024.
Definition / general
- Cutaneous eruption, papulosquamous, necrotic or mixed lesions (Clin Exp Dermatol 2021;46:1561)
- Relapsing course with long periods of remission (J Am Acad Dermatol 2006;55:557)
- Clonal T cell receptor gene rearrangement was reported (Arch Dermatol 2002;138:1063)
Essential features
- Asymptomatic red-brown and small sized papulosquamous lesions arise in crops and usually involve trunk, upper extremities and buttocks
- Parakeratosis, spongiosis, intraepidermal lymphocytes and erythrocytes, superficial perivascular or lichenoid lymphocytic infiltrate, focal interface change, melanophages and extravasated erythrocytes
Terminology
- Guttate parapsoriasis, chronic lichenoid pityriasis, parapsoriasis lichenoides chronica
ICD coding
- ICD-10: L41.1 - pityriasis lichenoides chronica
Epidemiology
- Commonly affects children and young adults with equal sex ratios (slightly more common in males)
- Commonly occurs in winter and fall
- Prognosis is good
- References: J Am Acad Dermatol 2006;55:557, General Dermatology 2009;13:197
Sites
- Trunk, proximal extremities and buttocks
Pathophysiology
- Not exactly understood; infectious and drug related hypersensitivity reactions and premycotic lymphoproliferative disorder are the main hypotheses
Etiology
- Associated with genetic and environmental factors (viral infections, autoimmune diseases, drug and vaccine induced, etc.); there is some evidence of association with lymphoproliferative disorder
Clinical features
- Acute form: erythematous, vesiculopustular and necrotic lesions with the symptoms of itching and burning
- Chronic form: reddish brown papules, postinflammatory hypo and hyperpigmentation can be seen
- Upper limbs and flexor surfaces are more frequently involved than lower limbs and extensor surfaces; central, diffuse and peripheral forms can occur and atypical presentation may appear (Dermatol Pract Concept 2013;3:7, J Drugs Dermatol 2019;18:690)
Diagnosis
- Clinical history and examination (Pediatr Dermatol 2018;35:213)
- Skin biopsy (lichenoid and vasculopathic pattern) and immunofluorescence (IgM and C3 in the superficial dermal blood vessel walls) (Pediatr Dermatol 2015;32:579)
Laboratory
- Some patients have elevated serum immune complexes
Prognostic factors
- Relapsing and remitting course persists for months or a few years
- Treatment may or may not relieve symptoms
Case reports
- 5 year old boy with an eruption that started 10 days after second dose of MMR vaccine (J Dermatol 2012;39:492)
- 7 year old boy with lesions in centripetal distribution, which subsided and left behind hypopigmented macules (Rev Chil Pediatr 2015;86:121)
- 37 year old woman developed papular eruption after first dose of MMR vaccine (J Dtsch Dermatol Ges 2020;18:758)
- 38 year old man with cutaneous lesions after the treatment of ankylosing spondylitis (J Drugs Dermatol 2020;19:560)
- 15 patients had papular lesions mimicking pityriasis lichenoides chronica (PLC) in mycosis fungoides (MF) patients receiving PUVA (Arch Dermatol Res 2019;311:673)
- Few reports of PLC cases have been associated with lymphoma:
- 17 year old girl with the diagnosis of cytotoxic MF evolving from PLC (Dermatology 2002;205:176)
- 91 year old man presented with PLC as paraneoplastic dermatosis (Indian J Hematol Blood Transfus 2014;30:246)
Treatment
- Topical steroids
- Topical immunomodulators (tacrolimus, pimecrolimus)
- Oral antibiotics (erythromycin, tetracycline such as doxycycline)
- Phototherapy
- Systemic steroids
- Reference: Am J Clin Dermatol 2007;8:29
Clinical images
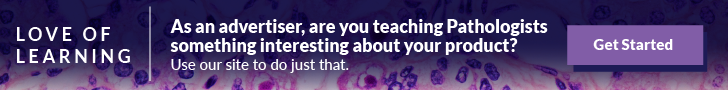
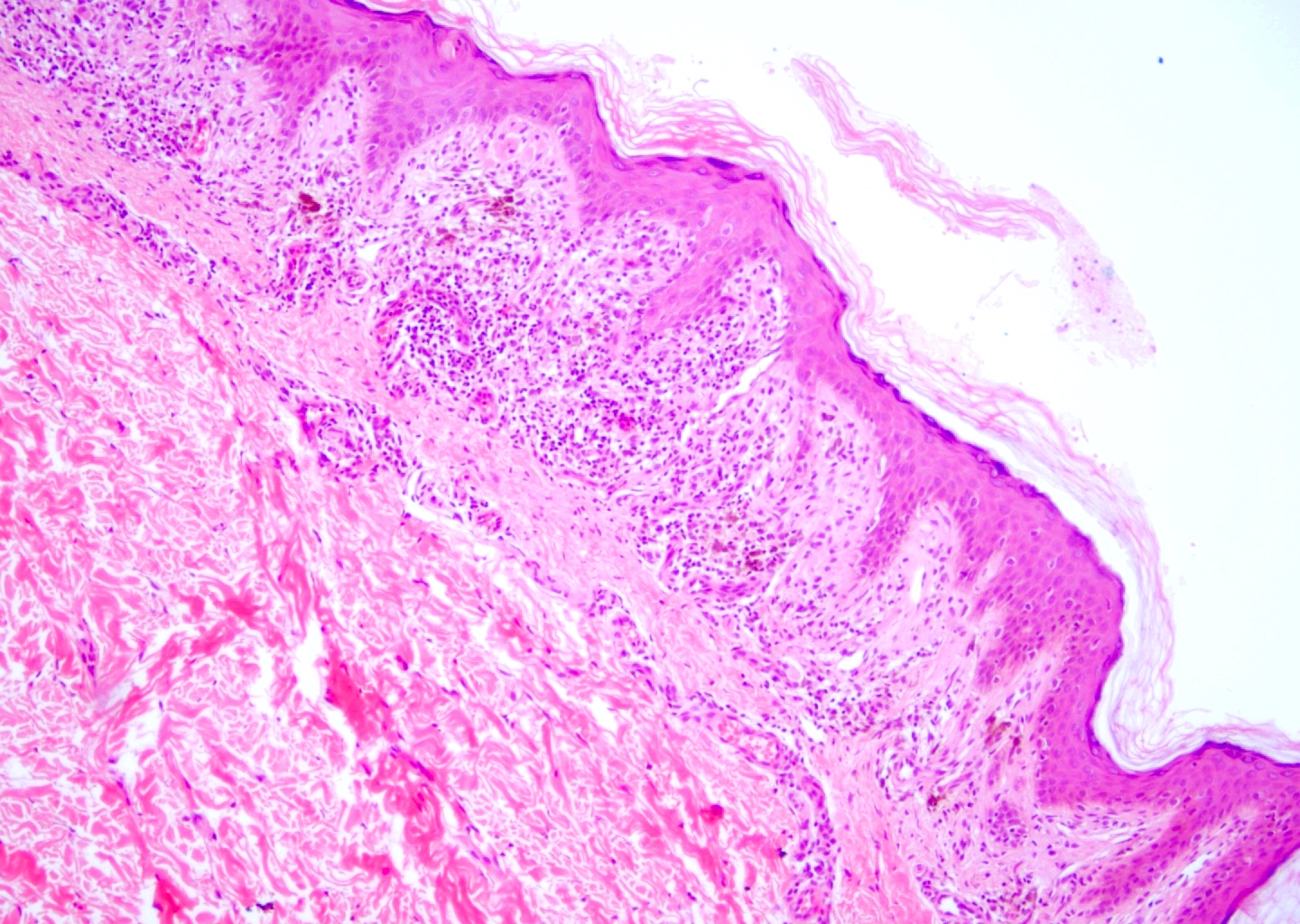
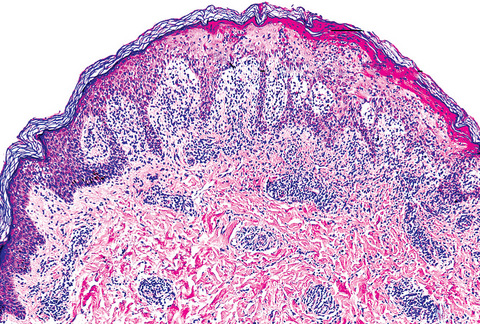
Microscopic (histologic) description
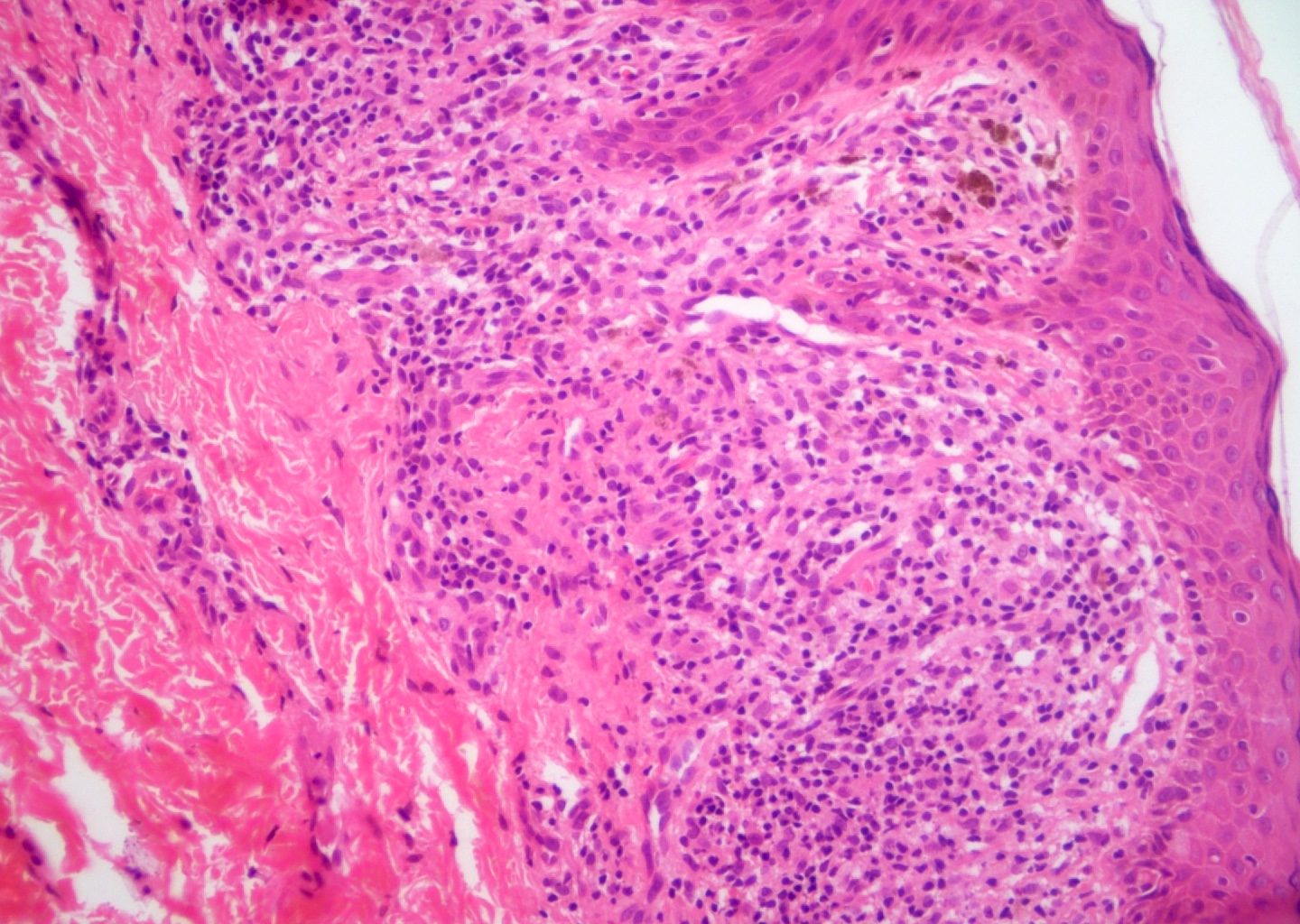
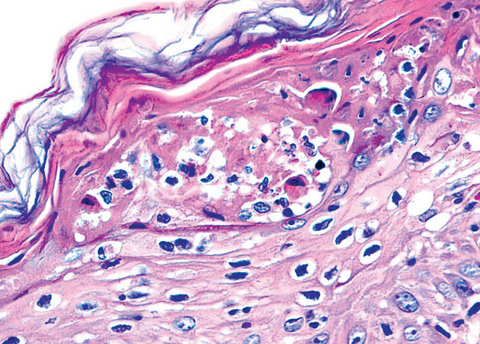
- Parakeratosis, mild to moderate acanthosis, mild spongiosis, sparse necrotic keratinocytes, minimal vacuolar degeneration of the basal layer, focal exocytosis of small numbers of lymphocytes and intraepidermal erythrocytes
- Mild superficial perivascular and lichenoid lymphocytic infiltrate, focal interface change, melanophages and extravasated erythrocytes without (occasionally focal) fibrinoid necrosis of vessels; neither eosinophils nor plasma cells present
- Dilatation and congestion of superficial vessels, papillary dermal edema and pigment incontinence
- Pityriasis lichenoides et varioliformis acuta (PLEVA, acute form of the disease) is similar to PLC but with more pronounced histologic features: more interface damage, more inflammation, more erythrocytes in dermis and epidermis
- Acute and chronic refer to the characteristics of the lesions
- Also shares clinical and some immune histologic features with lymphomatoid papulosis (Am J Surg Pathol 2012;36:1021)
- CD4:CD8 ratio > 1; monoclonal T cell population may mimic MF (Indian J Dermatol 2012;57:424)
- Some cases reported as a form of MF and T cell dyscrasias arising in association with pitryiasis lichenoides in children and adults (J Turk Acad Dermatol 2014;8:1483c3, Australas J Dermatol 2021 Nov 9 [Epub ahead of print])
- Adnexotropism was described (Am J Dermatopathol 2020;42:1)
Microscopic (histologic) images
Contributed by Gülçin (Güler) Şimşek, M.D. and Mark R. Wick, M.D.
Immunofluorescence description
- IgM and C3 in the walls of the superficial dermal blood vessels and along the dermoepidermal junction in some patients
Sample pathology report
- Trunk, papulosquamous lesion, punch biopsy:
- Lichenoid / perivascular interface dermatitis (given the history, compatible with pitryiasis lichenoides chronica) (see comment)
- Comment: Parakeratosis, mild superficial perivascular and lichenoid lymphocytic infiltrate, focal interface change, exocytosis of small numbers of lymphocytes and extravasated dermal and intraepidermal erythrocytes. The histologic features are consistent with pitryiasis lichenoides chronica. Clinicopathologic correlation is recommended.
Differential diagnosis
- Guttate psoriasis:
- Focal parakeratosis consisting of neutrophils and granular layer loss
- Papillary dermis includes lymphocytes and neutrophils
- Pityriasis rosea:
- Nonspecific features of superficial perivascular dermatitis
- Erythroid extravasation is frequent but intraepidermal erythrocytes is uncommon
- Lichen planus:
- Lichenoid and interface dermatitis
- Significant vacuolar degeneration of the basal layer, many cytoid bodies
- Syphilis:
- Great imitator; physical examination and skin biopsy may be misdiagnosed as pitryiasis lichenoides, especially PLEVA
- Serologic tests are needed
- Lymphomatoid papulosis:
- Immunohistochemistry can be needed for challenging cases (Dermatol Clin 2019;37:471)
- Mycosis fungoides, poikilodermatous / lichenoid types:
- Intraepidermal atypical lymphocytes and Pautrier’s microabscess (Ann Dermatol 2016;28:540)
- Inflammatory vitiligo:
- Hypopigmented lesions may resemble PLC and may be evident for as long as 2 years
- Head and neck involvement should think vitiligo
- Histology shows more basal hypopigmentation and absence of melanocytes (Australas J Dermatol 2021 Nov 9 [Epub ahead of print], Am J Dermatopathol 2016;38:608)
- Lichenoid drug eruption:
- Lesions are reversible, dependent on drug withdrawal (Dermatol Online J 2017;23:13030/qt7xd8j71z)
- Viral exanthem:
- Usually lesions are not crusted and heal in a few months
- Atypical viral exanthems may be problematic (Infect Dis Rep 2012;4:e12)
Additional references
Board review style question #1
An 11 year old boy presented with depigmented papulosquamous lesions on the anterior part of the trunk and upper extremities. Clinical picture and biopsy reveal the findings shown in the images above. What is the most likely diagnosis?
- Lichen planus
- Lichenoid drug eruption
- Mycosis fungoides
- Pityriasis lichenoides chronica
- Pityriasis lichenoides et varioliformis acuta
Board review style answer #1