Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sulejmani P, Schukow C, Ahmed A. Regressed melanoma (tumoral melanosis). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticregressedmelanoma.html. Accessed April 25th, 2024.
Definition / general
- The definition and classification of histologic regression in melanoma can vary considerably among institutions and even among individual pathologists (Lab Invest 2017;97:657)
- On histologic examination, regression can be characterized by the presence of a host response to melanoma consisting of dermal melanophages with associated fibrosis, chronic inflammation, telangiectasias, epidermal attenuation or apoptosis of keratinocytes / melanocytes
Essential features
- Regression in melanoma can occur spontaneously or in response to treatment (Lab Invest 2017;97:657)
- Histopathological examination reveals a dermal infiltrate comprised of melanophages, chronic inflammation, fibrosis and telangiectasias
- Conflicting data have been reported on the prognosis of regressed melanoma; although it has been proposed that partial regression in < 50 - 75% of tumor cells has no effect on prognosis, whereas extensive regression > 75% of tumor tissue may be associated with metastatic disease (An Bras Dermatol 2021;96:797, Arch Dermatol 2002;138:603, World J Surg 1992;16:196, Arch Dermatol 1987;123:1326)
Terminology
- Regressive melanoma / partial regression
- Tumoral melanosis
ICD coding
Epidemiology
- Melanoma is the sixth most common fatal malignancy in the United States and the second most common cancer in women aged 20 - 29 years (Exp Ther Med 2020;20:87)
- It is expected that ~1 million cases of melanoma are diagnosed yearly in the United States
- Patients < 50 years of age have a lower incidence of melanoma but a higher rate of new, changed and regressed nevi than patients > age 50 (Arch Dermatol 2005;141:998)
Sites
- Regression in melanoma can occur throughout the body
- Although rare, fully regressive melanomas are most commonly found on the lower extremities and trunk in elderly patients (J Clin Aesthet Dermatol 2016;9:42)
- ~12% are located on the head or neck, while ~9% of regressive melanomas are located on the hands or feet (J Clin Aesthet Dermatol 2016;9:42)
Pathophysiology
- Melanoma cells express proteins with strong immunogenic effects such that melanomas with increased expression of MelanA (MART1), gp100 or HLA-A-0201 show increased rates of spontaneous regression (EJC Suppl 2013;11:97)
- Regression is a phenomenon in which the host's cytotoxic T lymphocytes attack the primary melanocytic tumor cells and leave behind a fibrotic scar (J Clin Aesthet Dermatol 2016;9:42)
- Regression of melanoma clinically can demonstrate subtle hyperpigmentation, followed by depigmentation of parts of or the entirety of the lesion yielding blue, pink, white or gray areas (Lab Invest 2017;97:657)
- Some authors postulate 3 levels of regression (Lab Invest 2017;97:657)
- Early stage: characterized by mononuclear inflammatory cell infiltrate with mature lymphocytes and keratinocytes and dermal layer disruption
- Intermediate stage: characterized by lack of melanocytes, the presence of macrophages, lymphohistiocytic infiltrate, fibroblastic proliferation, mild collagen deposition and increased vascular pattern in the superficial dermal layer
- Late stage: lesion with complete absence of melanocytes, fibrosis in the superficial / papillary dermis, ectatic capillaries, variable numbers of melanophages and a small number of inflammatory cells (Exp Ther Med 2020;20:87)
Etiology
- Risk factors for melanoma include ultraviolet (UV) light radiation, prior history of sunburns, increased numbers of congenital or acquired nevi and family history of melanoma (i.e., genetic susceptibility) (Exp Ther Med 2020;20:87)
- There are no specific factors that cause regression; however, the majority of the cases are described after metastasis (J Natl Cancer Inst 2001;93:1047)
Clinical features
- ~10 - 35% of cutaneous melanoma cases may completely or partially spontaneously regress (Histopathology 1992;20:315)
- Histologic regression may not necessarily correlate with clinical regression (i.e., clinically looks like melanoma)
- Management of regressed melanoma still determined by stage (dependent on Breslow depth and presence or lack of ulceration)
Diagnosis
- Diagnosis of regressive melanoma is made in conjunction with clinical, dermatoscopic and pathologic findings (J Clin Aesthet Dermatol 2016;9:42)
- Diagnosis depends on histologic examination
- Dermatoscopic examination of fully regressed melanoma may reveal scar-like depigmentation, pink macules, linear / irregular vessels, globular vessel patterns, blue-gray peppered papular remnants and white transverse bands (Br J Dermatol 2008;158:1224)
Prognostic factors
- According to a recent cohort study of 17,721 Dutch and 4,980 Australian patients with stage 1 or 2 melanoma, regression was significantly associated with improved overall survival (especially tumors with Breslow thickness ≤ 4.0 mm) (JAMA Dermatol 2021;157:166)
- However, it is also known that the majority of regressive melanomas are discovered after the occurrence of metastasis, making it a potential negative prognostic factor in melanoma (Exp Ther Med 2020;20:87)
Case reports
- 40 year old man with metastasis to his brain, 45 year old woman with left sided axillary lymphadenopathy and 45 year old man with a primary lesion on his back (Rom J Morphol Embryol 2014;55:635)
- 62 year old man with completely regressed melanoma on his back without metastasis (J Clin Aesthet Dermatol 2016;9:42)
- 62 year old woman with multiple lymph nodes, brain and lung metastases (Exp Ther Med 2020;20:87)
Treatment
- Mohs micrographic surgery may be appropriate in certain cases; if signs of regression are present at Mohs layer margins, removal of additional layers may be required (Clin Cosmet Investig Dermatol 2018;11:309)
- Immunotherapies such as PD1 and CTLA4 blockers have shown efficacy in some patients, especially when combined with chemotherapy or radiotherapy (Radiol Case Rep 2018;13:580)
Clinical images
Gross description
- Asymmetric, variegated or pigmented patch, plaque or nodule with variable black, gray and pink discolorations
- Ulceration, crusting, active exsanguination or granulation may be present
- Reference: J Clin Aesthet Dermatol 2016;9:42
Frozen section description
- Frozen section diagnosis of regressed melanoma is difficult and should be deferred for paraffin sections (Cancer 1983;51:1168)
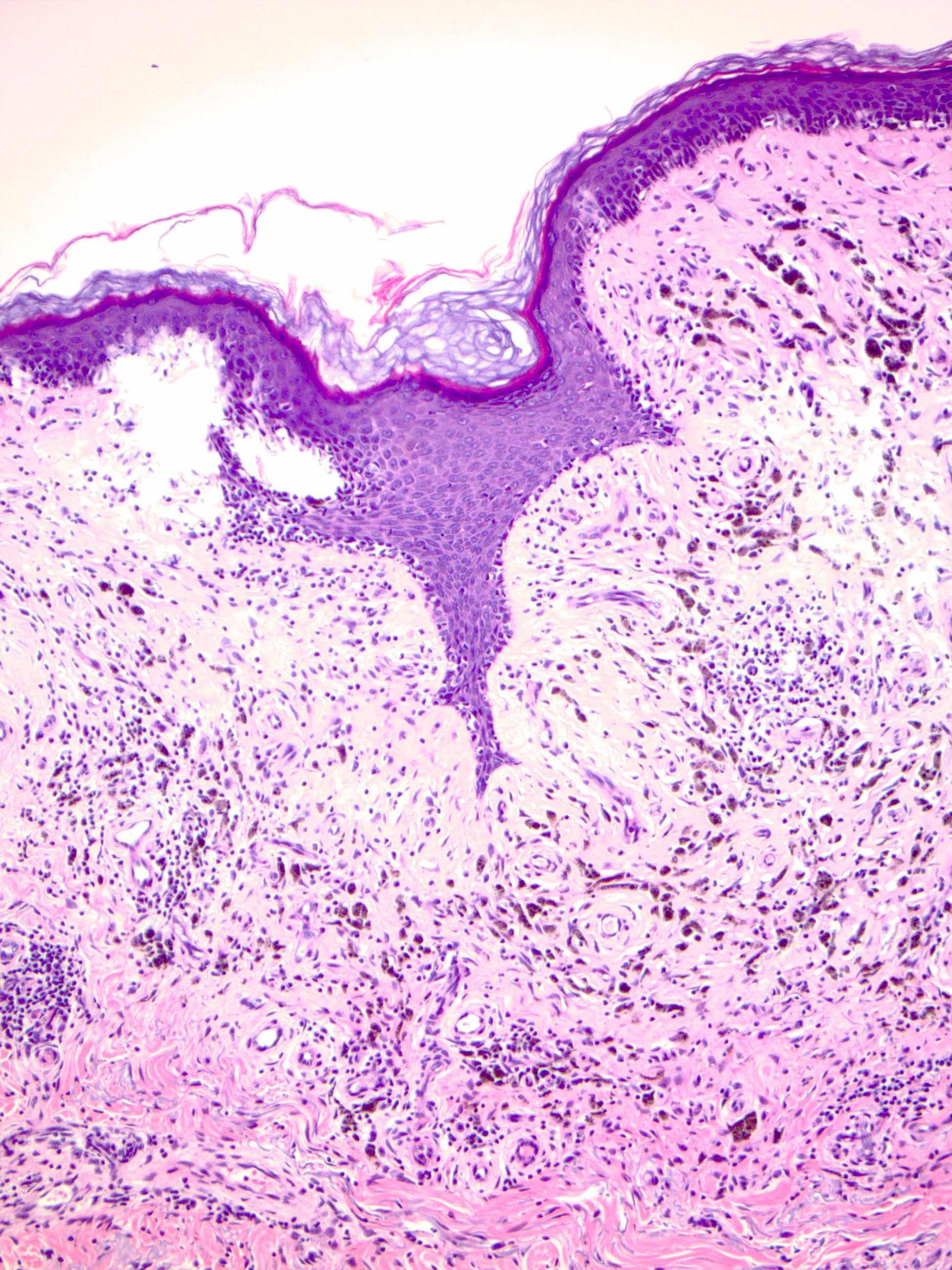
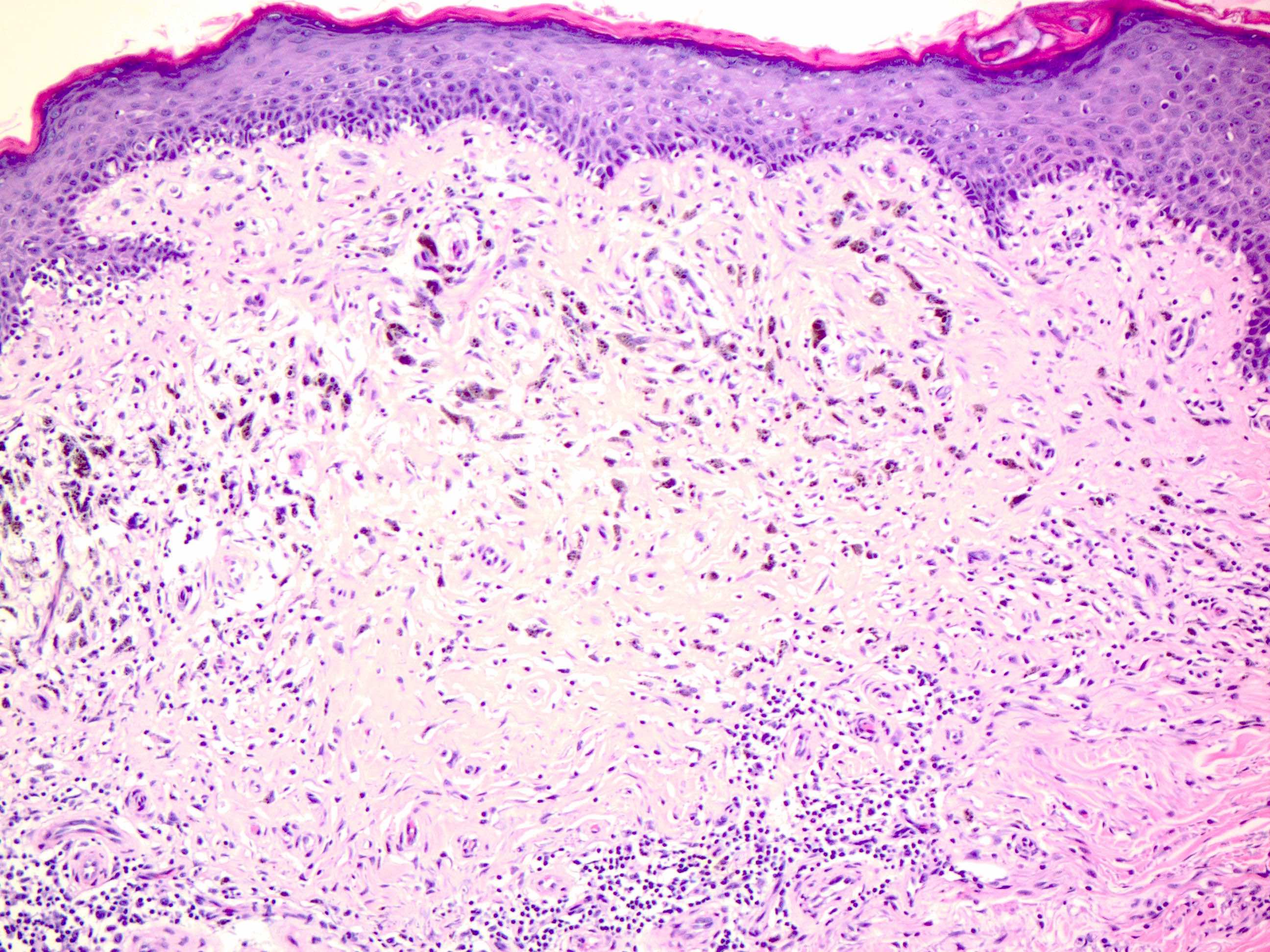
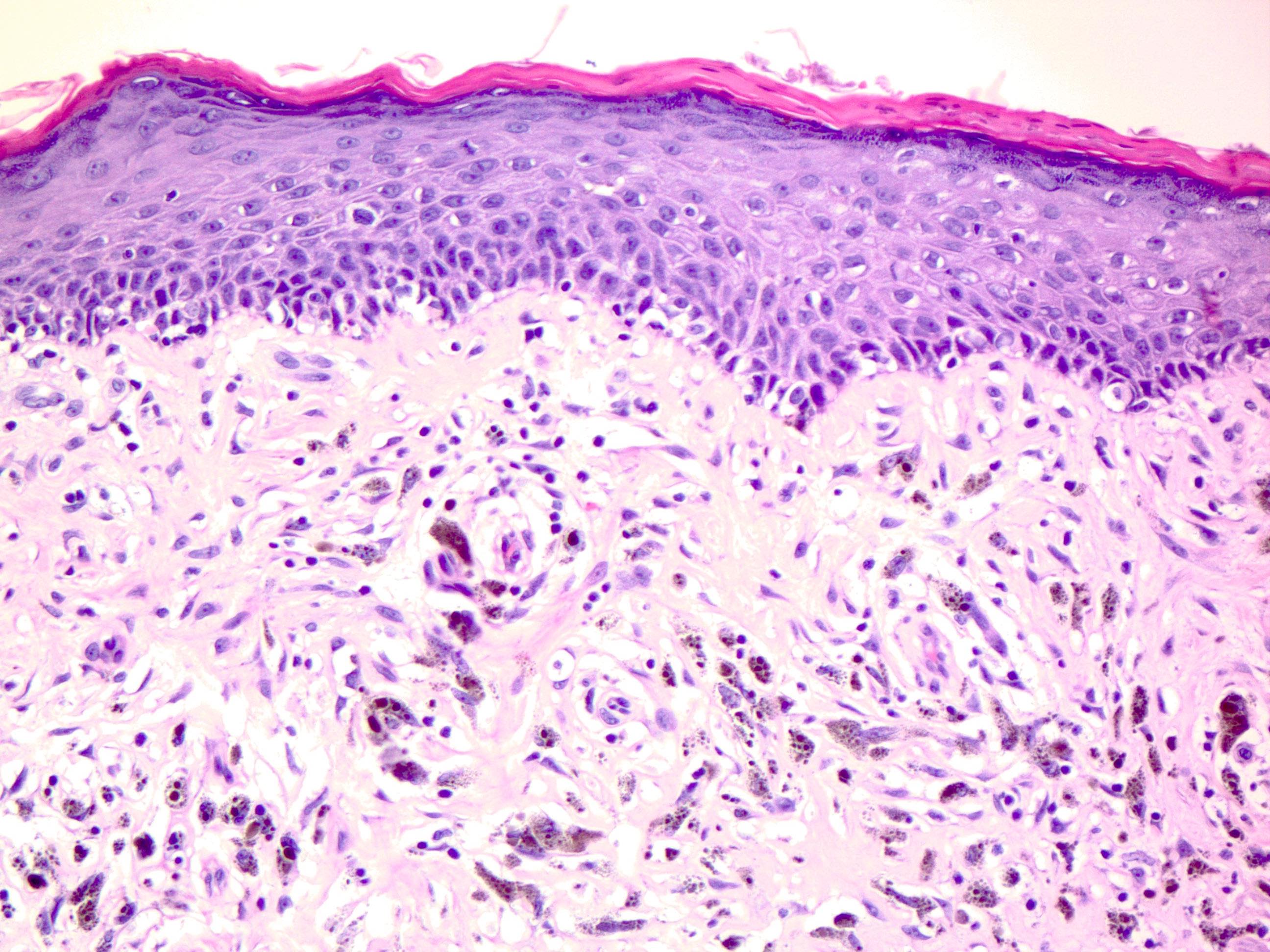
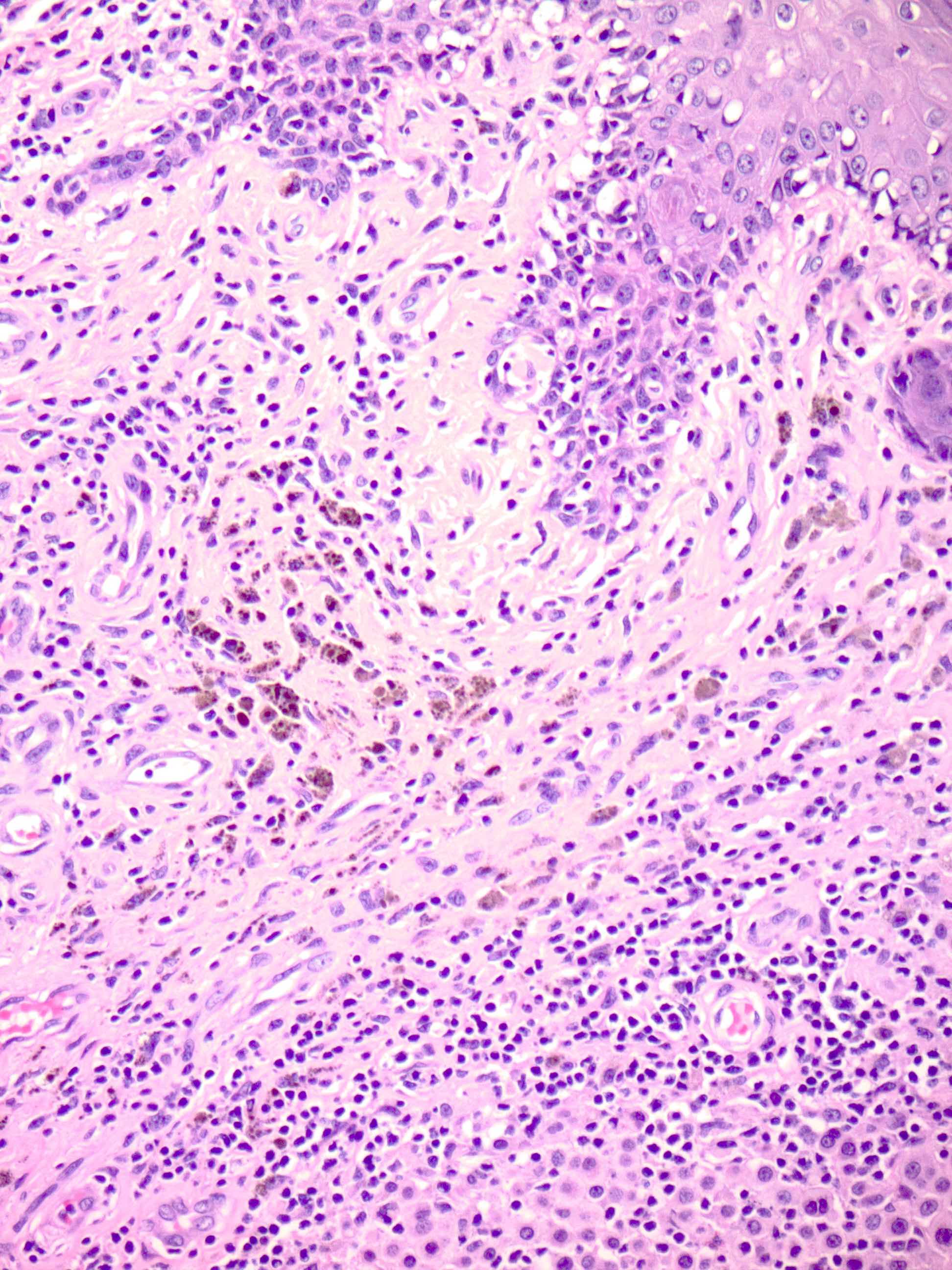
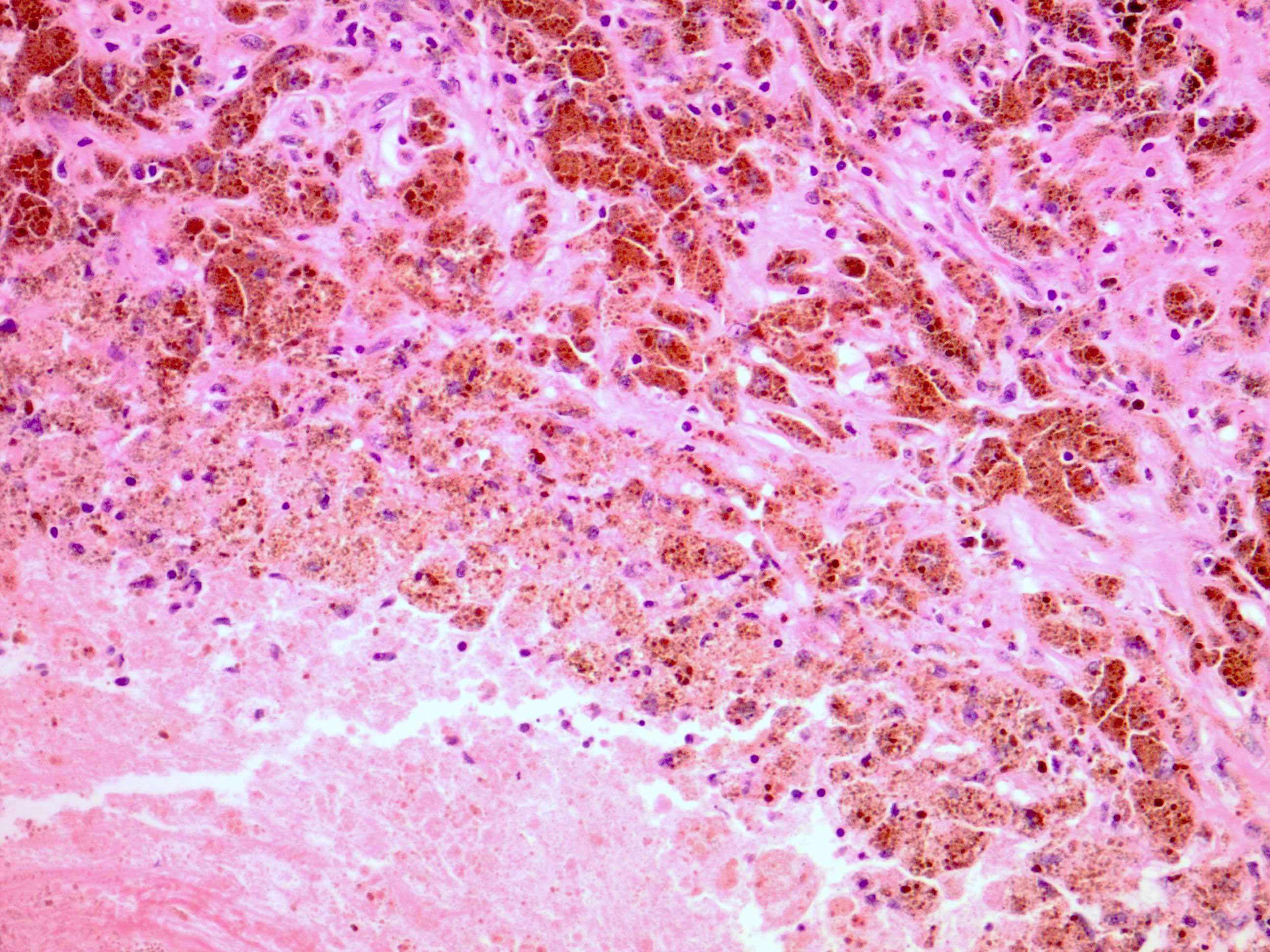
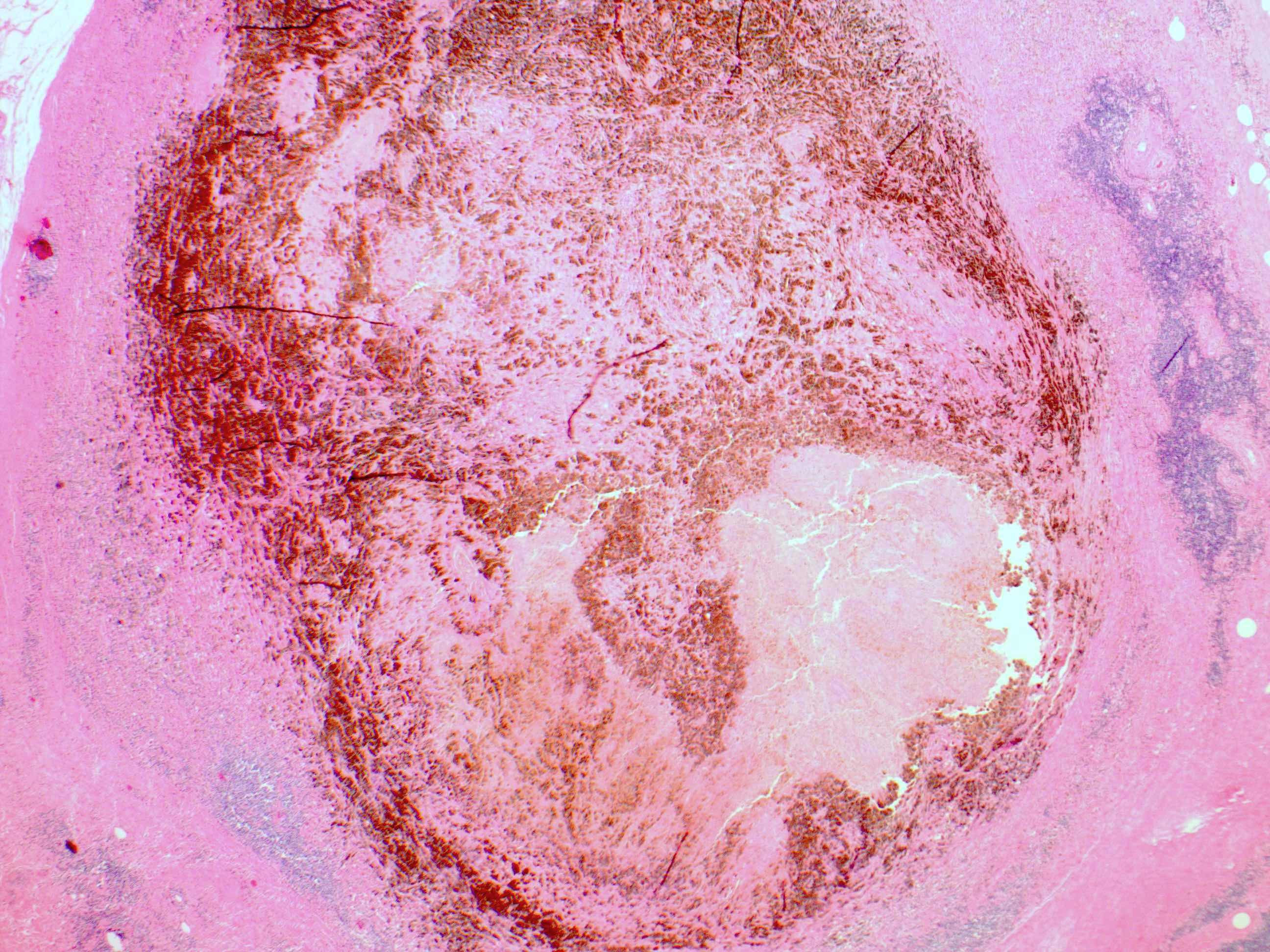
Microscopic (histologic) description
- Variably decreased number of melanoma cells with varying degrees of the following
- Dermal fibrosis
- Inflammatory infiltrate
- Melanophages
- Ectatic blood vessels
- Epidermal attenuation
- Apoptosis of keratinocytes or melanocytes
- Importantly, however, there remains a lack of well defined or agreed upon criteria (Lab Invest 2017;97:657)
Microscopic (histologic) images
Positive stains
- CD3, CD4, CD8 may be present in local T cells, suggesting active immune response (Exp Ther Med 2020;20:87)
- CD68 can highlight melanophages (Lab Invest 2017;97:657)
Negative stains
- Negative staining for MelanA, SOX10, S100, HMB45 (J Cutan Pathol 2015;42:388, Am J Dermatopathol 2007;29:22)
Molecular / cytogenetics description
- Comparative genomic hybridization (CGH) and fluorescence in situ hybridization (FISH) have been found to be helpful in distinguishing difficult cases of melanoma, including regressed melanomas
- CEP6, 6p23, 6p25 and 11q13 are suggestive of malignancy (J Clin Aesthet Dermatol 2016;9:42)
Sample pathology report
- Skin lesion, biopsy:
- Melanoma in situ with features of regression, extends to peripheral margins (see comment)
- Comment: SOX10 and MelanA immunostains highlight the intraepidermal melanocytic proliferation, demonstrating confluence of growth and pagetoid spread, supporting the above diagnosis. Additionally noted is the presence of superficial dermal fibrosis with associated melanophages, chronic inflammation and telangiectasias. On histologic grounds, these findings are most consistent with that of regression. In this regard, the possibility of a previously regressed invasive component cannot be entirely excluded.
Differential diagnosis
- Epidermal nevi:
- Typically present as a linear tan patch or plaque along Blaschko lines that often evolve to become thicker, darker and more verrucous during puberty (Dermatol Clin 2022;40:61)
- Pigmented actinic keratosis:
- A variant of actinic keratosis in which melanin may be present in keratinocytes of the lower epidermis, in melanocytes or in dermal melanophages (Am J Dermatopathol 2022;44:784)
- May show mild keratinocyte dysplasia involving only the basal epidermal layers which can be misdiagnosed as melanoma in situ
- Pigmented basal cell carcinoma:
- A variant of basal cell carcinoma with pigmented nests of basaloid tumor cells
- Peripheral palisading and retraction clefting can commonly be seen on microscopy (J Clin Diagn Res 2013;7:3010)
- Pigmented squamous cell carcinoma:
- A variant of squamous cell carcinoma with abundant pigmentation among intraepidermal / dermal aberrant keratinocytes
- Tumor cells may express both melanin positivity (e.g., MelanA) and cytokeratin (e.g., AE1 / AE3) (An Bras Dermatol 2018;93:96)
- Macular seborrheic keratosis:
- Acanthosis, hyperkeratosis and pseudohorn cysts may be present (Open Access Maced J Med Sci 2018;6:2270)
- Regressed lichenoid keratosis:
- More frequently have necrotic keratinocytes in the epidermis
- Less often have dense infiltrates of melanophages in papillary dermis
Board review style question #1
A 60 year old man presents with an 11 mm x 9 mm asymmetric, variegated pigmented lesion with gray and pink discoloration on his right leg diagnosed as regressed melanoma. Which of the following would be revealed by histopathology?
- Dense, dermal melanophage infiltrate but no atypical melanocytes
- Large basaloid lobules with peripheral nuclear palisade within fibromyxoid stroma
- Lobules of capillary sized vascular channels, lined by single layer of flattened endothelial cells
- Lymphocytes surrounding the entire melanocytic proliferation in a band-like pattern
- Spindled banal appearing melanocytes in the dermis with pigment in the cytoplasm
Board review style answer #1
A. Dense, dermal melanophage infiltrate but no atypical melanocytes. Regressed melanoma can present clinically by initially subtle hyperpigmentation, followed by depigmentation of parts of or the entirety of the lesion yielding blue, pink, white or gray areas. Histopathology is characterized by dense, dermal melanophage infiltrate but no atypical melanocytes. Answer B is incorrect because it describes basal cell carcinoma. Answer C is incorrect because it describes lobular capillary hemangioma. Answer D is incorrect because it describes features of a halo nevus. Answer E is incorrect because it describes blue nevus.
Comment Here
Reference: Regressed melanoma (tumoral melanosis)
Comment Here
Reference: Regressed melanoma (tumoral melanosis)
Board review style question #2
Which immunohistochemical stain is positive in completely regressed melanomas?
- Fontana-Masson
- HMB45
- MelanA
- S100
- SOX10
Board review style answer #2
A. Fontana-Masson. Fontana-Masson stains the melanin pigment in melanophages. Answers B - E are incorrect because regressed melanoma is characterized by negative staining for MelanA, SOX10, S100 and HMB45.
Comment Here
Reference: Regressed melanoma (tumoral melanosis)
Comment Here
Reference: Regressed melanoma (tumoral melanosis)