Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Tran TA, Fanaian N. Spiradenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticeccrinespiradenoma.html. Accessed September 21st, 2025.
Definition / general
- Benign (multi) nodular solid tumor showing eccrine differentiation
Essential features
- Benign neoplasm, excision is curative
- Predilection for head and neck
- Usually asymptomatic but can be painful, belonging to the painful skin tumors in the acronym BLEND TAN EGG (blue rubber bleb nevus, leiomyoma, eccrine spiradenoma, neuroma, dermatofibroma, tufted angioma, angiolipoma, neurilemmoma, endometrioma, granular cell tumor, glomus tumor) (Indian J Dermatol Venereol Leprol 2019;85:231)
- Association with the Brooke-Spiegler syndrome
- Multiple dark nests of cells confined to dermis (blue balls in the dermis) composed of 2 epithelial cell types: small dark peripheral cells and larger pale central cells, with intratumoral lymphocytes
Terminology
- Spiradenoma
- Eccrine spiradenoma
Epidemiology
- Usually in adults
- Rarely congenital or infants (Arch Craniofac Surg 2017;18:211)
Sites
- Head / face and neck
- Other sites (extremities and trunk) less common
Clinical features
- Commonly presenting as solitary nodule
- Rarely as multiple lesions in combination with other types of adnexal tumors as part of the Brooke-Spiegler syndrome
- Predilection site: head and neck area, less commonly trunk and extremities
- Usually asymptomatic, although often cited as a painful skin tumors in the acronym BLEND TAN EGG (blue rubber bleb nevus, leiomyoma, eccrine spiradenoma, neuroma, dermatofibroma, tufted angioma, angiolipoma, neurilemmoma [schwannoma], endometrioma, granular cell tumor, glomus tumor) (Indian J Dermatol Venereol Leprol 2019;85:231)
- Firm, round and smooth surface nodule
- Skin colored, gray-pink, reddish or blue
- Small, usually 1 - 3 cm in size, may be larger, rare giant variants
Diagnosis
- Clinical examination and dermoscopy
- Excisional biopsy for a definitive diagnosis (Arch Craniofac Surg 2017;18:211)
Prognostic factors
- Benign neoplasm
- Malignant transformation is a very rare phenomenon with the malignant component classified into basal cell adenocarcinoma-like, low grade pattern, basal cell adenocarcinoma-like, high grade pattern, invasive adenocarcinoma, NOS, sarcomatoid carcinoma / carcinosarcoma and malignant epithelial myoepithelial carcinoma (Am J Surg Pathol 2009;33:705, Int J Surg Pathol 2020;28:427)
Case reports
- 23 year old woman with zosteriform spiradenoma and spiradenocarcinoma (Indian Dermatol Online J 2015;6:S30)
- 28 year old woman with multiple supraclavicular subcutaneous nodules and intermittent pain (J Cytol 2017;34:39)
- 47 year old woman with shin lump (J Vasc Surg Cases Innov Tech 2019;5:583)
- 75 year old woman with auricular nodule (Ear Nose Throat J 2019;98:545)
- 84 year old woman with nipple mass (Histol Histopathol 2019;34:909)
Treatment
- Complete excision is curative
Clinical images
Gross description
- Usually less than 1 cm, rarely can be larger
- Gray-pink or blue nodule
- Either uninodular or multinodular tumor centered within the dermis
- Extension into the subcutaneous tissue is common
- Usually not connected to epidermis (Arch Craniofac Surg 2017;18:211)
Frozen section description
- Not typically submitted for frozen section
- Histologic features described below
- Might be mistaken for basal cell carcinoma at the time of Mohs surgery (Wien Med Wochenschr 2018;168:218)
Microscopic (histologic) description
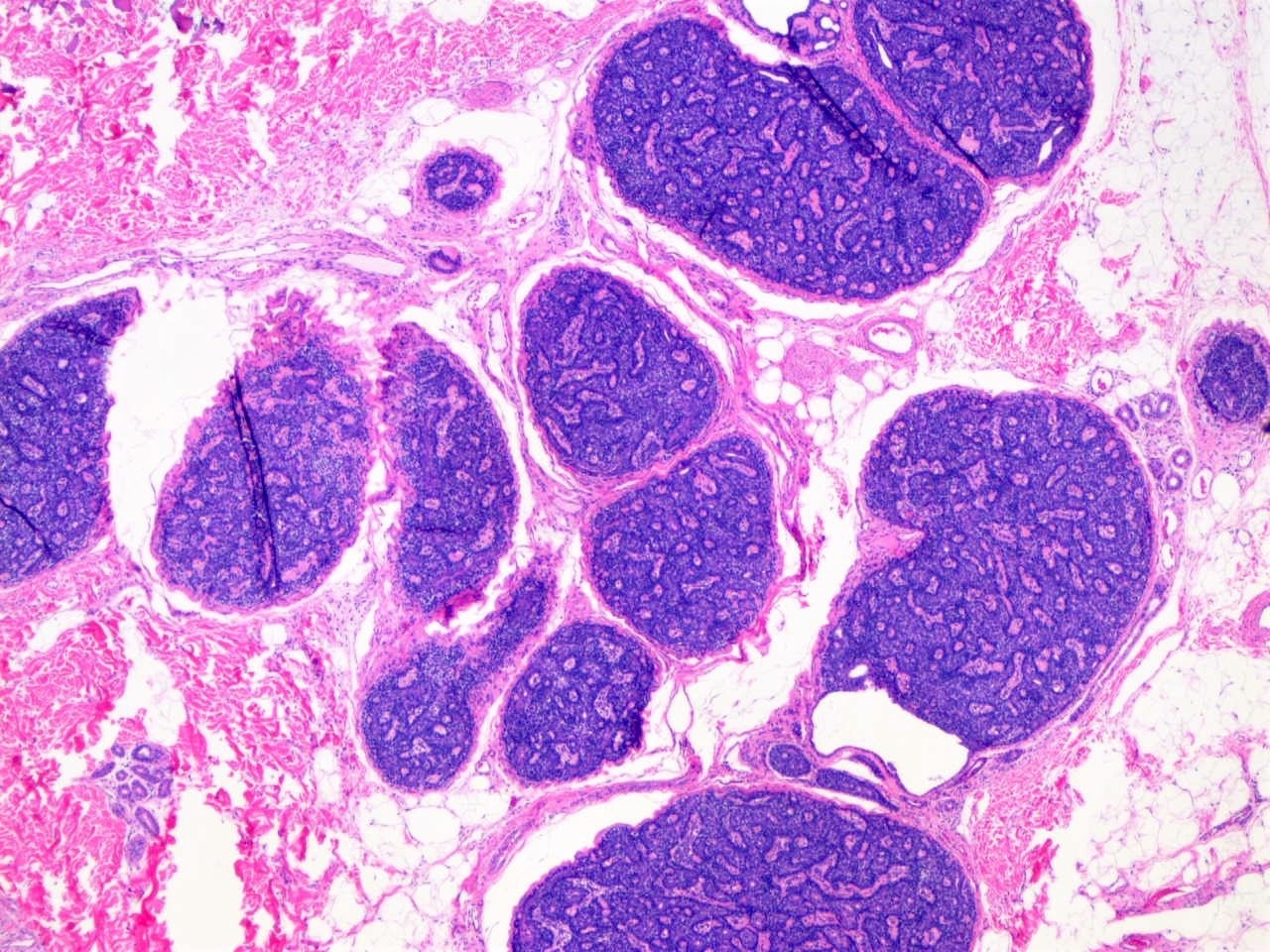
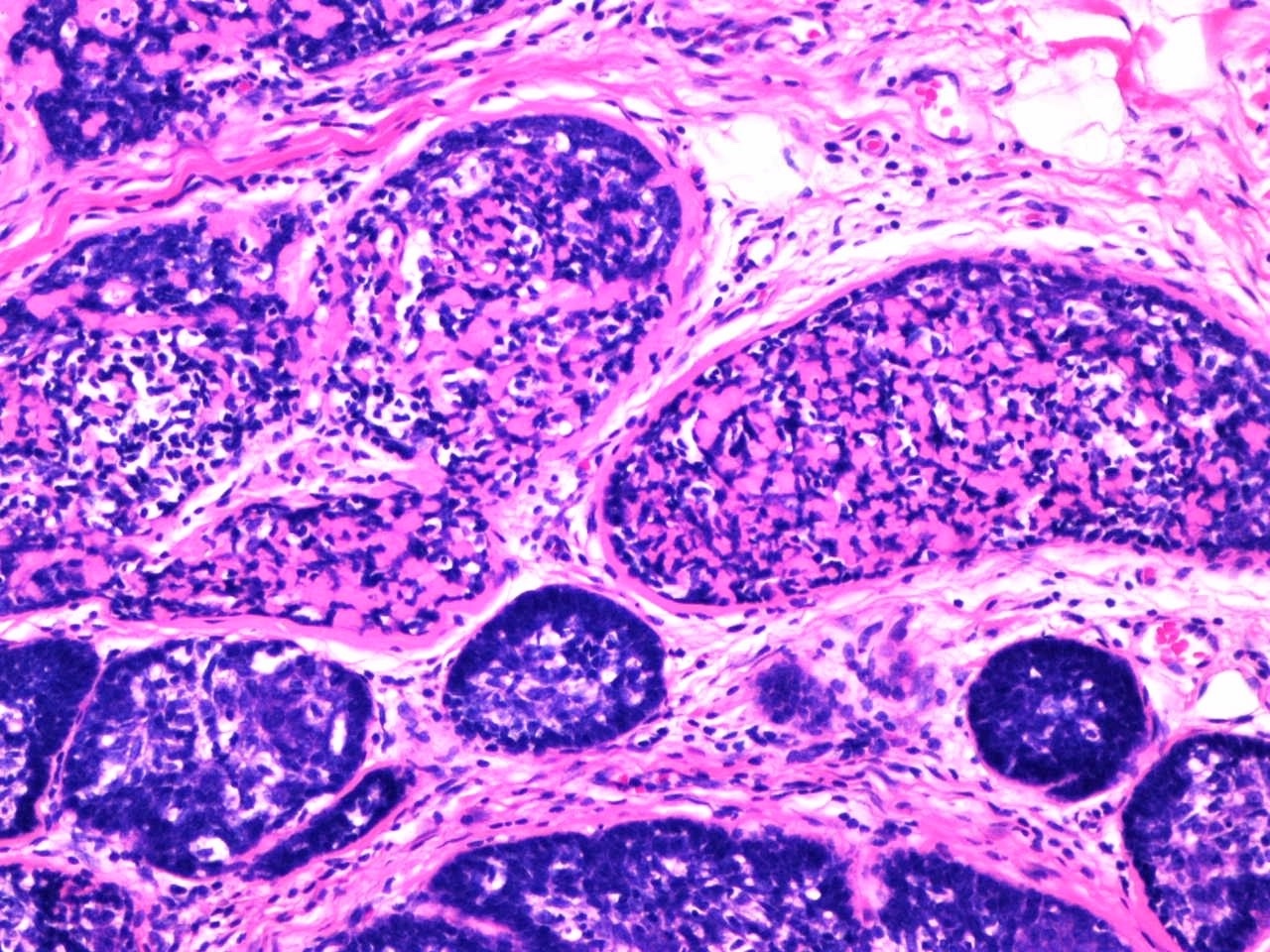
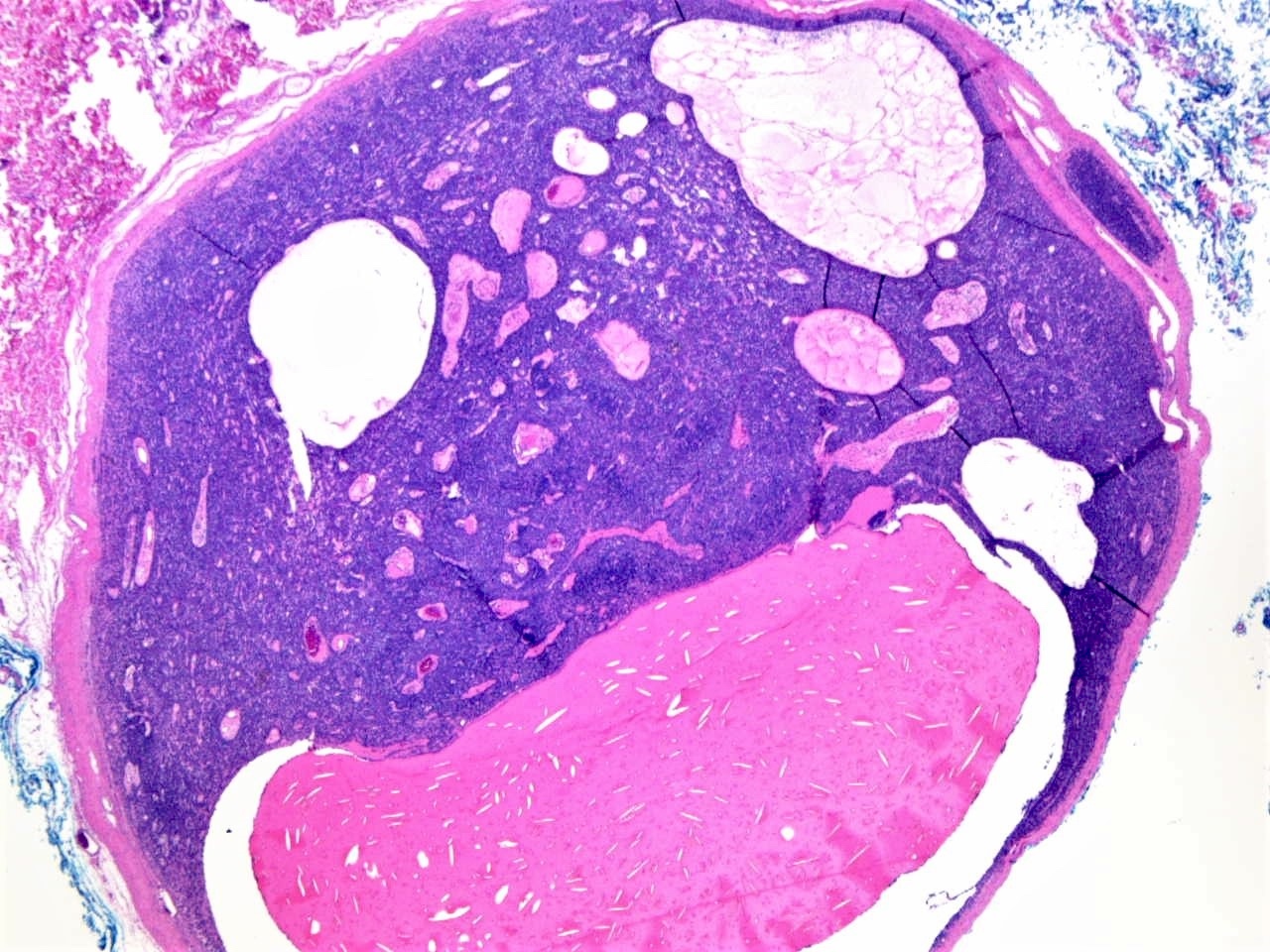
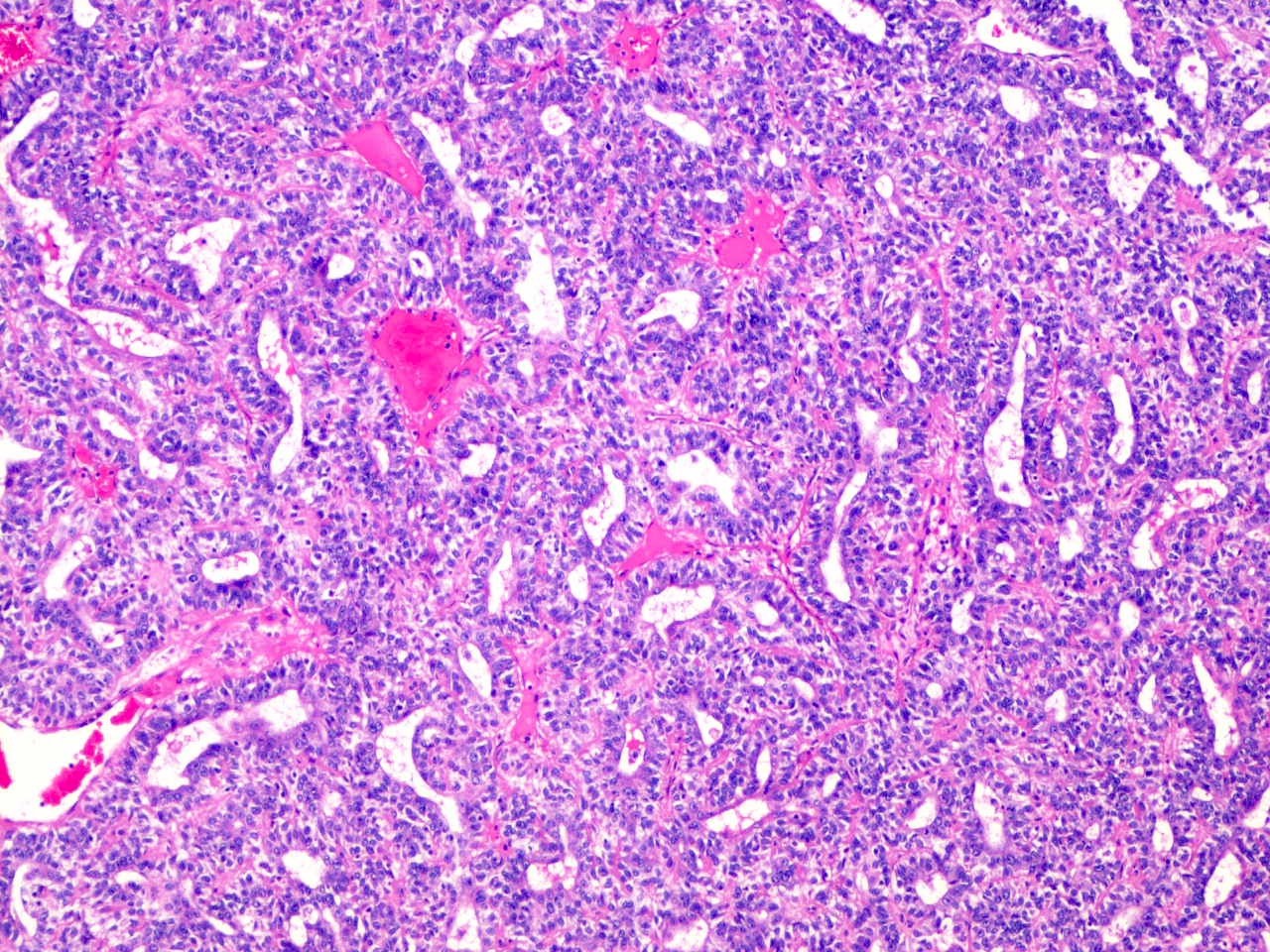
- Circumscribed uninodular or multinodular basophilic tumor (see Figure 1)
- Mostly centered in the dermis (blue balls)
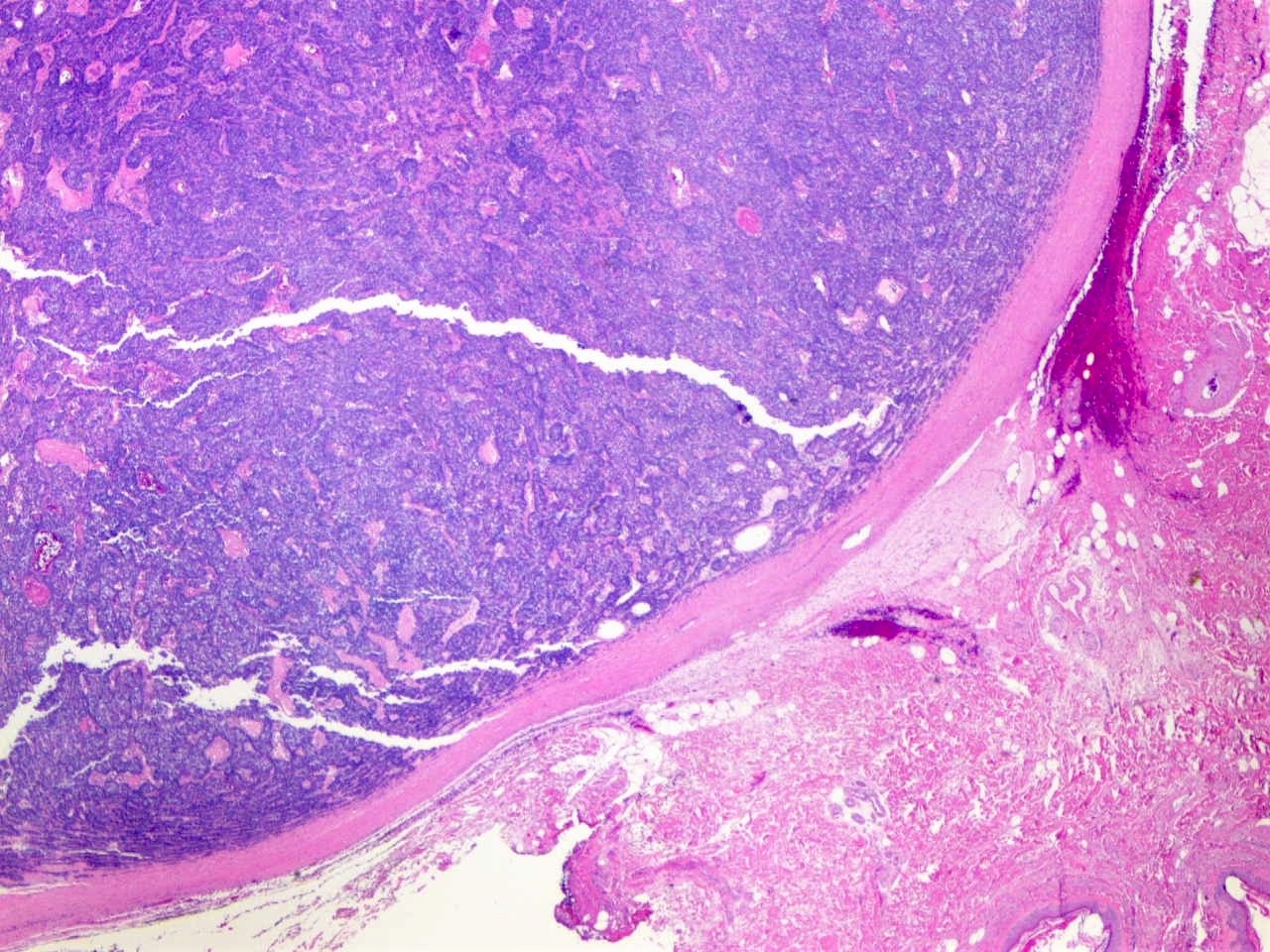
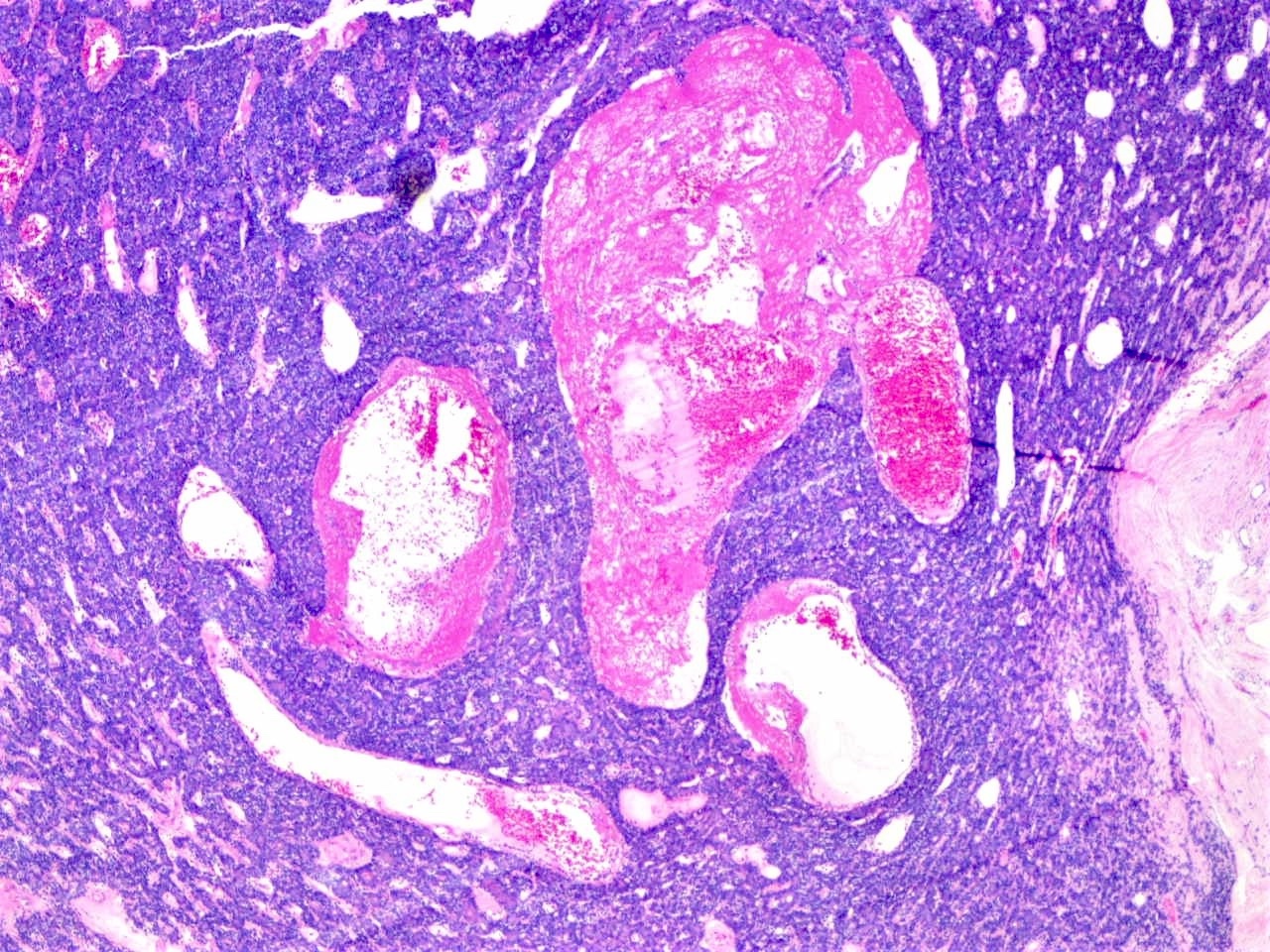
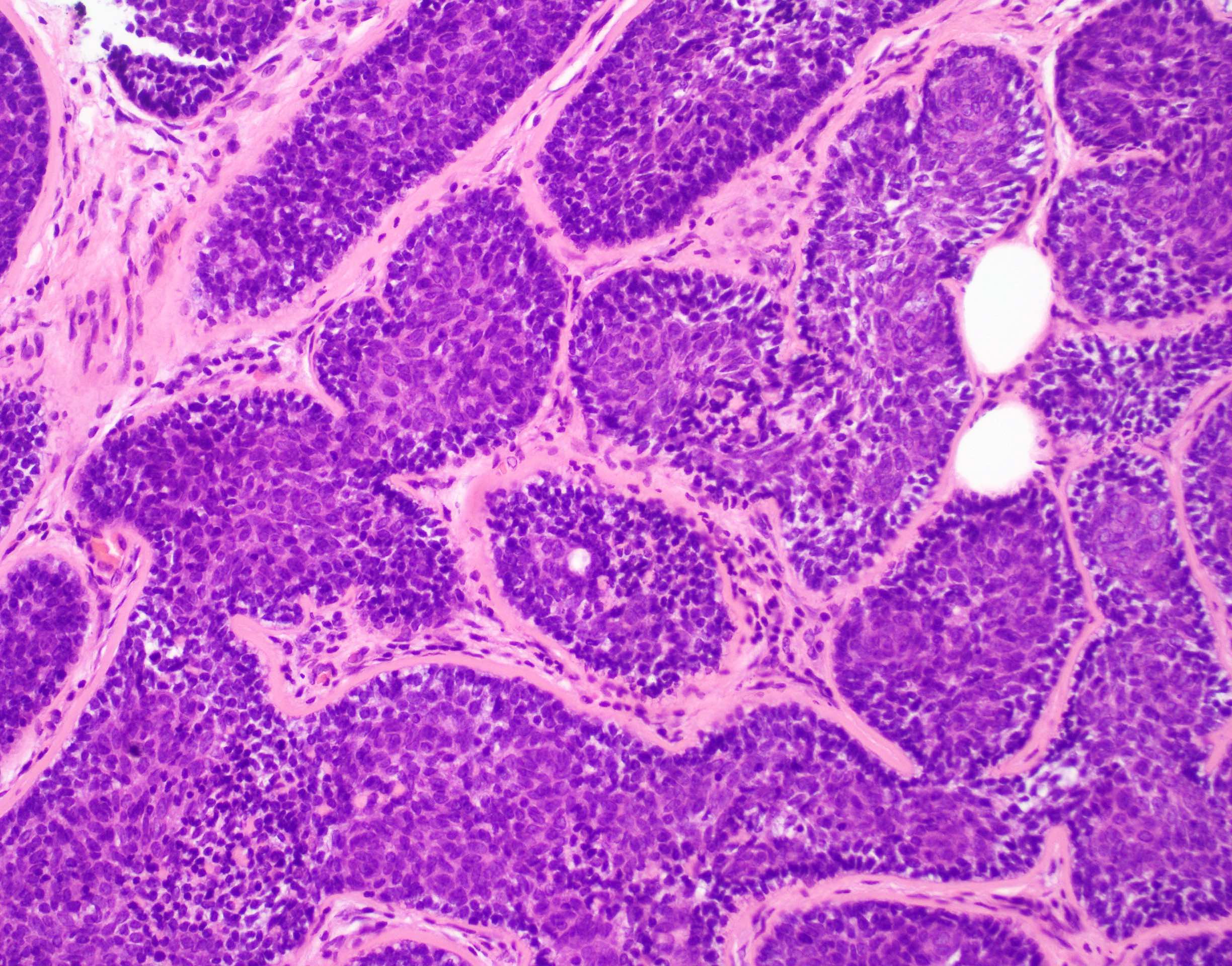
- Some tumors are encapsulated (see Figure 2)
- Extension into the subcutis is common
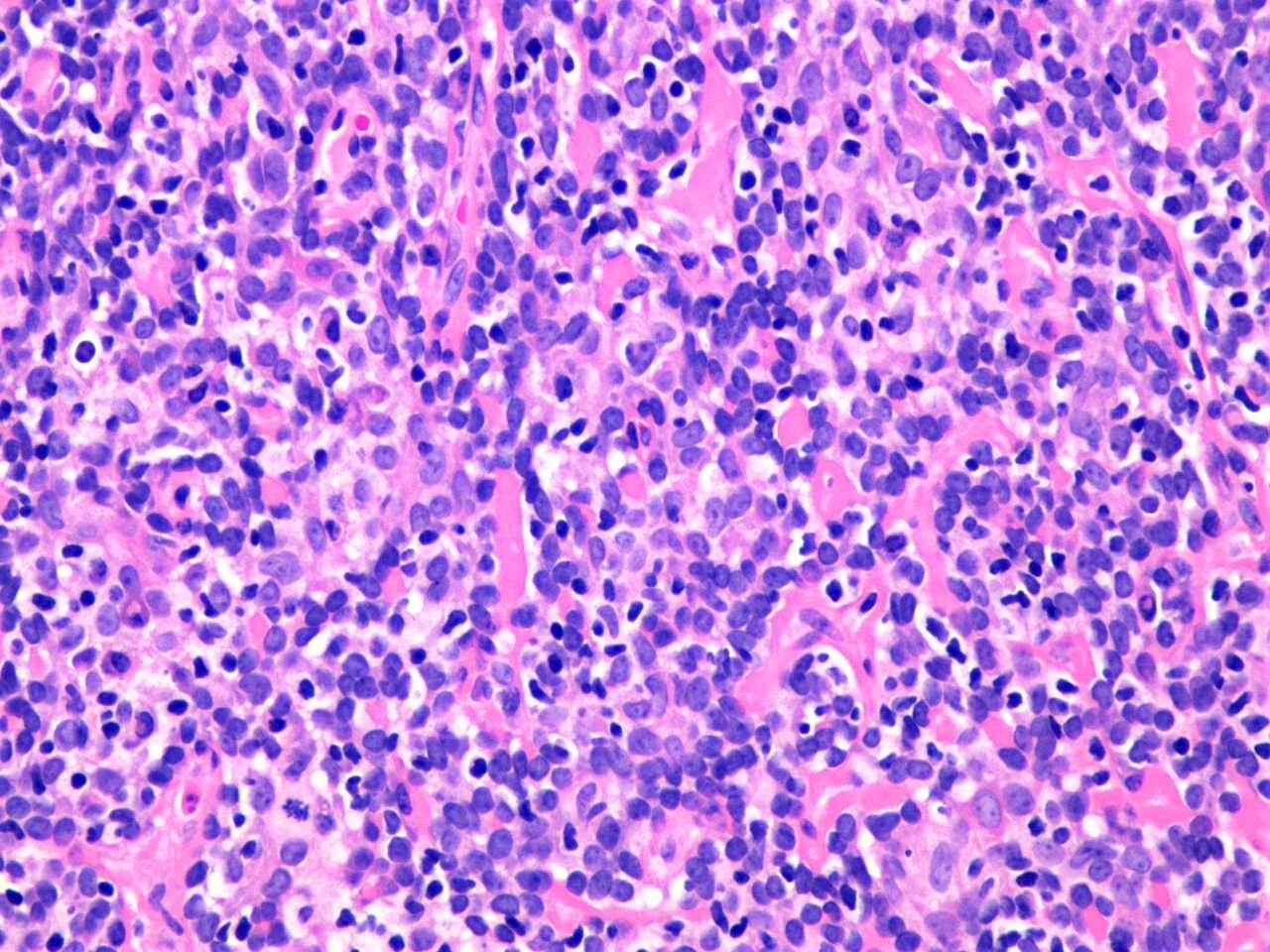
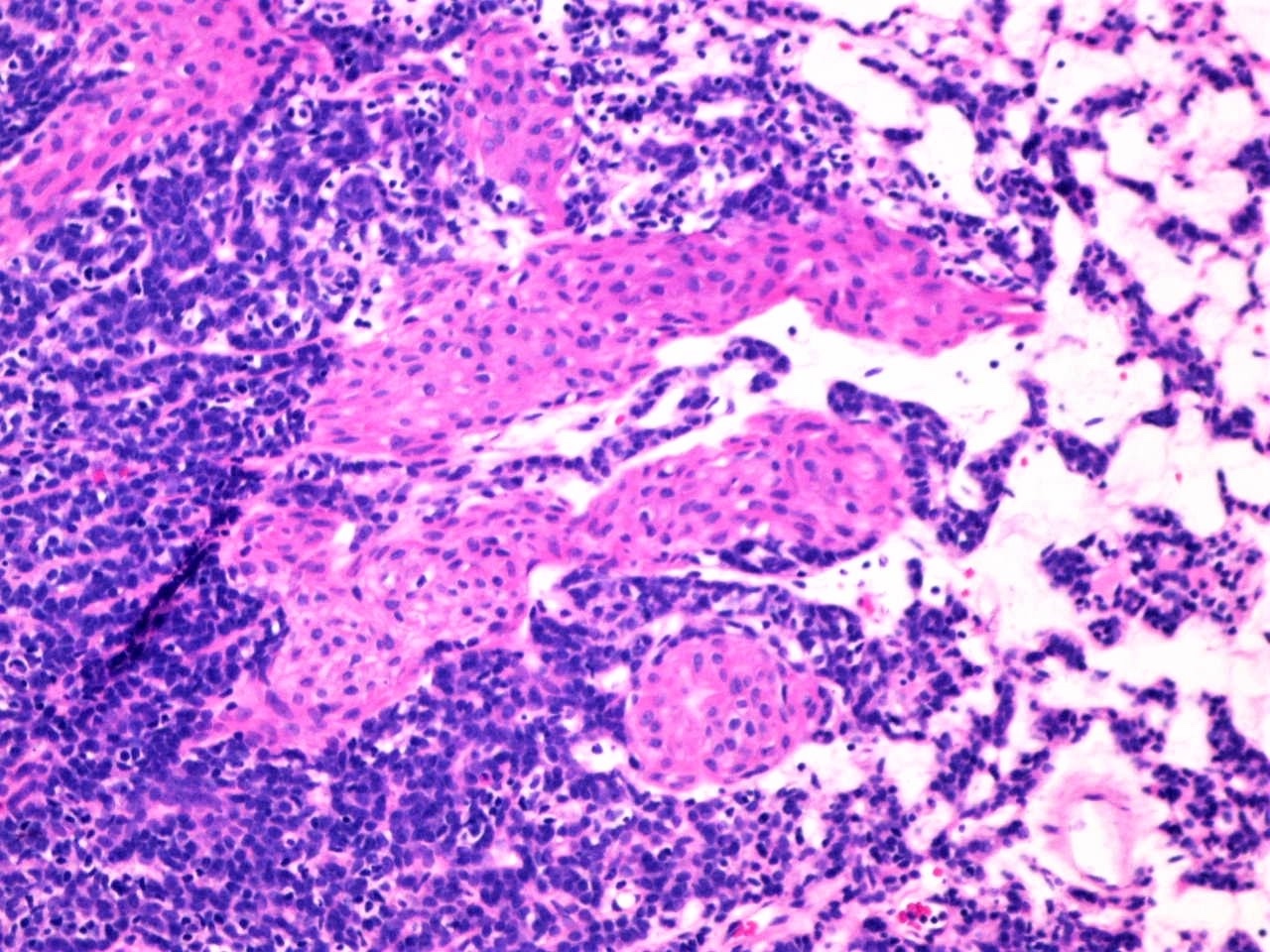
- 2 cell populations in the neoplastic nodules: centrally located large pale cells and small dark basaloid cells at the periphery (see Figure 3)
- Neoplastic cells are arranged in trabecular, reticular or solid fashion
- Intratumoral lymphocytes as an integral component of the tumor (see Figure 3)
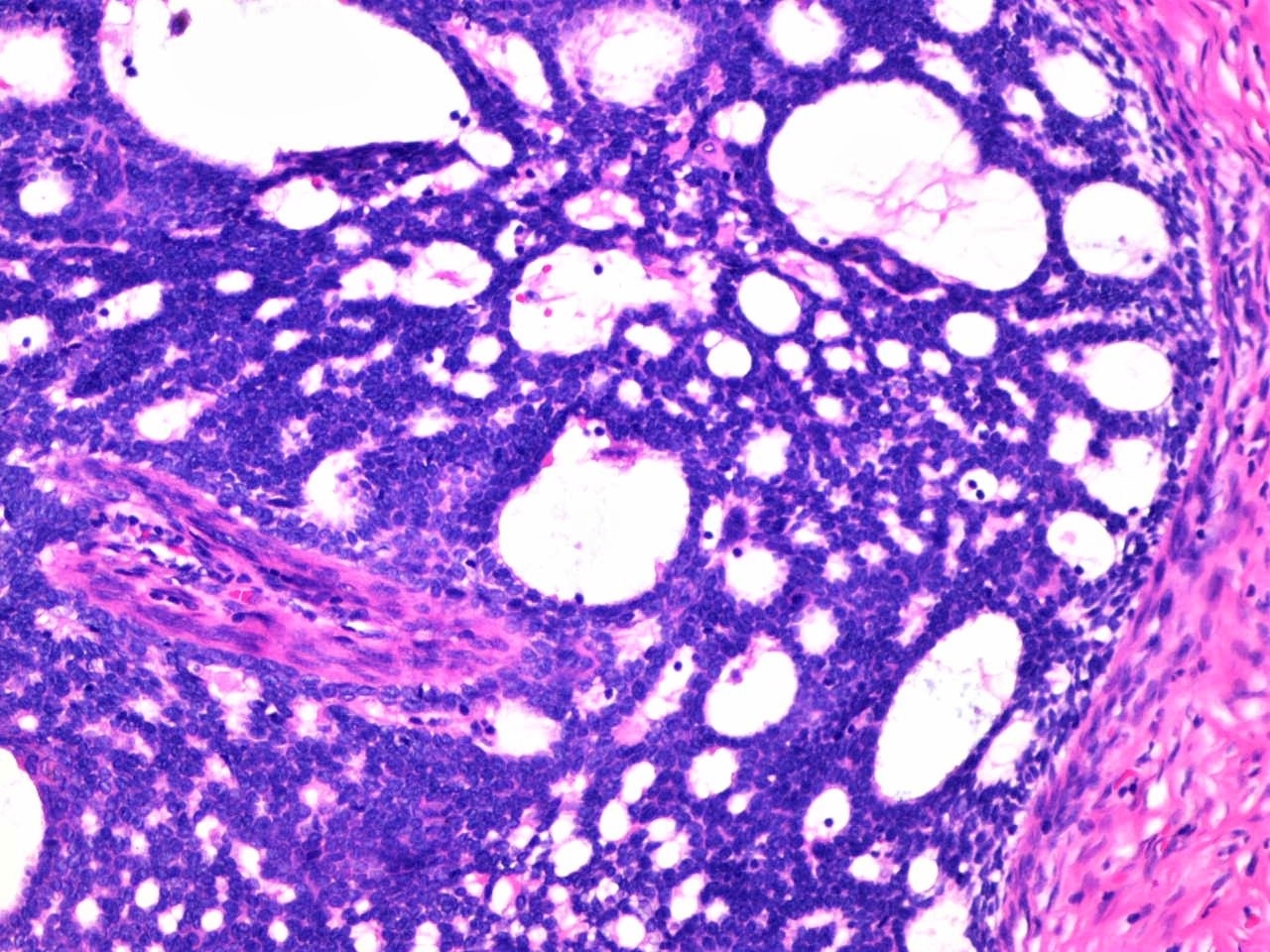
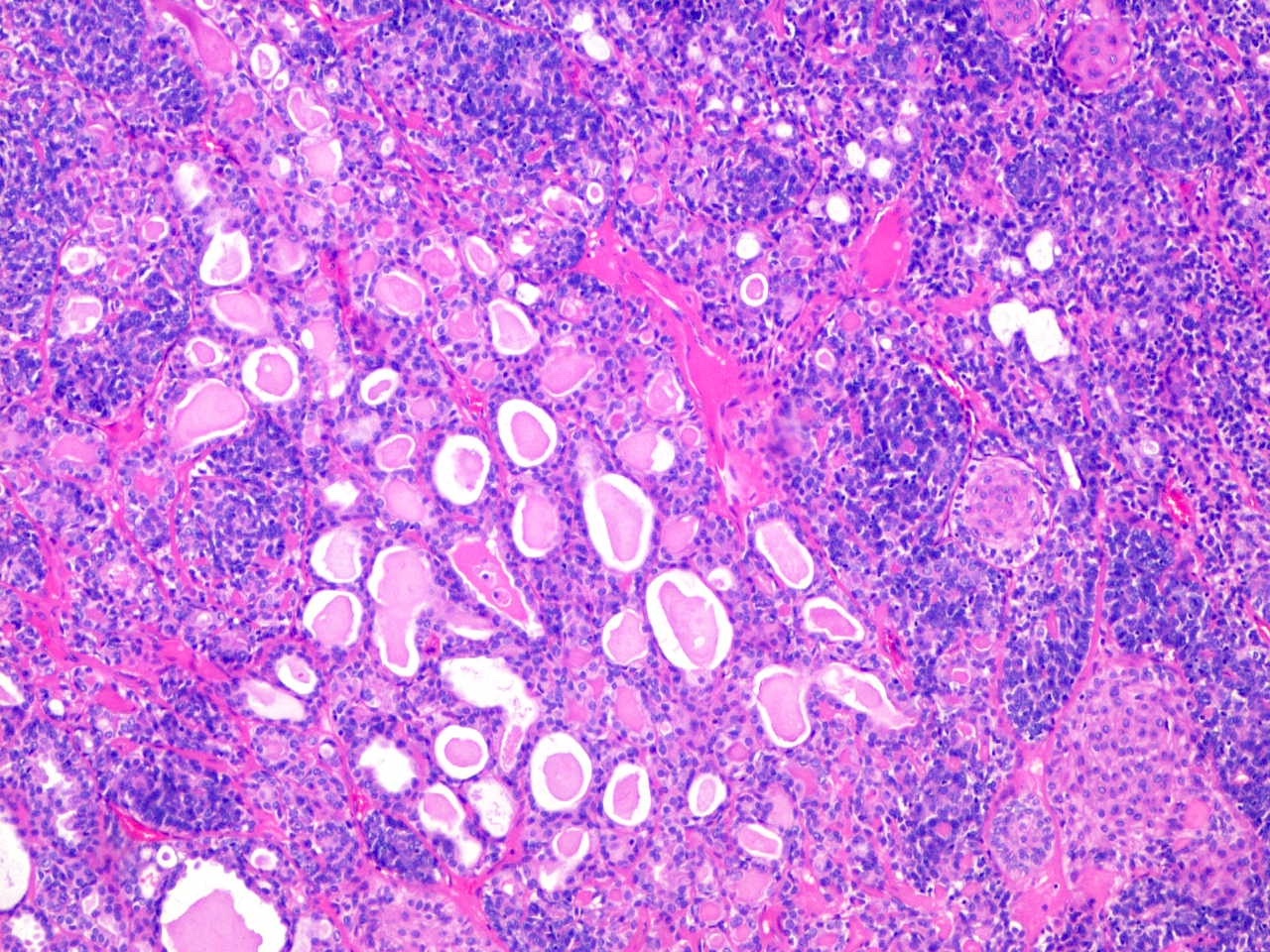
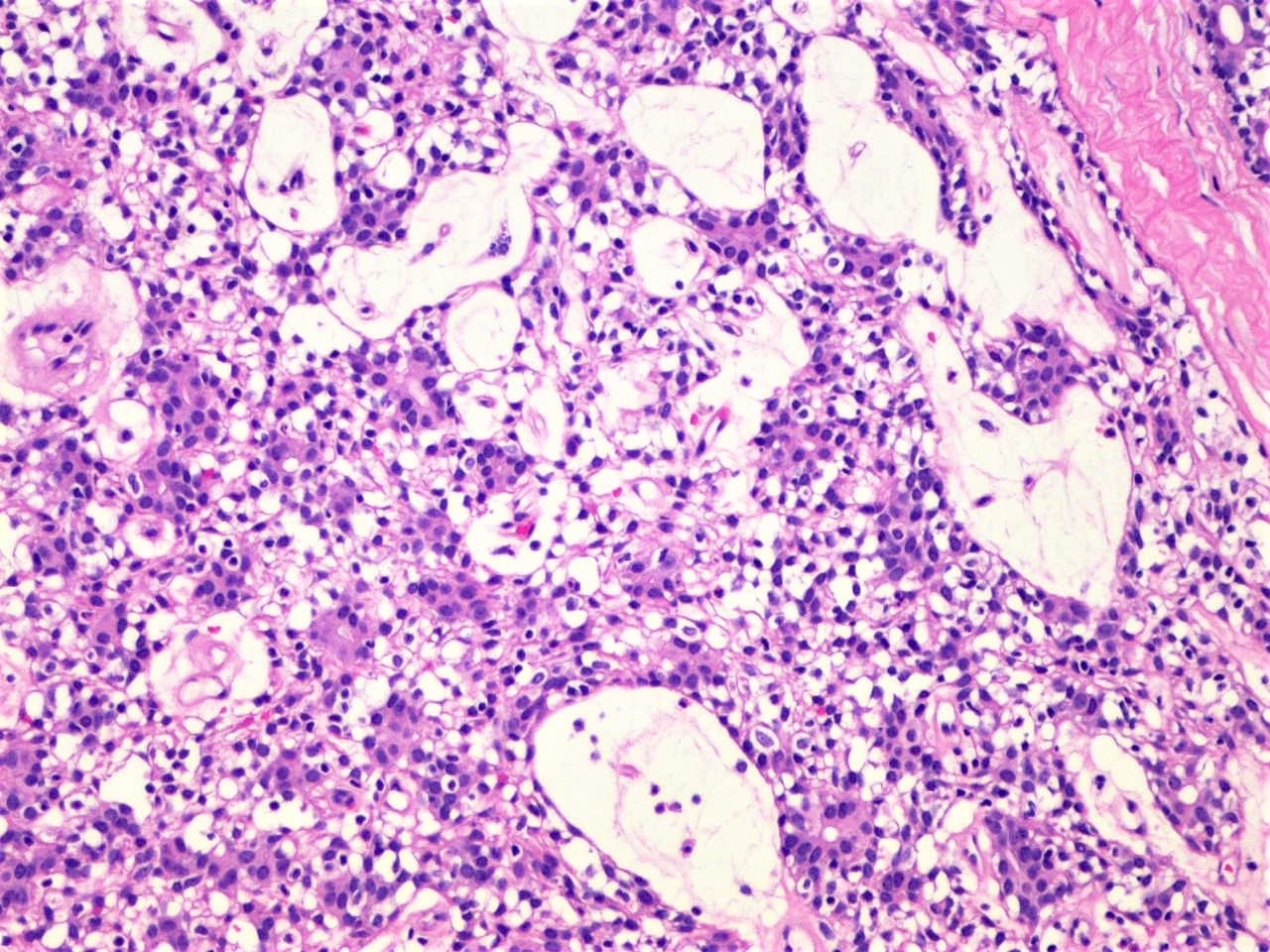
- Tubular / ductal structures (see Figure 4) and PAS positive basement membrane material (see Figure 5)
- Stroma between the nests of epithelial cells is often edematous with prominent vascularity (see Figure 6); may be hyalinized (see Figure 7)
- Vessels may be widely dilated (see Figure 7) / hemangiopericytoma-like
- Many T lymphocytes and Langerhans cells often scattered throughout lobules
- Mitoses extremely rare
- Morphologic variations:
- Architectural variations:
- Cystic changes (see Figure 8)
- Adenomatous (see Figure 9) (Am J Dermatopathol 2008;30:436)
- Adenomyoepitheliomatous component (see Figure 10) (Int J Surg Pathol 2020;28:427)
- Adenoid cystic-like pattern cylindromatous features (see Figure 11)
- Trichoepitheliomatous / trichoblastomatous differentiation
- Cytologic variations:
- Stromal variation: edematous, myxoid, lipomatous metaplasia, osseous metaplasia, myoid metaplasia
- Architectural variations:
Microscopic (histologic) images
Cytology description
- Rare case reports describing the fine needle aspiration (FNA) cytologic findings of spiradenoma
- Tight multilayered clusters of uniform benign cuboidal epithelial cells along with spindle shaped myoepithelial cells and occasional lymphocytes (J Lab Physicians 2014;6:130)
- Prominent basement membrane deposition with an irregular tubular and nesting growth pattern and bland basaloid cells (Acta Cytol 1990;34:275)
Positive stains
- Intraluminal material is PAS positive, diastase resistant
- Both cell populations (dark and pale) are positive for CK7, CK8 and CK18
- CEA and EMA highlight the ductal components
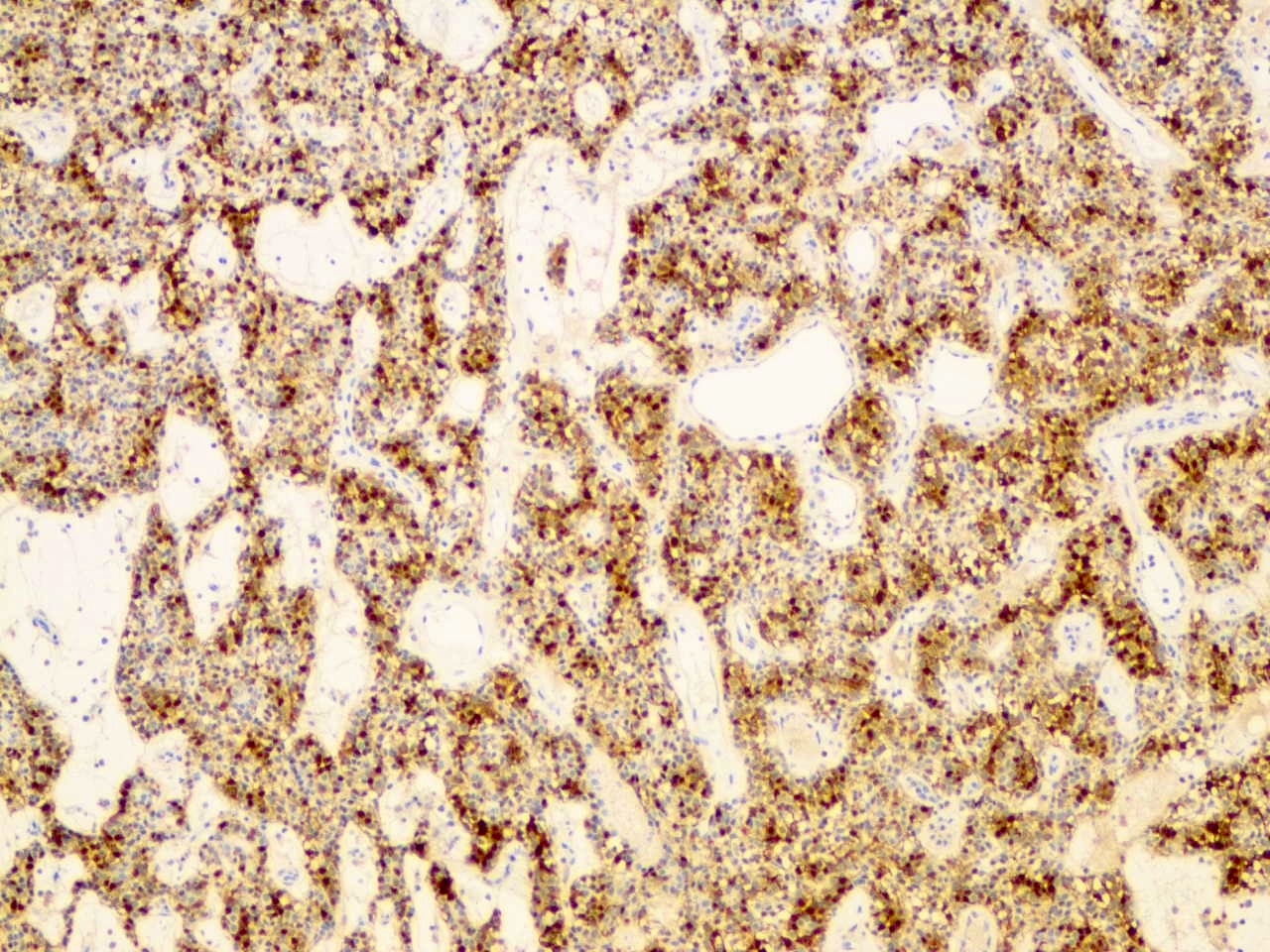
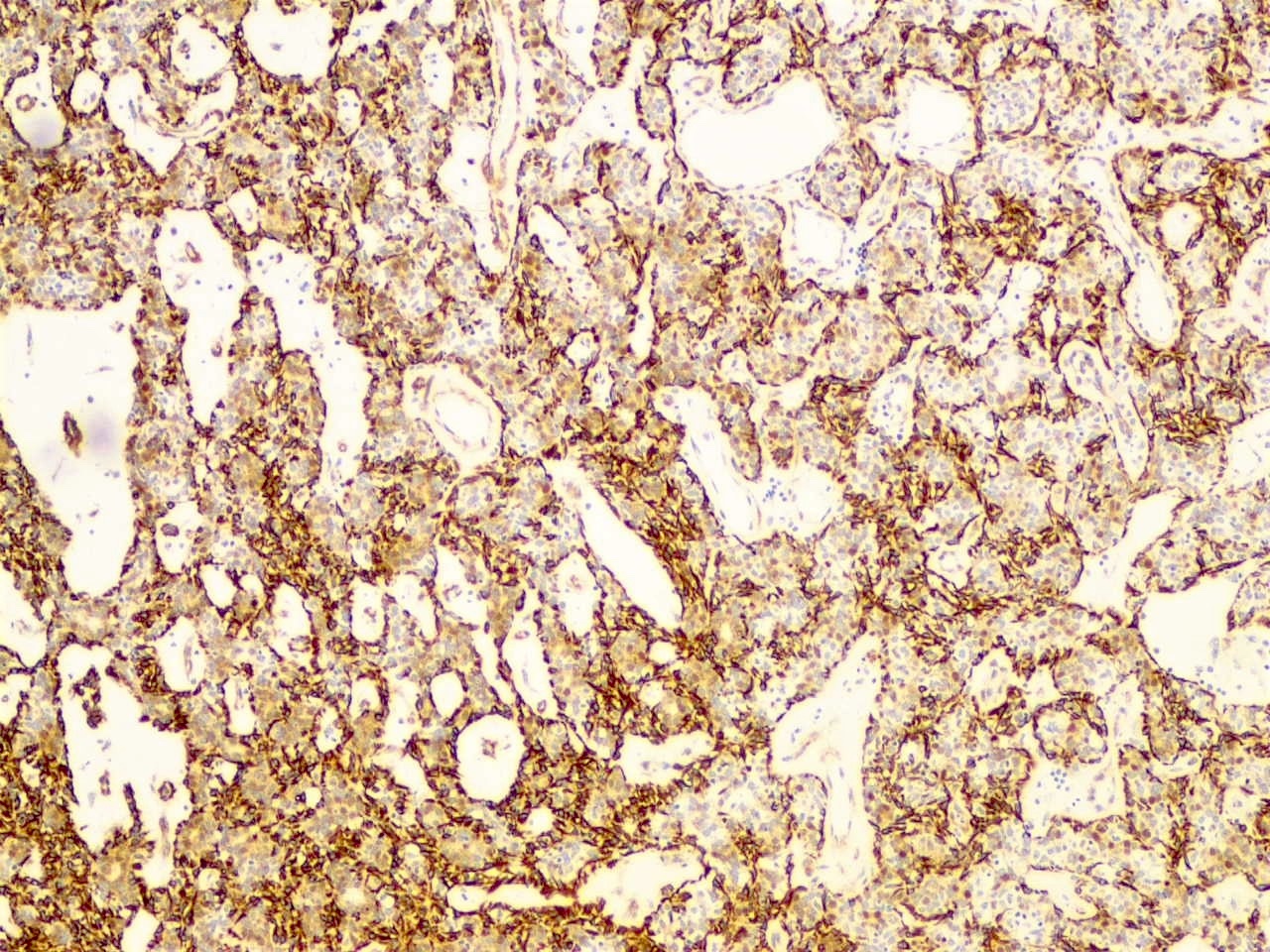
- S100 (see Figure 14) and SMA (see Figure 15) highlight myoepithelial cells
- Beta catenin positive (nuclear) (J Cutan Pathol 2011;38:657)
- Immunopositivity for IKH4 is supportive of eccrine differentiation over apocrine (J Cutan Pathol 1998;25:100)
Electron microscopy description
- Lobules separated by amorphous / fibrillar material
- Large pale cell has mitochondria, vesicles, glycogen in cytoplasm (J Invest Dermatol 1962;38:289)
Molecular / cytogenetics description
- Axin and GSK-3β (both induce degradation of beta catenin) downregulated (J Cutan Pathol 2011;38:657)
- Mutations in the tumor suppressor gene, CYLD (Nat Commun 2019;10:2213)
- Missense mutations in the alpha kinase domain of the ALPK1 gene (Nat Commun 2019;10:2213)
- p53 loss of function mutations described in rare cases of malignant transformation / spiradenocarcinoma (Nat Commun 2019;10:2213)
Videos
Spiradenoma: 5 minute pathology pearls
Spiradenoma and cylindroma: sweat gland tumor pathology
Spiradenoma for beginners
Sample pathology report
- Skin, left cheek, excision:
- Spiradenoma, completely excised with negative surgical margins
- Negative for malignancy
Differential diagnosis
- Cylindroma:
- Closely related tumor with morphologic overlap but generally more abundant eosinophilic material around clusters of dark cells with jigsaw pattern and usually lack of lymphocytes
- Poroma:
- Only basaloid cells, absence of the second pale cell population and intratumoral lymphocytes
- Spiradenocarcinoma / malignant spiradenoma / carcinoma ex spiradenoma:
- Infiltrative growth and nuclear atypia, arising from spiradenoma (both components identified)
Practice question #1
Practice answer #1
Practice question #2
Which of the following is true of spiradenoma?
- Composed of nests of a single cell type, forming dark nests in the dermis
- Even with complete excision, local recurrence is typical
- Intratumoral lymphocytes are a common component
- Usually centered in the epidermis
Practice answer #2
Practice question #3
Spiradenoma is an adnexal tumor which commonly occurs in what hereditary syndrome?
- Birt-Hogg-Dube syndrome
- Brooke-Spiegler syndrome
- Cowden syndrome
- Tuberous sclerosis
Practice answer #3