Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Bhatt M, Speiser J. Keloid. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocytickeloid.html. Accessed September 16th, 2025.
Definition / general
- Result of abnormal fibroblast activity in response to skin trauma or inflammation resulting in increased production of collagen and growth factors
- Nodule or mass forming scar that extends beyond the site of initial injury
Essential features
- Benign and potentially disfiguring fibrous tumor caused by increased fibroblast activity in response to skin trauma, causing increased collagen and growth factor production
- Common in individuals with darker skin and most common in African Americans (Cureus 2022;14:e23503)
- In comparison to hypertrophic scars, keloids extend beyond the site of initial injury
- Persist until treated, commonly by a combination of intralesional corticosteroids and surgical excision
- Recurrence is common despite treatment (Am Fam Physician 2009;80:253)
Terminology
- Keloid scar
ICD coding
Epidemiology
- Common in patients < 30 years of age (Am Fam Physician 2009;80:253)
- Commonly seen after ear piercings
- Most common in Black and darker pigmented individuals
- Positive family history increases risk of development
Sites
- Any site of trauma or injury to the skin can be affected
- Typically occurs in the head and neck region, including upper part of the back, deltoids and presternal areas
- Characteristically occurs on the earlobes from ear piercings
Pathophysiology
- Exact pathophysiology is unknown
- Commonly accepted to be due to a dysregulated fibroblastic phase of wound healing, in which fibroblasts have increased proliferative activity and decreased apoptosis resulting in increased collagen, extracellular matrix and cytokine production (J Clin Aesthet Dermatol 2020;13:33, StatPearls: Keloid [Accessed 31 May 2024])
- Primary drivers of keloid formation are considered to be transforming growth factor beta (TGFβ) and platelet derived growth factor (PDGF) (StatPearls: Keloid [Accessed 31 May 2024])
- TGFβ promotes chemotaxis of fibroblasts to the site of inflammation and produces collagen
- Abnormalities in this pathway lead to fibrosis and an abnormal scar response
Etiology
- Caused by genetic and environmental factors
- Can occur as a result of increased tension in a wound
- Occurs in susceptible individuals after any type of skin trauma including surgery, piercings, acne, tattooing, insect bites, burns, lacerations, abrasions, vaccinations and any other process resulting in cutaneous inflammation (StatPearls: Keloid [Accessed 31 May 2024])
Clinical features
- Occurs after trauma to the skin
- Keloids can take on various shapes depending on site of injury (Scars Burn Heal 2021;7:2059513120980320)
- Ranges in color from flesh colored to red or brown
- Initial presentation commonly includes erythema, pruritis or pain (Scars Burn Heal 2021;7:2059513120980320)
- Rubinstein-Taybi and Goeminne syndromes are rare genetic conditions that are associated with an increased risk of developing keloids (StatPearls: Keloid [Accessed 31 May 2024])
Diagnosis
- Diagnosis is made clinically but lesions may be biopsied for confirmation or excised for cosmetic purposes
Prognostic factors
- Benign but may cause symptoms including pain and pruritus
- Persists unless treated; most commonly removed for cosmetic reasons and if symptomatic
- Despite treatment, recurrence is common (Scars Burn Heal 2021;7:2059513120980320)
Case reports
- 20 year old woman with development of nodules on earlobes after ear piercing (Malays Fam Physician 2020;15:83)
- 23 year old man with posterior ear lobe mass (Am Fam Physician 2018;98:603)
- 24 year old woman with recurrence 8 years after keloid resection (Medicine (Baltimore) 2023;102:e33444)
- 57 year old man with scar formation several months after trauma (J Pharm Bioallied Sci 2021;13:S871)
Treatment
- Complete surgical excision
- In conjunction with complete surgical excision, intralesional corticosteroid injections imiquimod, bleomycin or radiotherapy can be used to decrease the risk of recurrence (Dermatol Ther 2022;35:e15425)
- Compression bandages, silicone dressings, cryotherapy, laser therapy and intralesional 5-fluorouracil are also treatment options
Clinical images
Gross description
- Nodular or raised and irregularly shaped dermal skin lesion (Scars Burn Heal 2021;7:2059513120980320)
- Varies in color, can be flesh colored to red or brown
- Smooth, firm and rubbery
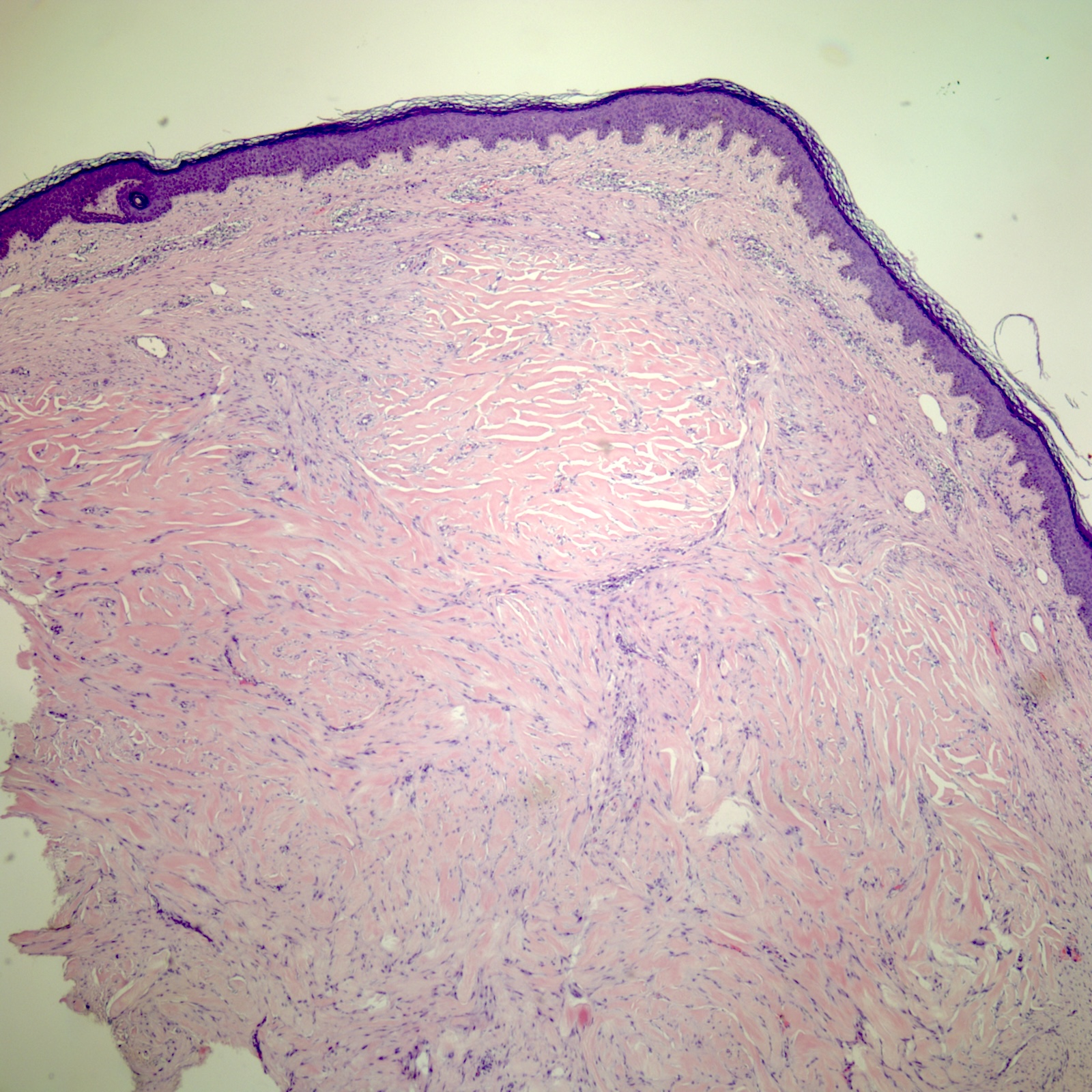
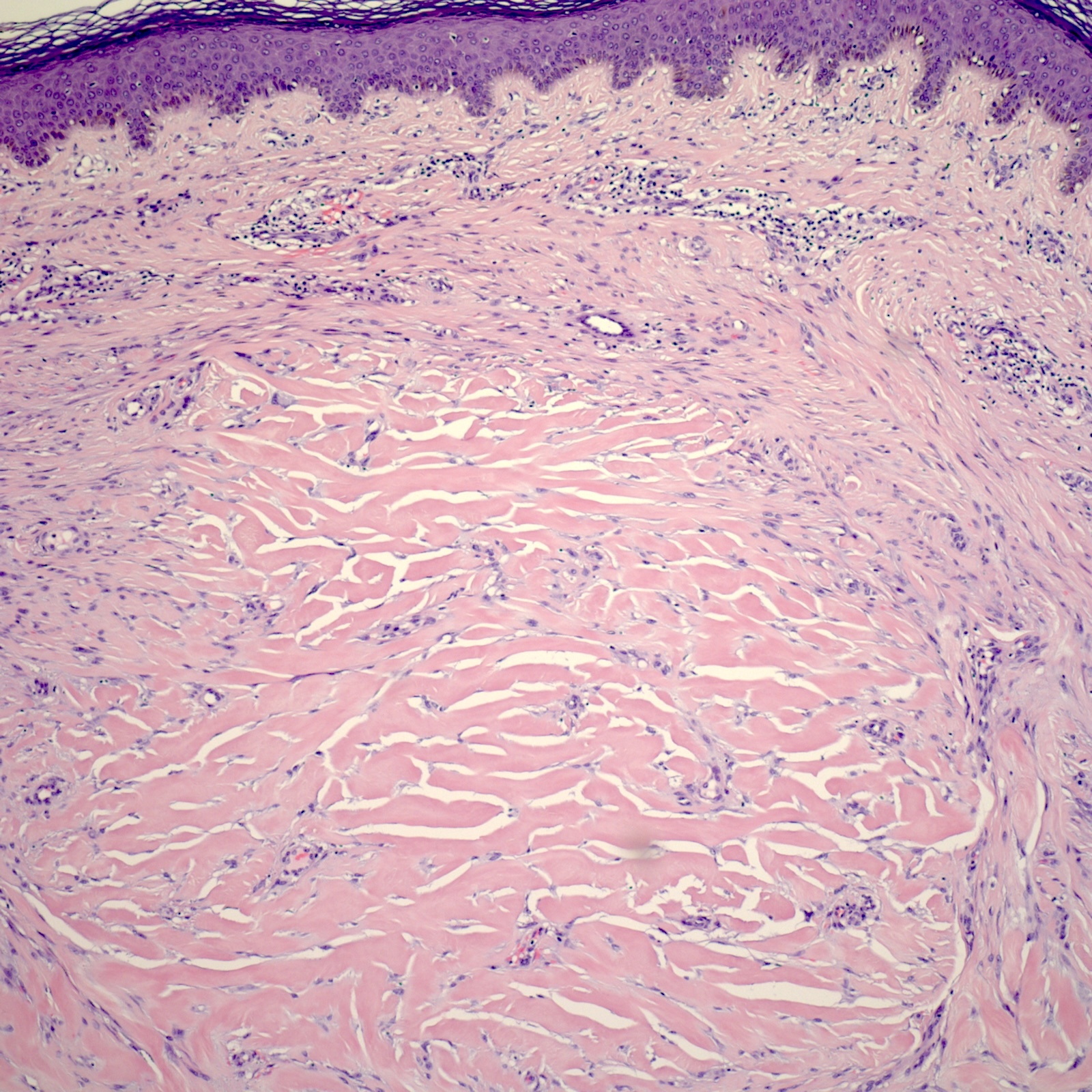
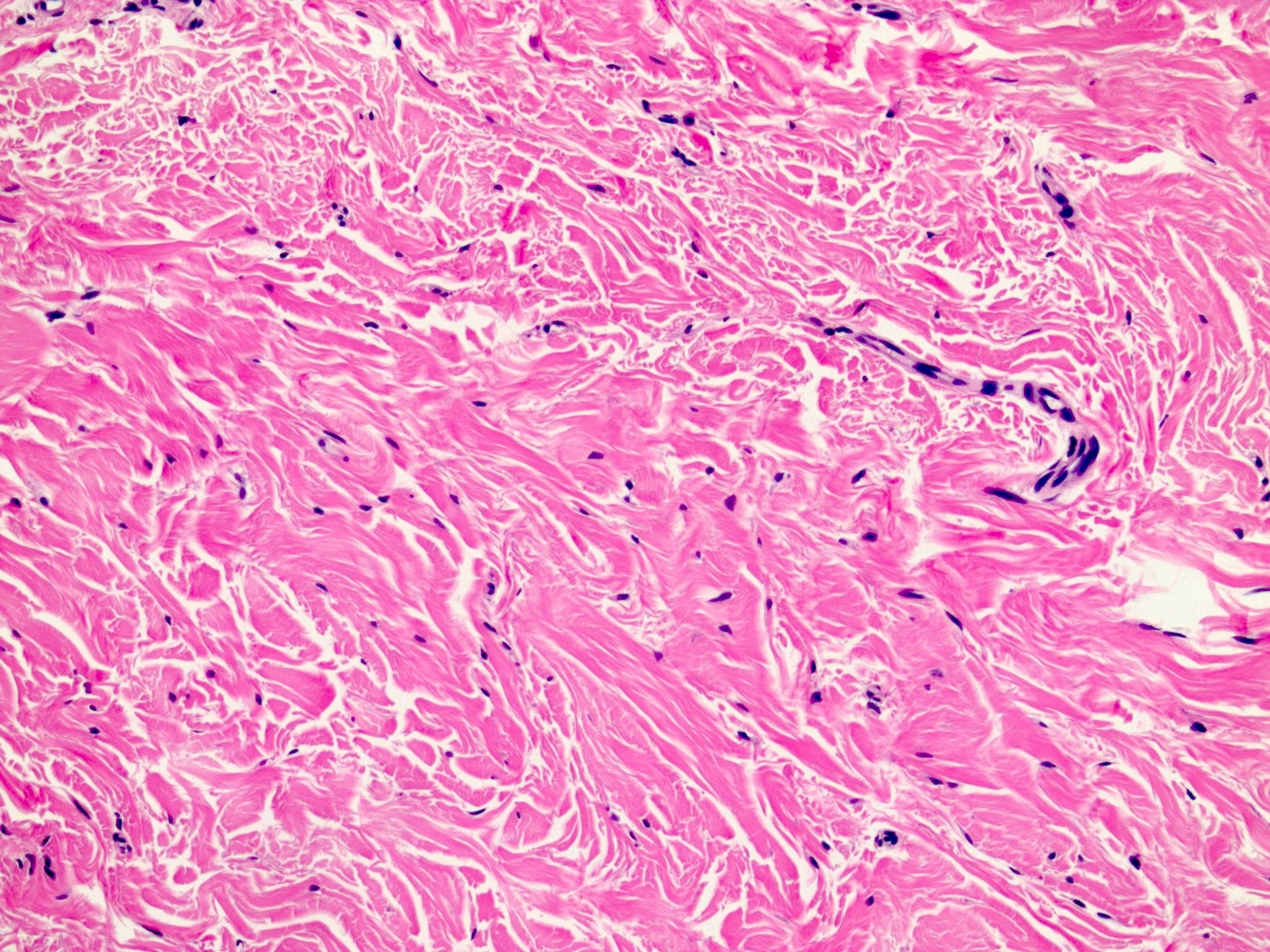
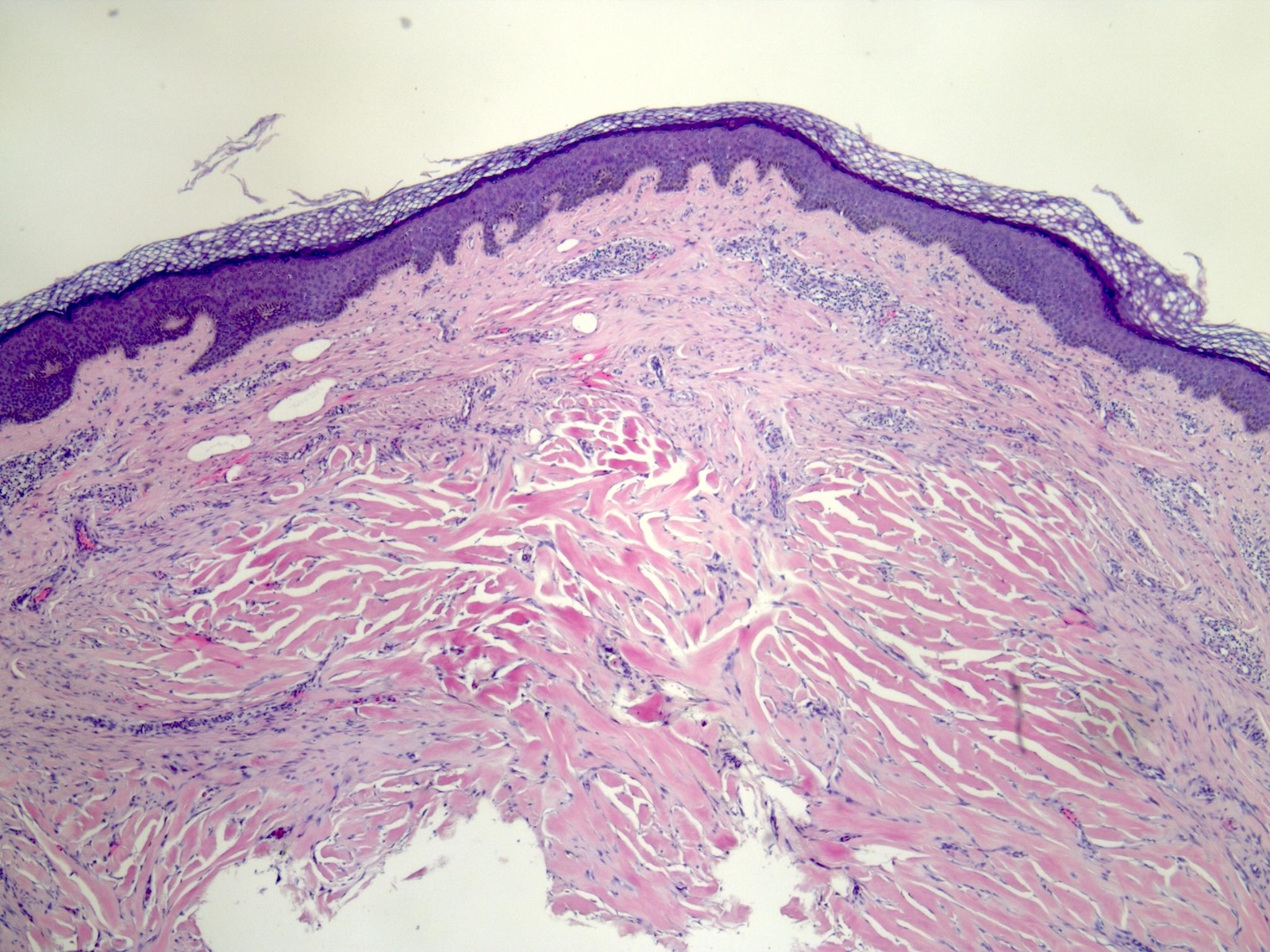
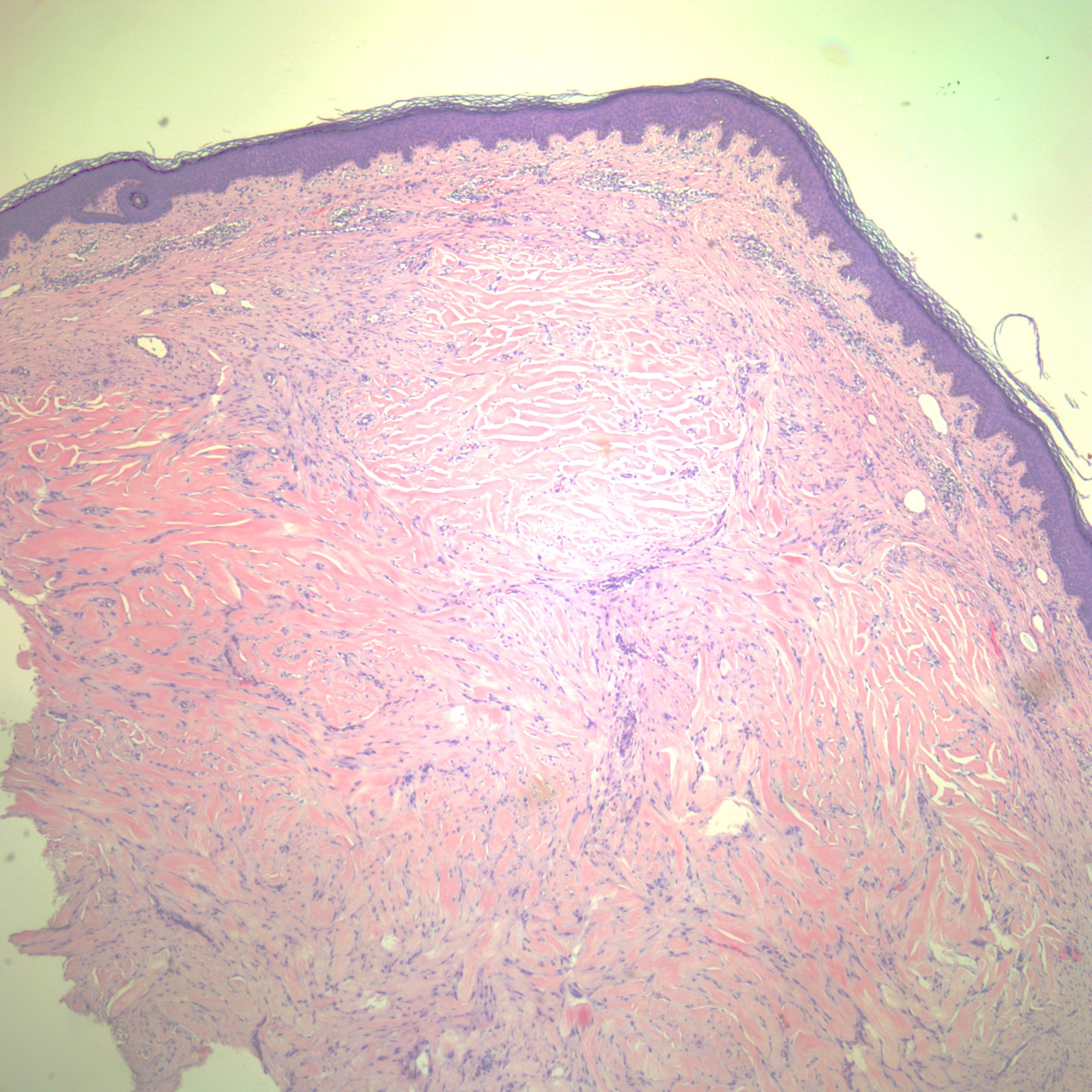
Microscopic (histologic) description
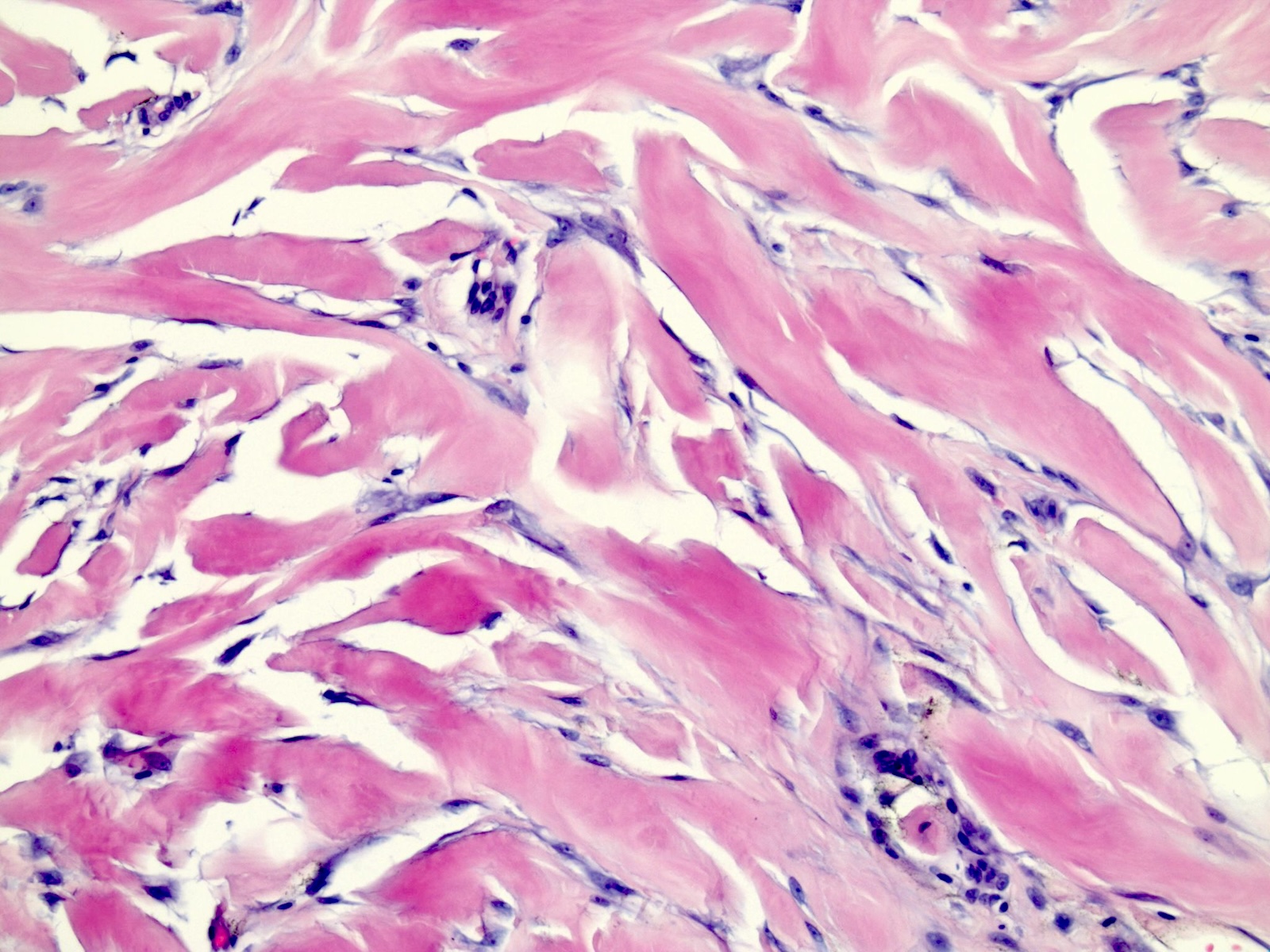
- Characteristic keloidal collagen is composed of broad, homogeneous, brightly eosinophilic bands of hyalinized collagen bundles
- Keloidal collagen is often described as bubble gum-like collagen
- Collagen bands are haphazardly arranged or form a nodular lesion in the reticular dermis sparing the papillary dermis (Am J Dermatopathol 2004;26:379)
- Focal aggregates of fibroblasts can be seen in between or around the collagen bands (Scars Burn Heal 2021;7:2059513120980320)
Microscopic (histologic) images
Videos
Dr. Gardner explains histological findings of keloids
Sample pathology report
- Skin, ear lobe, excision:
- Keloid
Differential diagnosis
- Hypertrophic scar:
- Does not grow outside of wound margins
- Can regress on its own
- Does not contain keloid type collagen bundles on histological exam (Weidner: Modern Surgical Pathology, 2nd Edition, 2009)
- Lacks hyalinized collagen fibers
- More delicate fibrillar collagen
- Dermatofibroma:
- Positive dimple sign on physical exam; lesion develops a central depression when lateral pressure is applied
- Coloration includes a central patch and surrounding delicate pigment network
- More common on the lower legs
- No history of preceding trauma
- Greater cellularity compared to keloid
- Positive dimple sign on physical exam; lesion develops a central depression when lateral pressure is applied
- Dermatofibrosarcoma protuberans:
- No history of trauma
- Harbors translocation t(17;22)(q22;q13) that results in a COL1A1::PDGFB fusion gene
- Most commonly found on the chest, shoulders and limbs
- Greater cellularity and more irregular borders, compared to keloid (StatPearls: Keloid [Accessed 31 May 2024])
- Rare and locally aggressive spindle cell tumor
- Keloidal variants (morphea and scleroderma); progression of disease, no history of trauma and may show signs of connective tissue disease
- Xanthoma disseminatum (StatPearls: Keloid [Accessed 31 May 2024]):
- Rare, histiocytic proliferation showing lesions that resemble keloid
- Lesions show a diffuse symmetric pattern
- May result in development of diabetes insipidus
- Lobomycosis:
Additional references
Practice question #1
Practice answer #1
D. Keloid. The image above shows a nodular bundle of keloidal collagen within the reticular dermis. The collagen bundles are thick eosinophilic bands arranged in a nodular or haphazard pattern, a characteristic finding in keloids. Also, the ear is the most common site for keloid formation. Answer C is incorrect because hypertrophic scars would have fewer thick collagen fibers. Answer A is incorrect because dermatofibromas are more common on the lower extremities and would show greater cellularity. Answer B is incorrect because dermatofibrosarcoma protuberans are most commonly found on the chest, shoulders and limbs and would demonstrate greater cellularity and irregular borders.
Comment Here
Reference: Keloid
Comment Here
Reference: Keloid
Practice question #2
Which of the following commonly occurs after excision of a keloid?
- Complete resolution
- Increase in propensity for development of squamous cell carcinoma
- Melanoma in situ
- Recurrence
Practice answer #2
D. Recurrence. Keloids are a benign entity that are known to have the potential to recur after surgical excision. Therefore, intralesional steroids or radiotherapy in conjunction with surgical management is usually the treatment of choice to prevent recurrence. Answers B and C are incorrect because keloids are not known to have malignant transformation or an increased propensity for cancer. Answer A is incorrect because recurrence is common despite treatment.
Comment Here
Reference: Keloid
Comment Here
Reference: Keloid
Practice question #3
Which of the following is a key difference between keloids and hypertrophic scars?
- Keloids grow beyond the wound site
- Keloids have an increased propensity for malignant transformation
- Keloids never recur after treatment
- Keloids occur exclusively in pigmented skin
Practice answer #3
A. Keloids grow beyond the wound site. On gross examination, keloids grow beyond the site of initial injury, while hypertrophic scars remain confined to the wound margins. Answer D is incorrect because keloids can occur in all skin types although individuals with darker pigmented skin are more prone to keloid formation after skin trauma. Answer C is incorrect because keloids can recur after treatment. Answer B is incorrect because keloids are benign skin lesions and do not have a propensity for malignant transformation.
Comment Here
Reference: Keloid
Comment Here
Reference: Keloid