Table of Contents
Definition / general | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Prognostic factors | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Battle L. Sebaceoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticsebaceoma.html. Accessed April 20th, 2024.
Definition / general
- Benign sebaceous neoplasm composed of basaloid cells and mature sebocytes
- Associated with Muir-Torre syndrome (MTS) but can also be an isolated (sporadic) tumor
Terminology
- Sebaceoma, as a term, is used for tumors with > 50% basaloid cells and sebaceous adenoma is used for tumors with < 50% basaloid cells
- Sebaceous epithelioma, as a term, is confusing and is best not used
- Sebaceous epithelioma could refer to a low grade form of sebaceous carcinoma, a basal cell carcinoma with sebaceous differentiation or sebaceous proliferations of uncertain potential and thus is not a useful term
ICD coding
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
Epidemiology
- F:M = 4:1
- Wide age range but the majority of patients are in the sixth to ninth decades
Sites
- Primarily occurs on the face and scalp
- Occurrence on non head and neck regions should prompt consideration of Muir-Torre syndrome
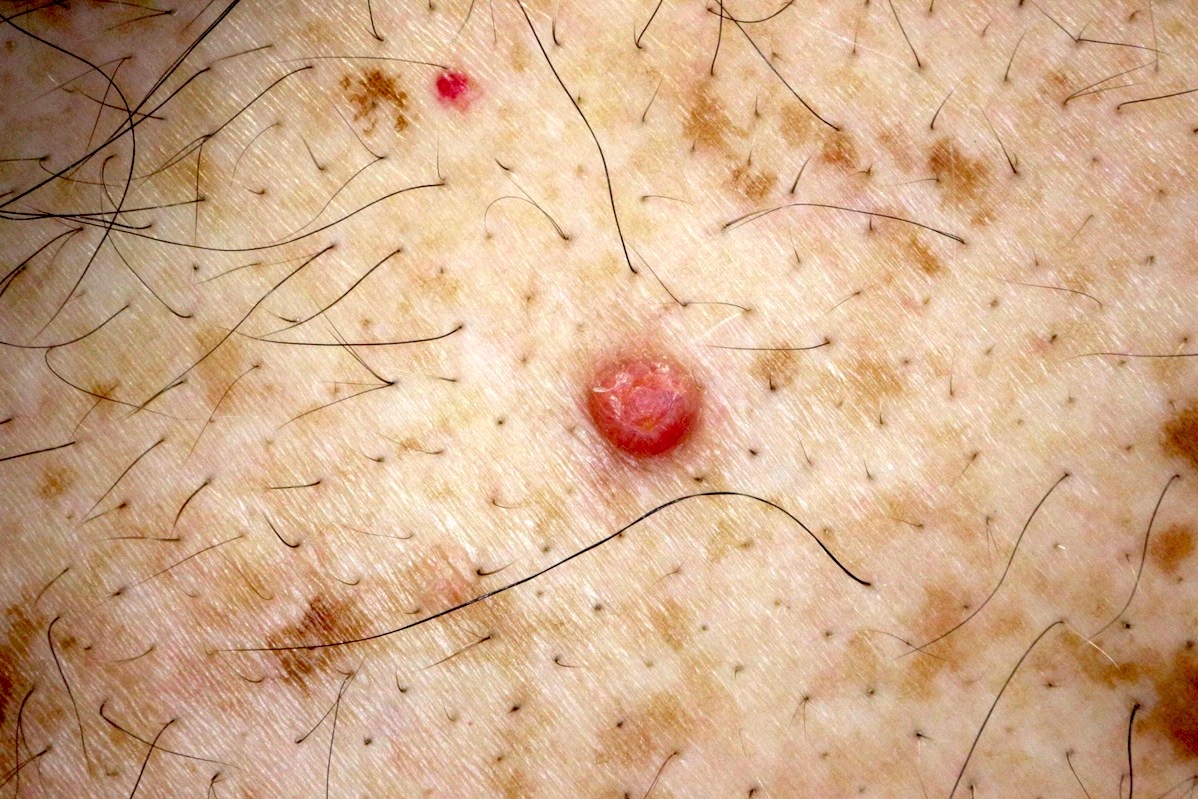
Clinical features
- Yellow to orange or flesh colored papule, nodule or tumor
- Muir-Torre syndrome (MTS) is considered a phenotypic variant of hereditary nonpolyposis colorectal carcinoma syndrome (HNPCC, Lynch syndrome) and is caused by germline mutations in one allele of the DNA mismatch repair (MMR) genes, most commonly MLH1, MSH2, MSH6 and PMS2
- MTS is associated with sebaceous neoplasia (most commonly sebaceous adenoma), colorectal, GU and other visceral adenocarcinomas
- MSH2 is the gene most commonly mutated in MTS
- If there is concern for MTS (personal or family history of colorectal, GU or breast cancer; or an older patient with numerous sebaceous neoplasms, especially not on the head and neck), further testing for MMR IHC or microsatellite instability can be performed
- IHC cannot differentiate between loss of MLH1 expression caused by a germline mutation versus a somatic hypermethylation - some germline missense mutations may be erroneously interpreted as normal by IHC, because they may result in an antigenically intact but nonfunctional protein
- Microsatellite instability analysis (MSI): performed on formalin fixed tissue, is more sensitive at detecting patients with germline MMR defects than IHC
- Results are either MSI-H (high degree of MSI) or MSI-L (low degree of MSI)
- Germline mutation analysis: blood leukocyte genomic sequencing is preferred to identify germline mutations in the MLH1, MSH2, MSH6 and PMS2 genes - if there are no germline mutations, but the tumor shows MMR deficiency, there may be involvement of other MMR proteins, somatic mutations or hypermethylation of the promoter region
Prognostic factors
- Sebaceomas can be sporadic, not associated with MTS
- Loss of nuclear staining for MLH1, MSH2, MSH6 or PMS2 suggests microsatellite instability (MSI) and supports a diagnosis of Muir-Torre syndrome
- Mutations in MLH1 and MSH2 have the most severe effect, producing a high frequency MSI phenotype
- When MSH2 is deficient, MSH6 usually is as well, because protein products of MSH2 and MSH6 form a heterodimer MMR recognition factor
- MSH6 is unstable without MSH2 and is quickly degraded
Treatment
- Once the diagnosis is established, no further treatment is needed
- However, complete excision should be considered if the tumor is only partially biopsied or there is concern for basal cell carcinoma with sebaceous differentiation or sebaceous carcinoma
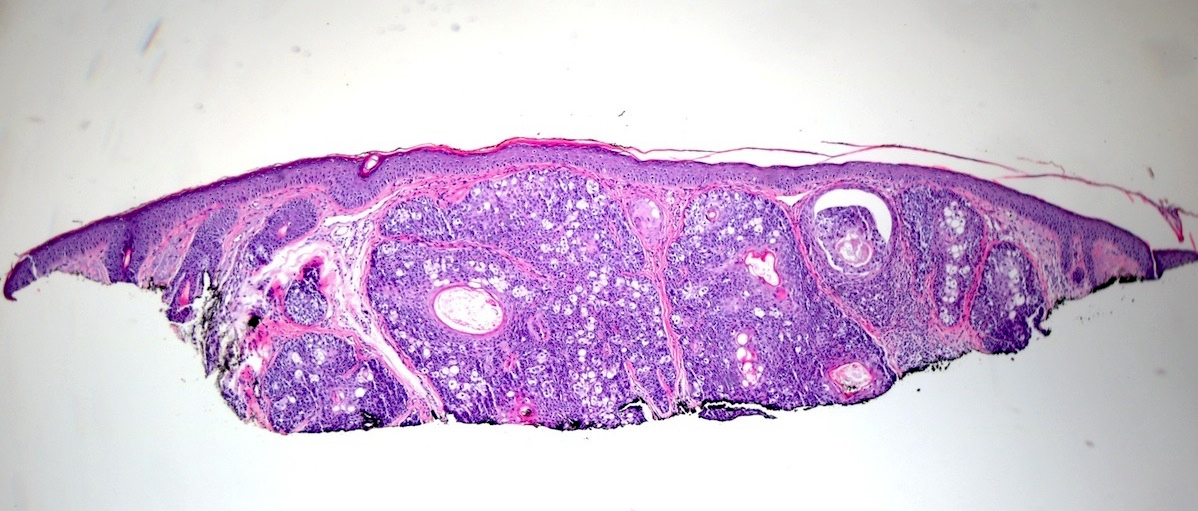
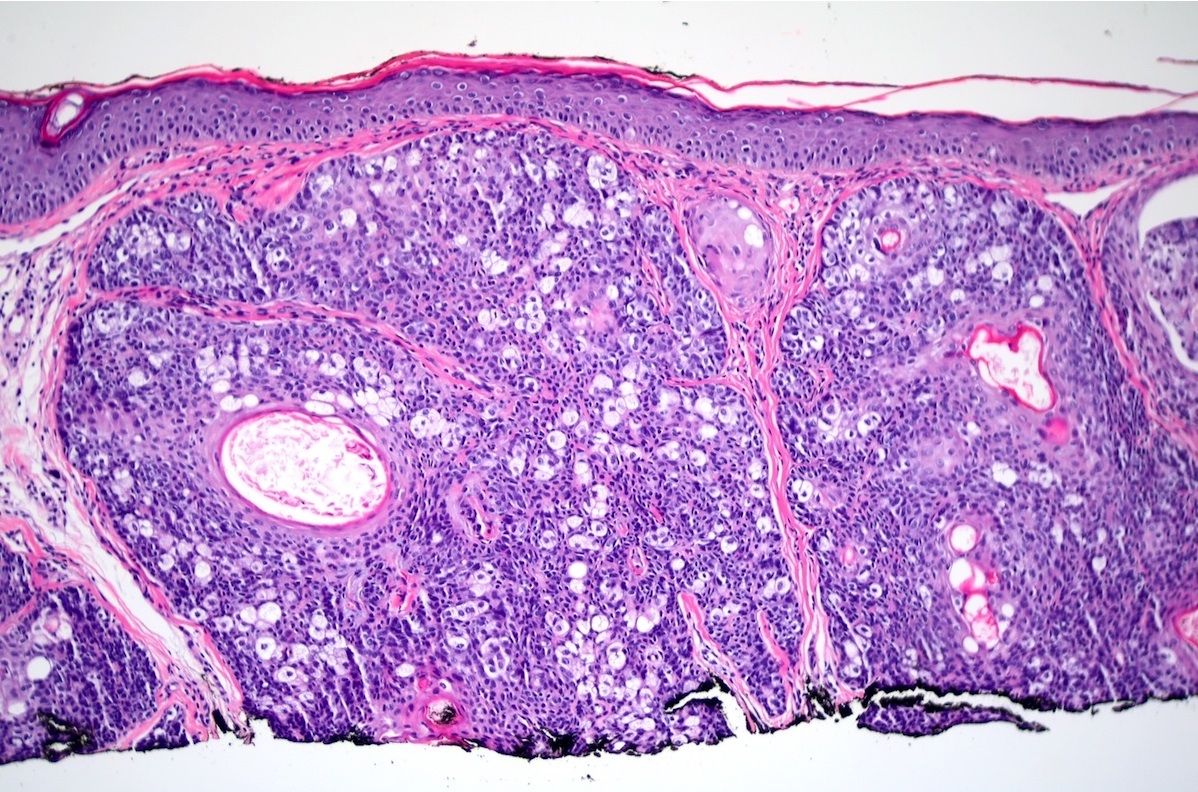
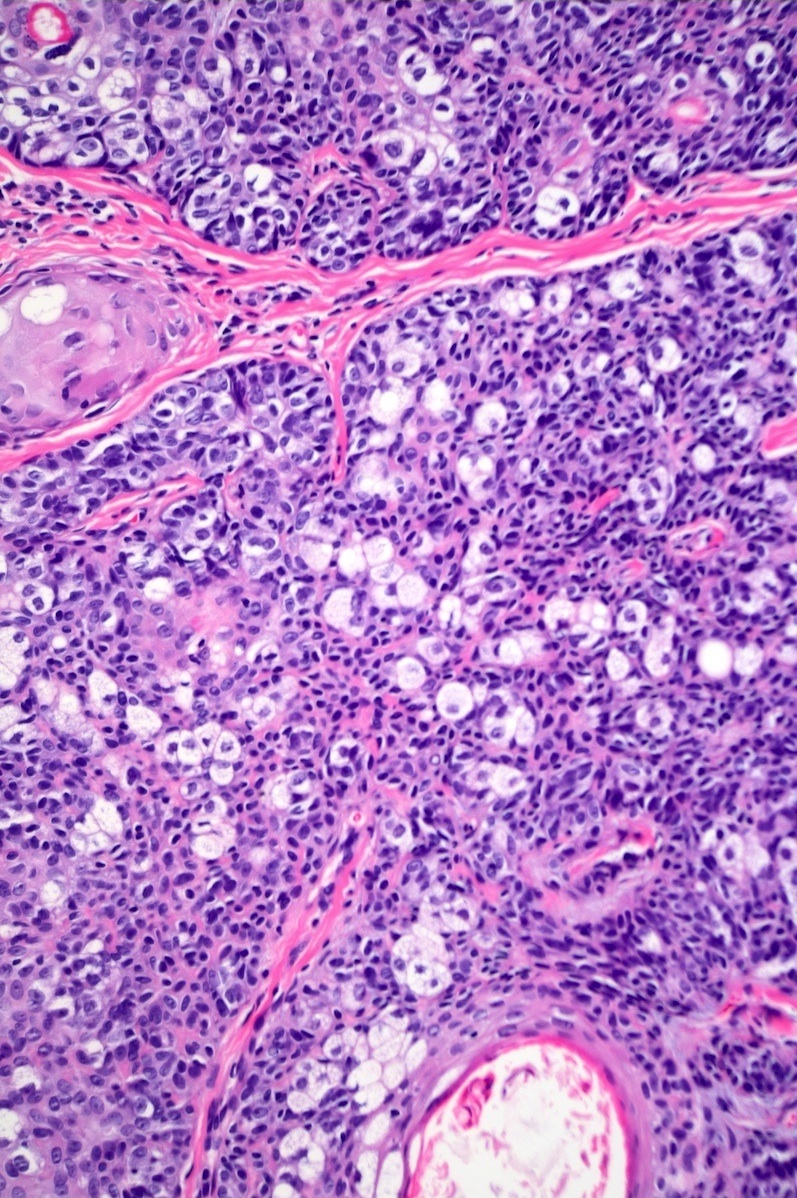
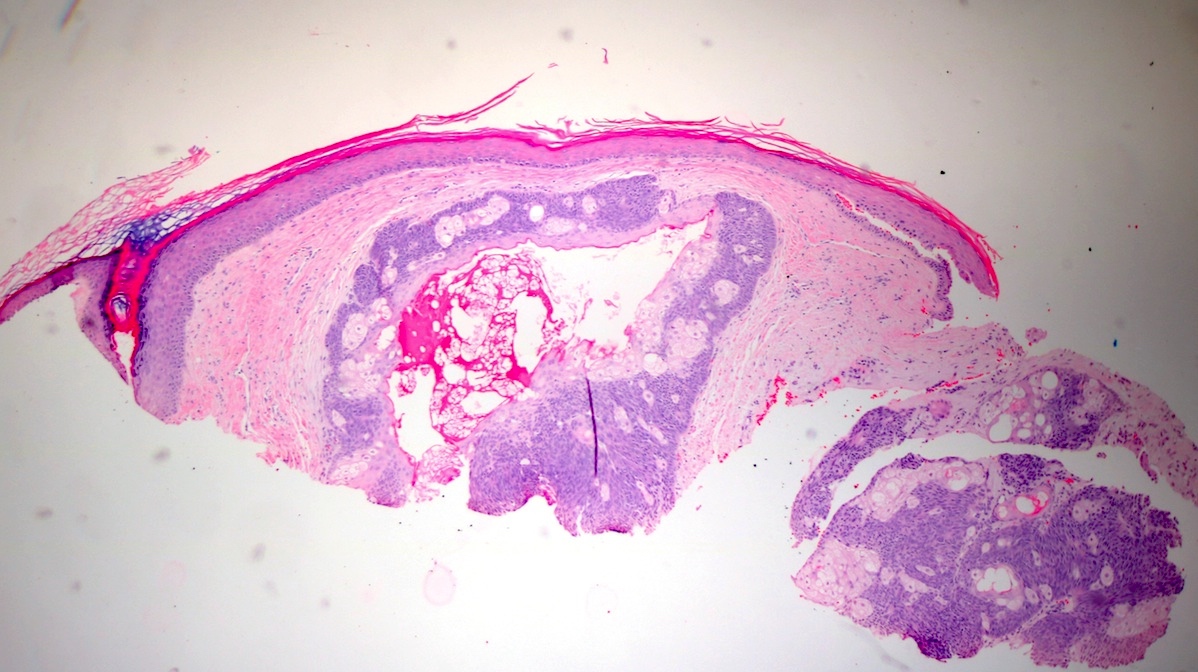
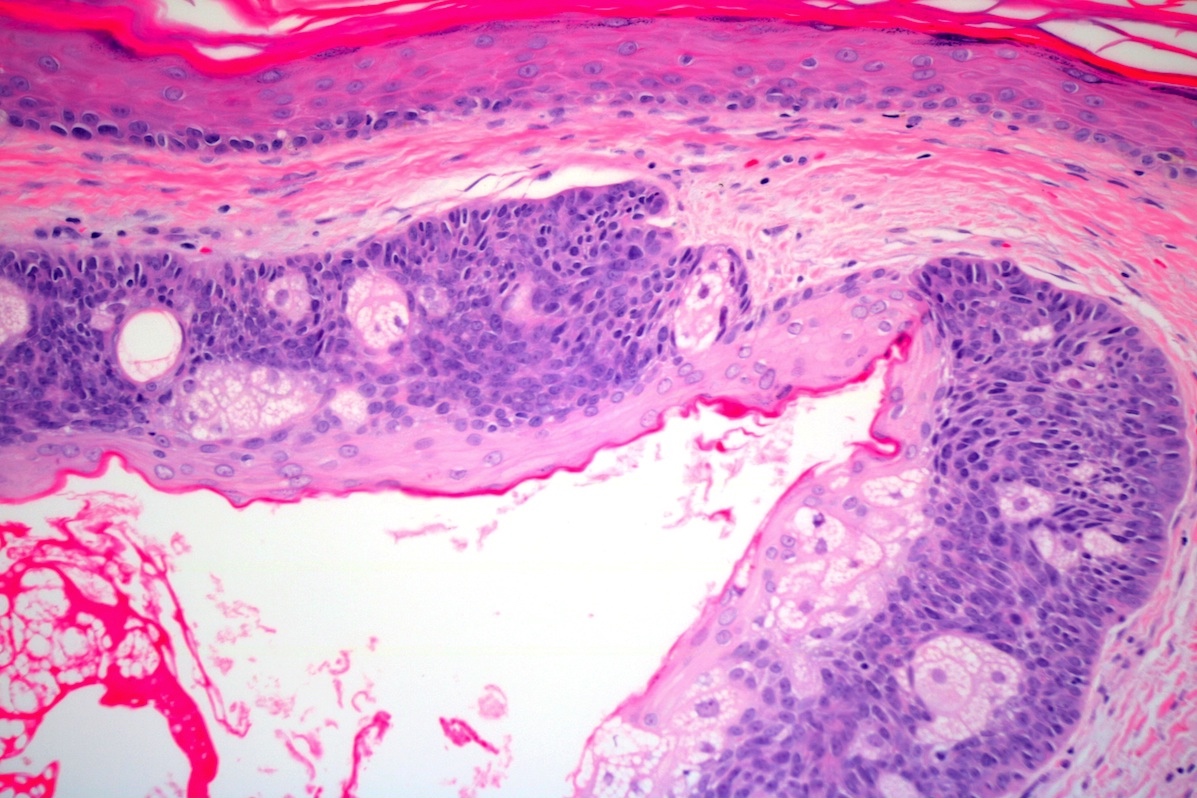
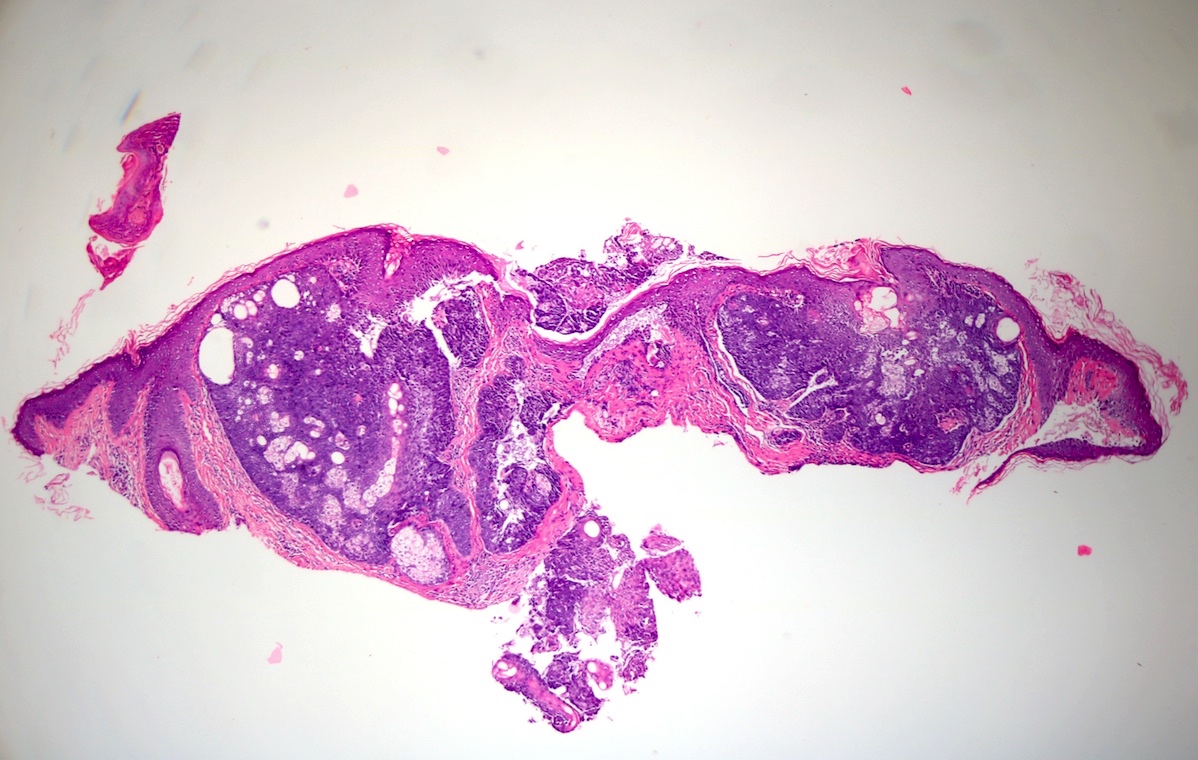
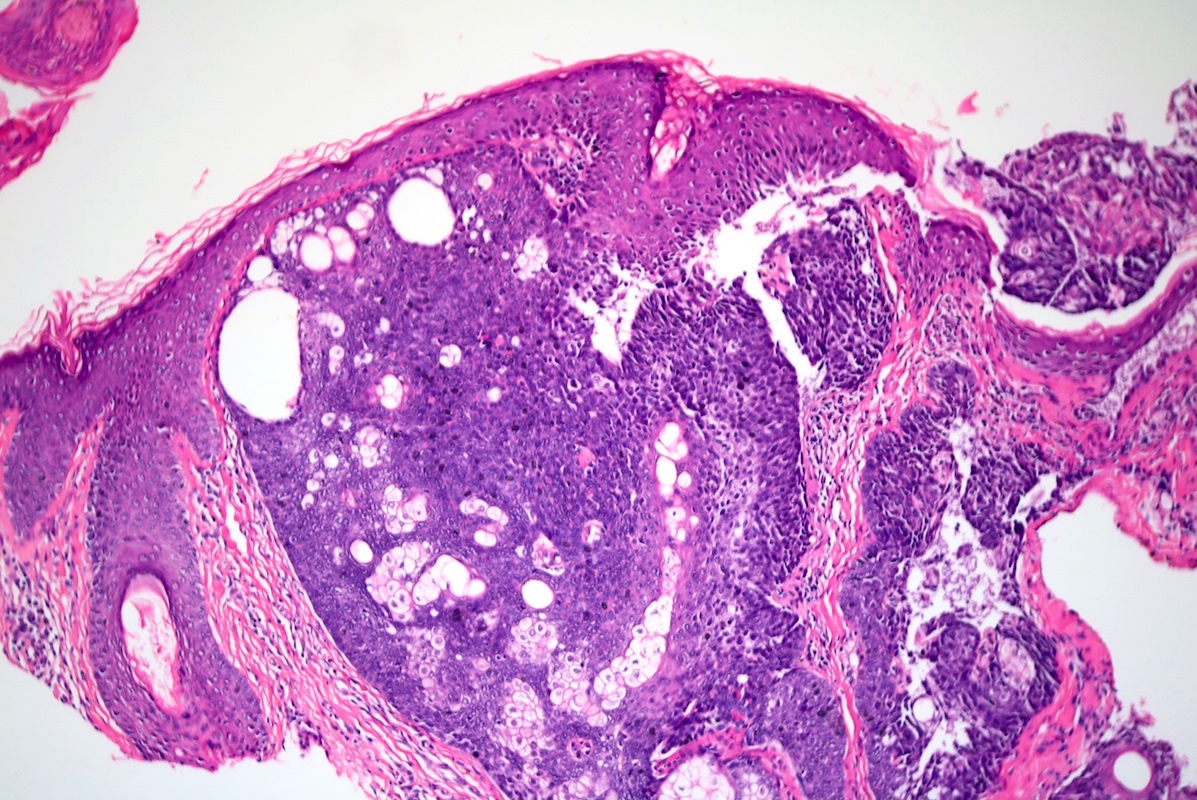
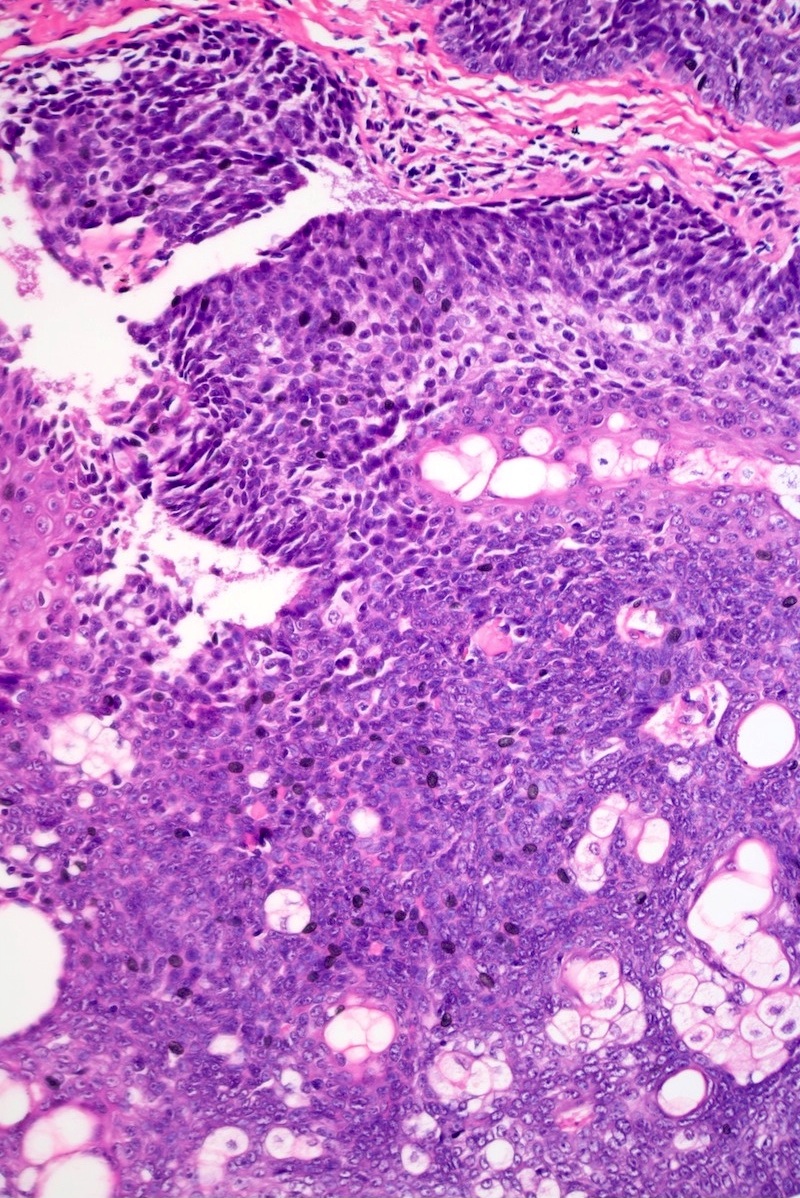
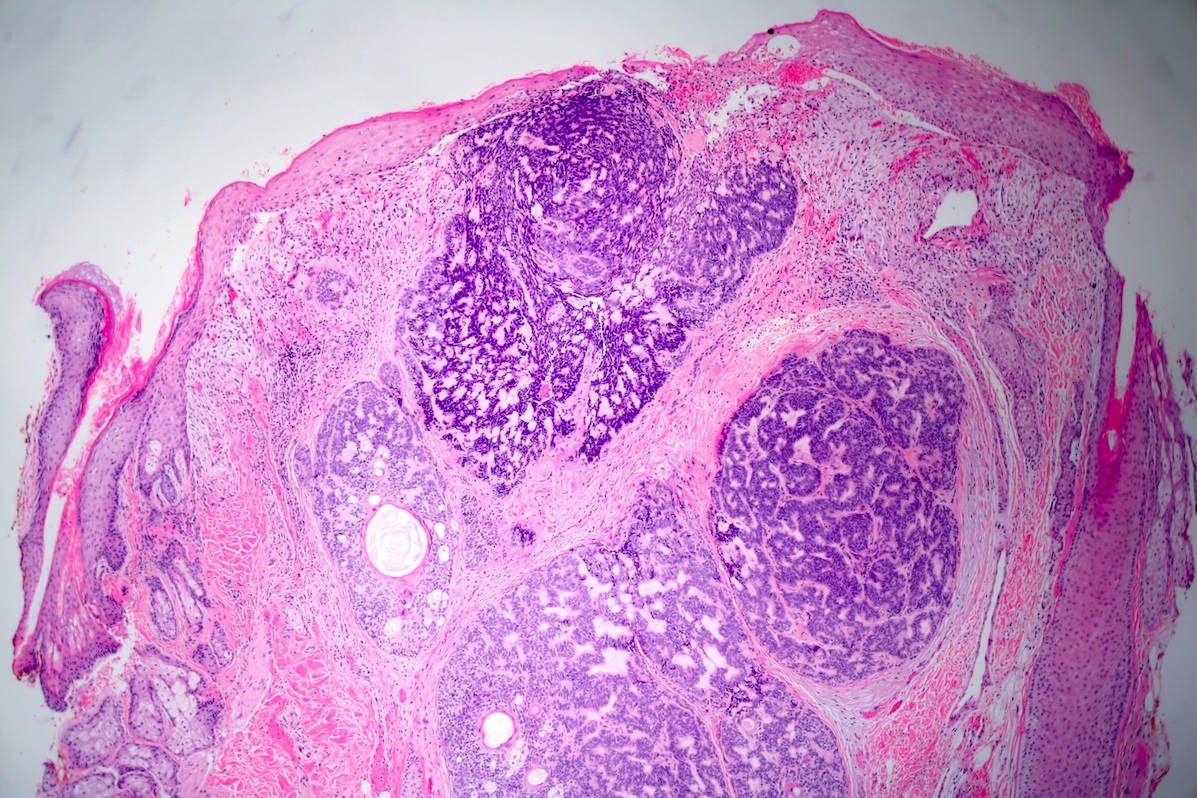
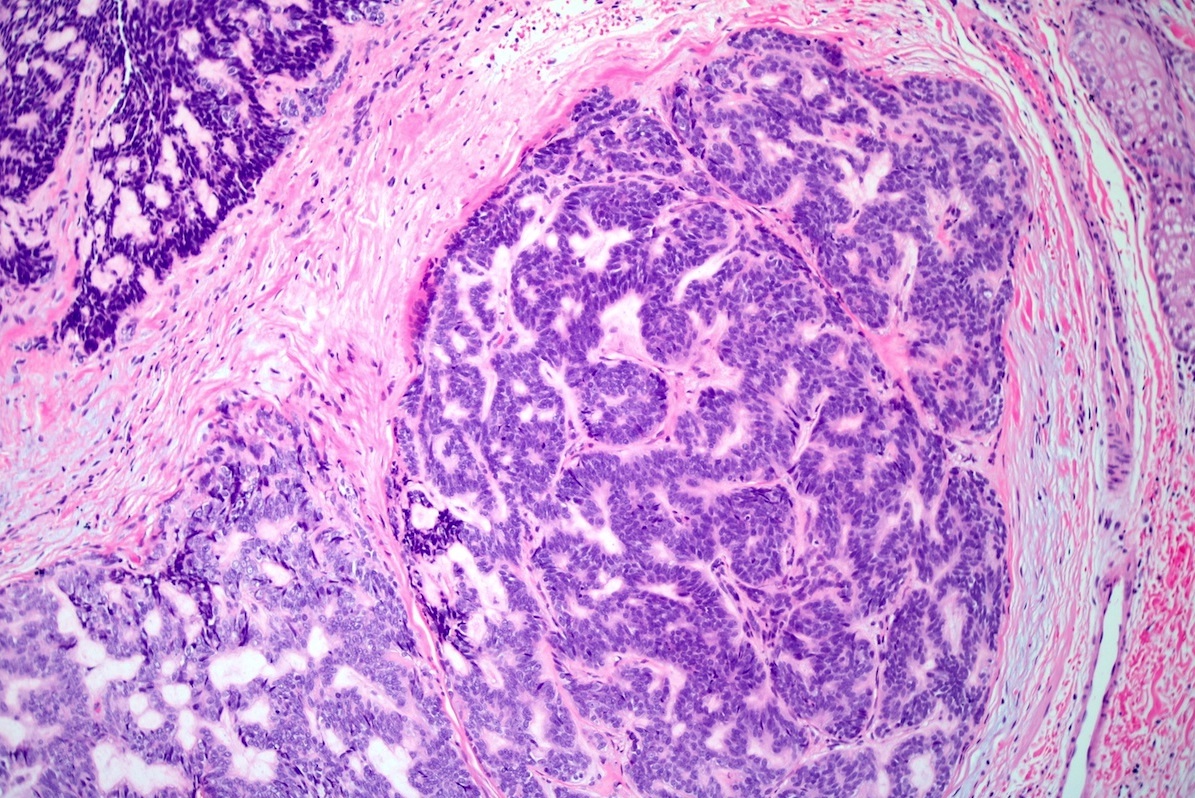
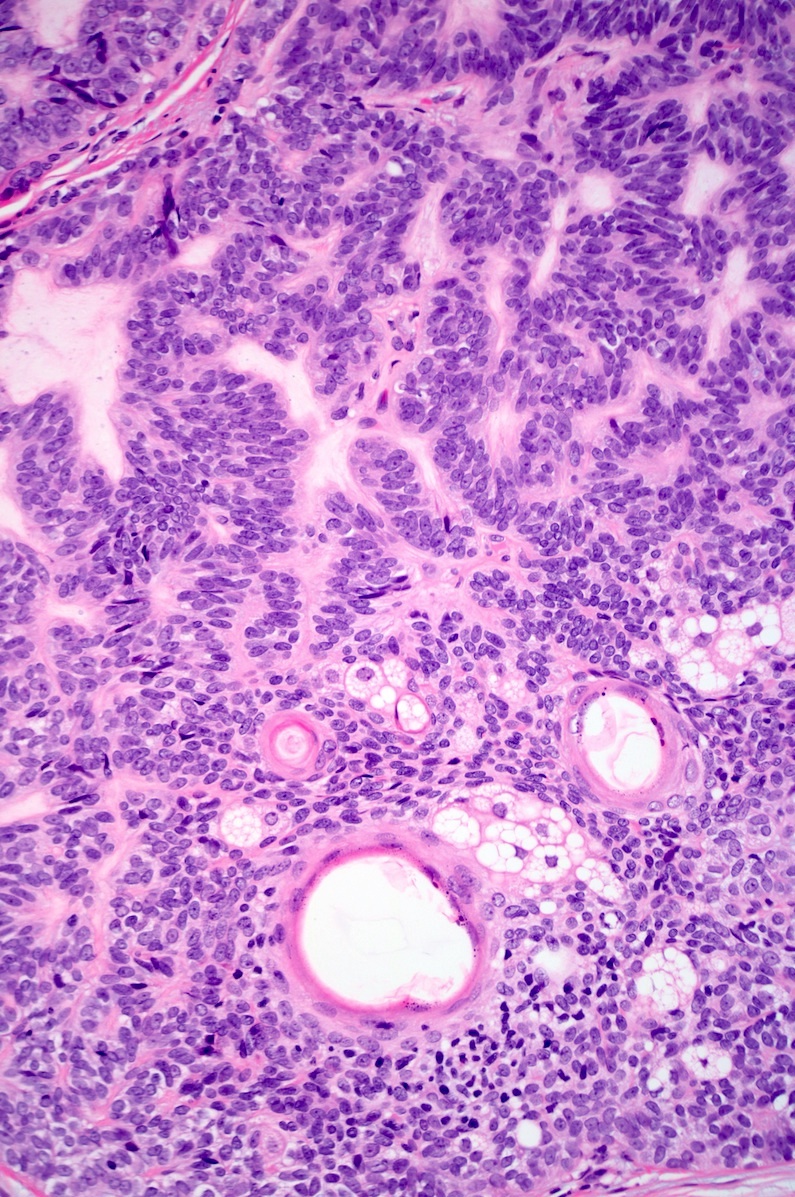
Microscopic (histologic) description
- Dermal nodule with variable epidermal involvement consisting of basaloid cells and mature sebocytes
- Greater than 50% of the tumor is made up of basaloid cells
- Variants of sebaceoma have been described with carcinoid-like, reticulated, cribriform, rippled and Verocay body-like features
Microscopic (histologic) images
Positive stains
- EMA, D2-40, Factor XIIIa (clone AC-1A1) nuclear
Videos
Muir-Torre Syndrome
Differential diagnosis
- Basal cell carcinoma with sebaceous differentiation:
- Predominantly shows peripheral palisading and cleft formation with incidental sebaceous differentiation
- BerEP4 staining is positive in basal cell carcinoma and negative in sebaceoma
- Sebaceous adenoma:
- Tumor with < 50% basaloid cells, as opposed to a sebaceoma which has > 50% basaloid cells
- Sebaceous carcinoma:
- Has more nuclear pleomorphism, nucleolar prominence and mitotic activity than sebaceoma, infiltrative growth pattern
- Trichoblastoma with sebaceous differentiation:
- Look for focal hair differentiation and papillary mesenchymal bodies
Additional references
Board review style question #1
- What is the most common skin tumor associated with Muir-Torre syndrome?
- Basal cell carcinoma
- Sebaceoma
- Sebaceous adenoma
- Sebaceous carcinoma
Board review style answer #1
Board review style question #2
- What is the most common mutation seen in Muir-Torre syndrome?
- MLH1
- MSH2
- MSH6
- PMS2
Board review style answer #2