Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Yakoub M, Sharma D. Brunner gland lesions. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelbrunnersgland.html. Accessed September 17th, 2025.
Definition / general
- Brunner gland hyperplasia (BGH) is defined as benign hyperplastic proliferation of mature Brunner glands, commonly in the duodenal bulb
Essential features
- BGH clinical findings can be nonspecific; endoscopies show a polypoid / pedunculated mass that varies in size
- Histologic features show proliferation of Brunner glands that extends to the submucosa
- Smooth muscle proliferation and mature adipose tissue favors Brunner gland hamartoma
Terminology
- Brunner gland hamartoma, Brunner gland adenoma and Brunneroma: > 0.5 cm with dilated glands and smooth muscle proliferation (Adv Ther 2021;38:2779, Rev Esp Enferm Dig 2022;114:124)
ICD coding
- ICD-11: DA53.Y - other specified duodenal polyp
Epidemiology
- BGH represents < 1% of all gastrointestinal tumors and ~5% of benign duodenal tumors (Int J Clin Exp Pathol 2015;8:7565)
- More prevalent from 50 - 70 years old (World J Gastroenterol 2004;10:2616)
- Risk factors (World J Gastroenterol 2004;10:2616)
- High gastric acid secretion
- Helicobacter pylori infection
- Chronic pancreatitis
Sites
- Most common in proximal duodenum (57% in duodenal bulb) (Gastrointest Endosc 1998;47:403)
Pathophysiology
- Poorly understood
- Hypothesized to be embryonic dysplasia of the duodenum (Brunner gland hamartoma) (JNMA J Nepal Med Assoc 2019;57:50)
- High gastric acid secretion can cause BGH, increasing alkaline mucous secretion (Scand J Gastroenterol 1990;25:165)
- Relationship between H. pylori infection and BHG is not clearly understood
Etiology
- Majority of cases have unclear etiology
- High acid environment in the duodenum, H. pylori and chronic pancreatitis may cause duodenal mucosal injury and trigger a repair process that includes foveolar metaplasia and BGH (BMC Gastroenterol 2014;14:14)
Clinical features
- Majority of patients are asymptomatic
- Nonspecific symptoms (J Surg Case Rep 2018;2018:rjy305)
- Dyspepsia, nausea and vomiting
- Abdominal pain and distension
- Rare cases present with gastrointestinal bleeding and iron deficiency anemia (especially in hamartomas and large lesions) (Endosc Ultrasound 2015;4:266)
- Few cases present with intestinal obstructions (lesions > 2 cm) (Am J Gastroenterol 1995;90:290)
- Ampullary lesions can present with biliary obstruction (Endoscopy 2000;32:998)
Diagnosis
- Upper GI endoscopy (EGD)
- Some lesions (especially in posterior wall of duodenum) can be missed on EGD
- Sensitivity of EGD is 72 - 89% (Eur J Radiol 1993;16:115)
- Evaluates extent, size and origin of the lesion
- Duodenal nodule that can be covered by normal mucosa (Gastrointest Endosc 2006;64:464)
- Can mimic lipoma, endocrine tumor or gastrointestinal stromal tumor (GIST) (Trop Gastroenterol 2010;31:121)
- Radiology (barium Xray and abdominal CT)
- More sensitive for larger lesions (J Comput Assist Tomogr 2010;34:543)
- See Radiology description
Radiology description
- Barium Xray
- Sessile or pedunculated polypoid filling lesions (large Brunner gland hamartomas) (Gastroenterol Hepatol (N Y) 2008;4:473)
- Multiple small filling defects and cobblestone pattern (diffuse nodular BGH) (AJR Am J Roentgenol 2006;187:715)
- CT (Dig Liver Dis 2021;53:134)
- Mass in the duodenum with central low attenuation
- Shows the relationship with adjacent organs
Prognostic factors
- Overall good prognosis for most lesions
- Very rare cases of BGH have been reported showing dysplasia or invasive carcinoma (2% and 0.3%, respectively) (Am J Surg Pathol 2005;29:1442, J Gastroenterol 2002;37:293)
Case reports
- 22 year old woman presented with duodenal intussusception due to BGH (Ann Surg 1959;150:160)
- 33 year old woman with large BGH presented with bleeding (Case Rep Surg 2021;2021:8861308)
- 57 year old man with pyloric obstruction due to Brunner gland hamartoma (J Surg Case Rep 2020;2020:rjaa191)
- 60 year old man with BGH mimicking malignant pathology (Int J Surg Case Rep 2021;81:105827)
Treatment
- Endoscopic or surgical resection
- Pancreaticoduodenectomy has been reported for giant hamartomas and diffuse nodular BGH (J Korean Med Sci 2008;23:540)
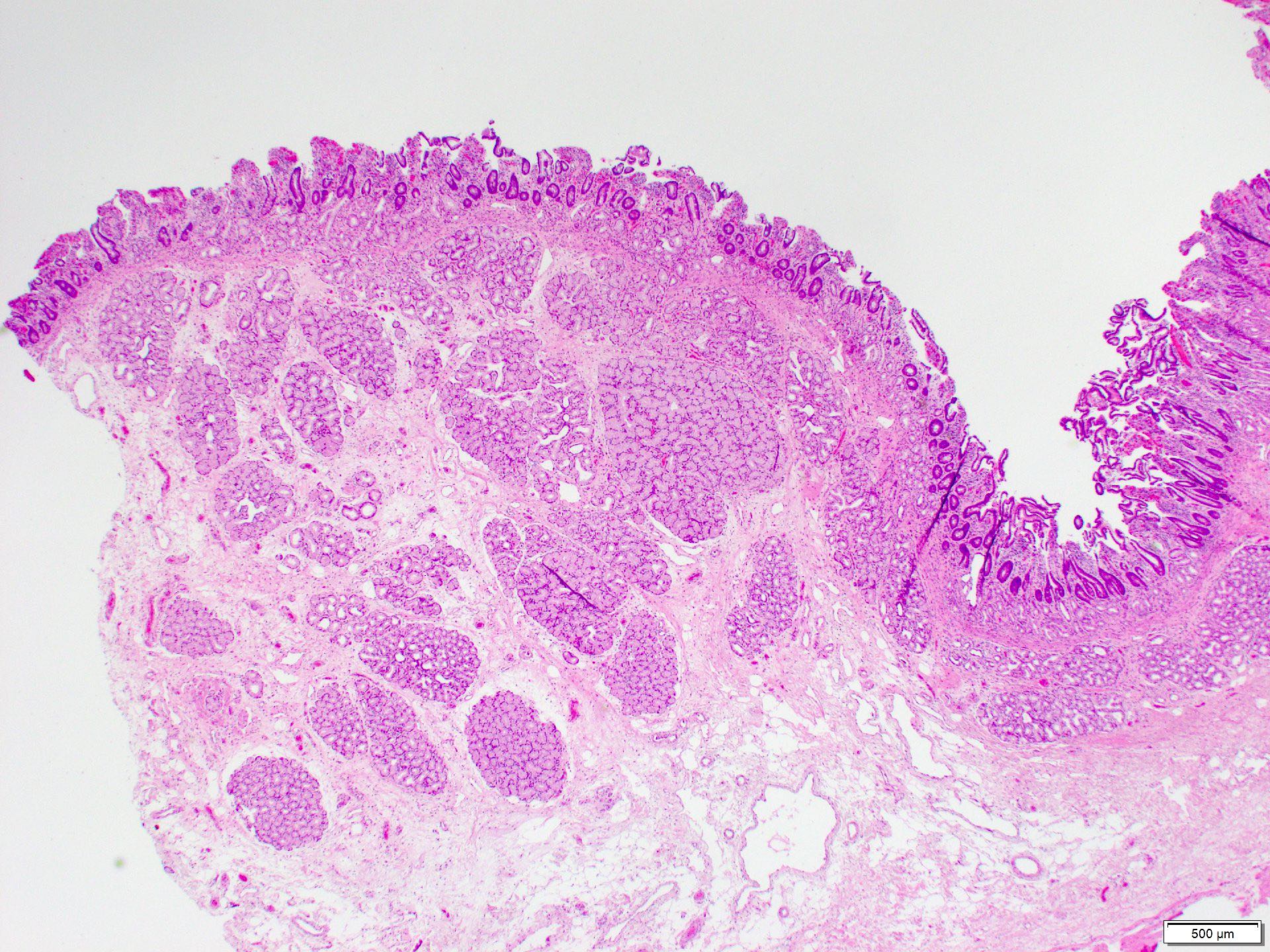
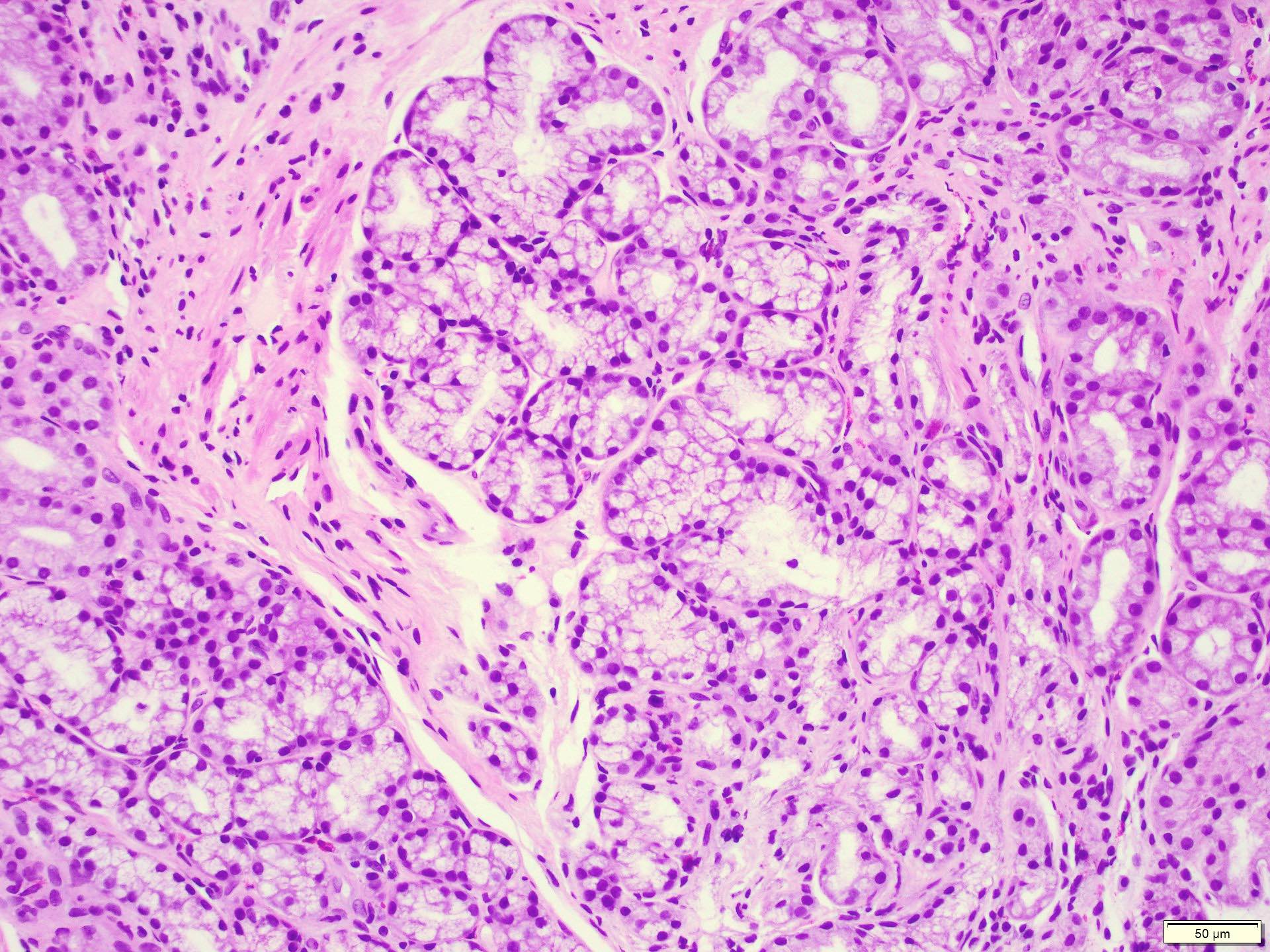
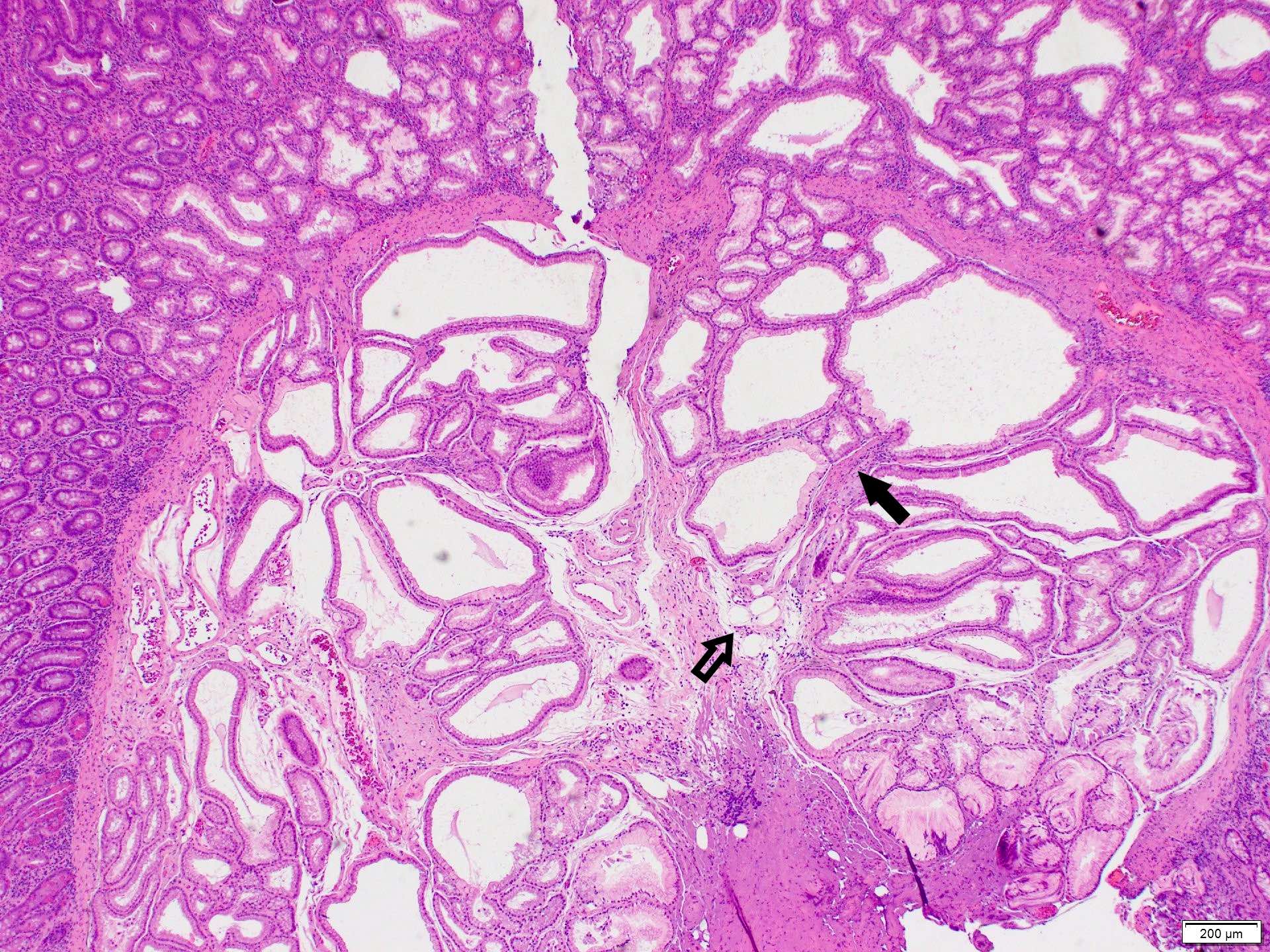
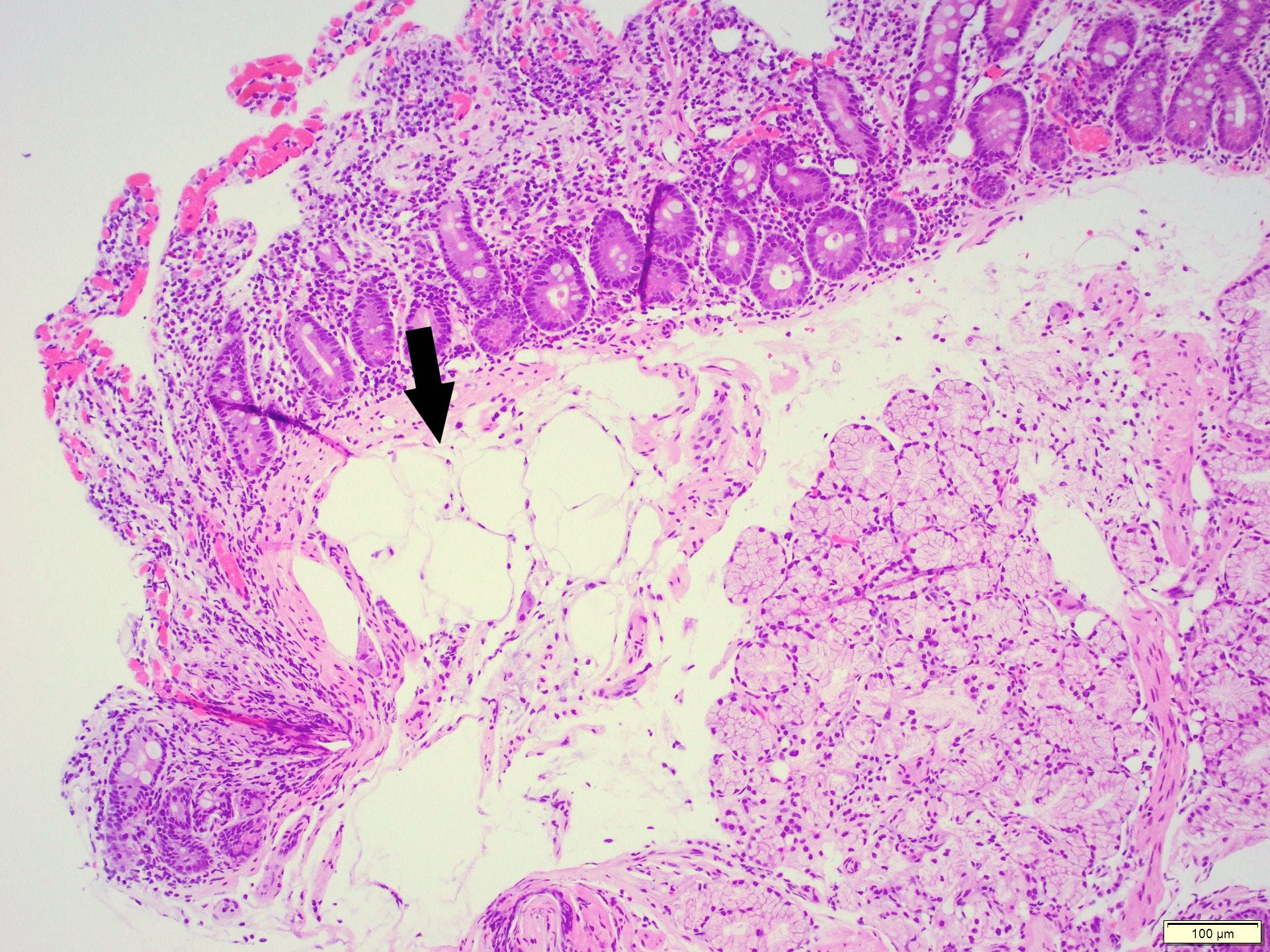
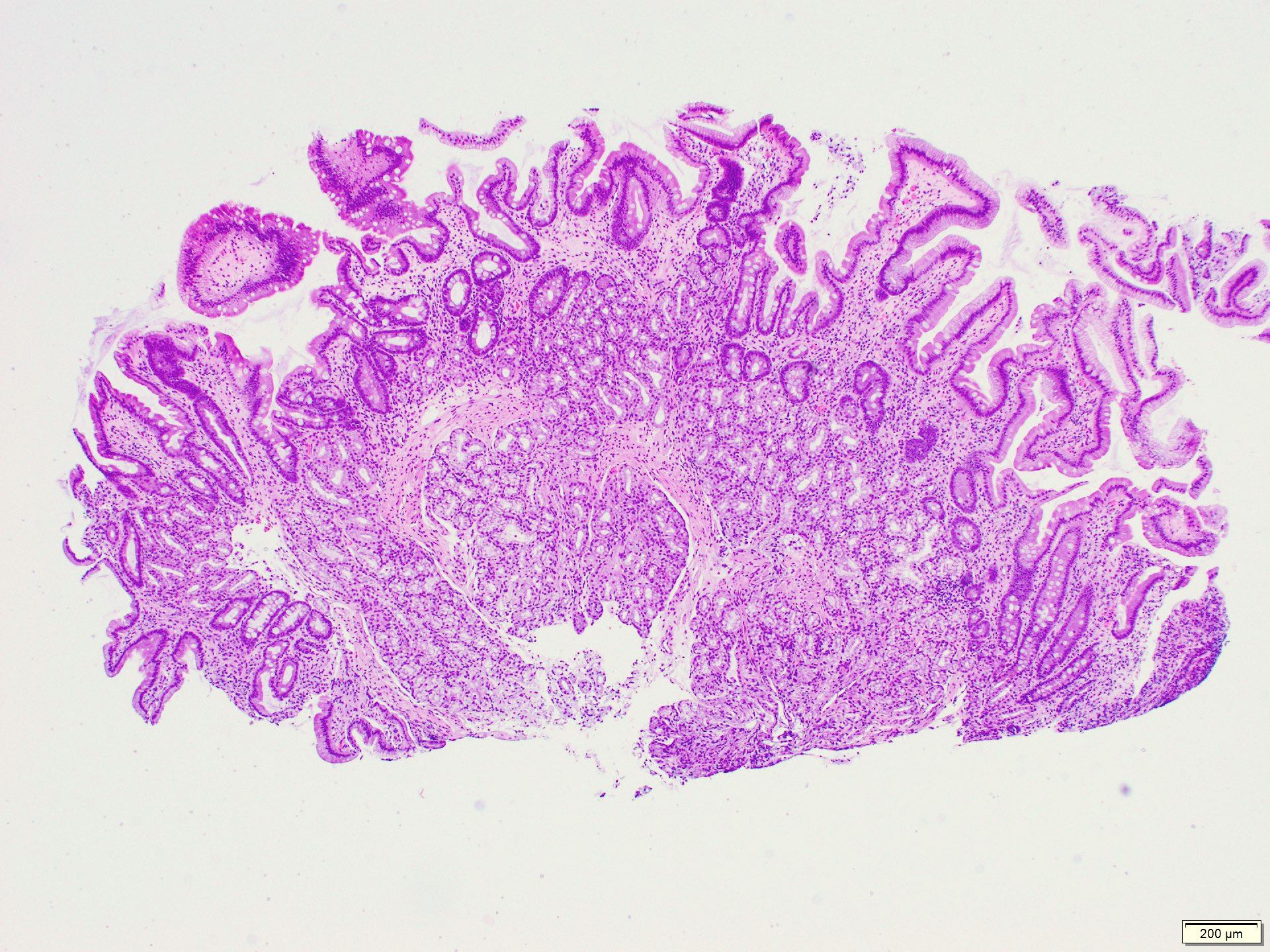
Microscopic (histologic) description
- Brunner gland hyperplasia
- Closely packed clusters of cuboidal cells with basal round to flat nuclei and foamy cytoplasm with neutral mucin
- Features of peptic duodenitis, foveolar metaplasia or mucosal injury can be seen (Scand J Gastroenterol 1990;25:165)
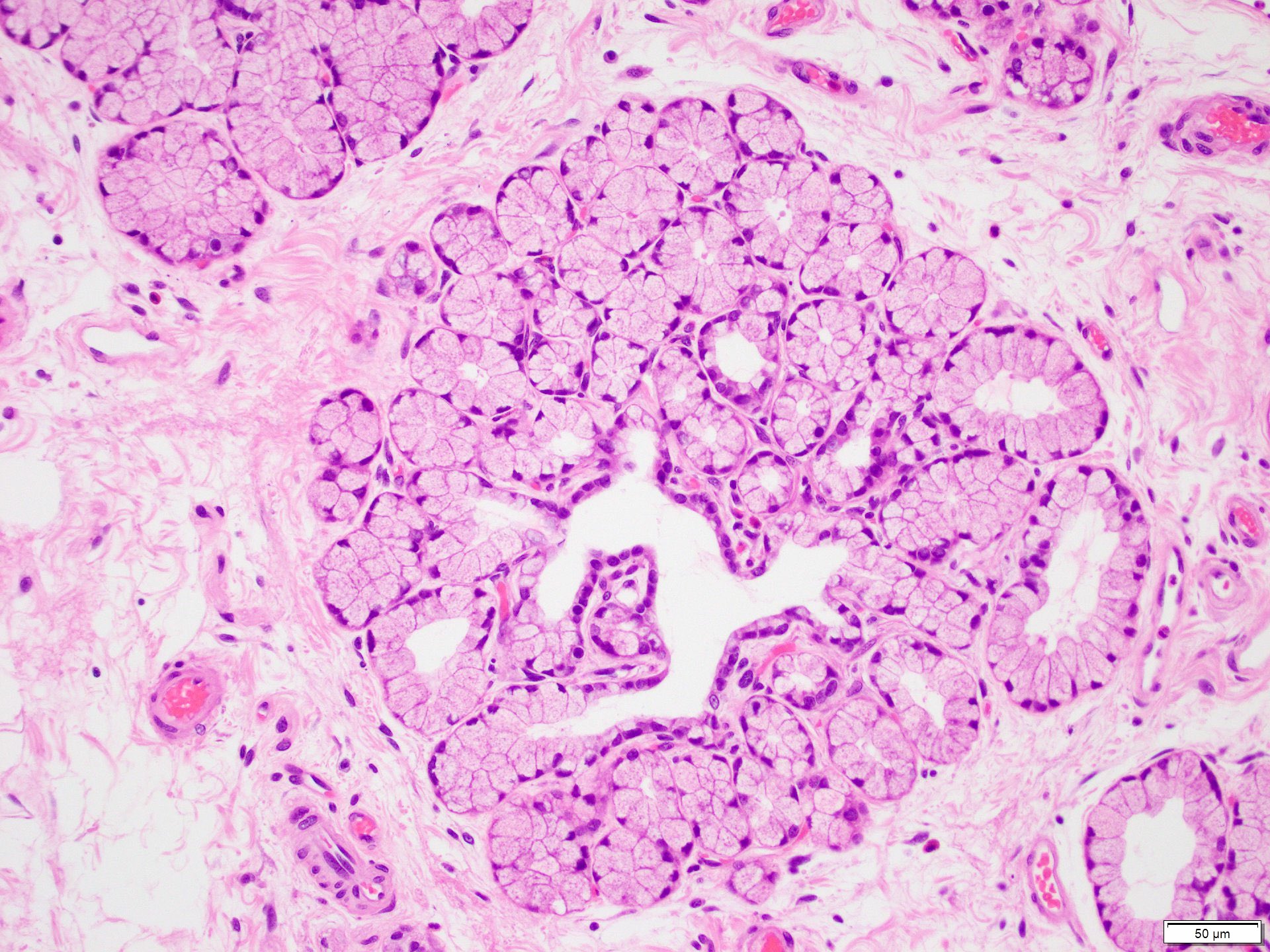
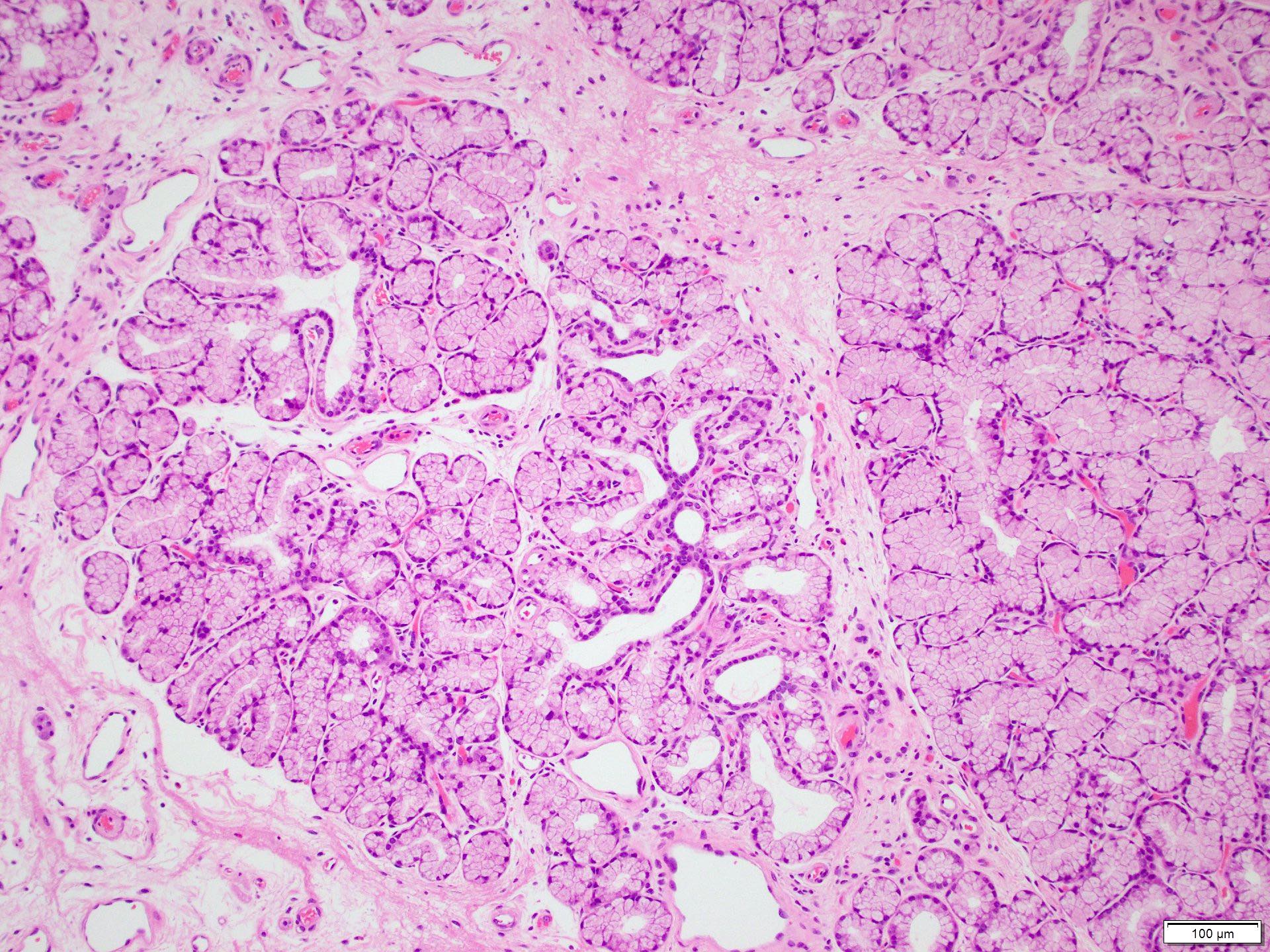
- Brunner gland hamartoma
- Typically, larger size: > 0.5 cm
- Smooth muscle and adipose tissue, intermixed with proliferating Brunner glands and cystically dilated ducts
- Brunner glands can be intermingled with mature adipose tissue / adipocytes
- Brunner gland adenoma
- Similar morphology to Brunner gland hyperplasia or hamartoma, with cytological atypia, nuclear enlargement and mitosis (Int J Clin Exp Pathol 2015;8:7565)
Microscopic (histologic) images
Positive stains
Sample pathology report
- Duodenum, polyp, biopsy:
- Polypoid duodenal mucosa with prominent Brunner glands consistent with Brunner gland hyperplasia
- Negative for dysplasia or malignancy
Differential diagnosis
- Gastric heterotopia:
- Commonly in first and second parts of duodenum
- Gastric oxyntic glands with foveolar epithelium on the surface
- Pancreatic heterotopia:
- Variable mixture of elements of normal pancreatic tissue including acini, ducts or islet cells
- Neuroendocrine tumors:
- Commonly in first and second parts of duodenum, including the ampulla
- Nests of uniform cells with round to oval nuclei with salt and pepper chromatin
- Tumor cells are positive for chromogranin A and synaptophysin
- Duodenal adenoma:
- Common in the ampullary area
- Tubular or villous architecture with dysplasia of the surface epithelium
- Gastrointestinal stromal tumor (GIST):
- Leiomyoma:
- Incidental finding
- Can be merged with muscularis mucosa
- Positive for smooth muscle actin and desmin
- Lipoma:
- Rare, submucosal
- May be ulcerated
- Needs to be distinguished from fat rich Brunner gland hamartoma
Additional references
Practice question #1
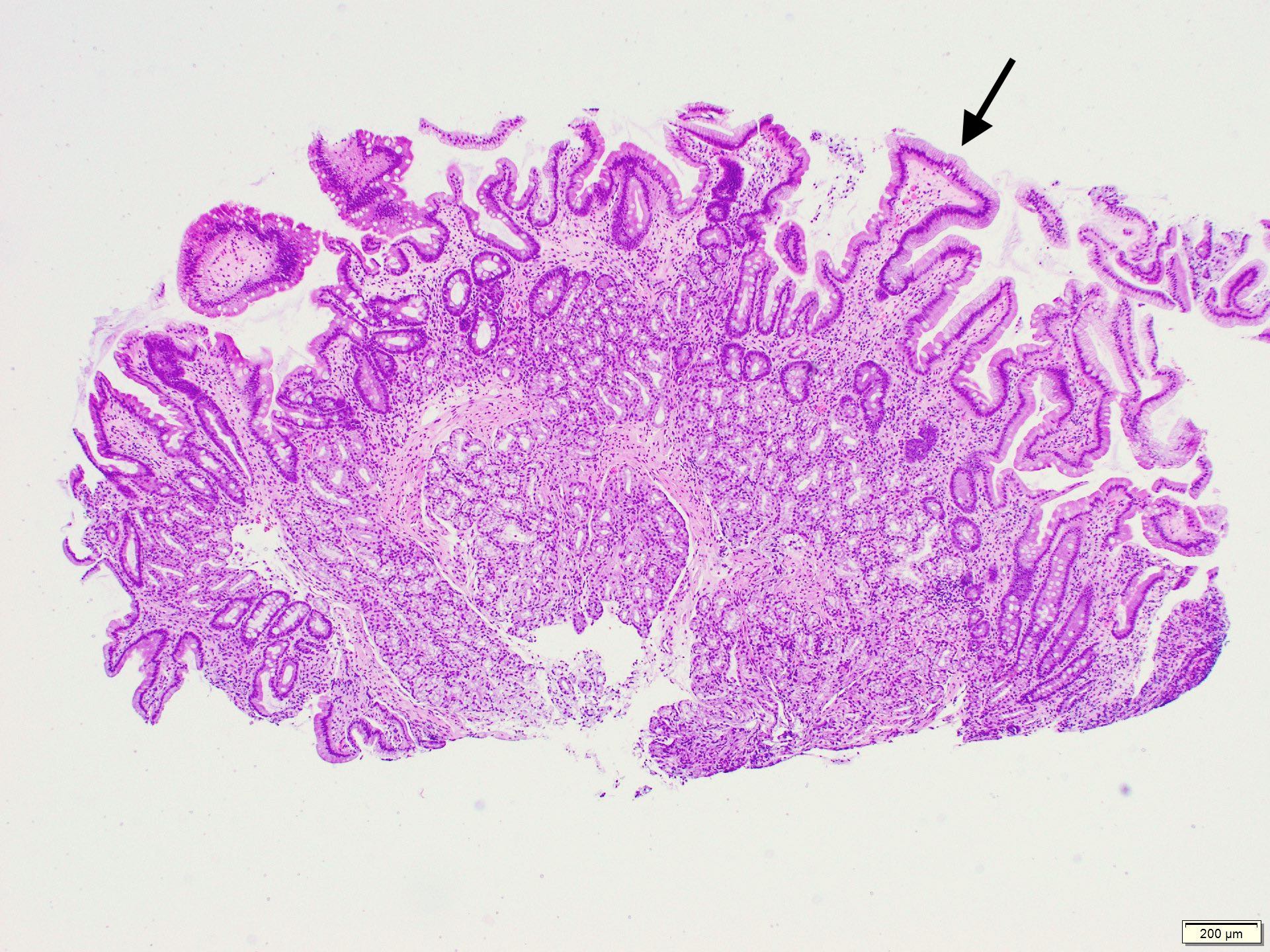
A 52 year old man with history of dyspepsia and abdominal pain. The upper GI endoscopy showed a 0.5 cm polyp in the duodenal bulb. Which of the following is a possible etiology of the findings depicted in the image above?
- Gastric atrophy
- Immunosuppression
- Increased duodenal acidic environment
- Inflammatory bowel disease
Practice answer #1
C. Increased duodenal acidic environment. The biopsy findings show Brunner gland hyperplasia with focal foveolar metaplasia. A possible etiology of Brunner gland hyperplasia is increased gastric acidity with compensatory increased alkaline secretion by Brunner glands in the duodenum. Answer D is incorrect due to a lack of chronic inflammation and mucosal injury. Answer B is incorrect due to lack of additional findings associated with immunosuppression like infectious agents or inflammation. Answer A is incorrect as Brunner gland hyperplasia is usually associated with gastric increased acid secretion, not gastric atrophy.
Comment Here
Reference: Brunner gland hyperplasia
Comment Here
Reference: Brunner gland hyperplasia
Practice question #2
The figure above is from a duodenal biopsy in a patient with duodenal polyp on upper GI endoscopy. Which of the following, if present, favors a diagnosis of Brunner gland hamartoma over Brunner gland hyperplasia?
- Lesion size < 0.5 cm
- Presence of foveolar metaplasia
- Smooth muscle proliferation
- Superficial lesion limited to the mucosa
Practice answer #2
C. Smooth muscle proliferation. Brunner gland hamartoma is typically a larger lesion (> 0.5 cm), composed of proliferation of Brunner glands, smooth muscle and mature adipose tissue. Brunner gland hyperplasia usually presents as a small lesion (< 0.5 cm) showing only hyperplastic Brunner glands with or without foveolar metaplasia. Answer D is incorrect as both Brunner gland hamartoma and hyperplasia can extend to the submucosa. Answer A is incorrect as Brunner gland hamartoma is usually > 0.5 cm in size. Answer B is incorrect as foveolar metaplasia is mostly associated with Brunner gland hyperplasia.
Comment Here
Reference: Brunner gland hyperplasia
Comment Here
Reference: Brunner gland hyperplasia