Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Yakoub M, Sharma D. Juvenile polyposis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallboweljuvenilepolyposis.html. Accessed April 25th, 2024.
Definition / general
- Juvenile polyposis (JP) of small intestine is a rare condition that is characterized by presence of multiple hamartomatous polyps in the small bowel typically presenting during childhood
- This topic describes features of juvenile polyps in the small intestine that differ from colonic juvenile (retention) polyp
Essential features
- Clinical findings of sporadic juvenile polyps can be nonspecific
- Multiple juvenile polyps of small intestine with or without multiple colorectal juvenile polyps are required diagnostic criteria for juvenile polyposis syndrome (JPS)
- Juvenile polyps in small intestine can present with intussusception
- Histologic features show cystically dilated or branched glands with edematous and inflamed stroma with or without dysplasia
- Close surveillance and genetic testing are recommended for symptomatic cases
Terminology
- Hamartomatous gastrointestinal polyposis
ICD coding
- ICD-11: DA98.Z - polyps of small intestine, unspecified
Epidemiology
- Juvenile polyposis syndrome (JPS) has an incidence of 1 per 100,000 live births in western countries (Bull World Health Organ 1990;68:655)
- Incidence of small intestine JP is very low compared to colorectal JP and is most commonly located in the duodenum, ranging between 14 and 33% (Endoscopy 2009;41:1001)
- JPS is an autosomal dominant inherited disease associated with the presence of mutation in SMAD4 / DPC4 or BMPR1A genes (Clin Genet 2009;75:79)
Sites
- The most common site for small intestine JPS is the duodenum (14 - 33%) (Ann Surg Oncol 1998;5:751)
Pathophysiology
- Classical mutational profile in JPS involves either the bone morphogenetic protein receptor 1A (BMPR1A), located at 10q23 or SMAD4 gene, located at 18q21 (Clin Genet 2009;75:79, Gut 2008;57:623)
- Juvenile polyposis of infancy shows contiguous deletion of BMPR1A and PTEN genes at chromosome 10q23 (Am J Hum Genet 2006;78:1066)
- Neoplasia may arise in JPS from adenomatous epithelium within the polyp through a landscaper mechanism and abnormal stromal environment that affects TGFβ signaling (Science 1998;280:1036)
- Pathophysiology and etiology of sporadic / solitary juvenile polyps in small bowel is unknown
Etiology
- See Pathophysiology
Clinical features
- Can be asymptomatic
- Clinical presentation includes (Am J Surg 1975;129:198, Folia Med (Plovdiv) 2022;64:693)
- Abdominal pain, nausea and vomiting
- Gastrointestinal bleeding and iron deficiency anemia
- Intermittent obstruction including intussusception
- Endoscopic findings
- Video capsule endoscopy
- Minimally invasive
- Can explore the entire small bowel
- Diagnostic sensitivity for epithelial and subepithelial polyps ≤ 1 cm is 75% and 83%, respectively (Endoscopy 2005;37:960)
- Double and single balloon enteroscopy
- Enables sampling and intervention
- Diagnostic sensitivity in double balloon enteroscopy for epithelial and subepithelial polyps ≤ 1 cm is 100% and 97%, respectively (Gastrointest Endosc 2012;76:344)
- Video capsule endoscopy
- JPS can present with duodenal adenocarcinoma; however, the risk analysis of cancer development in a juvenile polyp is unclear (Ann Surg Oncol 1998;5:751)
Diagnosis
- Diagnostic criteria of JPS are based on these criteria (Histopathology 1988;13:619, J Pediatr Gastroenterol Nutr 2019;68:453)
- More than 3 - 5 juvenile polyps in colon or rectum
- Multiple juvenile polyps throughout gastrointestinal tract (including stomach and small intestine)
- Any number of juvenile polyps and positive family history
- Diagnostic criteria of isolated or single small intestine juvenile polyps are unclear (J Pediatr Gastroenterol Nutr 2020;71:491)
- Diagnosis can be reached by integrating histology, immunohistochemistry and next generation sequencing (Fam Cancer 2022;21:441)
Laboratory
- Genetic testing of the following gene mutations
- SMAD4 and BMPR1A: for juvenile polyposis syndrome
- PTEN: identified in juvenile polyposis of infancy and Cowden syndrome
- STK11 / LKB1: seen in Peutz-Jeghers syndrome
- Preferred for at risk patients, starting at age of 4 (Curr Mol Med 2007;7:29)
- Upper and lower endoscopy surveillance starting at age 12 if symptomatic (Dis Colon Rectum 2012;55:1038)
Radiology description
- Magnetic resonance enterography (MRE)
- Noninvasive
- Compared to video capsule endoscopy, magnetic resonance enterography showed comparable rates of detection for large (> 15 mm) polyps (Abdom Imaging 2012;37:279)
Prognostic factors
- Risk of upper gastrointestinal cancer, risk analysis is unclear
Case reports
- 3 year old girl presented with chronic iron deficiency anemia caused by a single painless juvenile polyp in the small intestine (J Pediatr Gastroenterol Nutr 2020;71:491)
- 35 year old woman presented with a juvenile polyp complicated with intussusception of the small intestine (Folia Med (Plovdiv) 2022;64:693)
- 50 year old woman presented with severe iron deficiency anemia and numerous stomach and jejunum polyps (Fam Cancer 2022;21:441)
- 73 year old woman with an isolated benign hamartomatous (juvenile-like) polyp (Am J Case Rep 2023:24:e938929)
Treatment
- Screening and management for small intestine JPS are based on symptoms (Am J Gastroenterol 2015;110:223)
- Goal is preventing malignancy through close surveillance and endoscopic resection if symptomatic
- Sirolimus studies showed decreased disease burden in JPS and juvenile polyposis of infancy (Pediatrics 2019;144:e20182922)
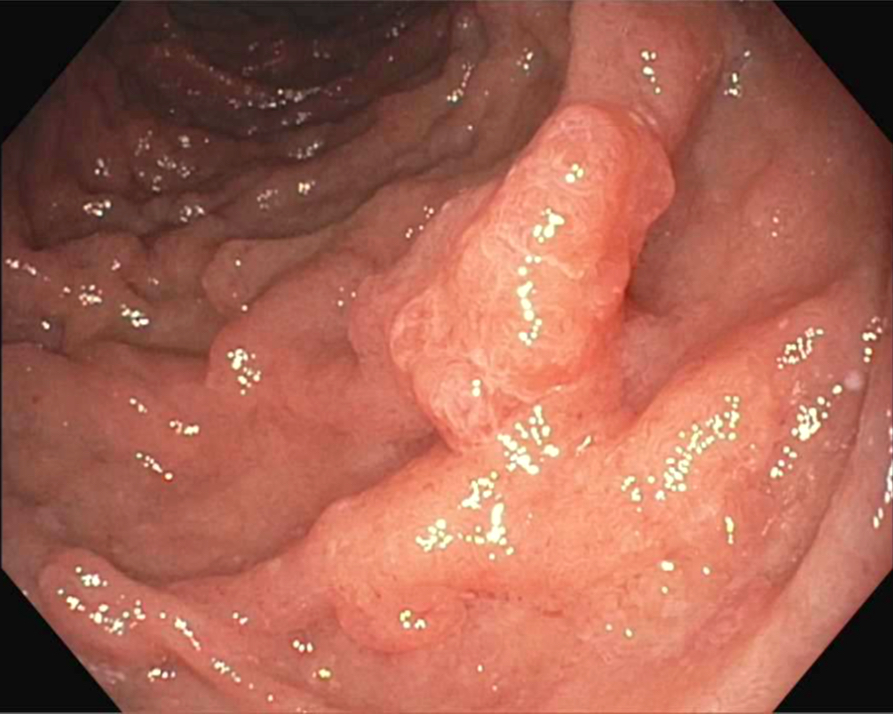
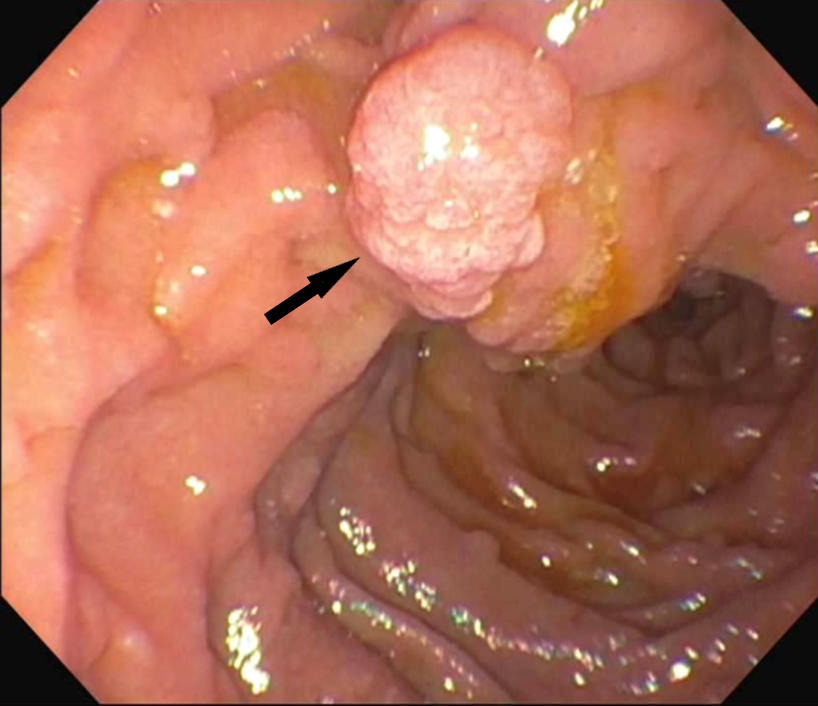
Clinical images
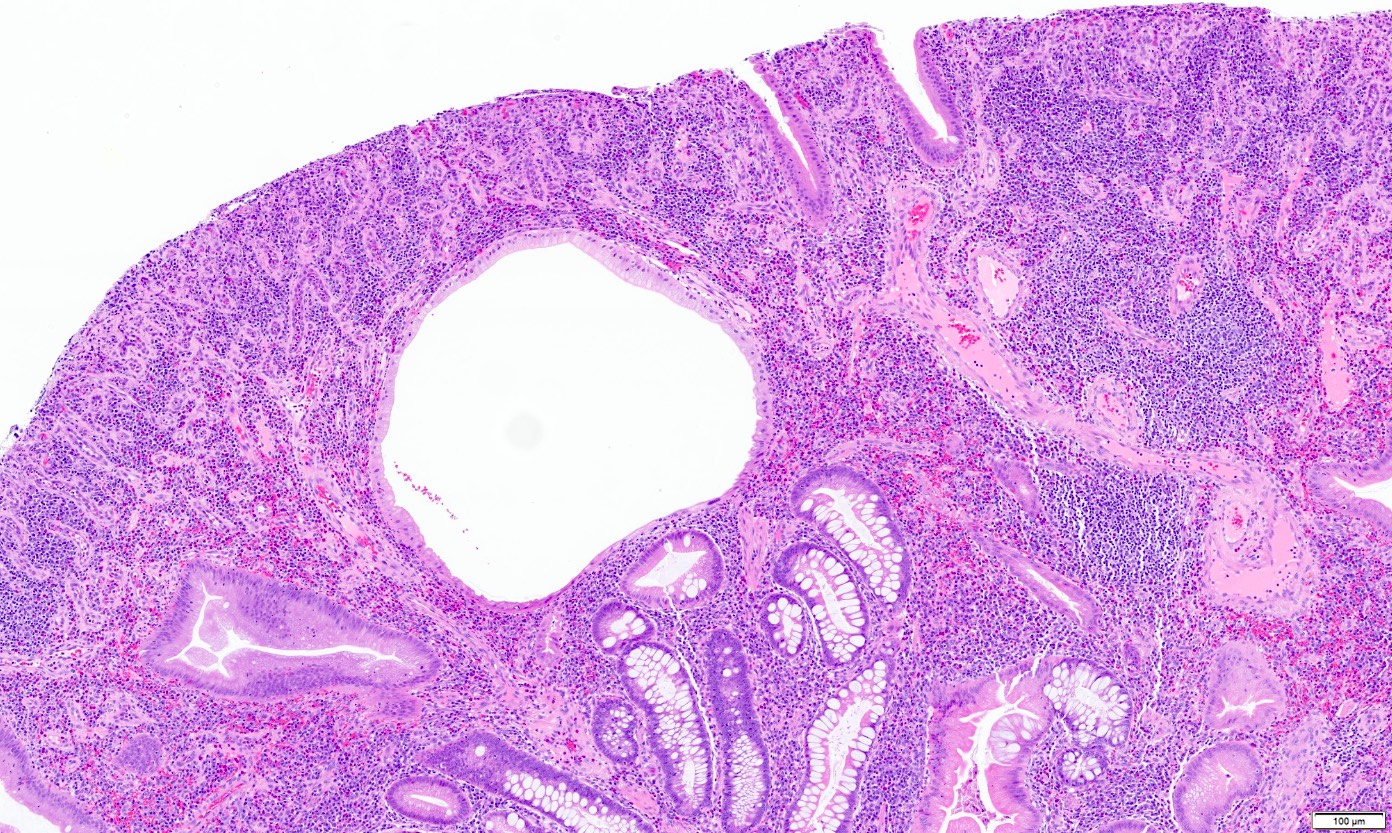
Gross description
- Multiple polyps in JPS, up to 200 polyps, with variable size reaching up to a few centimeters in some cases (J Gastroenterol Hepatol 2005;20:1634)
- Surface of the polyp may show erosion or ulceration
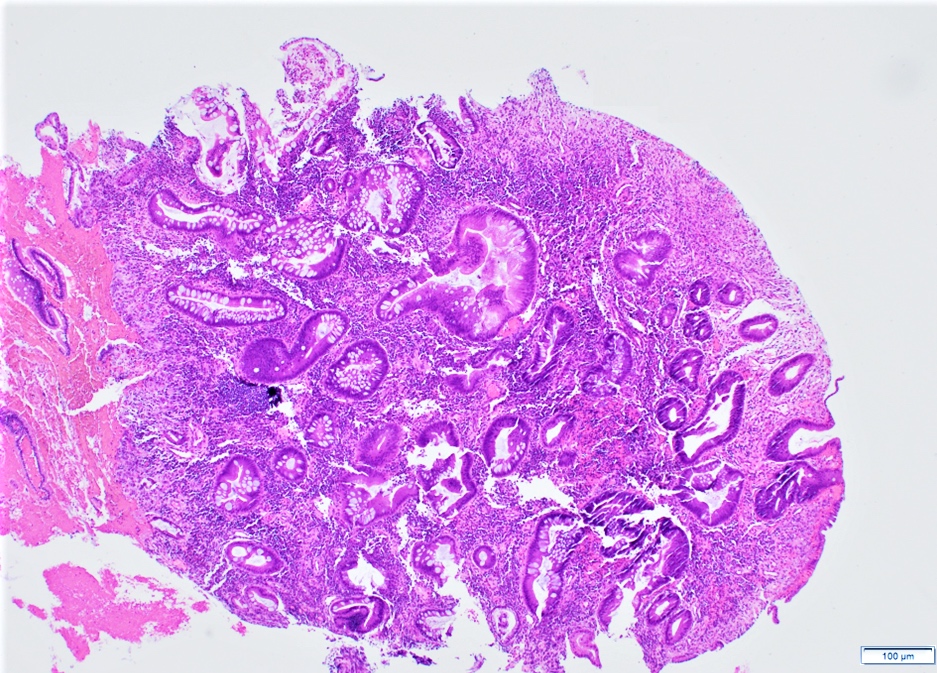
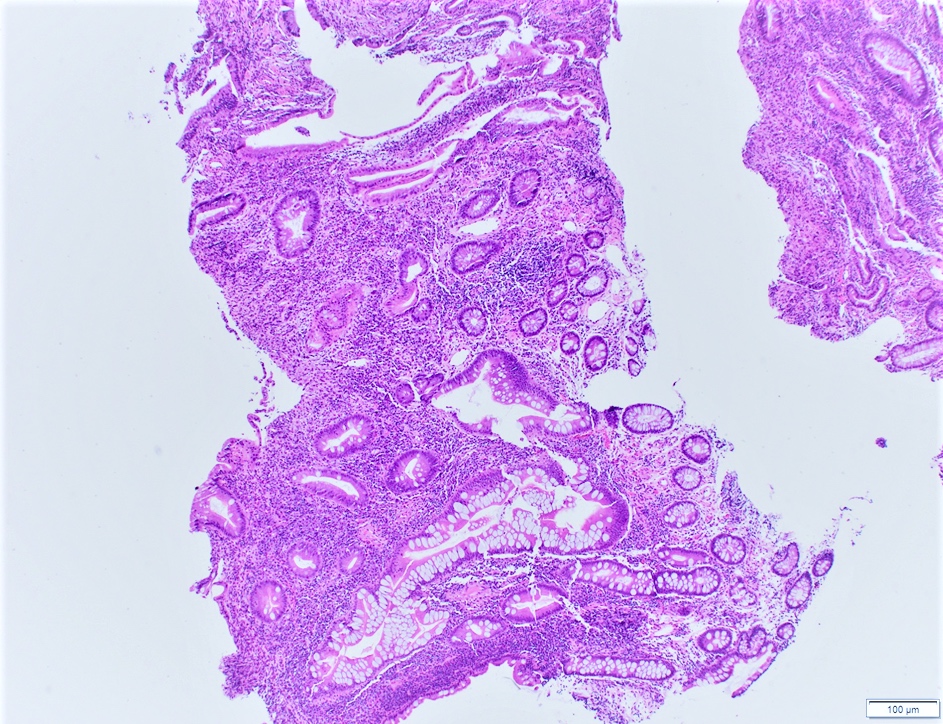
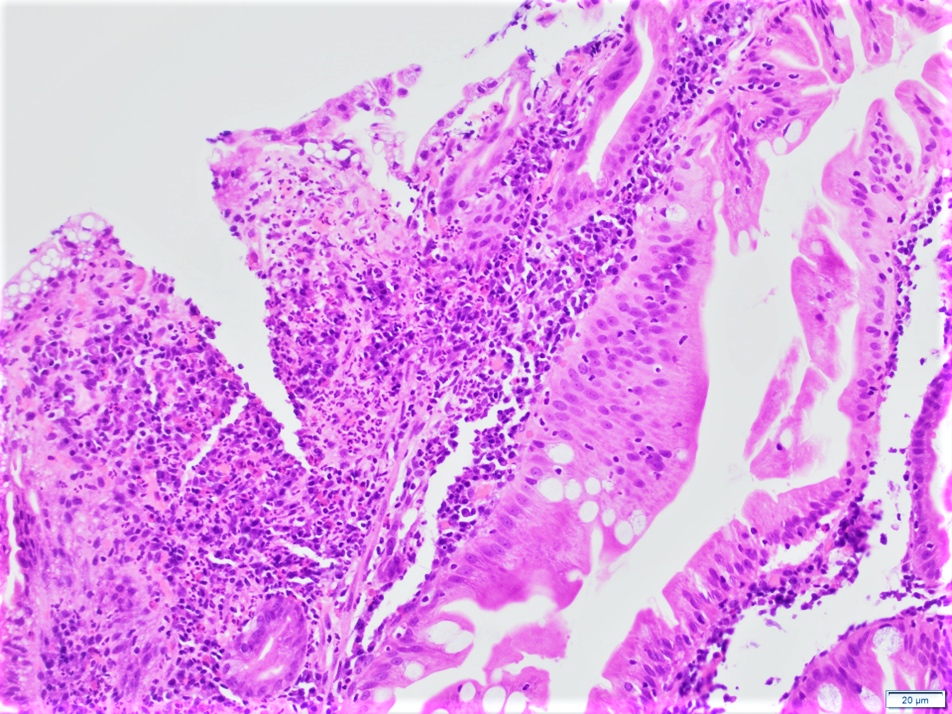
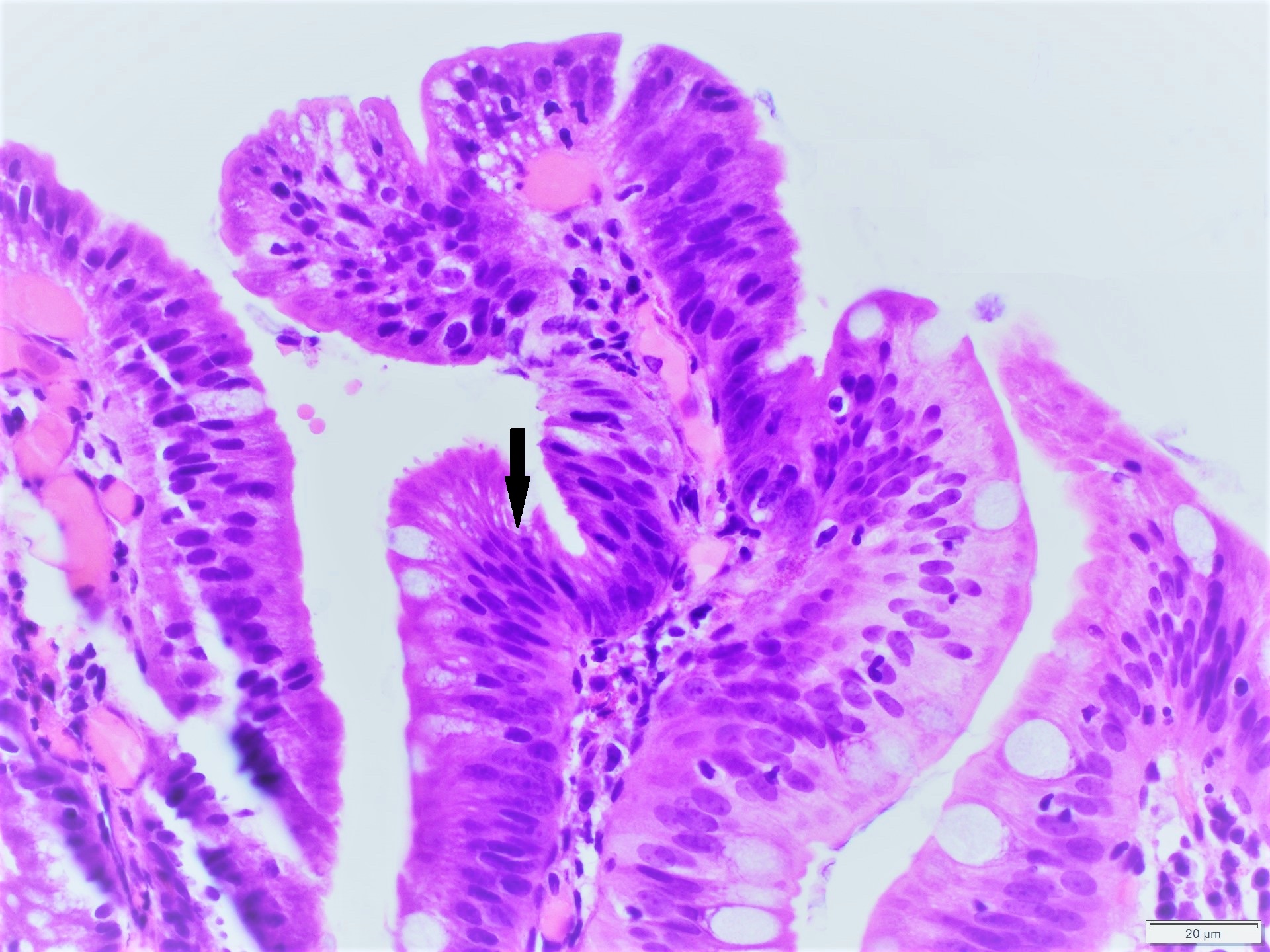
Microscopic (histologic) description
- Solitary or multiple hamartomatous polyps
- Classic solitary polyps (Histopathology 1988;13:619)
- Eroded surface and reactive epithelium
- Abundant edematous stroma with inflammatory cells and granulation tissue
- Cystically dilated glands
- Hyperplastic glands can be seen
- Multilobulated / atypical polyp
- Finger-like lobules
- Increased epithelial - stromal ratio
- Budding and branching glands
- Focal dysplasia can be present (Am J Surg Pathol 2011;35:530)
Microscopic (histologic) images
Contributed by Divya Sharma, M.D., Rachel Sheridan, M.D. and Sara Szabo, M.D.
Negative stains
- Loss of SMAD4 expression in ~50% of JPS patients with germline SMAD4 mutation (somatic inactivation of the SMAD4 wild type allele) (Clin Cancer Res 2010;16:4126)
- Loss of SMAD4 is not seen in sporadic juvenile polyps or in patients with BMPR1A mutations
Molecular / cytogenetics description
- Genetic testing for germline mutations in SMAD4, BMPR1A and PTEN genes
Sample pathology report
- Duodenum, polyp, endoscopic resection:
- Polypoid mucosa with edematous stroma and cystically dilated glands consistent with features of juvenile polyps
- Negative for dysplasia or malignancy
Differential diagnosis
- Peutz-Jeghers polyp:
- Commonly in jejunum and ileum
- Papillary villous architecture with tree-like arborization of smooth muscles and normal overlying epithelium
- STK11 / LKB1 gene mutations
- Inflammatory polyp:
- Branched and cystically dilated glands with reactive atypia of the mucosa
- Lamina propria acute and chronic inflammation
- Hyperplastic polyp:
- Common in second part of duodenum
- Classically a solitary polyp
- Epithelial serrations and bland cytology
- Association with BRAF V600E and KRAS
- Cowden syndrome polyp:
- Dilated glands with expanded stroma
- Can be associated with intramucosal lipoma
- No dysplasia
- Histologically can be similar to juvenile polyp
- PTEN gene mutations
- Cronkhite-Canada polyp:
- Ill defined polyps
- Cystically dilated glands with edematous stroma
- Mononuclear and eosinophilic infiltrate
- Histologically can be similar to juvenile polyp
- Nonhereditary
- Ménétrier disease:
- Most commonly located in stomach
- Presentation with small bowel polyposis is rare
- Marked foveolar hyperplasia with no atypia
- Interstitial edema with mild inflammatory infiltrate
Additional references
Board review style question #1
Upper esophagogastroduodenoscopy (EGD) in a 12 year old patient with history of abdominal pain and nausea showed multiple polyps in the second part of the duodenum. The largest polyp was biopsied and the microscopic findings demonstrated surface erosion and cystically dilated glands. Which of the following is a criterion for a diagnosis of juvenile polyposis syndrome (JPS) in this patient?
- 2 colon polyps from the same patient with similar morphology to the duodenal polyp
- Germline mutation in STK11 gene
- Multiple duodenal polyps that are at least 10 mm in size
- Positive family history
Board review style answer #1
D. Positive family history. The biopsy findings show a polyp with features suggestive of a juvenile polyp (eroded surface, inflammatory stroma and dilated glands). A diagnosis of JPS requires one of the following criteria
Answer B is incorrect as STK11 mutations are seen in Peutz-Jeghers syndrome. Answer A is incorrect because the diagnostic criteria of JPS requires the presence of more than 3 - 5 colorectal polyps. Answer C is incorrect as there is no polyp size cut off criteria for the diagnosis of JPS.
Comment Here
Reference: Juvenile polyposis
- More than 3 - 5 juvenile polyps in colon or rectum
- Multiple juvenile polyps throughout gastrointestinal tract (including stomach and small intestine)
- Any number of juvenile polyps and positive family history
Answer B is incorrect as STK11 mutations are seen in Peutz-Jeghers syndrome. Answer A is incorrect because the diagnostic criteria of JPS requires the presence of more than 3 - 5 colorectal polyps. Answer C is incorrect as there is no polyp size cut off criteria for the diagnosis of JPS.
Comment Here
Reference: Juvenile polyposis
Board review style question #2
The microscopic image above is from a biopsy of a duodenal polyp. Which of the following features, if present, favors a diagnosis of juvenile polyp over an inflammatory polyp?
- Clinical history of inflammatory bowel disease
- Hyperplasia of the glands with gland branching and cystic dilatation
- Reactive atypia of the mucosal glands
- Solitary polyp and mucosal hyperemia seen on esophagogastroduodenoscopy (EGD)
Board review style answer #2
B. Hyperplasia of the glands with gland branching and cystic dilatation. These features are generally nonspecific; however, they are less likely to be seen in inflammatory polyps.
Answer C is incorrect because reactive atypia in the glands can be seen in both juvenile and inflammatory polyps. Answers A and D are incorrect as these features favor a diagnosis of an inflammatory polyp.
Comment Here
Reference: Juvenile polyposis
Comment Here
Reference: Juvenile polyposis