Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Abdulameer S, Mantilla JG. Kaposi sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuekaposi.html. Accessed September 10th, 2025.
Definition / general
- Vascular neoplasm caused by human herpesvirus 8 (HHV8)
- Tends to be indolent but may be locally aggressive
Essential features
- Malignant vascular neoplasm of intermediate behavior
- In all forms and cases, the etiologic agent is human herpesvirus 8 (HHV8)
- Histologic features are similar for all clinical variants
- Slit-like vascular spaces formed by spindled endothelial cells with minimal to moderate atypia; hemorrhage, hemosiderin deposition and plasma cells are common
Terminology
- Idiopathic multiple pigmented sarcoma of the skin (J Emerg Med 1995;13:671)
- Multiple hemorrhagic sarcoma of Kaposi (Am J Pathol 1927;3:321)
ICD coding
Epidemiology
- Depends on the clinical variant of Kaposi sarcoma (4 subtypes) (Nat Rev Dis Primers 2019;5:9, StatPearls: Kaposi Sarcoma [Accessed 6 October 2022])
- Classic / sporadic (Mediterranean) (Cancers (Basel) 2021;13:5692)
- Middle aged to elderly; M > F
- Ethnic groups from regions with high prevalence of HHV8 (Middle East, Eastern Europe and the Mediterranean) are at increased risk
- Endemic (African)
- Male adults and children of both sexes
- Not related to HIV
- Mirrors HHV8 seropositivity
- Most commonly in sub-Saharan Africa
- Iatrogenic (transplant related) (Cancers (Basel) 2021;13:5692)
- M > F
- Patients > 50 years
- Solid organ transplant patients
- Risk correlates with the level of immunosuppression; hence, the risk is higher in multiorgan transplants and with greater HLA mismatching
- Epidemic (HIV / AIDS associated) (Cancers (Basel) 2021;13:5692)
- Patients infected with HIV
- Risk increases with declining CD4 cell counts and is reduced with the early use of combined antiretroviral therapy (cART)
- Kaposi sarcoma in men who have sex with men (MSM) without HIV infection (AIDS 2008;22:1163)
- Very rare
- MSM without HIV infection who are not immunocompromised
- Favorable prognosis
- Classic / sporadic (Mediterranean) (Cancers (Basel) 2021;13:5692)
Sites
- Skin is the most common location
- Visceral involvement includes lymph nodes, lungs, gastrointestinal system and other viscera; respiratory involvement can be fatal
- Classic / sporadic (Mediterranean)
- Usually few lesions limited to the lower limbs
- Visceral and mucosal involvement is uncommon
- Endemic (African)
- Children develop visceral involvement including the lymph nodes
- Skin involvement is not typical in children
- Adults develop cutaneous lesions akin to classic Kaposi sarcoma; can sometimes be locally aggressive
- Adults can present with lower limb lymphedema
- Visceral involvement may occur in some adult patients
- Iatrogenic (transplant related)
- Typically affects the lower limbs
- Mucosal and visceral involvement is relatively common
- Epidemic (HIV / AIDS associated)
- Skin lesions on the limbs, trunk and face; lesions can be localized or disseminated
- Mucosal and visceral lesions are more common in patients with low CD4 count and high viral loads
- Kaposi sarcoma in men who have sex with men (MSM) without HIV infection
- Few cutaneous lesions at any site
- Visceral and mucosal involvement is rare
- References: Nat Rev Dis Primers 2019;5:9, StatPearls: Kaposi Sarcoma [Accessed 6 October 2022]
Pathophysiology
- Endothelial cells infected with HHV8 undergo altered lymphatic differentiation and manufacture cytokines, thus creating a favorable milieu for angiogenesis (Philos Trans R Soc Lond B Biol Sci 2017;372:20160275)
- Kaposi sarcoma nodules tend to be clonally different (StatPearls: Kaposi Sarcoma [Accessed 6 October 2022])
Etiology
- HHV8
- Enveloped, double stranded DNA virus
- HHV8 virus belongs to the Herpesviridae family of DNA viruses
- Diseases associated with HHV8 virus infections include Kaposi sarcoma (KS), primary effusion lymphoma (PEL) and multicentric Castleman disease (MCD)
Clinical features
- Progressive, enlarging red to violaceous skin lesions (Arch Pathol Lab Med 2013;137:289)
- Patch stage
- Red or purple macules or patches
- Plaque stage
- Thickened red, purple or brown plaques
- Tumor stage
- Nodule formation
- Patch stage
- Skin lesions may be painful with associated lymphedema and secondary infection
- All clinical subtypes of Kaposi sarcoma may show these stages
- Multiple different stages may be present simultaneously
- Clinical course of the subtypes of Kaposi sarcoma
- Classic / sporadic (Mediterranean)
- Usually indolent, rarely aggressive and disseminated
- Endemic (African)
- Usually indolent to locally invasive in adults
- Occasional rapid progression with visceral disease in adults
- Aggressive in children
- Iatrogenic (transplant related)
- May regress with modification of immunosuppression
- May be aggressive
- Epidemic (HIV / AIDS associated)
- Indolent or aggressive
- May regress with effective HIV treatment
- Kaposi sarcoma in men who have sex with men (MSM) without an HIV infection
- Usually indolent, although disseminated disease has been described
- Classic / sporadic (Mediterranean)
- References: Nat Rev Dis Primers 2019;5:9, StatPearls: Kaposi Sarcoma [Accessed 6 October 2022]
Diagnosis
- A biopsy or excision is needed for definitive diagnosis (StatPearls: Kaposi Sarcoma [Accessed 6 October 2022])
Laboratory
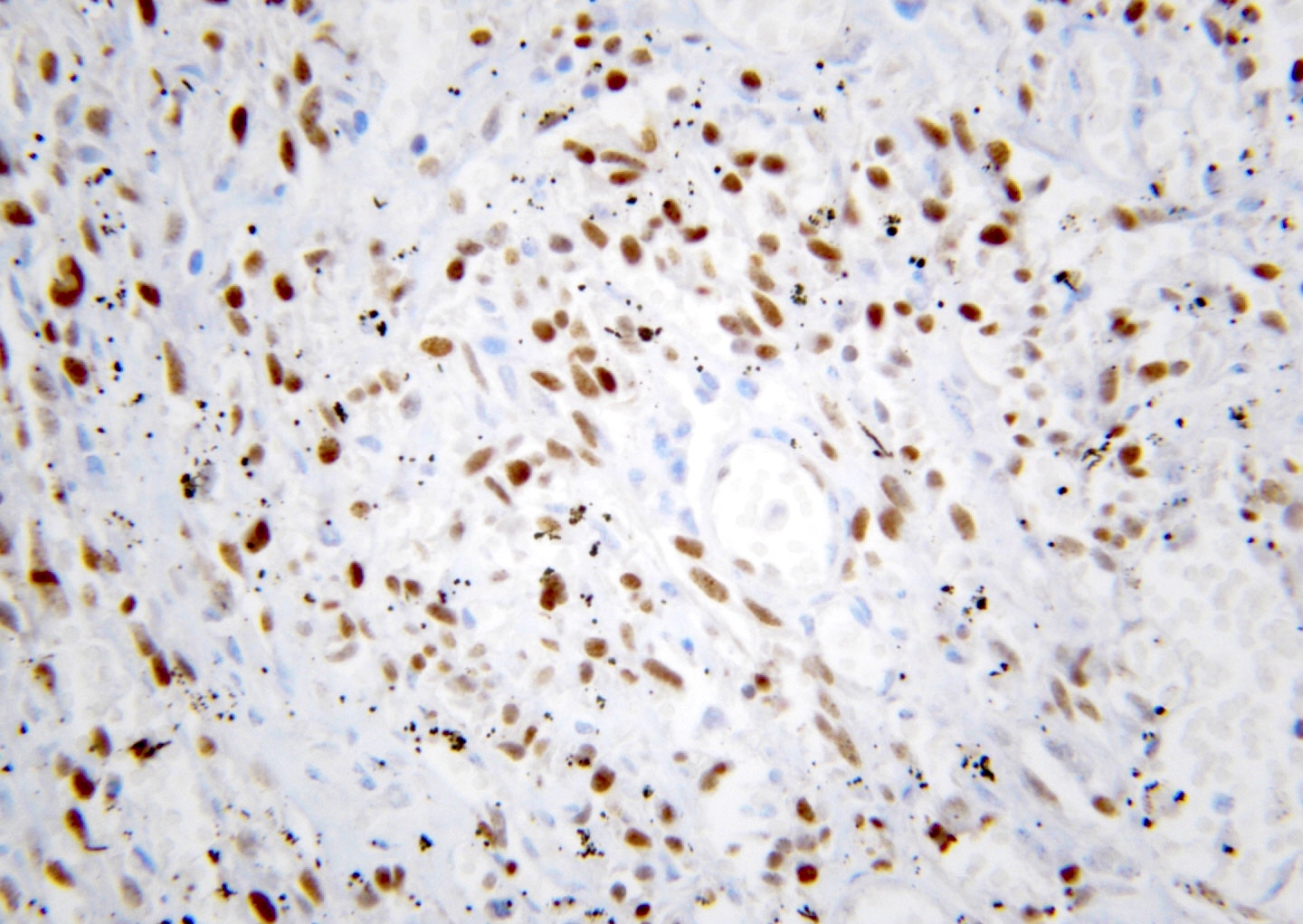
- IHC positivity for HHV8 LANA1 (latency associated nuclear antigen)
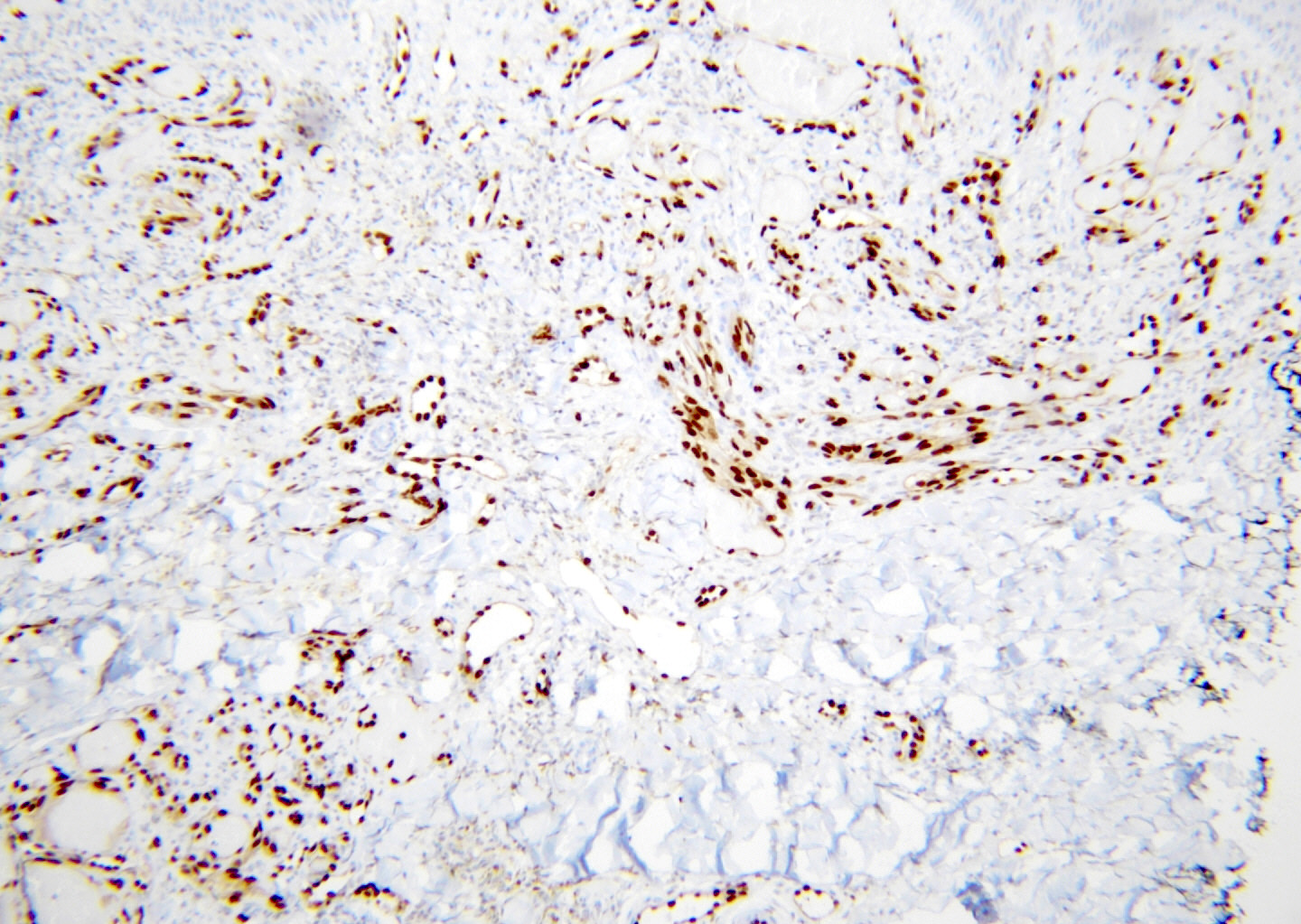
- Lesional cells also express ERG, CD34, CD31, factor VIII, D2-40
- Reference: StatPearls: Kaposi Sarcoma [Accessed 6 October 2022]
Radiology description
- Imaging facilitates the diagnosis, staging and follow up of Kaposi sarcoma
- Features are dependent upon site of involvement (Abdom Radiol (NY) 2021;46:5297)
Prognostic factors
- 20% of patients with the classic form of Kaposi sarcoma will die of disease; a similar percentage may develop secondary malignancies
- Endemic, HIV related and iatrogenic forms have a variable prognosis
- Prognosis may depend on CD4 count and the presence of opportunistic infections
- In patients with iatrogenic Kaposi sarcoma, the prognosis is dependent on their underlying condition and their ability to tolerate a reduction in immunosuppression
- Worse prognosis is usually found in patients with visceral organ involvement, particularly the lungs
- Reference: StatPearls: Kaposi Sarcoma [Accessed 6 October 2022]
Case reports
- 23 year old HIV+ man with Kaposi sarcoma as a presentation for HIV (Cureus 2021;13:e18936)
- 28 year old HIV+ man presented with disseminated Kaposi sarcoma (Clin Pract Cases Emerg Med 2021;5:491)
- 52 year old HIV+ man presented with pulmonary Kaposi sarcoma (Int J Infect Dis 2022;115:185)
- 61 year old HIV- man presented with disseminated Kaposi sarcoma following COVID-19 (Eur J Med Res 2021;26:152)
- 74 year old HIV- woman presented with Kaposi sarcoma lesions resembling a squamous cell carcinoma or superficial basal cell carcinoma (Dermatol Online J 2020;26:13030)
Treatment
- Treatment varies depending on the clinical subtype (Am J Clin Dermatol 2017;18:529):
- AIDS related disease responds favorably to HAART in 50% of cases
- Protease inhibitors may have direct effect against Kaposi sarcoma
- Combination of HAART and chemotherapy in advanced cases
- Cutaneous lesions can be treated by local excision, liquid nitrogen and injection of vincristine (StatPearls: Kaposi Sarcoma [Accessed 6 October 2022])
- Early stage classical Kaposi sarcoma is radiosensitive
- Endemic and systemic forms are mainly treated with chemotherapy
- Treatment of iatrogenic disease must balance reduction in transplant immunosuppression with risk of transplant rejection
- AIDS related disease responds favorably to HAART in 50% of cases
Clinical images
Gross description
- Red to purple lesions
- Hemorrhagic on cut surface, especially visceral lesions
Gross images
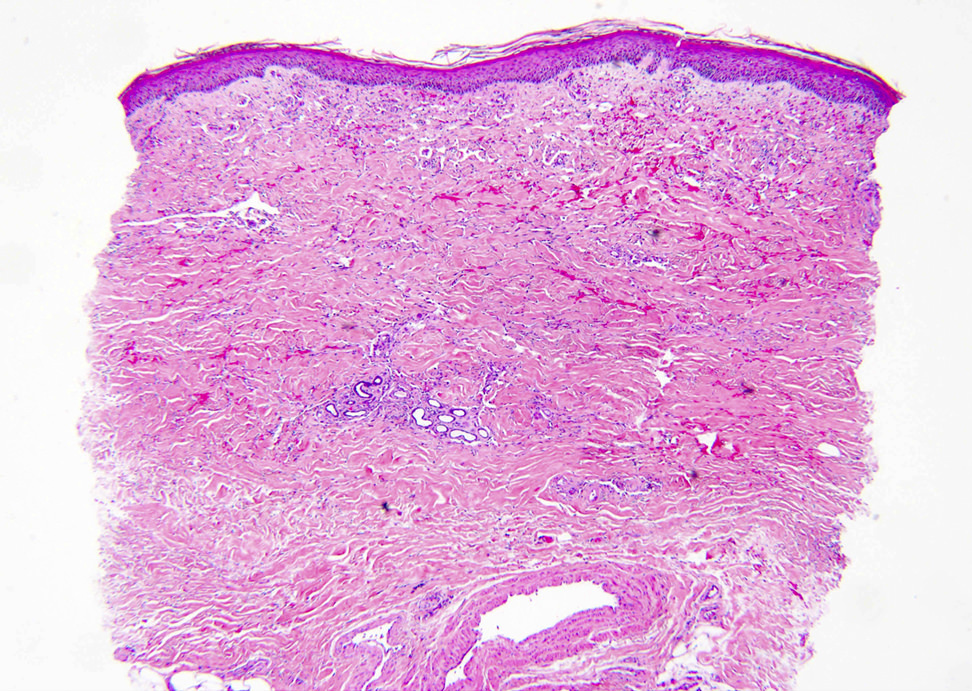
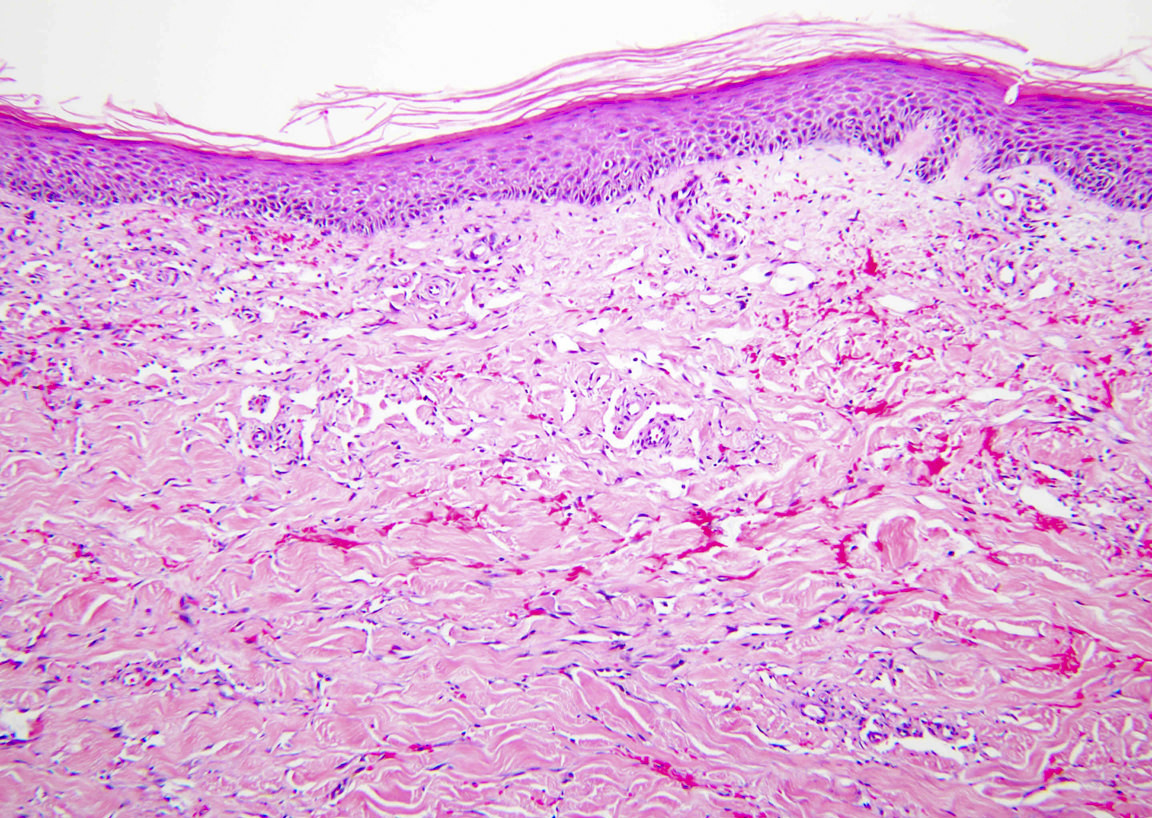
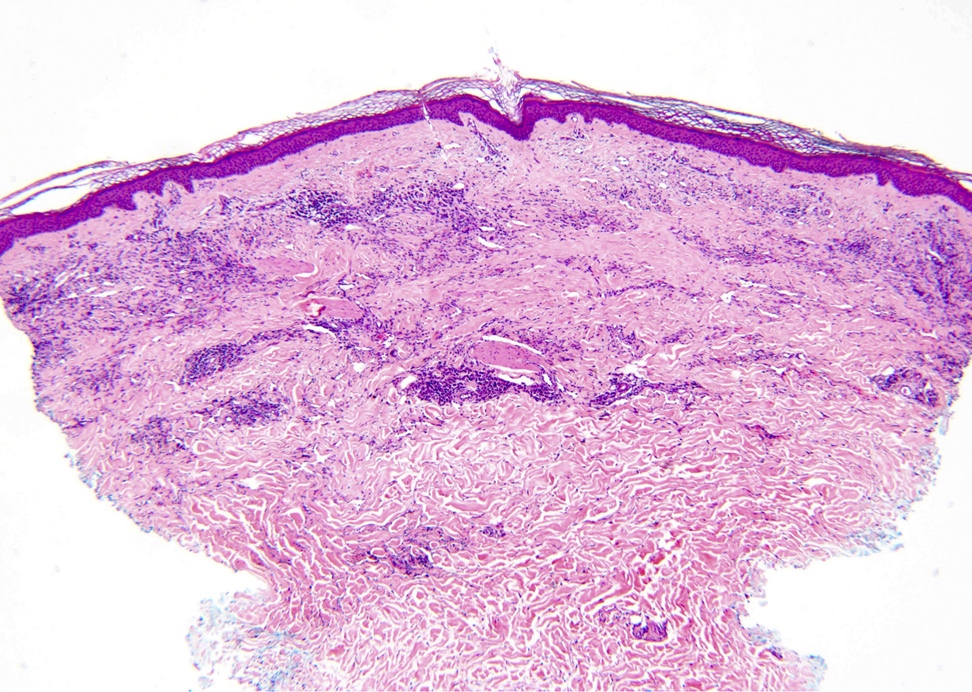
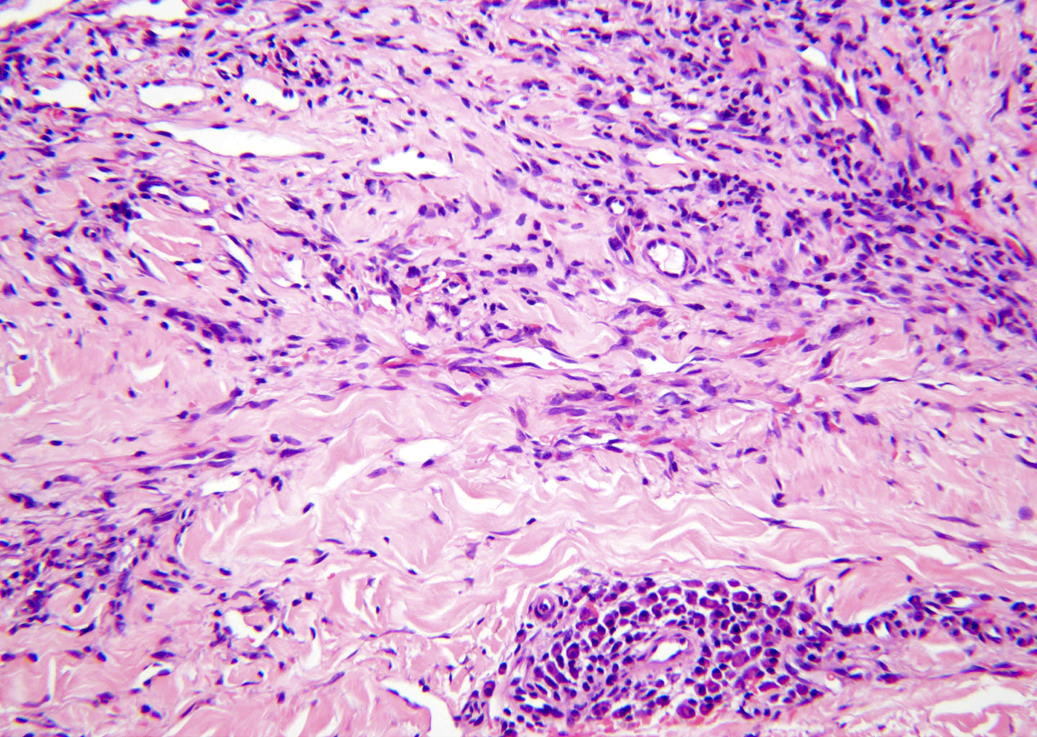
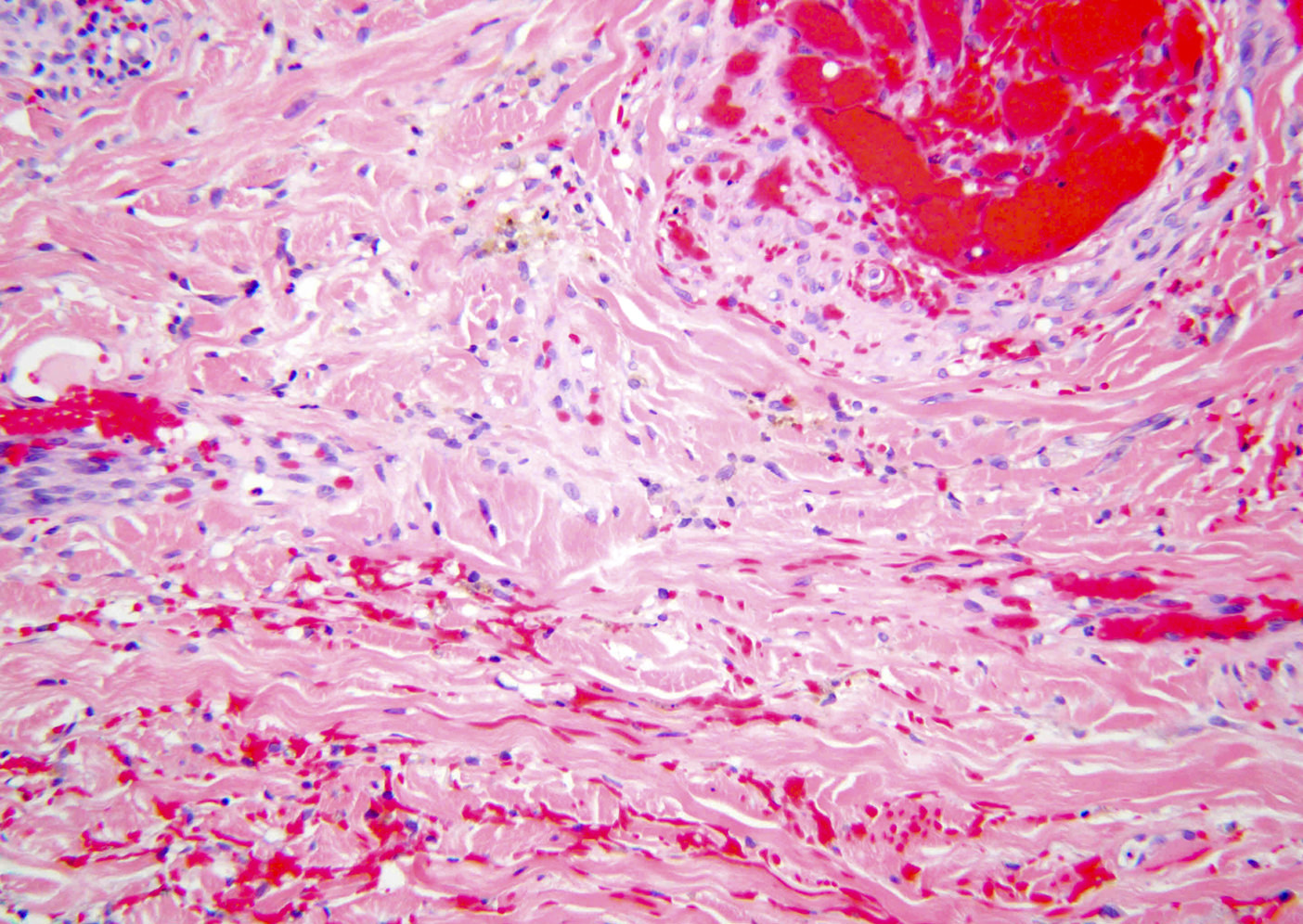
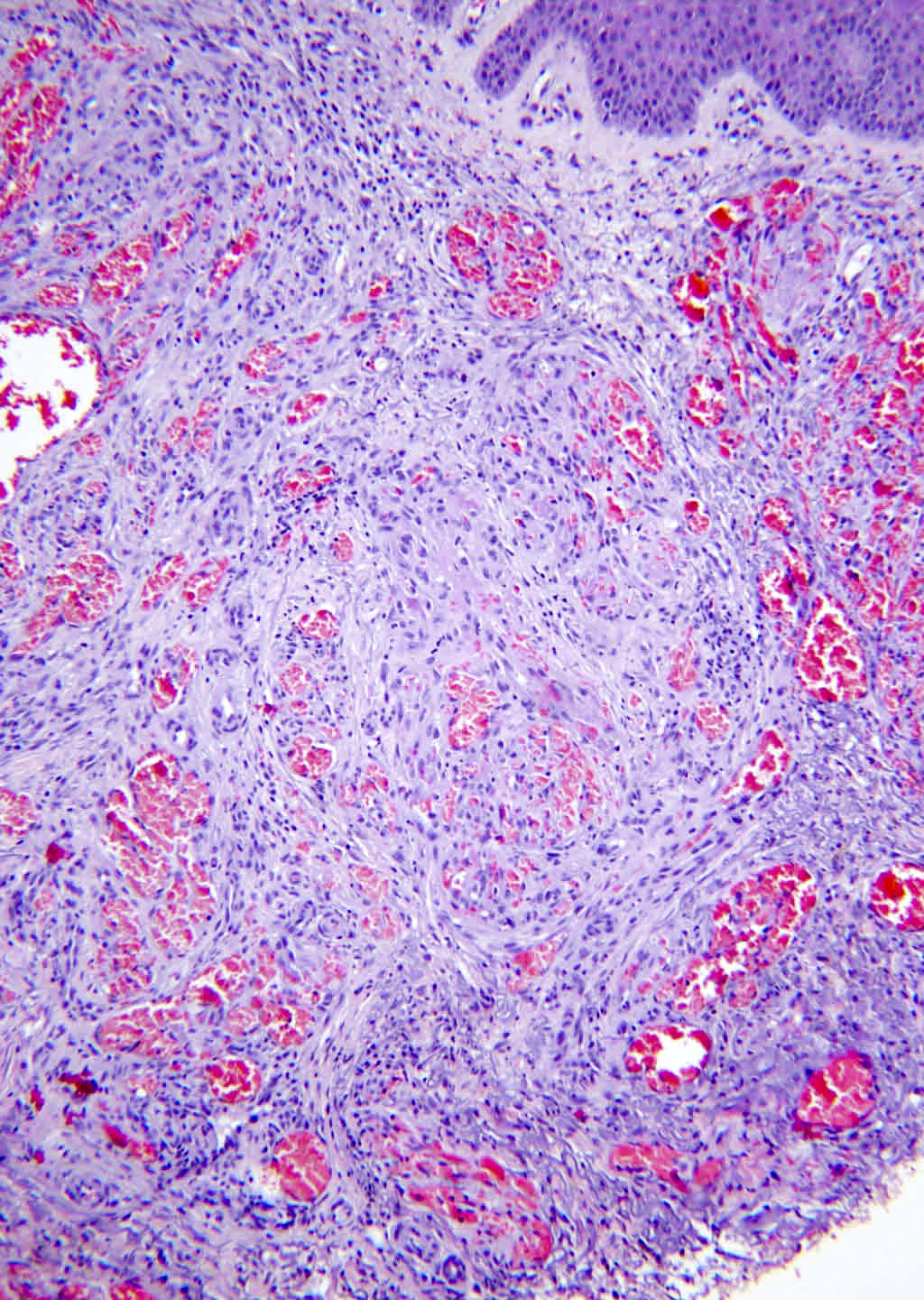
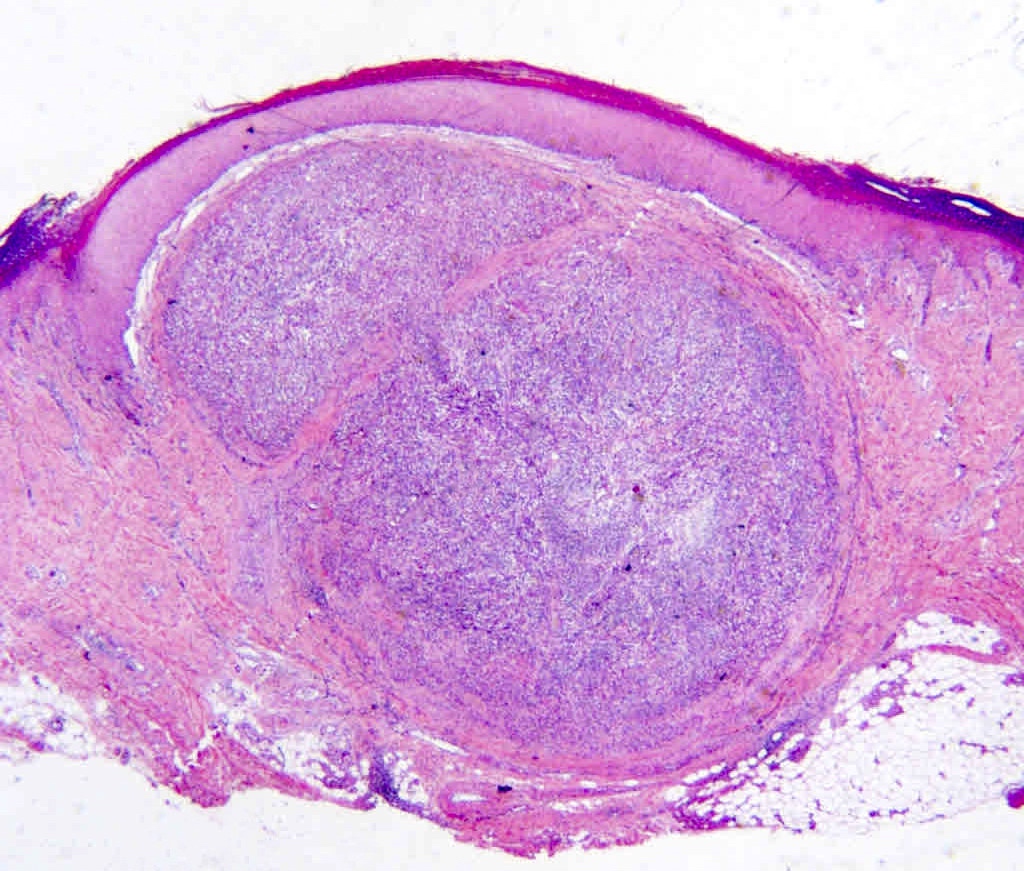
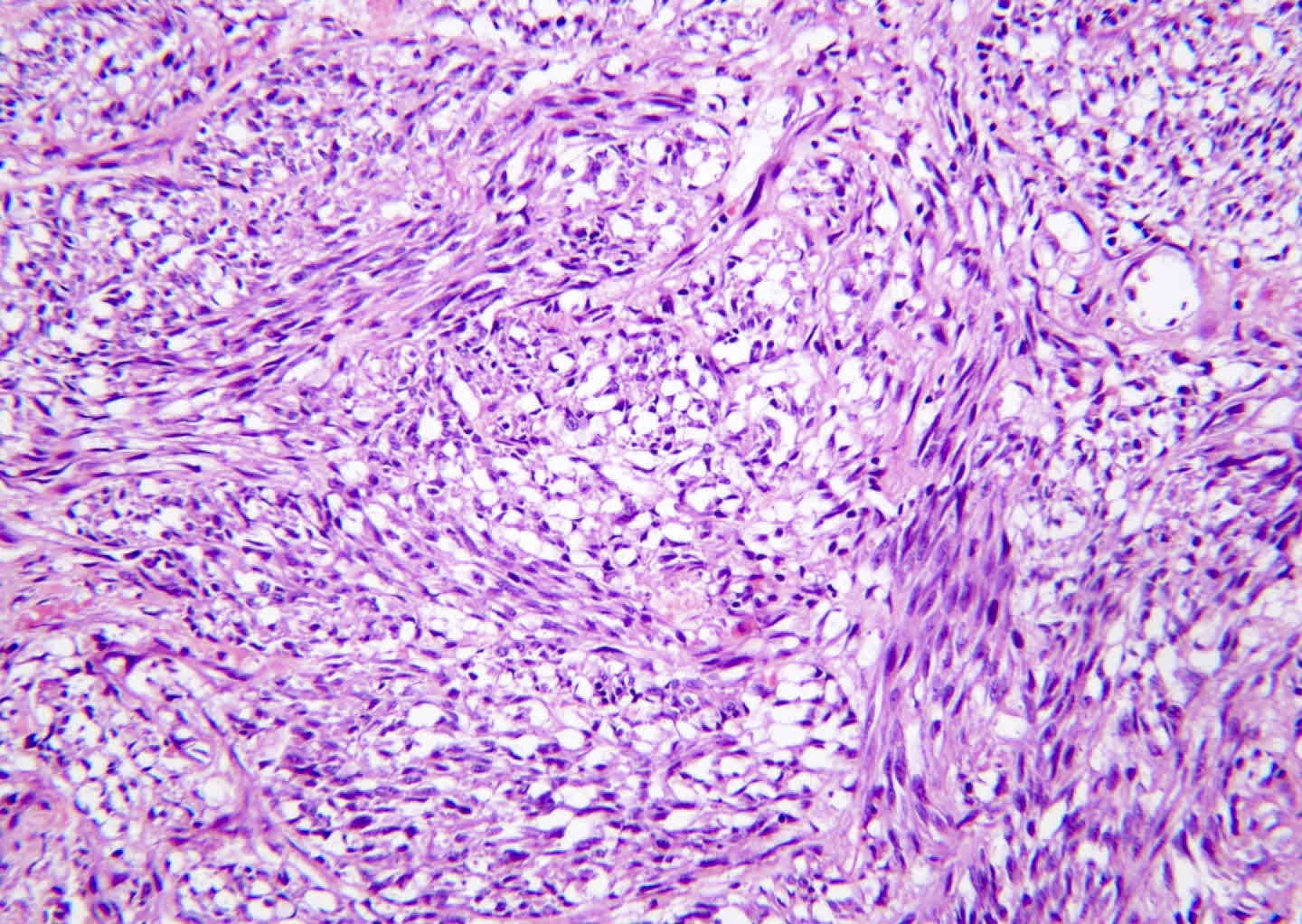
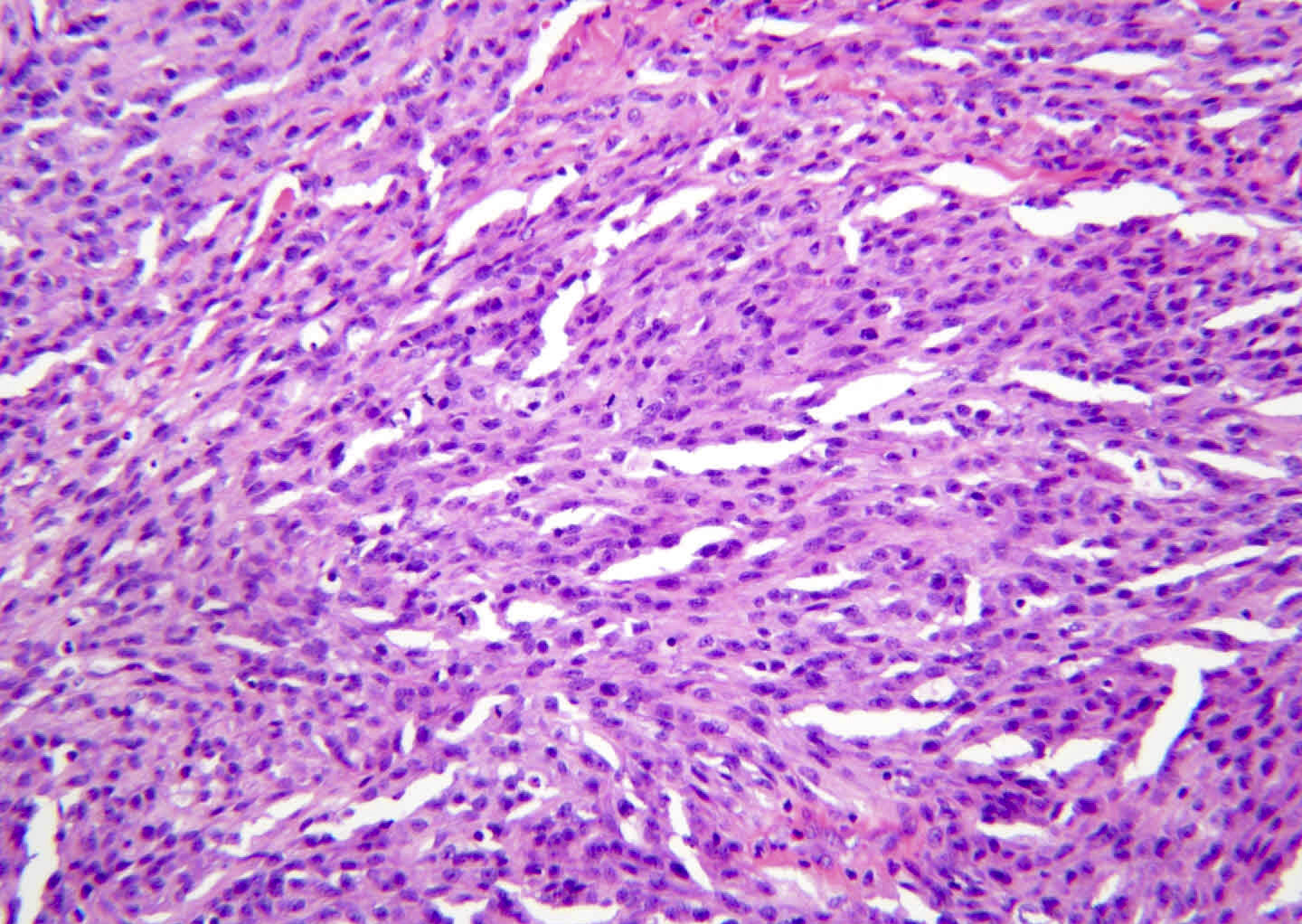
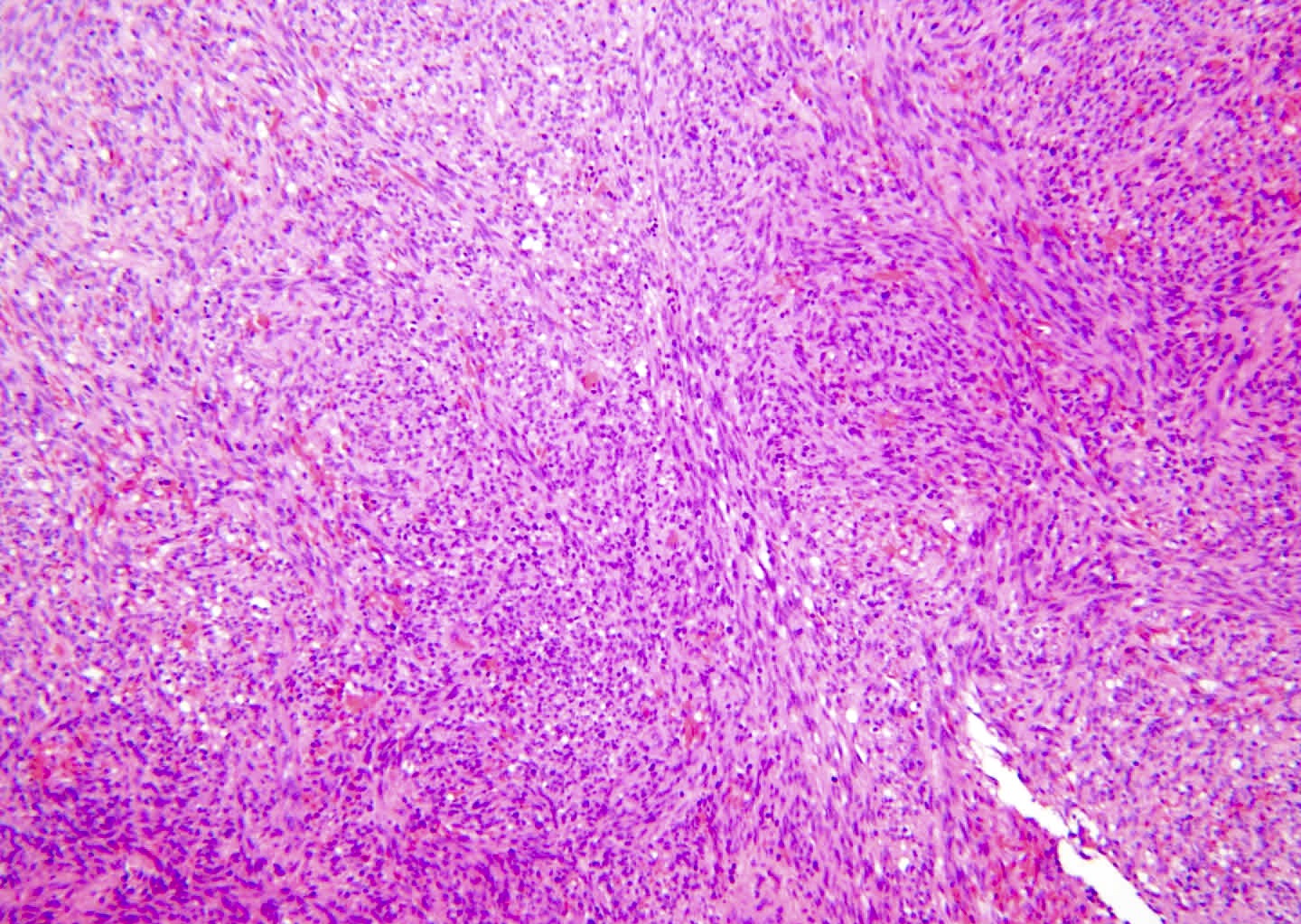
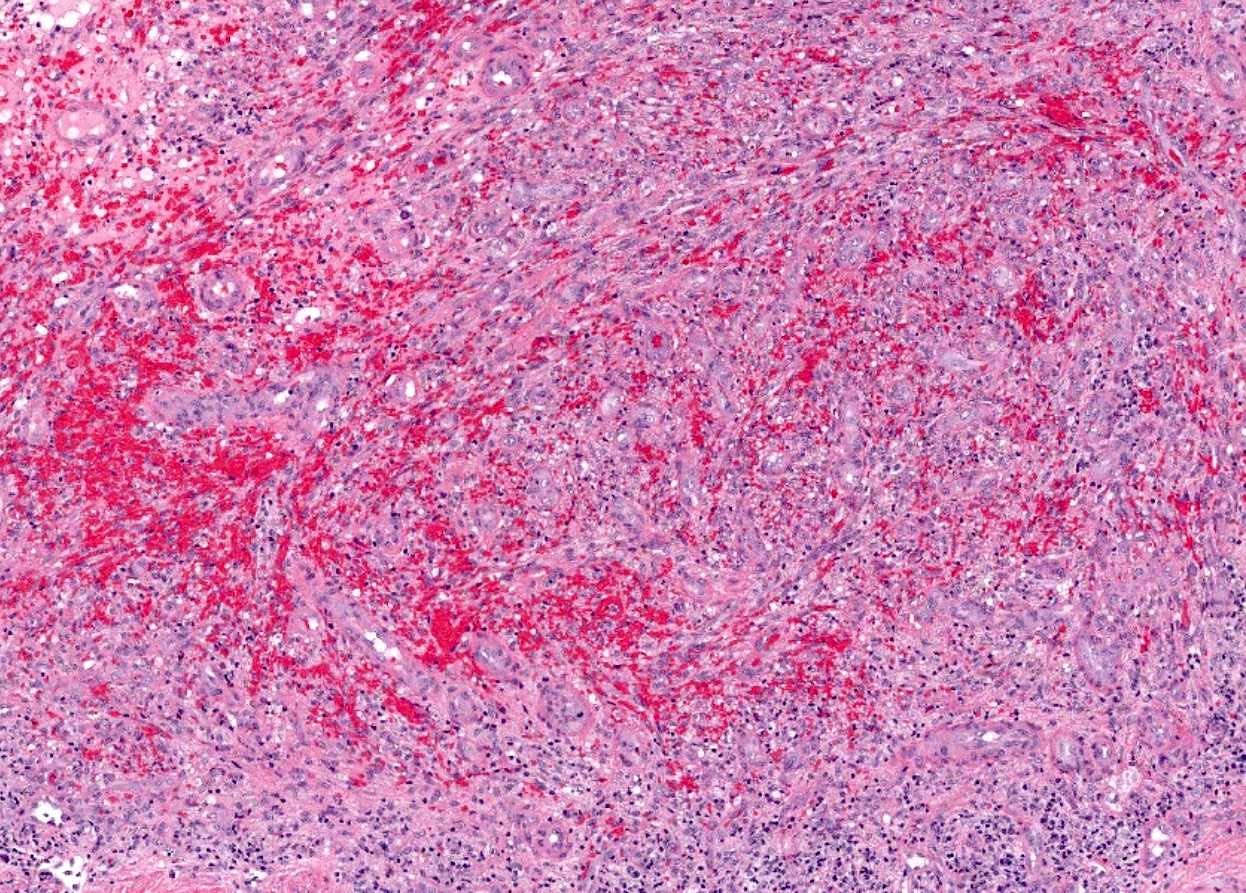
Microscopic (histologic) description
- Patch stage
- Dilated vascular channels dissecting through dermal collagen
- Promontory sign: tumor vascular channels surround and entrap native vessels (classic but uncommon feature)
- May be very subtle in early lesions
- Dilated vascular channels dissecting through dermal collagen
- Plaque stage
- More extensive, compressed, slit-like vascular channels infiltrating deeper dermis
- Infiltrative proliferation of spindled endothelial cells (may resemble fibroblasts)
- Spindle cells infiltrating and destroying eccrine coils is very characteristic
- Tumor (nodular) stage
- Discrete nodules composed of intersecting fascicles of uniform spindle cells
- Intervening blood filled spaces between spindle cells
- Slit-like spaces (longitudinal section)
- Sieve-like spaces (cross section)
- Intracytoplasmic hyaline globules may be seen
- All stages
- Mitoses are common but pleomorphism is usually minimal
- Rare poorly differentiated cases may have severe pleomorphism; it's important to confirm the diagnosis with HHV8 IHC in order to exclude angiosarcoma
- Extravasated erythrocytes and hemosiderin deposits are common
- Plasma cells are present in most cases
- Mitoses are common but pleomorphism is usually minimal
- Distinction of stage is not required in pathology report (Arch Pathol Lab Med 2013;137:289)
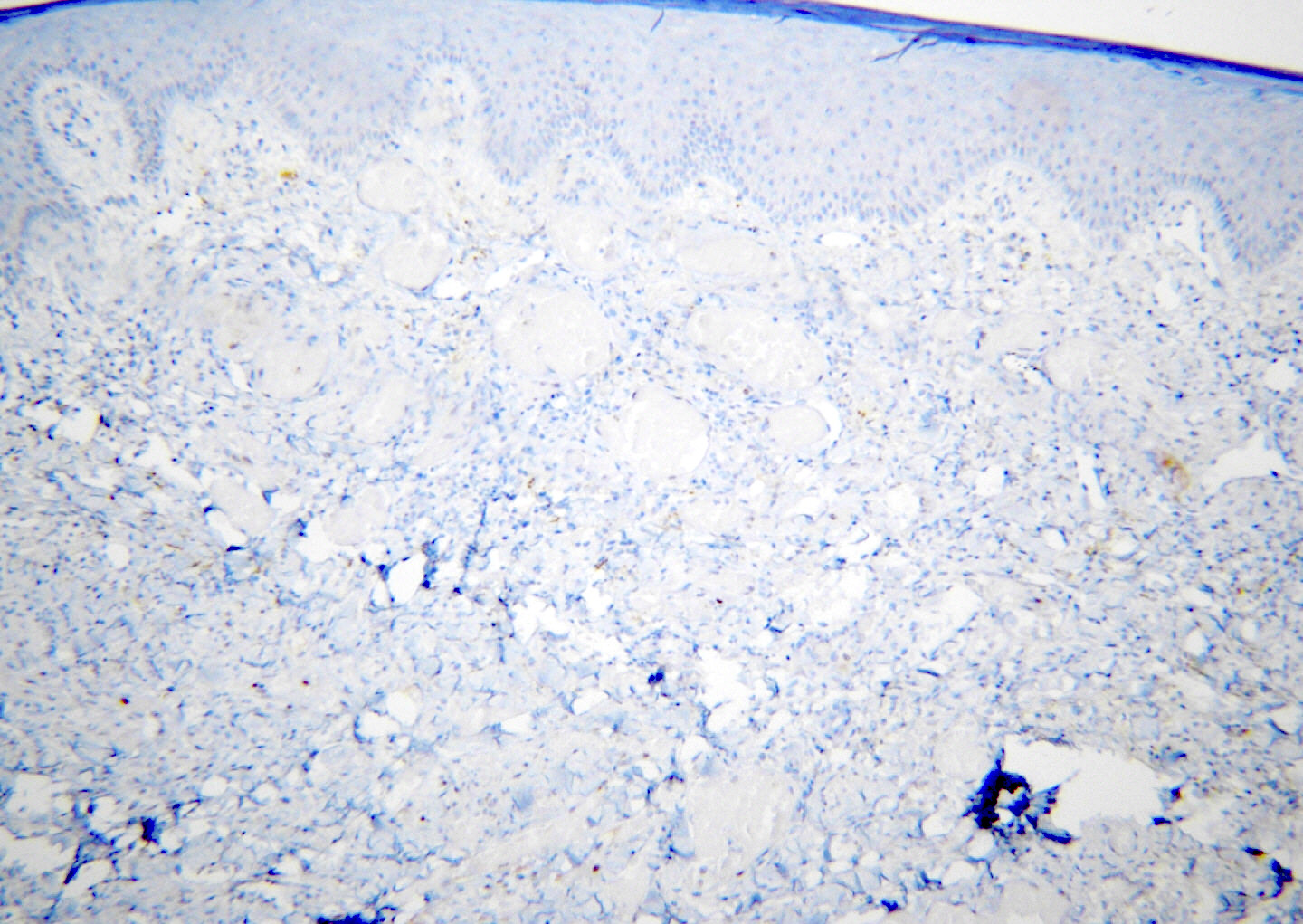
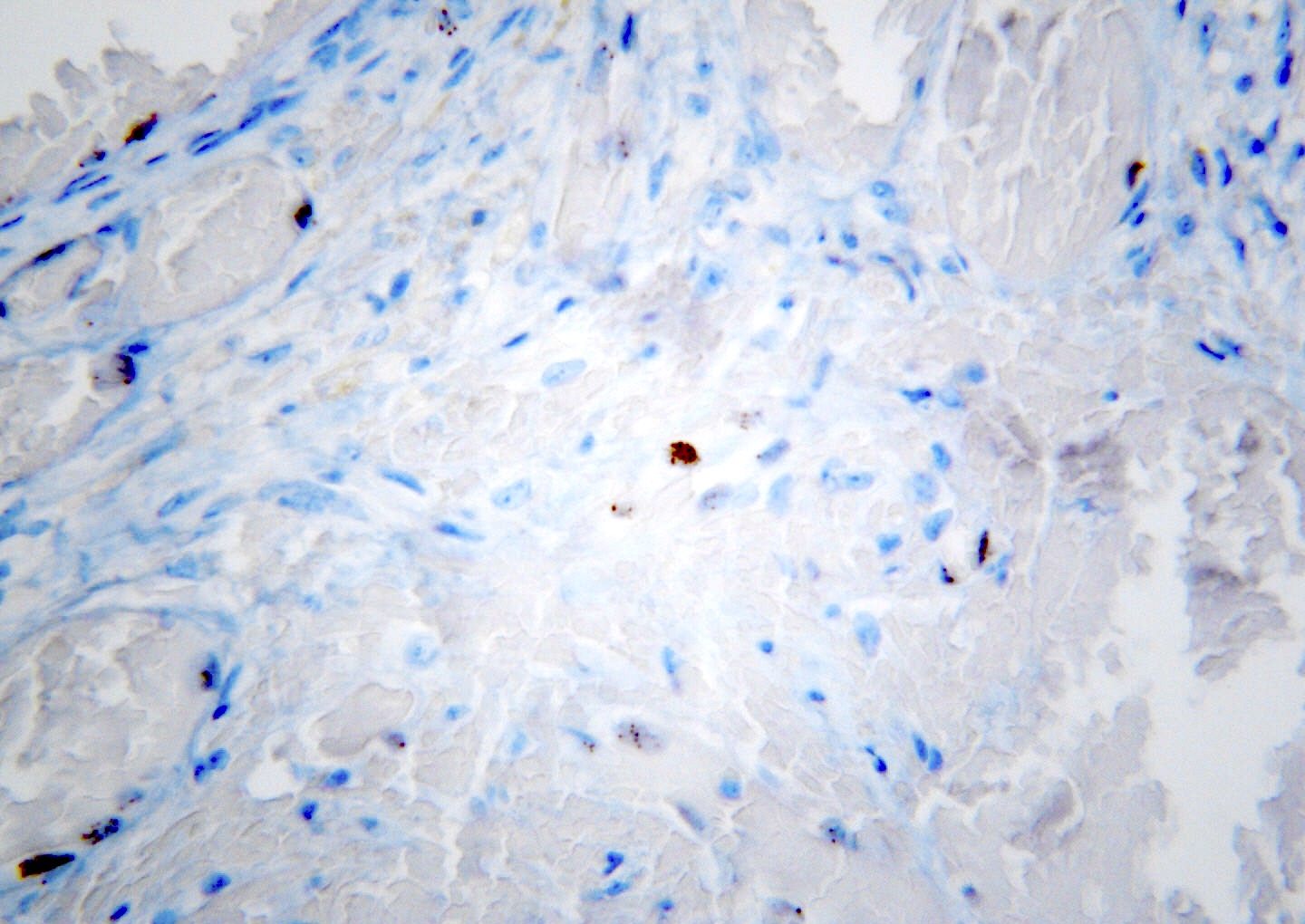
Microscopic (histologic) images
Contributed by Michella Whisman, M.D. and Mark R. Wick, M.D.
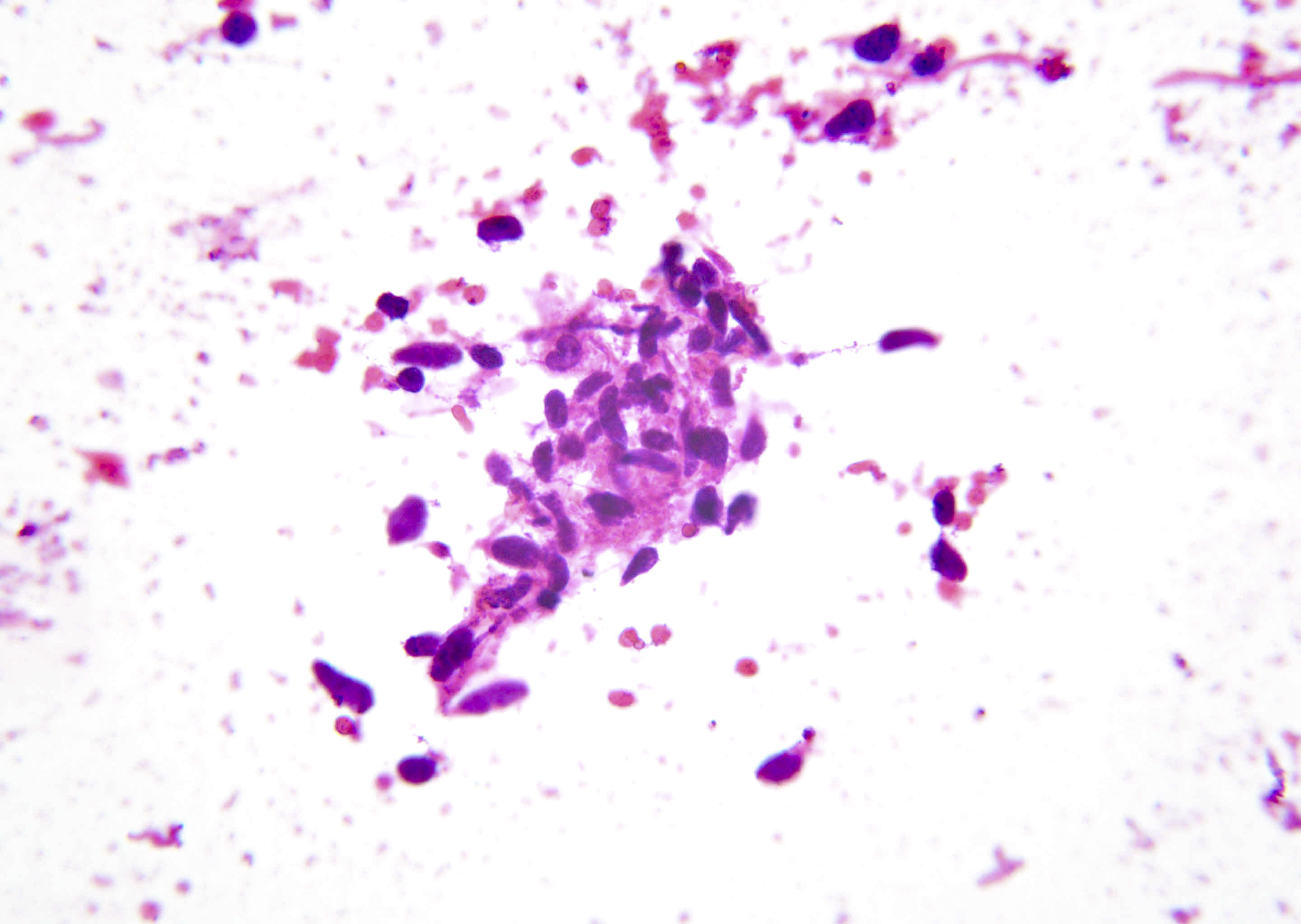
Cytology description
- Cohesive spindle cells in hemorrhagic background (Arch Pathol Lab Med 2013;137:289)
Positive stains
- HHV8 (also referred to as LANA1) nuclear staining in virtually 100% of cases
- May be focal, especially in early patch stage lesions
- Typically has unique granular / speckled / stippled nuclear staining pattern
- ERG, CD34, CD31, D2-40 (Am J Surg Pathol 2011;35:432)
- Subset of cases lack CD31 expression (Arch Pathol Lab Med 2012;136:1329)
- Hyaline globules are PAS positive, diastase resistant
Negative stains
Videos
Kaposi sarcoma:
5 minute pathology pearls
Sample pathology report
- Skin, left lower leg, shave biopsy:
- Kaposi sarcoma (see comment)
- Comment: Histologic sections contain a dermal based neoplasm composed of sheets of uniform, relatively bland spindle cells with poorly formed slit-like vascular channels. There is extensive extravasation of red blood cells. Mitotic activity is conspicuous and no tumor necrosis is identified. Immunohistochemical stains show diffuse reactivity for ERG and HHV8.
Differential diagnosis
- Angiosarcoma:
- Infiltrative vascular channels, usually with marked nuclear atypia
- HHV8 negative
- Most common sites include the head / neck of elderly patients and previously irradiated sites (most commonly breast)
- Visceral lesions have a dismal prognosis
- Severe vascular stasis (acroangiodermatitis):
- Fibroblastic spindle cell component rather than endothelial
- Negative for vascular markers
- HHV8 negative
- Hobnail hemangioma (targetoid hemosiderotic hemangioma):
- Slit-like vascular channels but no spindle cell proliferation
- HHV8 negative
- Spindle cell hemangioma:
- Spindled endothelial cells with slit-like channels but also has epithelioid cells
- Biphasic: solid spindled / epithelioid zone and zone of dilated cavernous vessels
- Usually lacks plasma cells and hemorrhage
- HHV8 negative
- Kaposiform hemangioendothelioma:
Practice question #1
Practice answer #1
C. The tumor is Kaposi sarcoma, which is caused by HHV8. HHV8 may also lead to primary effusion lymphoma and multicentric Castleman disease. Merkel cell carcinoma is caused by polyomavirus. Burkitt lymphoma can be associated with EBV. Adult T cell leukemia is associated with HTLV1.
Comment Here
Reference: Kaposi sarcoma
Comment Here
Reference: Kaposi sarcoma
Practice question #2
Practice answer #2
A. Enveloped, double stranded DNA virus. The HHV8 virus is an enveloped, double stranded DNA virus.
Comment Here
Reference: Kaposi sarcoma
Comment Here
Reference: Kaposi sarcoma