Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Obeidin F, Alexiev B. Pseudomyogenic hemangioendothelioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuepseudomyogenichemangio.html. Accessed September 2nd, 2025.
Definition / general
- Rarely metastasizing vascular tumor with histology mimicking a myoid tumor or epithelioid sarcoma
Essential features
- Locally aggressive but rarely metastasizing vascular tumor occurring most commonly in young adults < 40 years old
- Histology: fascicles or sheets of plump spindled to epithelioid cells with bright eosinophilic cytoplasm
- Immunohistochemistry: keratin+, ERG+, FLI1+, CD31+, FOSB+, CAMTA1-, INI1 retained
- Molecular: t(7;19) SERPINE1-FOSB
Terminology
- Synonyms: epithelioid sarcoma-like hemangioendothelioma, fibroma-like variant of epithelioid sarcoma
ICD coding
- ICD-10: D49.2 - neoplasm of unspecified behavior of bone, soft tissue and skin
Epidemiology
- Mean age: 31 years old; 82% ≤ 40 years old
- Male predominance (M:F = 4.6:1) (Am J Surg Pathol 2011;35:190)
Sites
- Most common location is the lower extremities
- Lower limbs: 54%
- Upper limbs: 24%
- Trunk: 18%
- Head and neck: 4%
- Often multifocal (~67% of reported cases)
- Tissues affected (Am J Surg Pathol 2011;35:190)
- Dermis: 31%
- Subcutaneous tissue: 20%
- Muscle: 34%
- Bone: 14%
- Tumors with only bone involvement have similar demographics (BMC Cancer 2019;19:872)
Pathophysiology / etiology
- Driven by overexpression of FOSB, a protein involved in the AP-1 transcription complex that plays a role in cell growth and proliferation, cellular differentiation and apoptosis
- SERPINE1 is highly expressed in vascular tissues and acts as the promoter for FOSB expression when fused (Cancer Genet 2011;204:211)
Clinical features
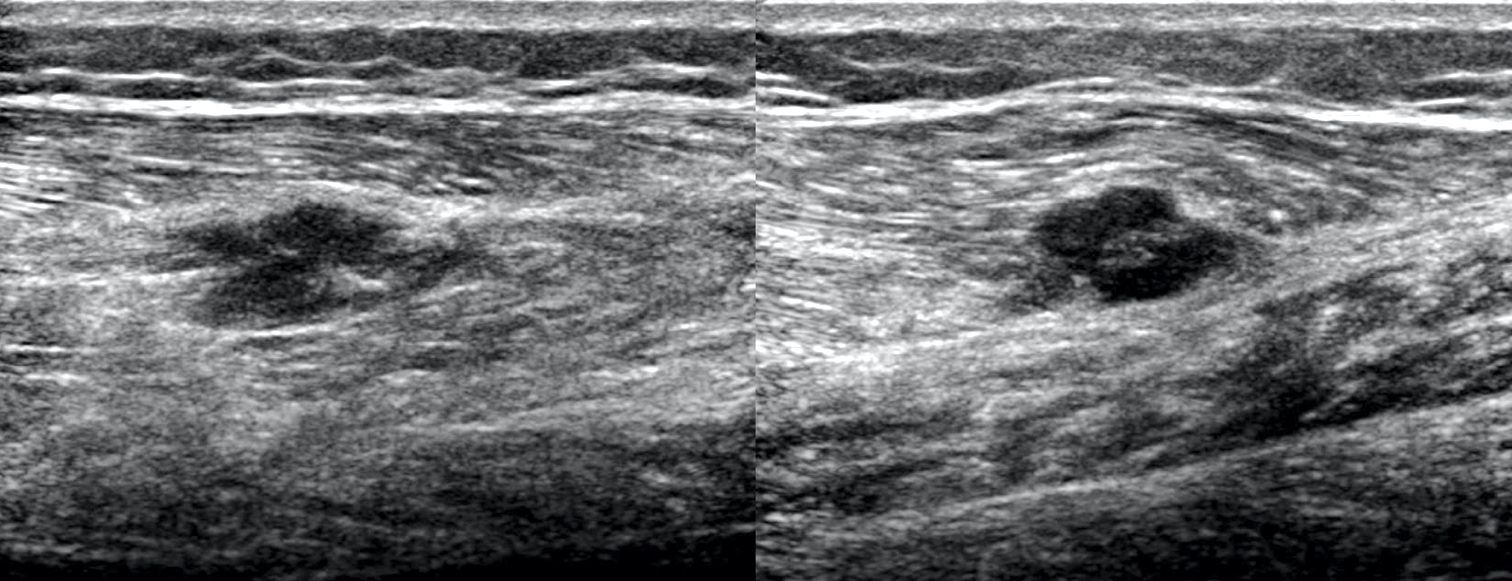
- Half present as painful and half as painless nodules
- 58% with local recurrence; only rarely metastasizes (Am J Surg Pathol 2011;35:190)
Diagnosis
- Evaluate soft tissue masses with CT or MRI imaging followed by imaging guided biopsy
- Diagnosis typically made on biopsy prior to definitive surgical treatment or adjuvant therapy
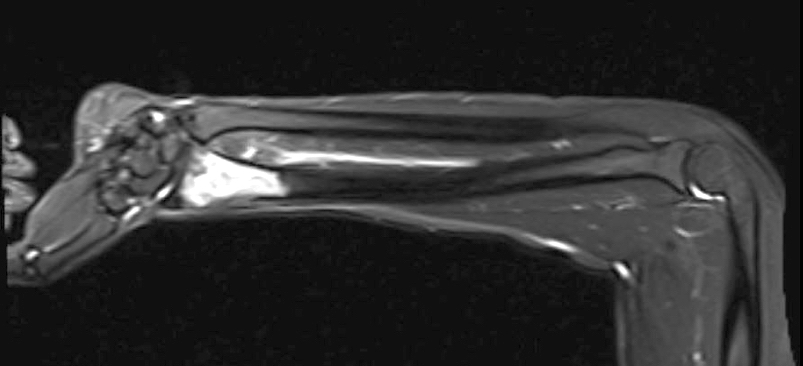
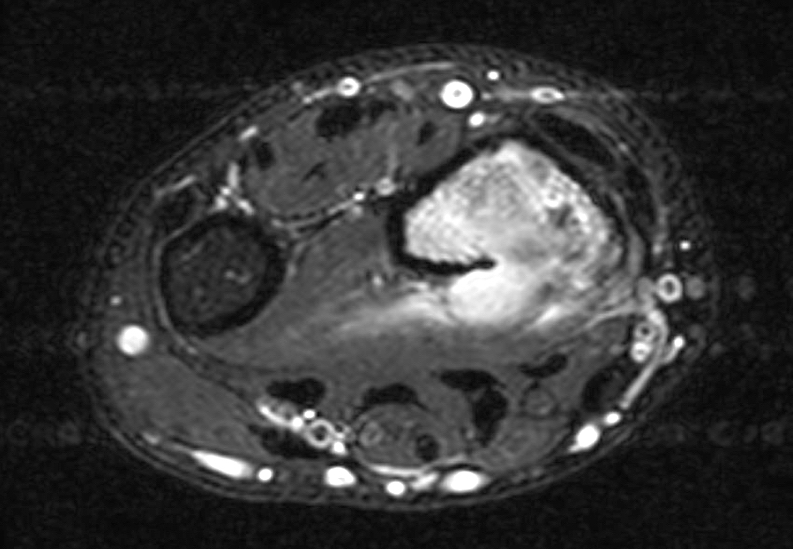
Radiology description
- Xray and CT: lytic, lobulated and well defined lesion
- MRI:
- Hypo to isointense on T1 weighted imaging
- Variably hyperintense on T2 and STIR weighted imaging
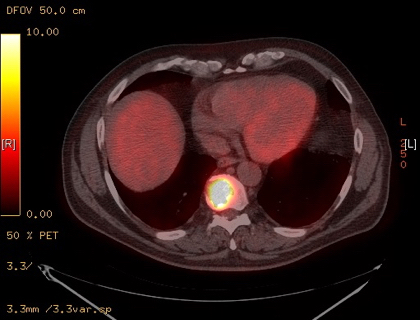
- Fluorodeoxyglucose (FDG) and methylene diphosphonate (MDP) avidity variable but may be used to follow for regression (Radiol Case Rep 2019;14:1228, Am J Surg Pathol 2016;40:587)
Radiology images
Prognostic factors
- Multifocality, age at presentation, gender and size may be prognostic but more studies are needed (Arch Pathol Lab Med 2019;143:763)
Case reports
- 14 year old girl with a history of fibrous dysplasia presenting with swelling over the left tibia and calcaneus (World J Surg Oncol 2016;14:198)
- 17 year old boy with multiple subcutaneous nodular lesions over the left leg and foot (Indian J Pathol Microbiol 2016;59:382)
- 20 year old woman with left ankle pain and a lytic bone lesion (BMC Cancer 2019;19:872)
- 43 year old woman with left breast pain and a breast mass (Diagn Pathol 2019;14:79)
- 51 year old woman with multiple vulvar nodules (Diagn Pathol 2019;14:66)
- 63 year old man with a sacral mass (Radiol Case Rep 2019;14:1228)
Treatment
- Optimal treatment still unclear due to rarity
- Wide excision is recommended as first line ± adjuvant radio or chemotherapy because of the high risk of local recurrence
- Amputation may be needed in rare progressive cases (Am J Surg Pathol 2011;35:190)
- Responses have been seen in isolated case reports with gemcitabine / taxane cytotoxic chemotherapy or mTOR inhibitors (everolimus, sirolimus) (Clin Sarcoma Res 2015;5:22, Pediatr Blood Cancer 2018;65:1)
- Complete response to telatinib in one case report; other VEGFR / PDGFR inhibitors have been proposed as well (Clin Cancer Res 2018;24:2678)
Gross description
- Ill defined, usually multifocal
- White-brown cut surface, rarely with necrosis or hemorrhage
- Most tumors are 1 - 2.5 cm; mean size: 1.9 cm (Am J Surg Pathol 2011;35:190)
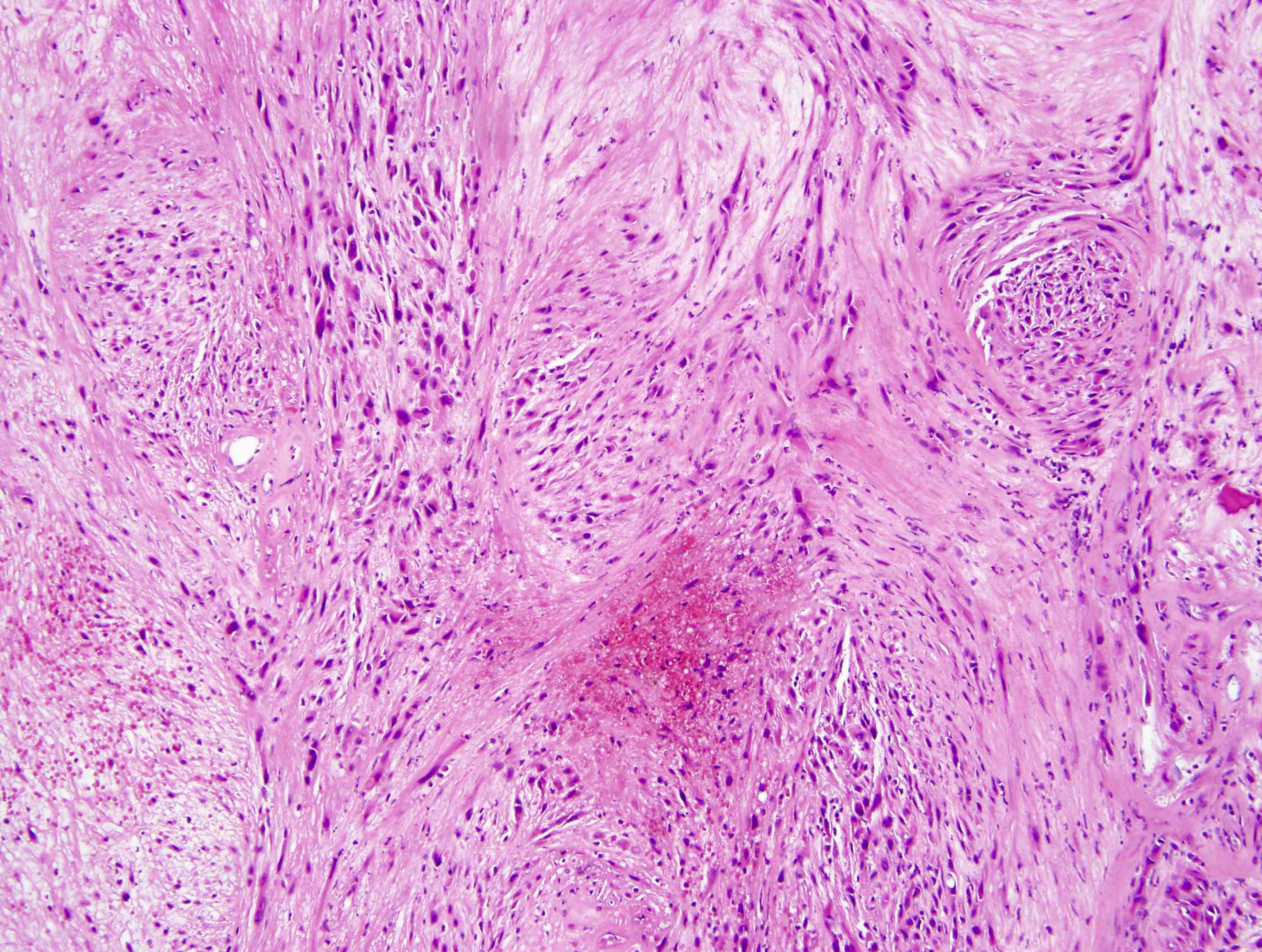
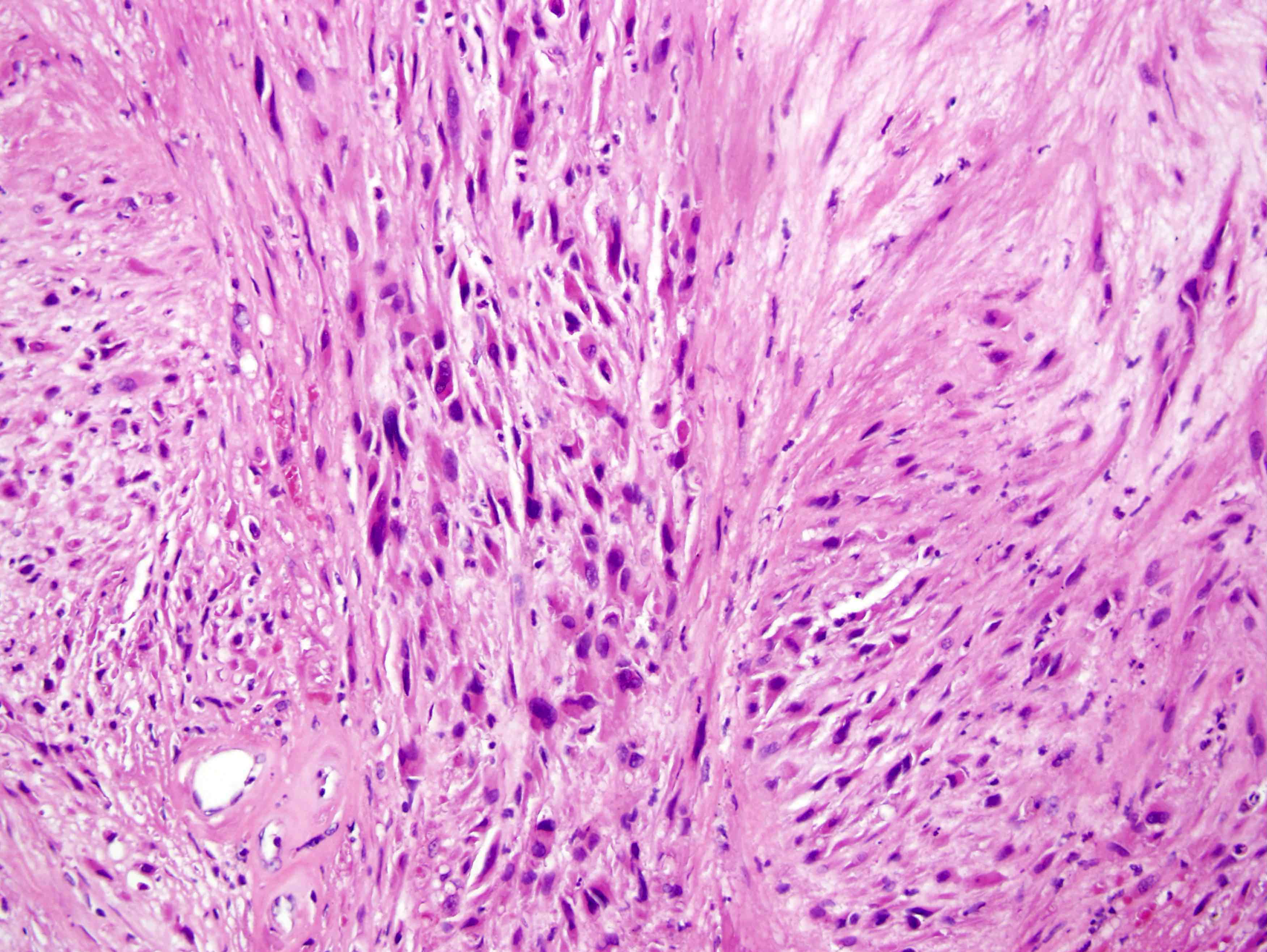
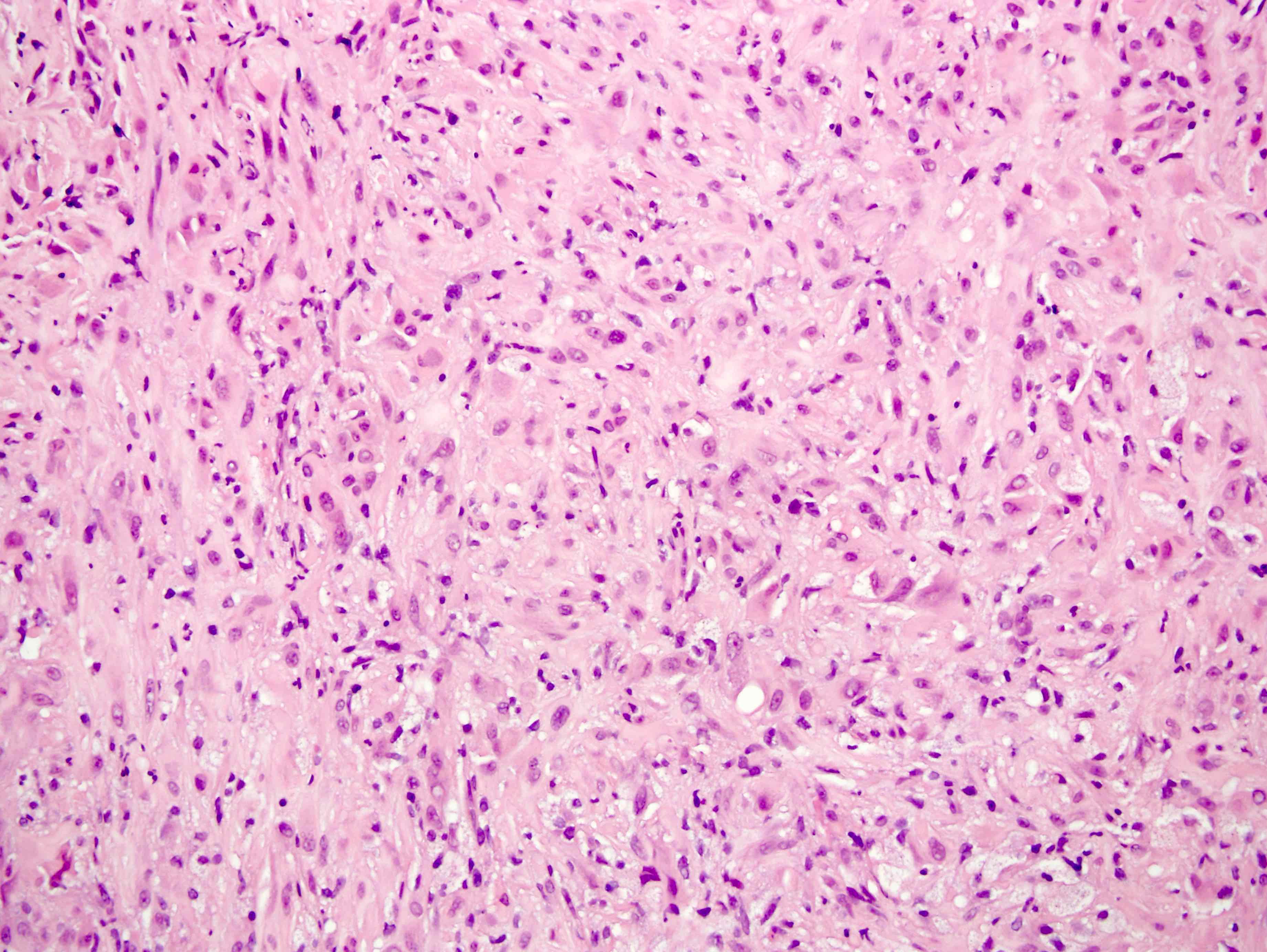
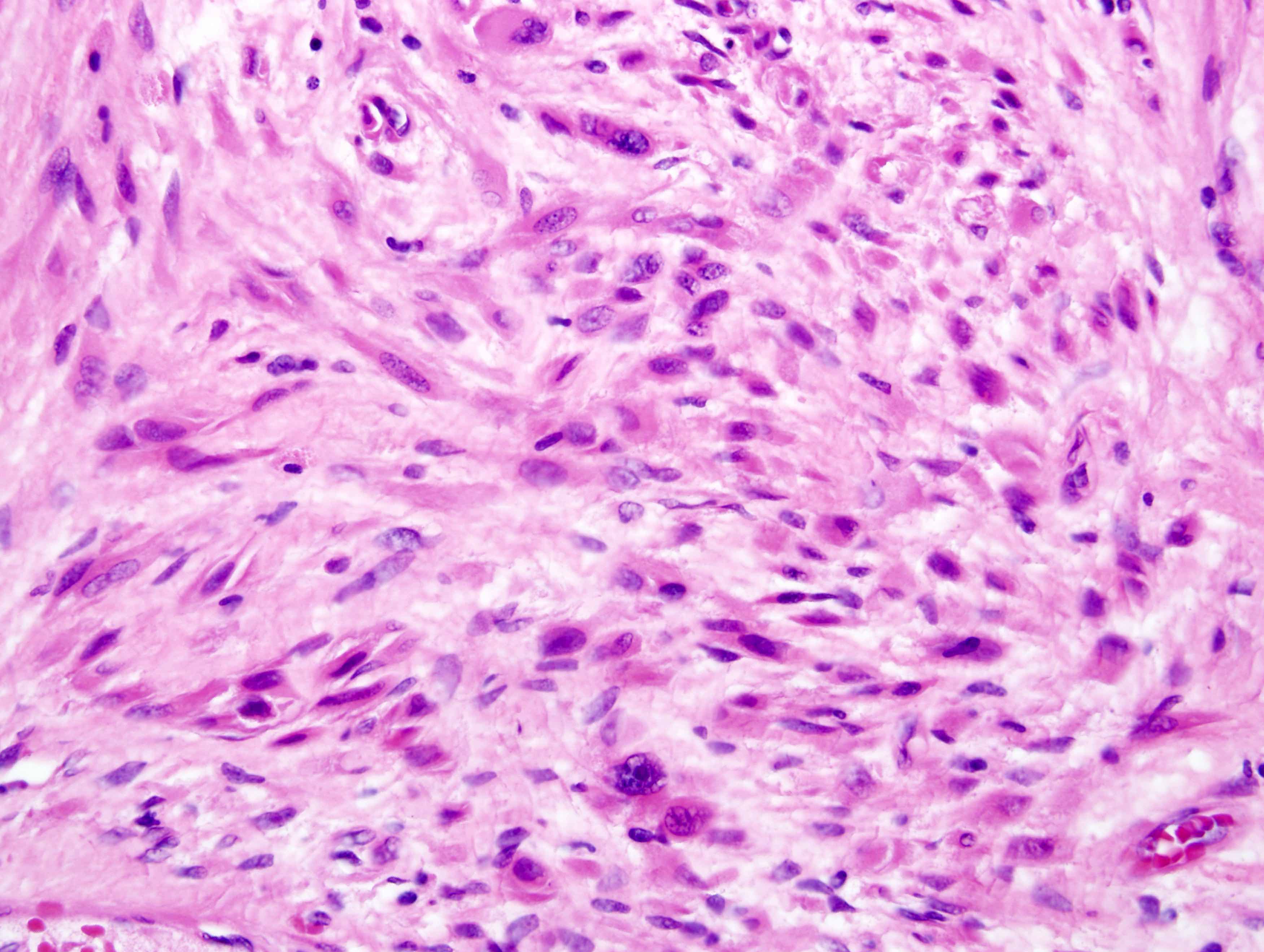
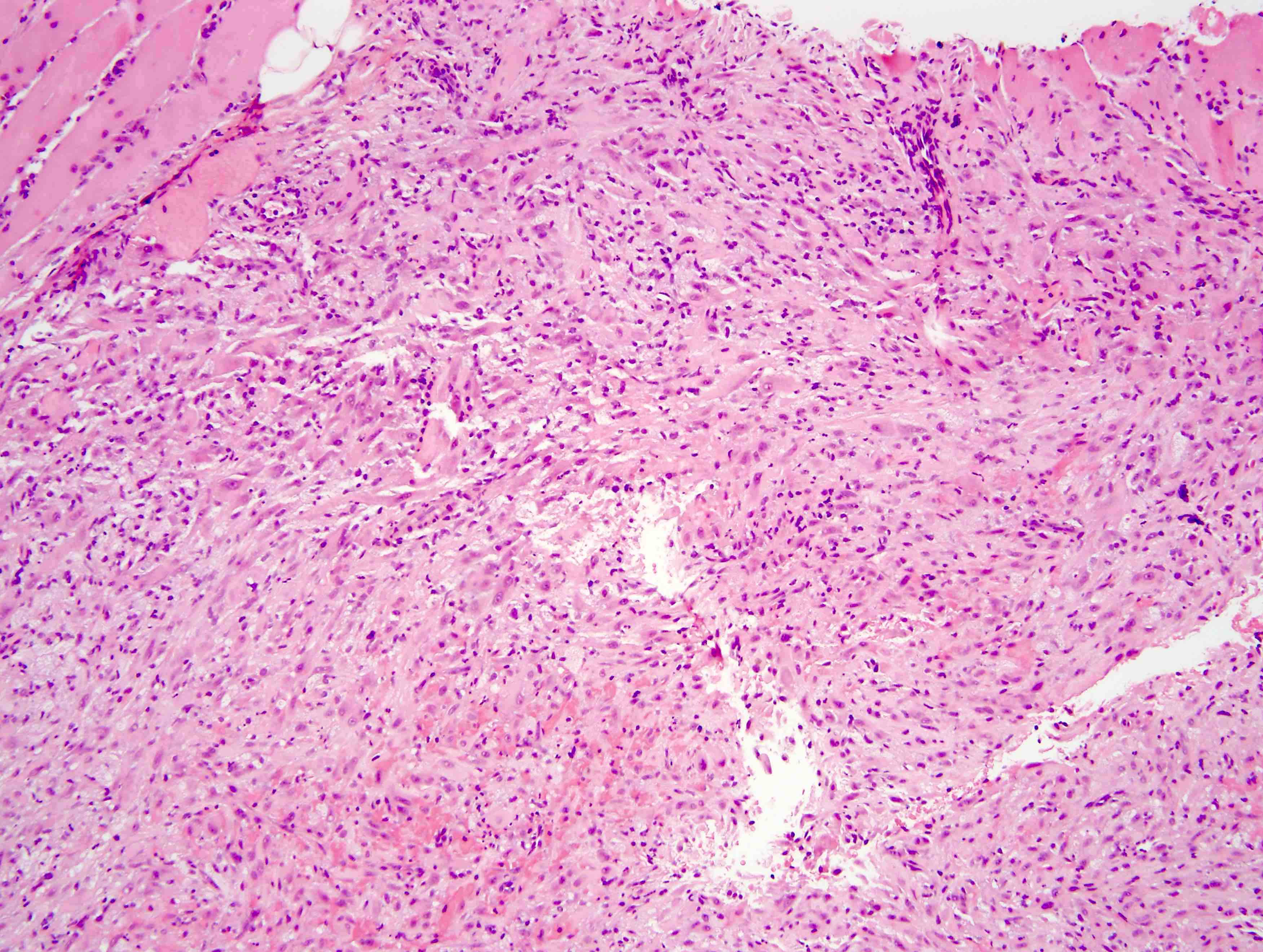
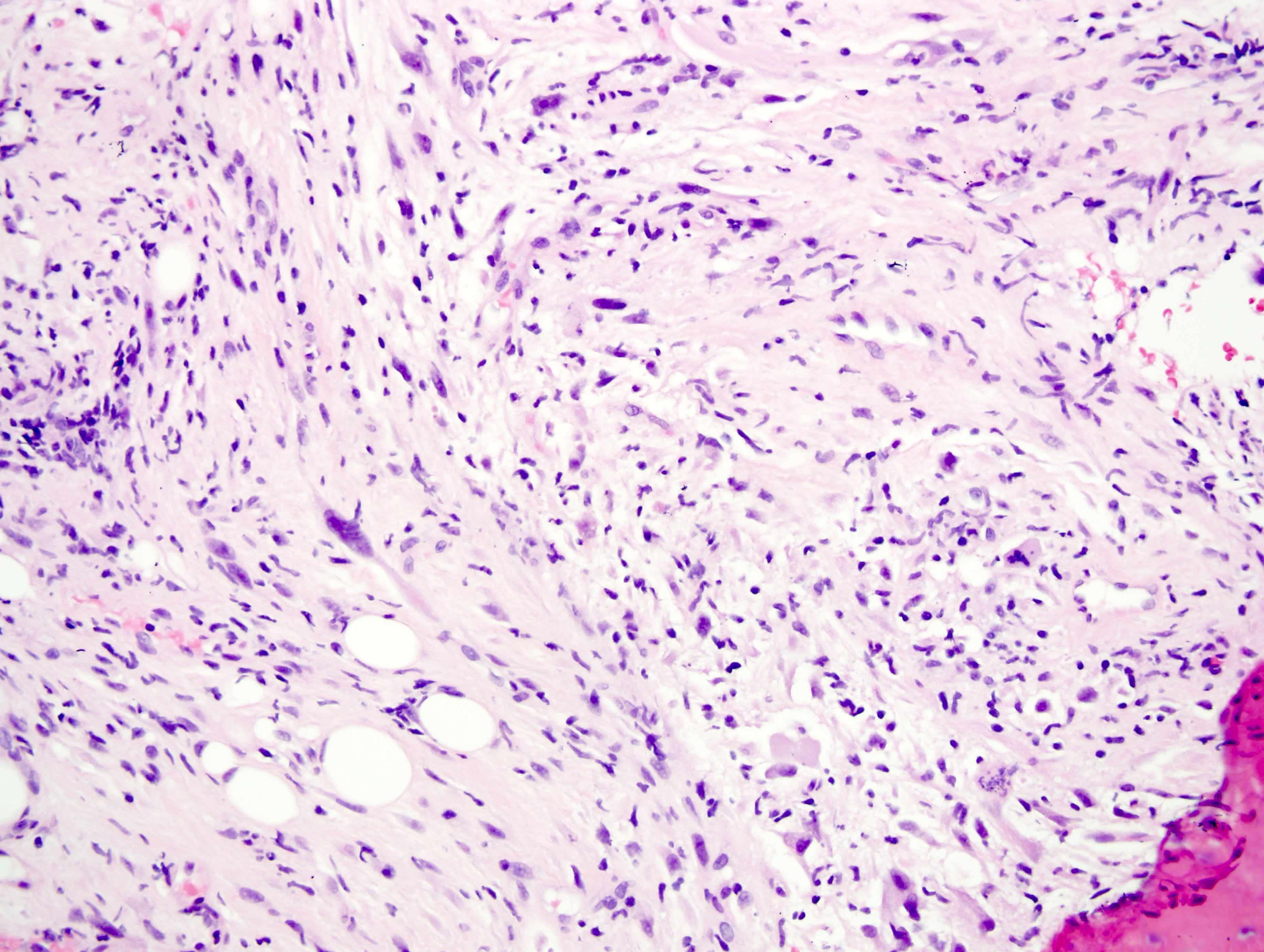
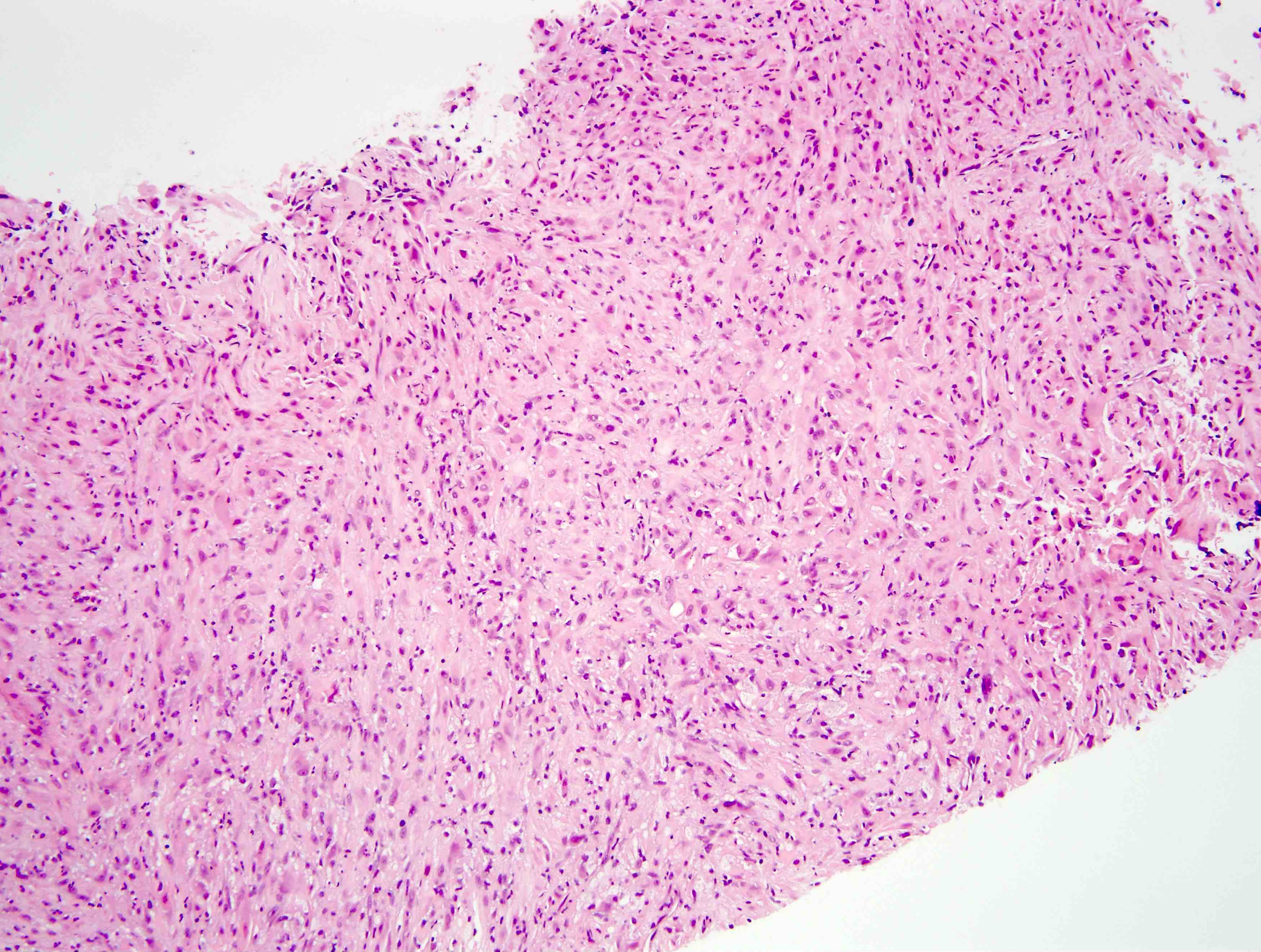
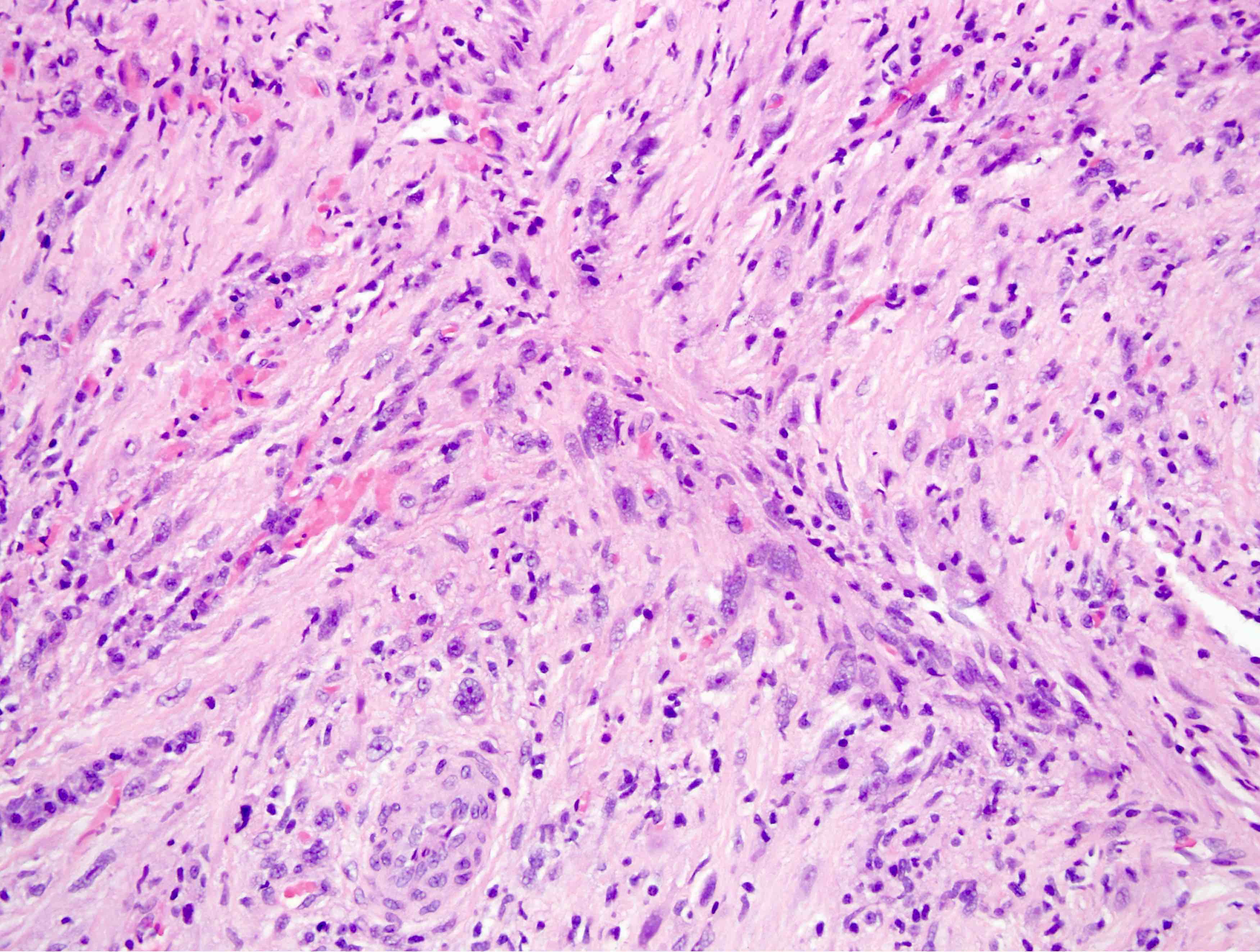
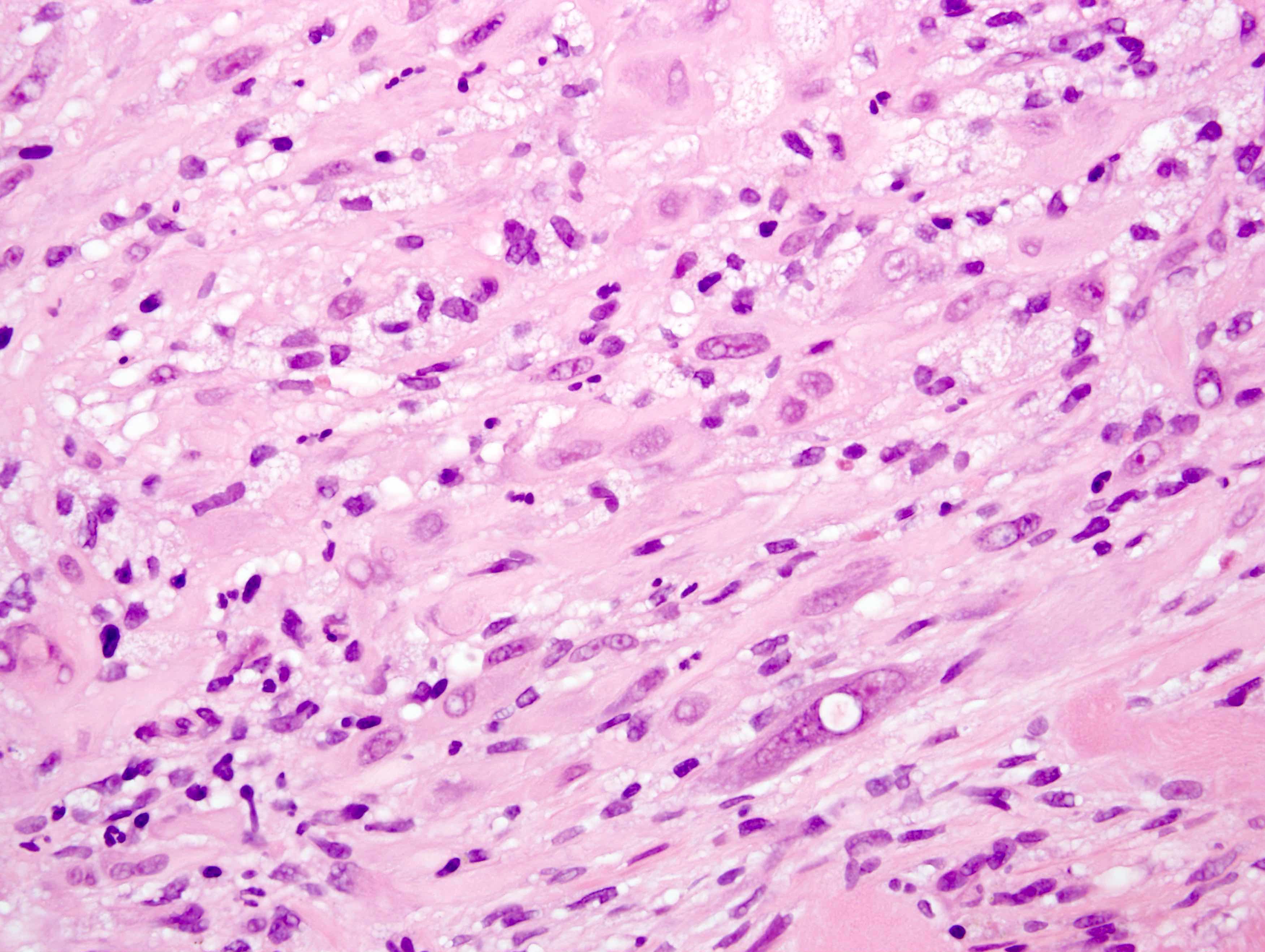
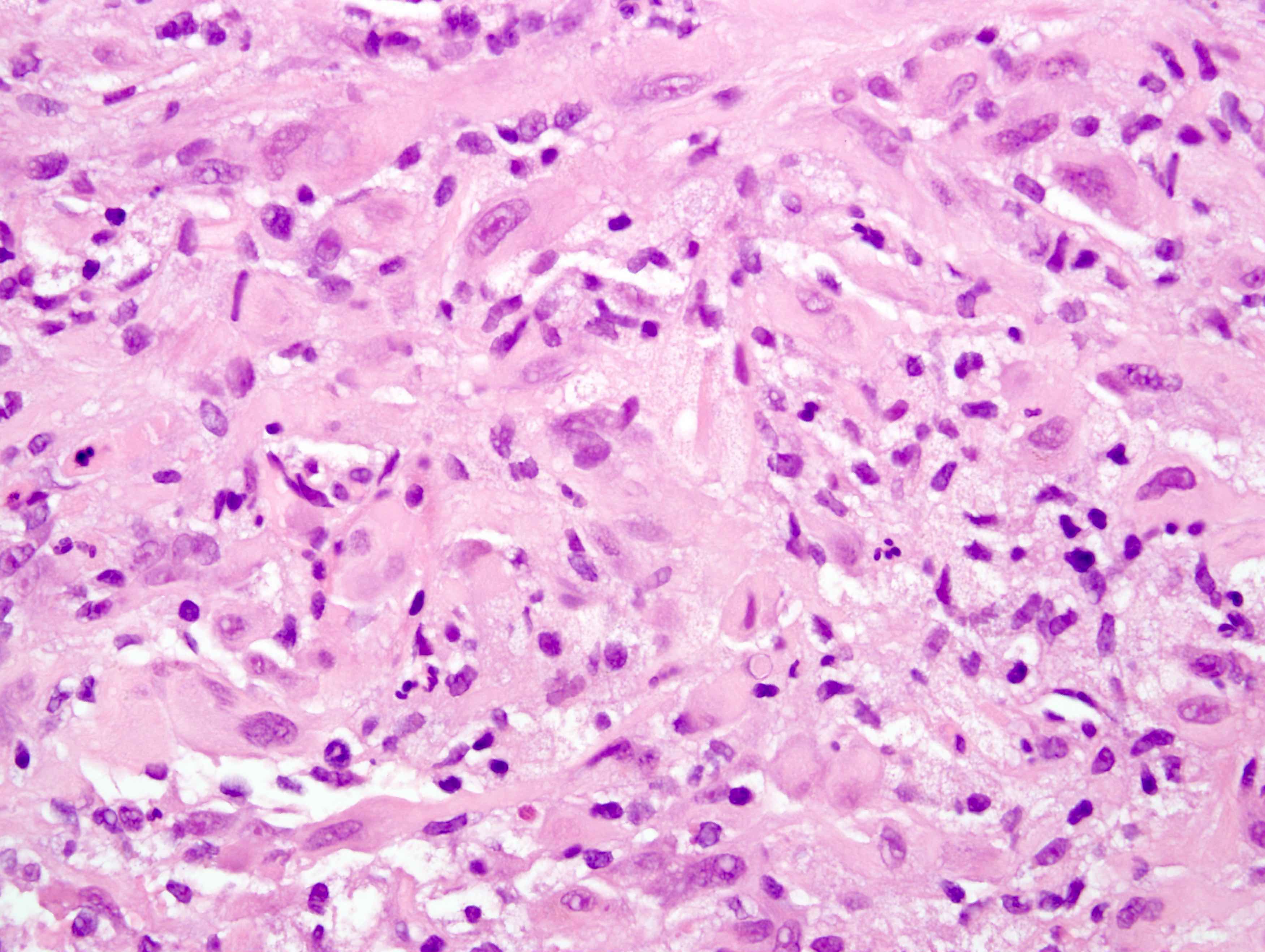
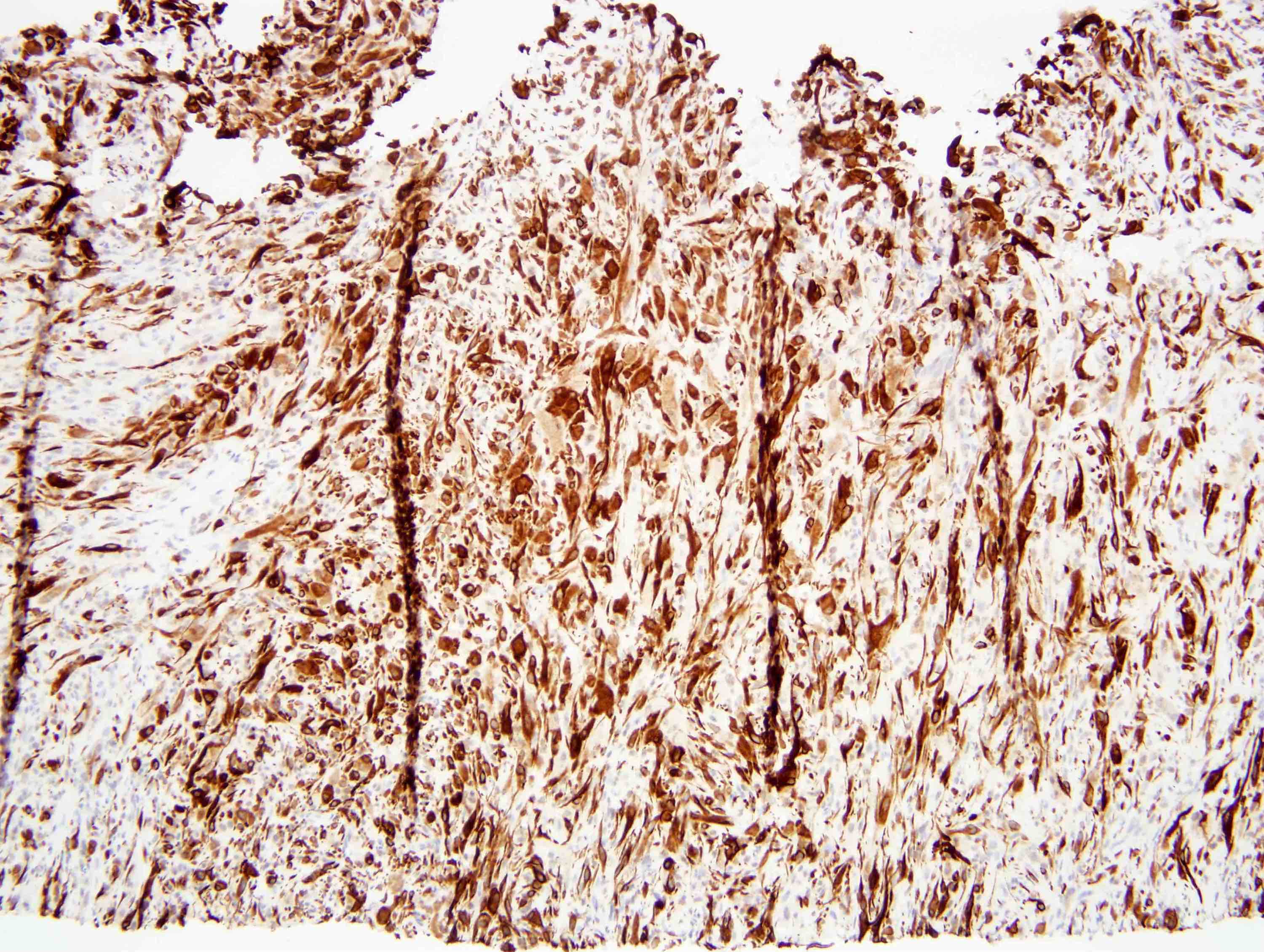
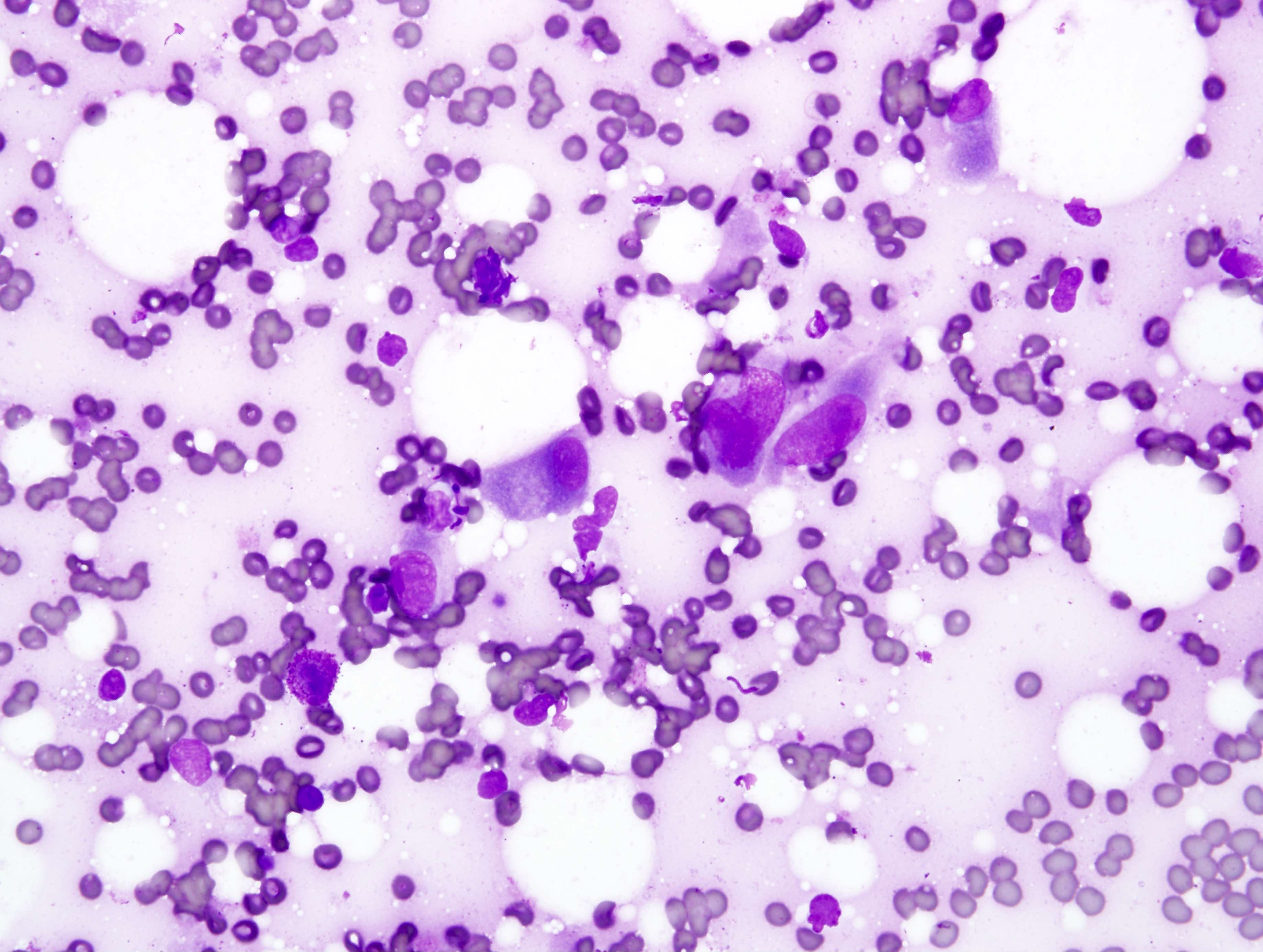
Microscopic (histologic) description
- Architecture (Arch Pathol Lab Med 2019;143:763, Am J Surg Pathol 2011;35:190):
- Vaguely nodular or plexiform; infiltrates surrounding soft tissues
- Desmoplastic reaction may be seen
- Sheets or short fascicles; often with variably prominent inflammatory (usually neutrophilic) infiltrate
- Sometimes has a myxoid background
- In cutaneous lesions, epidermal hyperplasia or ulceration may be present
- Cytologic features:
- Plump spindle to epithelioid cells with vesicular nuclei, variably prominent nucleoli and abundant deeply eosinophilic cytoplasm
- May resemble rhabdomyoblasts
- Usually only mild nuclear atypia
- Mitotic activity: typically < 5 - 10 mitoses/high power field (average of 2 mitoses/high power field)
- Necrosis, marked nuclear pleomorphism and intracytoplasmic vacuoles are rare
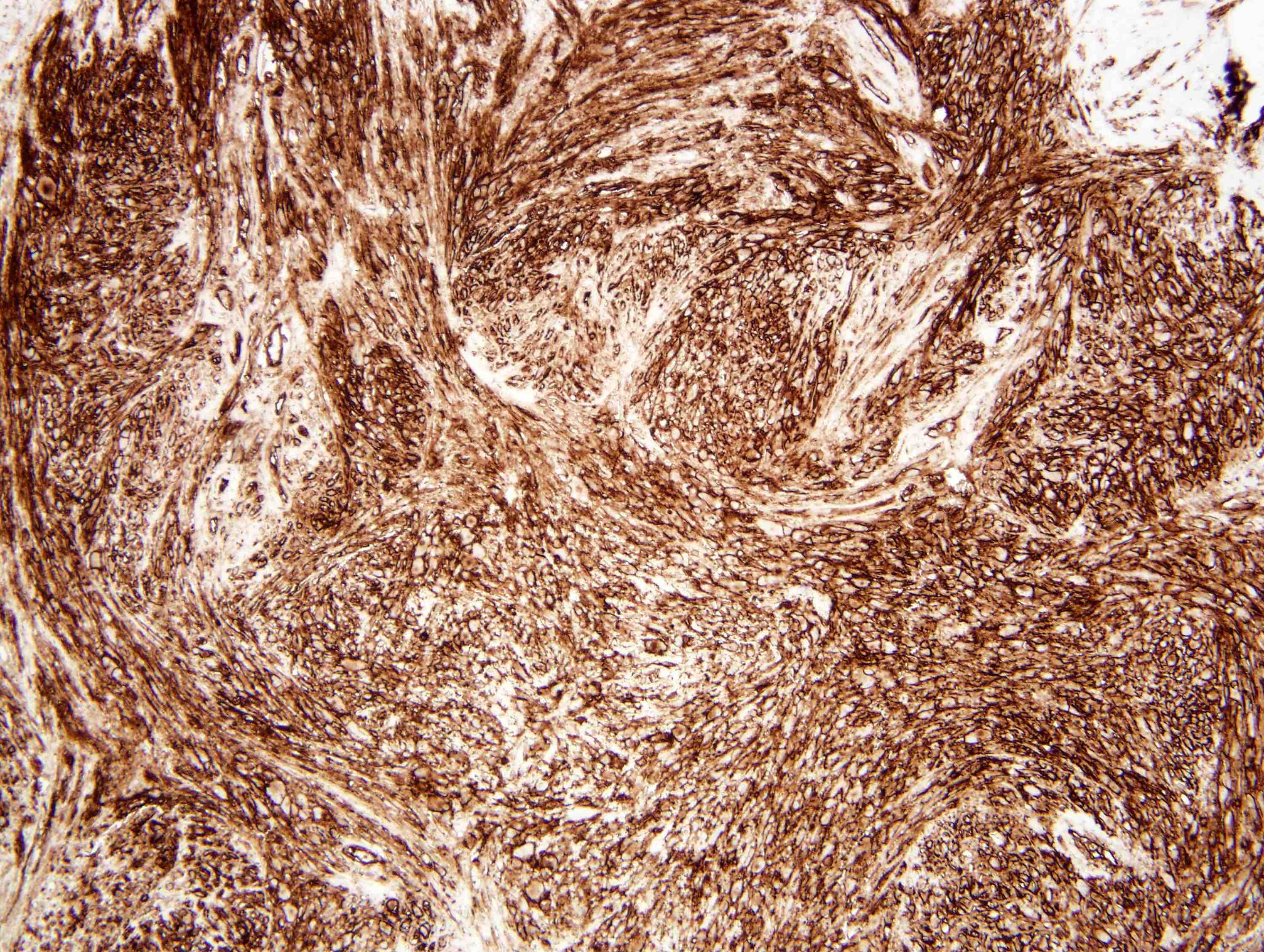
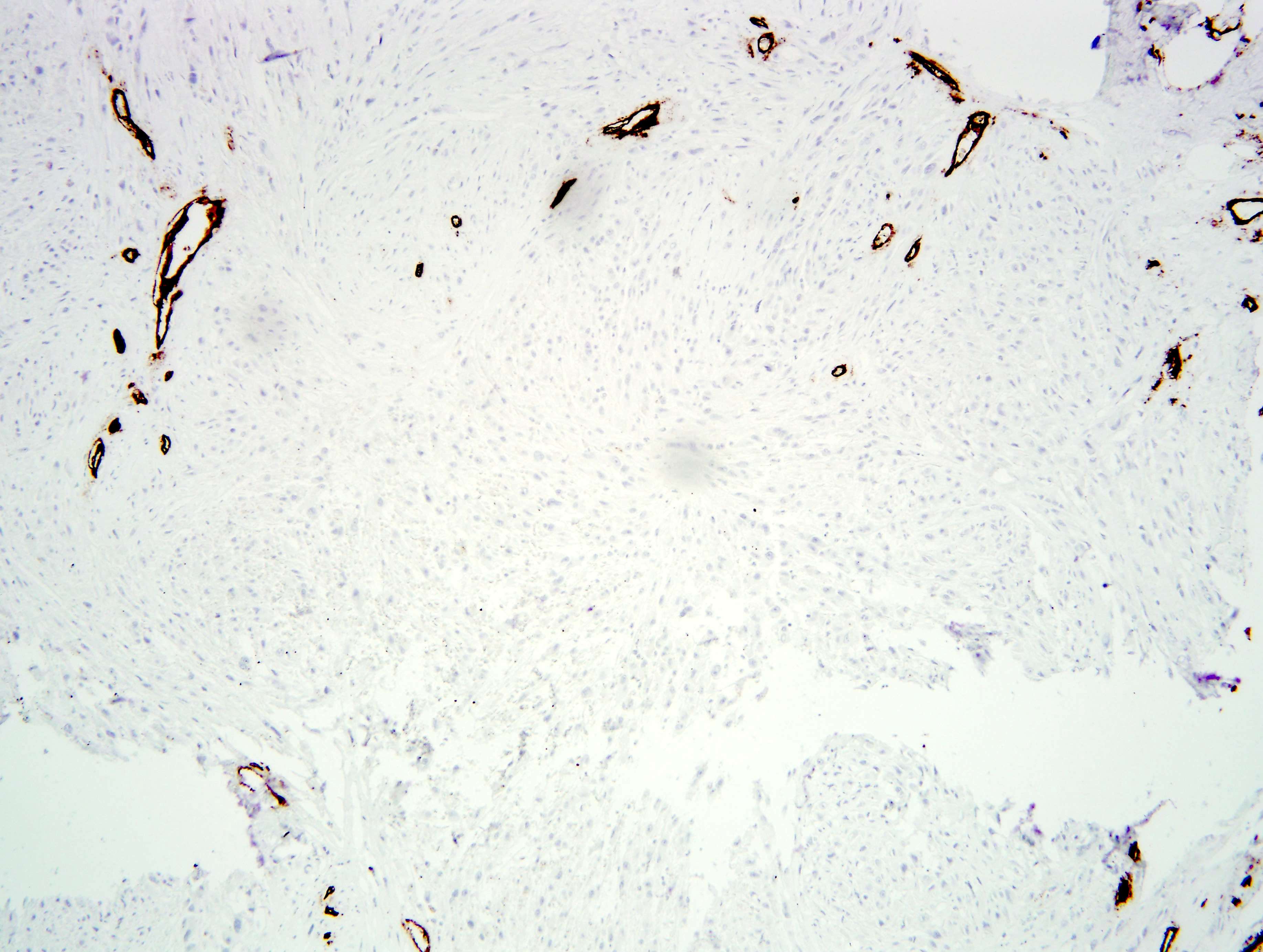
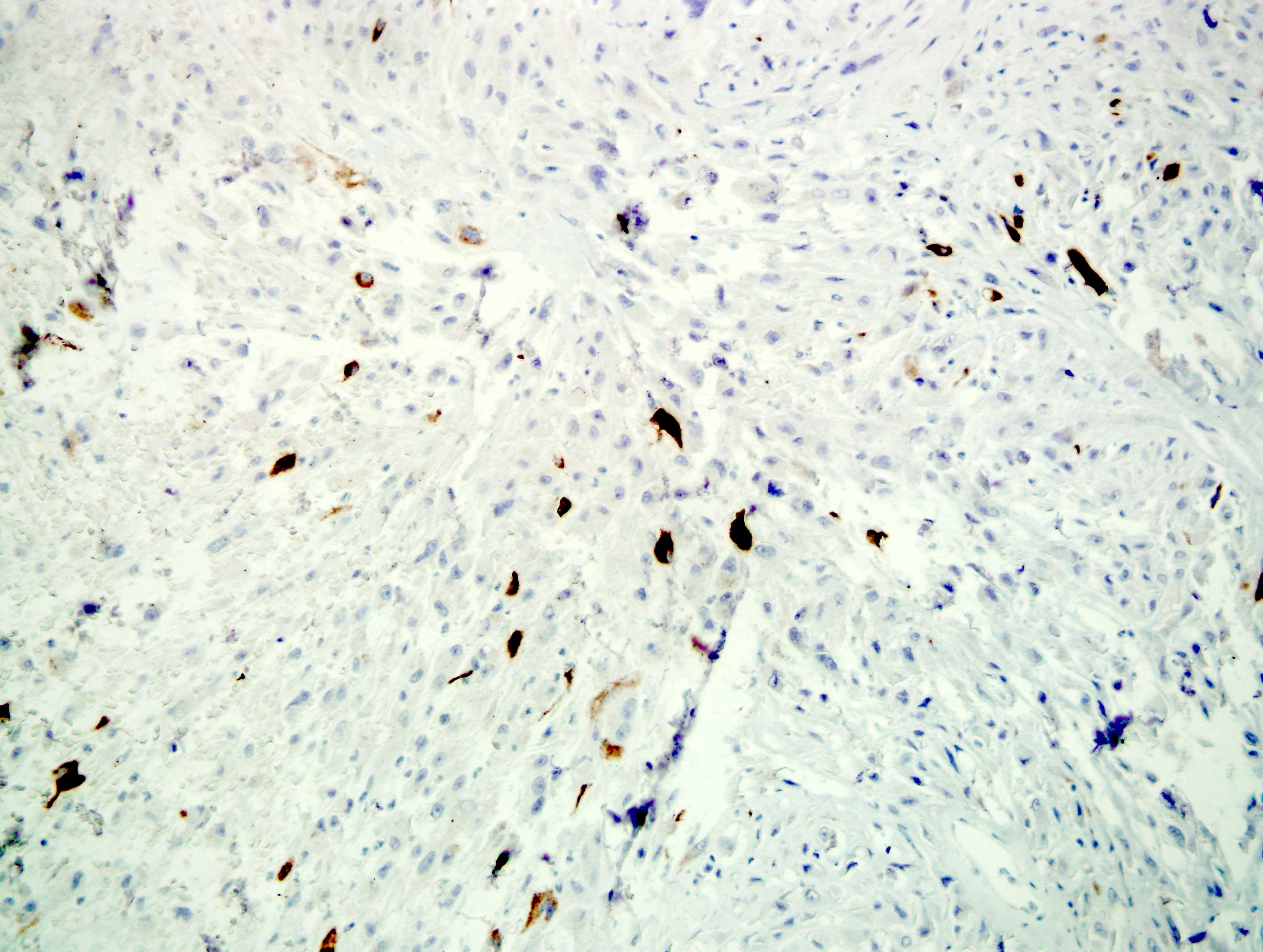
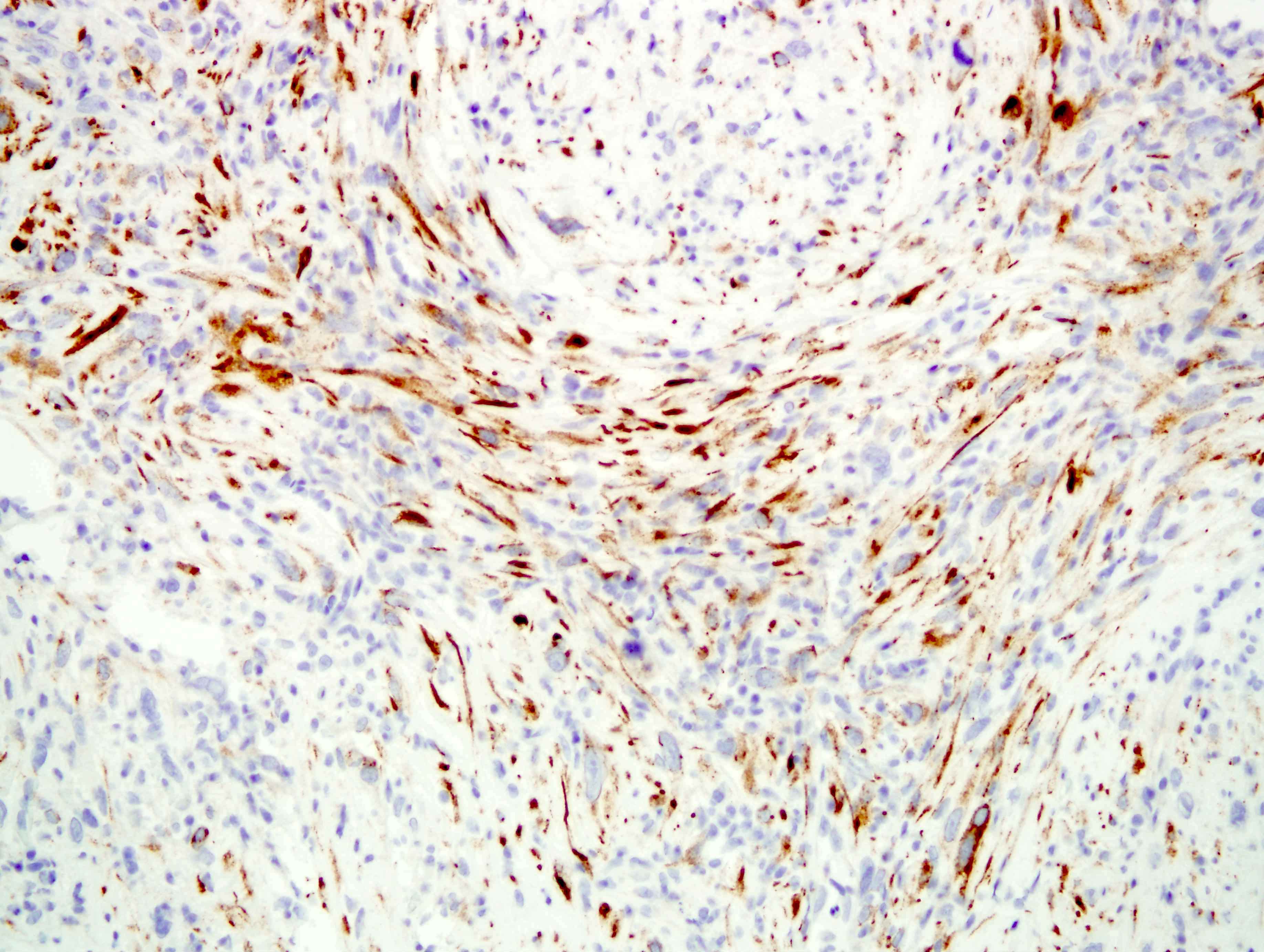
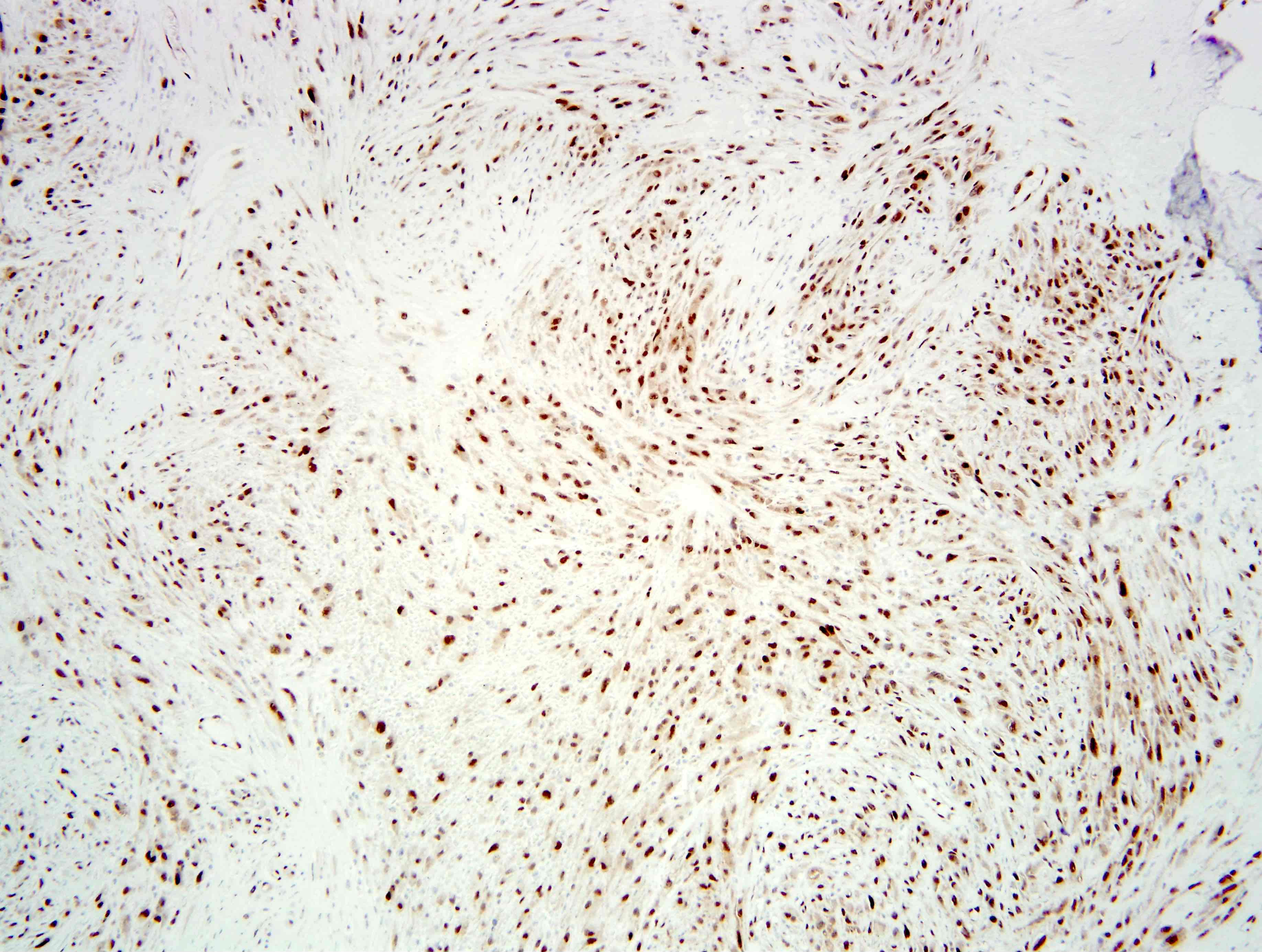
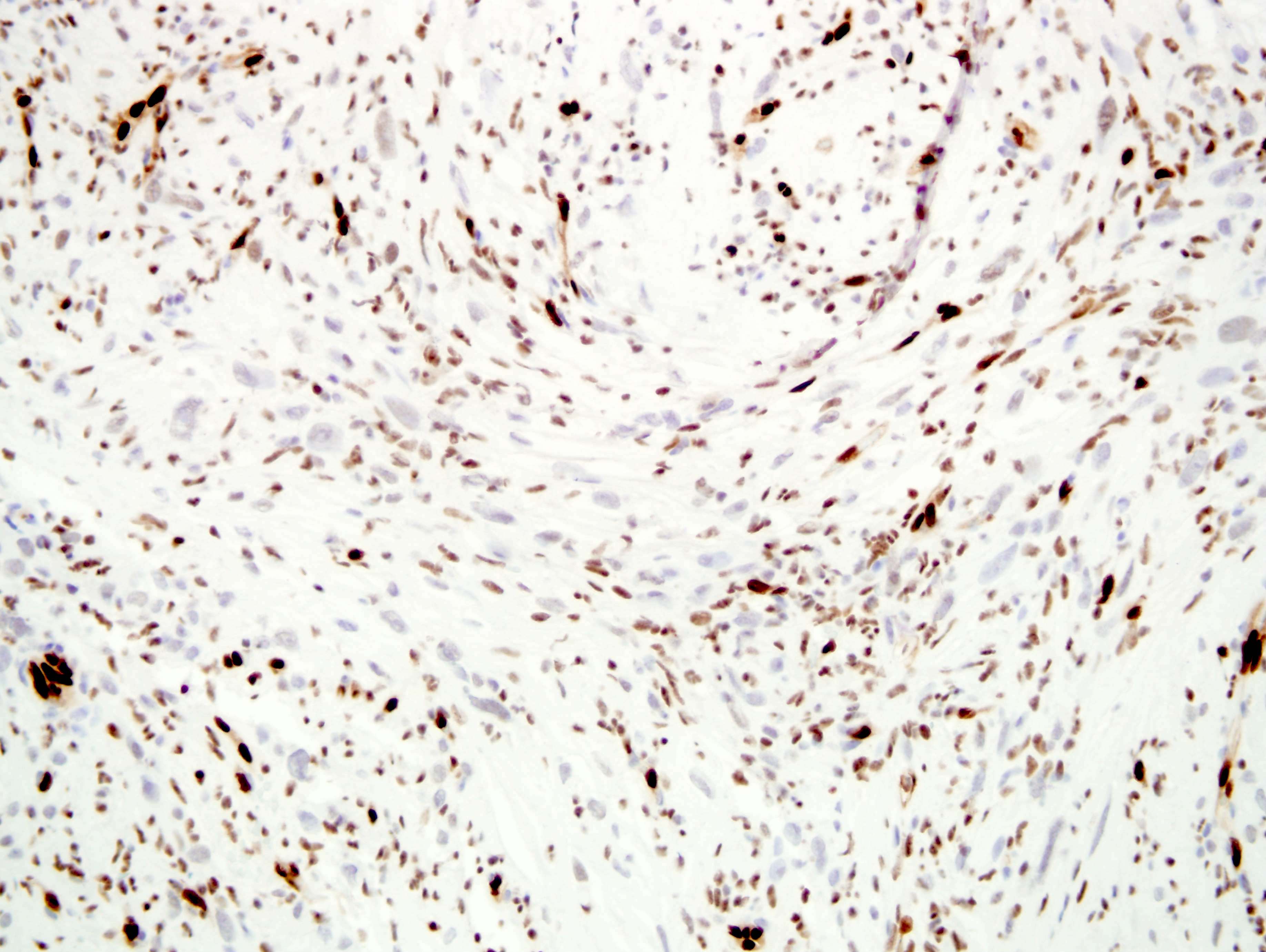
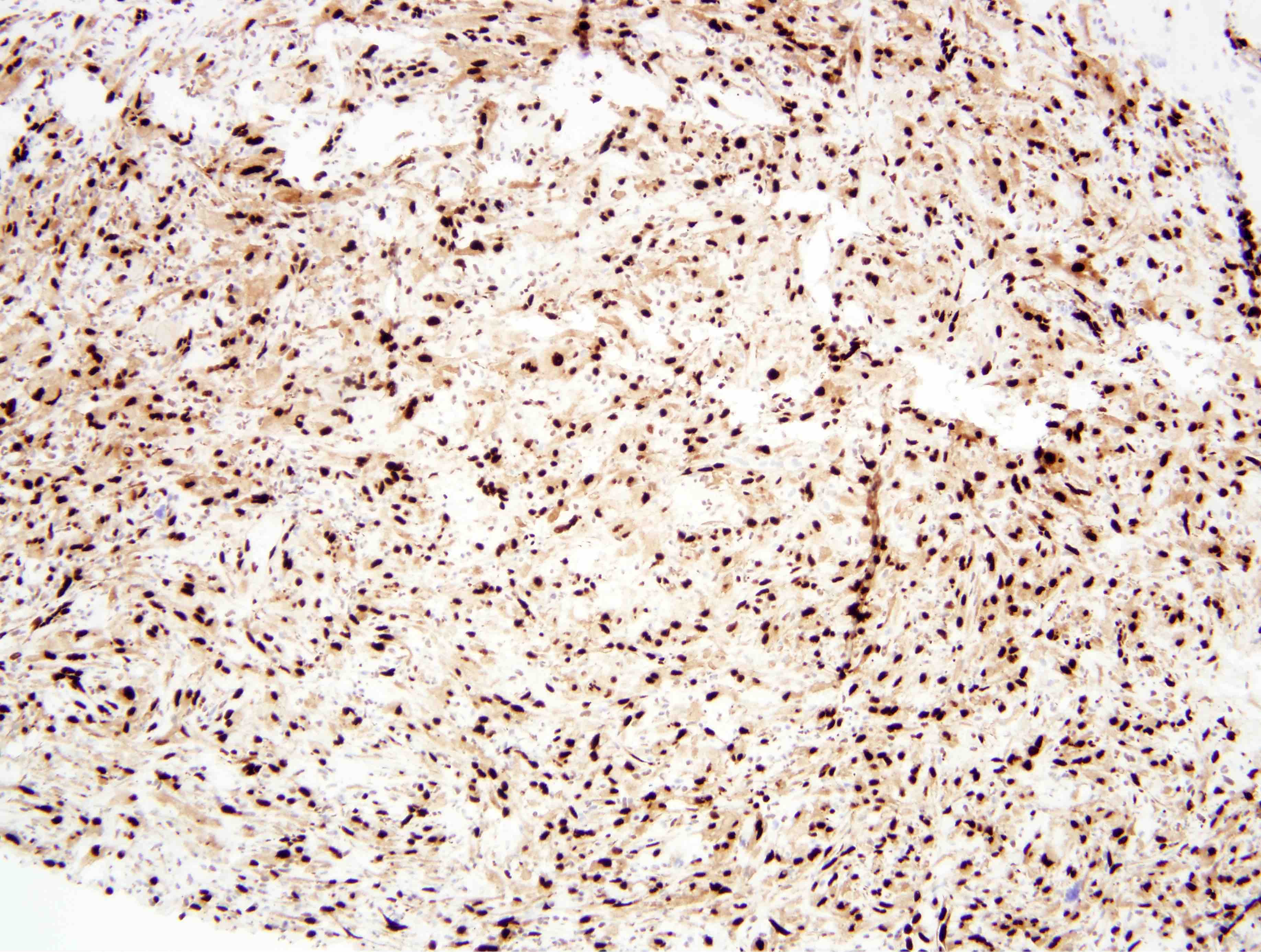
Microscopic (histologic) images
Contributed by Farres Obeidin, M.D. and Borislav Alexiev, M.D.
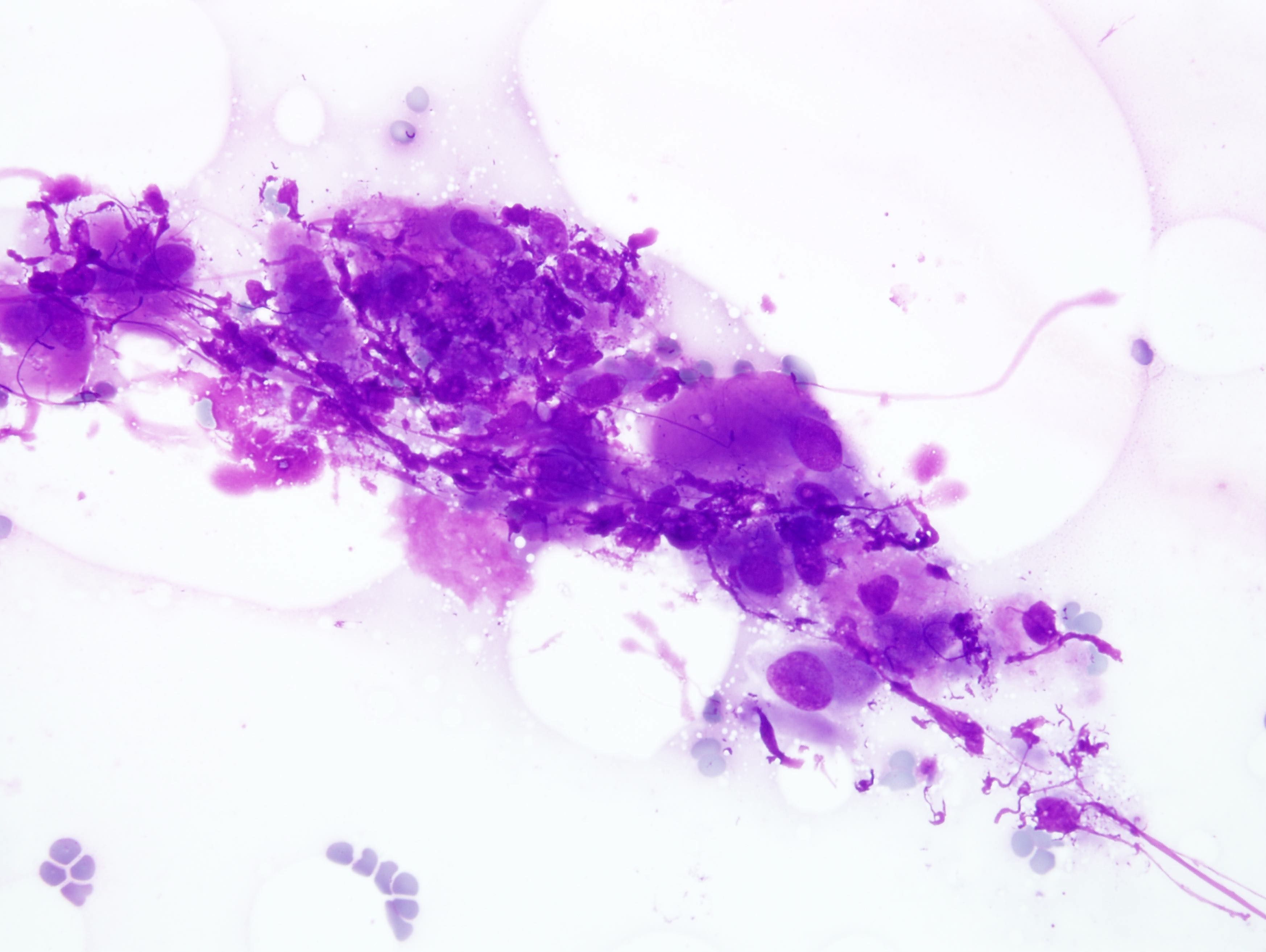
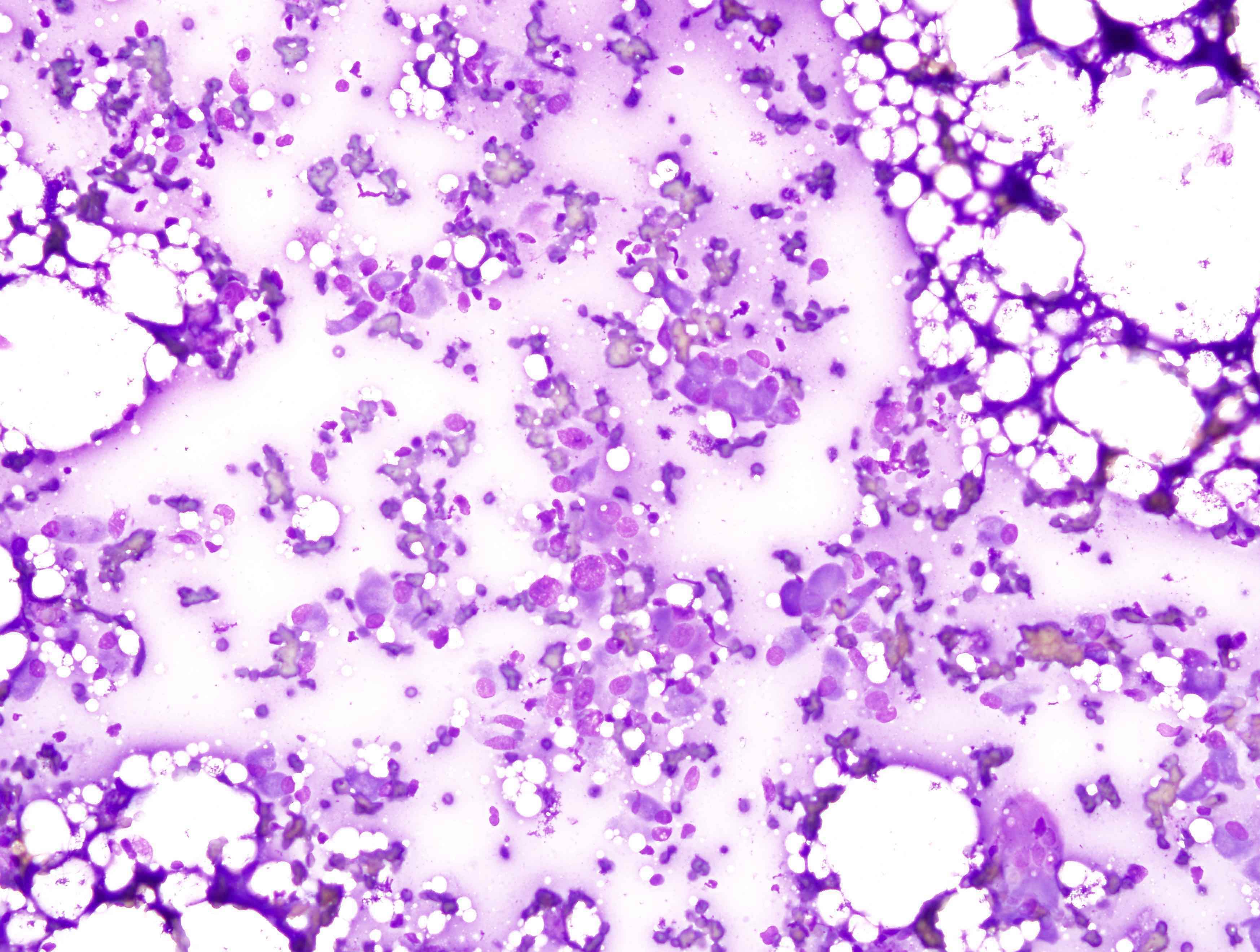
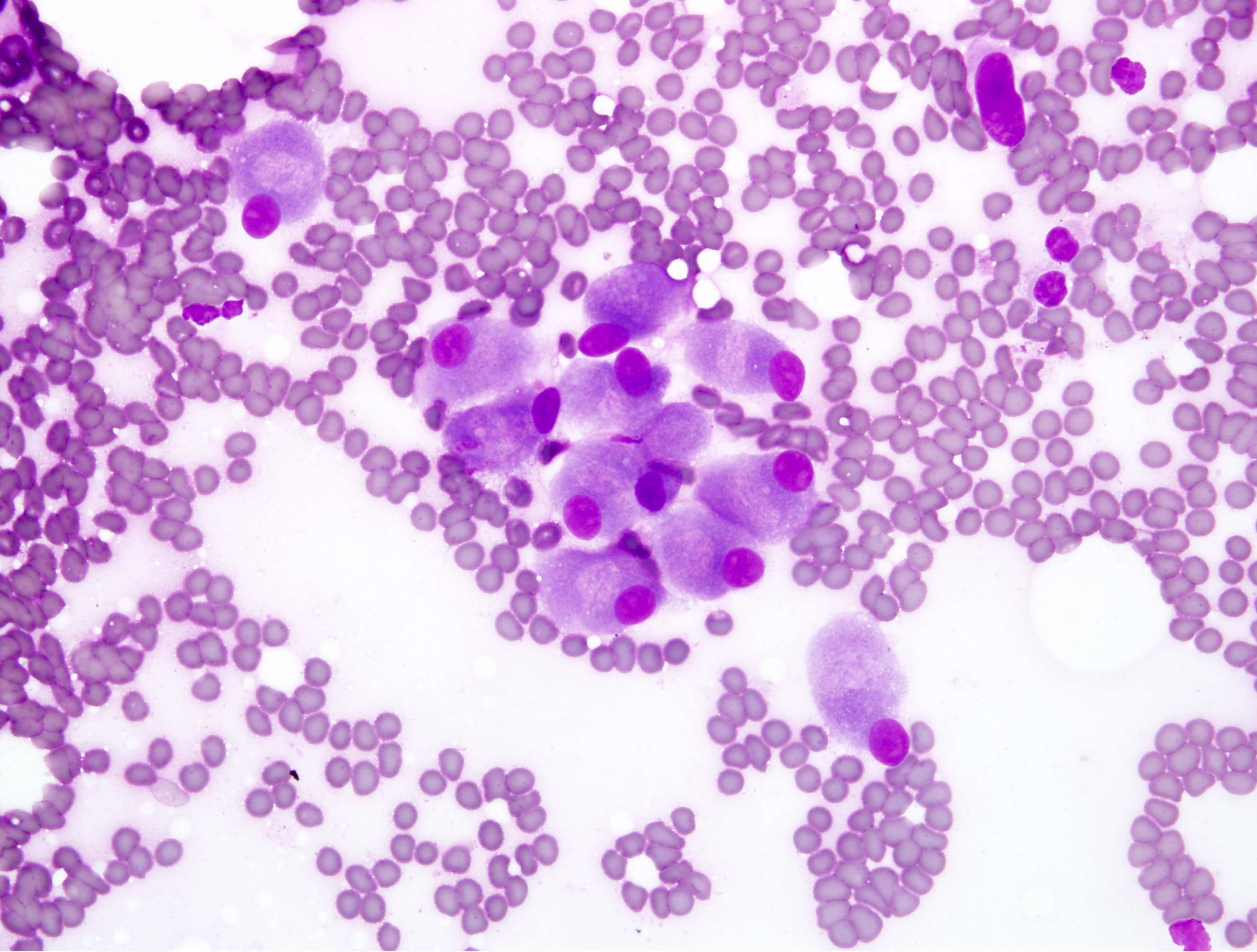
Cytology description
- Cells range from plump spindled to round, epithelioid
- Abundant pink cytoplasm, reminiscent of rhabdoid or plasmacytoid cells
Cytology images
Positive stains
- AE1 / AE3, ERG, FLI1
- FOSB
- CD31 (47%) (Am J Surg Pathol 2011;35:190)
- Focal positivity for CAM 5.2, SMA and EMA
- INI1 retained (Arch Pathol Lab Med 2019;143:763)
Negative stains
Electron microscopy description
- Only very rare cases have been evaluated by electron microscopy; no definitive Weibel-Palade bodies seen
- Prominent rough endoplasmic reticulum and intermediate filaments
- Submembranous pinocytic vesicles and scattered desmosome-like junctions (Am J Surg Pathol 2011;35:190)
Molecular / cytogenetics description
- Recurrent t(7;19)(q22;q13) translocation resulting in the fusion SERPINE1 and FOSB (J Pathol 2014;232:534)
Sample pathology report
- Right leg, mass, resection:
- Pseudomyogenic hemangioendothelioma (see comment)
- Comment: Microscopic sections show a multinodular spindle cell proliferation with prominent brightly eosinophilic cytoplasm. There is mild to moderate cytologic atypia and only rare mitotic activity. Stains for keratin AE1 / AE3, ERG, CD31 and FOSB are positive while CAMTA1 is negative and INI1 is retained, supporting the above diagnosis.
Differential diagnosis
- Depends on location
- Cutaneous / superficial tumors:
- Epithelioid sarcoma:
- Sarcomatoid carcinoma:
- Keratins may be positive in either
- Look for areas of traditional carcinoma or an in situ component
- Negative for vascular markers and FOSB
- Cellular fibrous histiocytoma:
- Polymorphous population of fibroblasts and histiocytes
- Factor XIII and often CD34 positive but tumor cells negative for vascular markers and FOSB
- Leiomyosarcoma or myofibroblastic lesions:
- Positive for desmin and SMA; h-caldesmon for leiomyosarcoma
- Negative for vascular markers
- Deep tumors (Am J Surg Pathol 2011;35:190):
- Epithelioid hemangioendothelioma:
- Lacks the bright eosinophilic cytoplasm and more commonly has intracytoplasmic lumina with red blood cells; typical cases have a prominent myxohyaline background
- Negative for FOSB, positive for CAMTA1
- Epithelioid angiosarcoma:
- Much more prominent nuclear atypia and mitotic activity with higher proliferation rate by Ki67
- May have more well formed vascular channels lined by malignant endothelial cells
- FOSB negative
- Rhabdomyosarcoma:
- Nodular / proliferative fasciitis
- Epithelioid hemangioendothelioma:
- Bone tumors (Skeletal Radiol 2015;44:727):
Practice question #1
A 30 year old man presents with multiple foot nodules. The largest nodule is biopsied and shows the histology pictured above. Stains for keratin and ERG are positive while CAMTA1 and CD34 are negative. INI1 is retained. Which of the following is true about this lesion?
- This tumor is aggressive and has high propensity for metastasis
- It typically harbors a YAP1-TFE3 translocation
- The cells have a myogenic immunophenotype
- FOSB immunostain is often positive
Practice answer #1
D. FOSB immunostain is often positive. This tumor is an example of a pseudomyogenic hemangioendothelioma (PHE). While locally aggressive, these tumors only rarely metastasize. YAP1-TFE3 translocations are seen in a small subset of epithelioid hemangioendothelioma. Pseudomyogenic hemangioendothelioma is typically negative for smooth muscle and skeletal muscle stains. Immunohistochemistry for FOSB is typically positive as these tumors harbor a recurring t(7;19) translocation involving SERPINE1 and FOSB.
Comment Here
Reference: Pseudomyogenic hemangioendothelioma
Comment Here
Reference: Pseudomyogenic hemangioendothelioma
Practice question #2
Which of the following translocations may be seen in pseudomyogenic hemangioendothelioma?
- t(7;19) SERPINE1-FOSB
- t(1;3) WWTR1-CAMTA1
- t(7;16) FUS-CREB3L2
- t(2;13) PAX3-FOXO1
Practice answer #2
A. t(7;19) SERPINE1-FOSB. Pseudomyogenic hemangioendothelioma is characterized by a t(7;19) SERPINE1-FOSB fusion in the majority of cases. The t(1;3) WWTR1-CAMTA1 translocation is seen in epithelioid hemangioendothelioma. Low grade fibromyxoid sarcoma harbors the t(7;16) FUS-CREB3L2 fusion and alveolar rhabdomyosarcoma shows the t(2;13) PAX3-FOXO1 fusion.
Comment Here
Reference: Pseudomyogenic hemangioendothelioma
Comment Here
Reference: Pseudomyogenic hemangioendothelioma