Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Potterveld S, Clay MR. Atypical lipomatous tumor / well differentiated liposarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuewdliposarcoma.html. Accessed September 5th, 2025.
Definition / general
- Locally aggressive mesenchymal tumor composed of mature adipocytes and stromal cells with at least focal cytologic atypia
- Adipocytic component and background cellular constituents vary in concentration and lead to several recognizable morphologic subtypes
Essential features
- Low grade lipogenic tumor with multiple morphologic subtypes and significant histologic variability
- Molecularly characterized by ring or giant marker / rod chromosomes composed of material from 12q13-15
- Results in localized amplification of several neighboring genes, including MDM2
- Behavior is dependent upon location, with deep seated lesions having the ability to dedifferentiate and subsequently metastasize
- Terminology is based on location (see Terminology)
- Wide local excision with negative margins is often curative
Terminology
- Use of the terminology atypical lipomatous tumor (ALT) and well differentiated liposarcoma (WDL) is based on a tumor's location in the body and primarily relates to resectability
- Tumors are morphologically and genetically identical, with the variation in terminology intended to avoid both undertreatment and overtreatment
- Tumors located in the periphery have no risk of metastasis
- For such lesions, complete resection is generally curative
- For these tumors, the designation as sarcoma is inappropriate and the term ALT is preferred
- If the tumor is deep seated (retroperitoneum, mediastinum, spermatic cord), the chance of achieving negative margins is significantly diminished and the risk of local recurrence, dedifferentiation (DDL) and death are increased
- Lesions are best regarded as true sarcomas and the terminology of well differentiated liposarcoma is more appropriate
- Suggestion: use of atypical lipoma is not recommended
ICD coding
- ICD-O:
- ICD-11:
- 2F7C & XH0RW4 - neoplasms of uncertain behavior of connective or other soft tissue & atypical lipomatous tumor
- 2B5H & XH7Y61 - well differentiated lipomatous tumor, primary site & liposarcoma, well differentiated
Epidemiology
- Most common adipocytic malignancy (40 - 45% of all liposarcomas)
- Peak age in adults is between 40 - 60 years
- Very rare in children but can be associated with Li-Fraumeni syndrome (Hum Pathol 2018;71:41, Pediatr Dev Pathol 2010;13:218)
Sites
- Most common site is the deep thigh of the lower extremity, followed by retroperitoneum, trunk, head and neck region and spermatic cord
- Numerous anatomic sites have been reported, including the subcutis and skin
Diagnosis
- Diagnosis typically requires surgical resection to ensure adequate sampling, as diagnostic accuracy is limited by sampling bias on core needle biopsy (AJR Am J Roentgenol 2021;216:997)
Radiology description
- Fat tissue density mass with thick or nodular enhancing septa on CT imaging
- Mass of fat isointense signal in all sequences, thick septa or nodular nonlipomatous areas with contrast enhancement on MRI imaging
- Retroperitoneal WDL typically shows fat with an abnormal appearance on MRI (stranding) that represents the thick fibrous bands
- Reference: Radiographics 2005;25:1371
Prognostic factors
- Most important factor is anatomic location
- Tumors do not metastasize unless they dedifferentiate, which is associated with significantly shorter overall survival (Am J Surg Pathol 2007;31:1)
- Subcutaneous or intramuscular tumors may recur but typically do not dedifferentiate or metastasize
- Risk of dedifferentiation is directly related to location and duration of growth
Case reports
- 36 year old woman with gluteal mass (World J Surg Oncol 2006;4:33)
- 43 year old woman with abdominal fullness and weight gain (Hinyokika Kiyo 2010;56:697)
- 73 year old man with mesenteric tumor (Case Rep Oncol 2011;4:178)
- Multiple cases of oral and salivary gland liposarcomas (Mod Pathol 2002;15:1020)
Treatment
- Surgical resection with widely negative margins is generally curative
- Retroperitoneal or central body site tumors are difficult to resect with a clear margin, frequently recur, can dedifferentiate and cause death (J Surg Res 2012;175:12)
- Positive margin status and sclerosing subtype are associated with reduced local recurrence free survival (Ann Surg Oncol 2004;11:78)
Clinical images
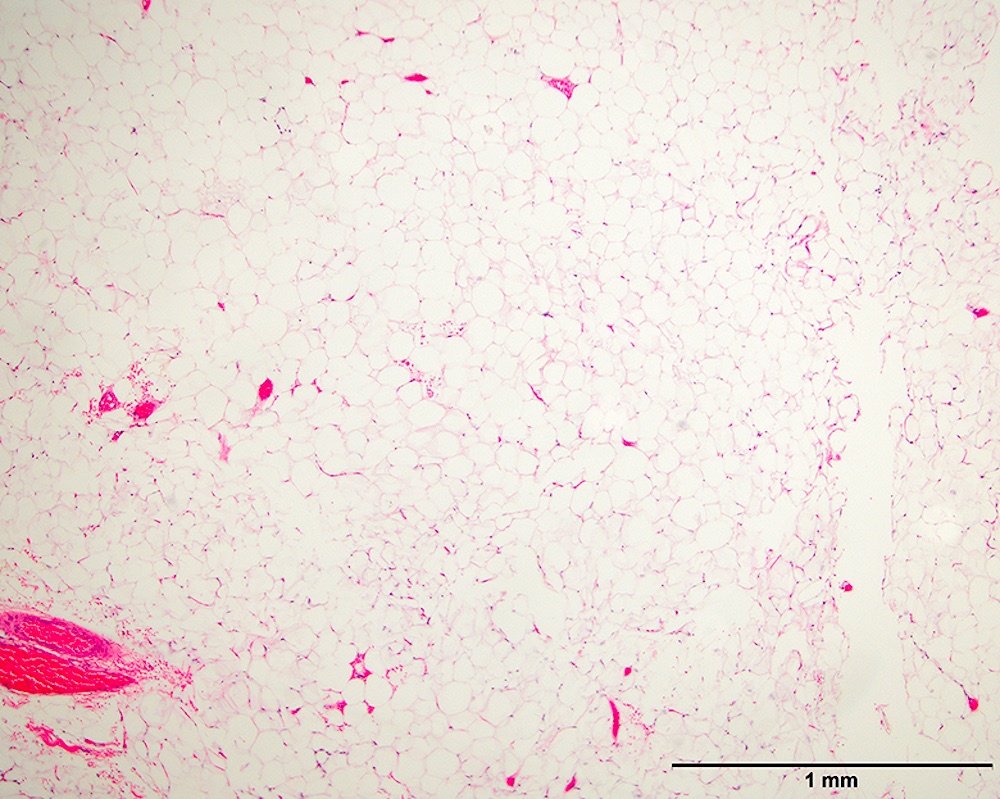
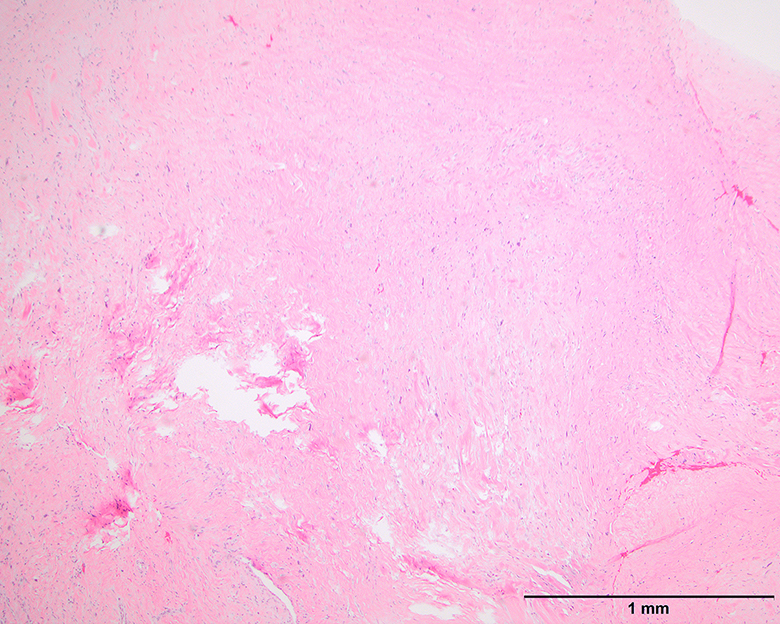
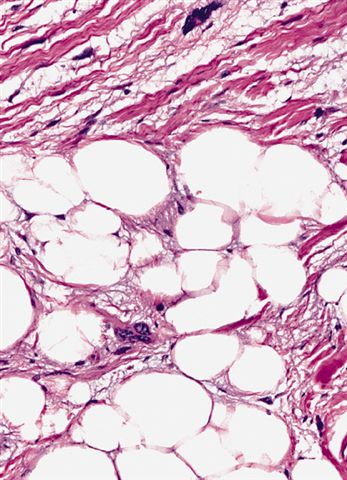
Gross description
- Typically multilobulated and well circumscribed
- Rarely are grossly infiltrative
- Marbled yellow cut surface in lipoma-like lesions, with more firm / fibrotic white areas grossly in lesions with less adipocytic differentiation (Semin Diagn Pathol 2019;36:112)
- Fat necrosis in large lesions, especially at the periphery
- Sample carefully to look for dedifferentiated components
- Dedifferentiated areas are nonlipogenic and can stand out as firm nodules or be more diffusely admixed with low grade areas
Gross images
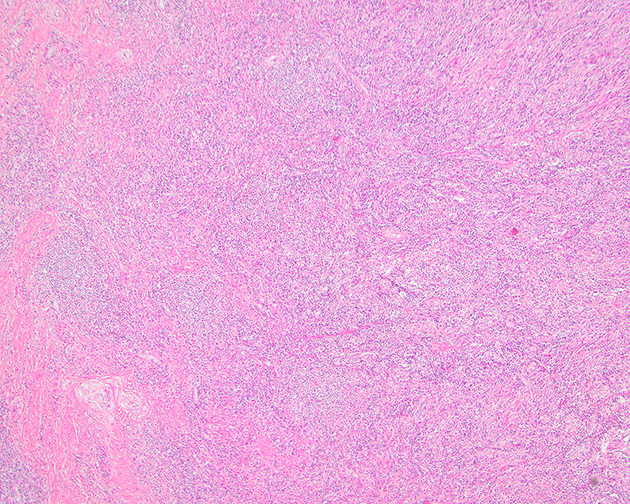
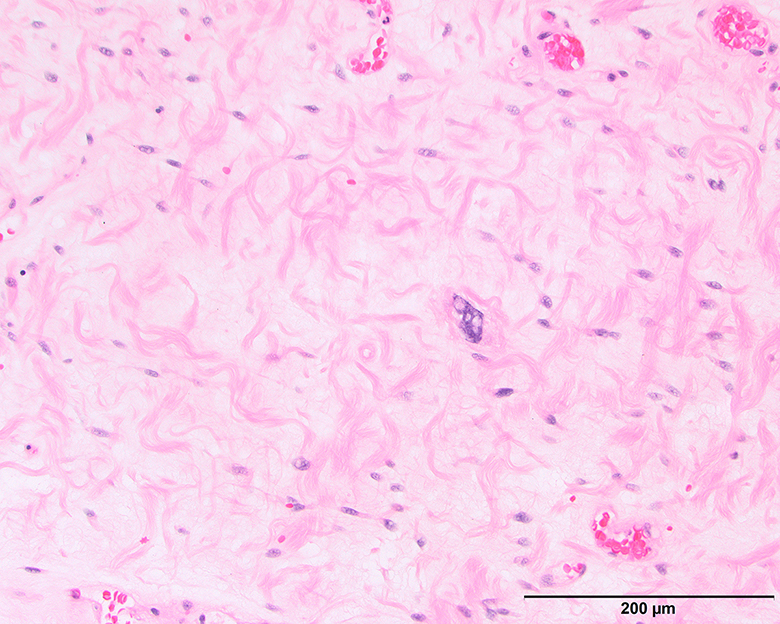
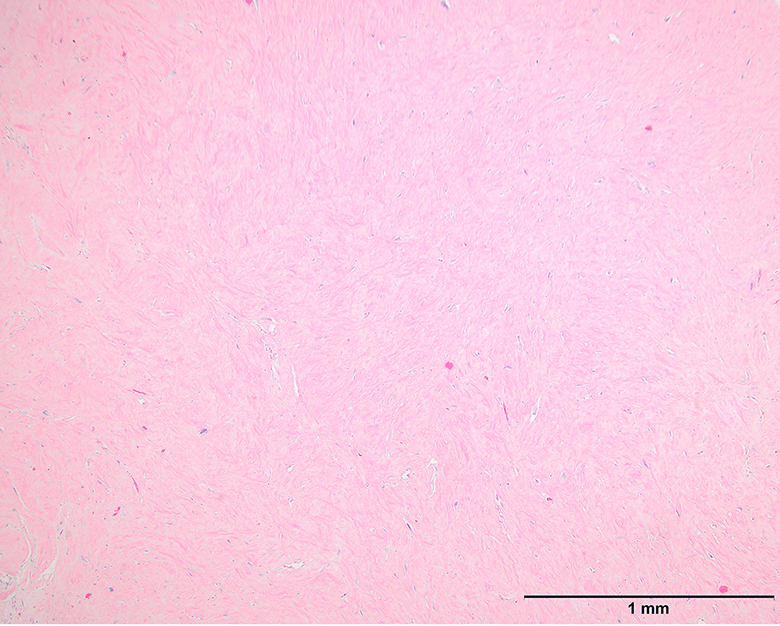
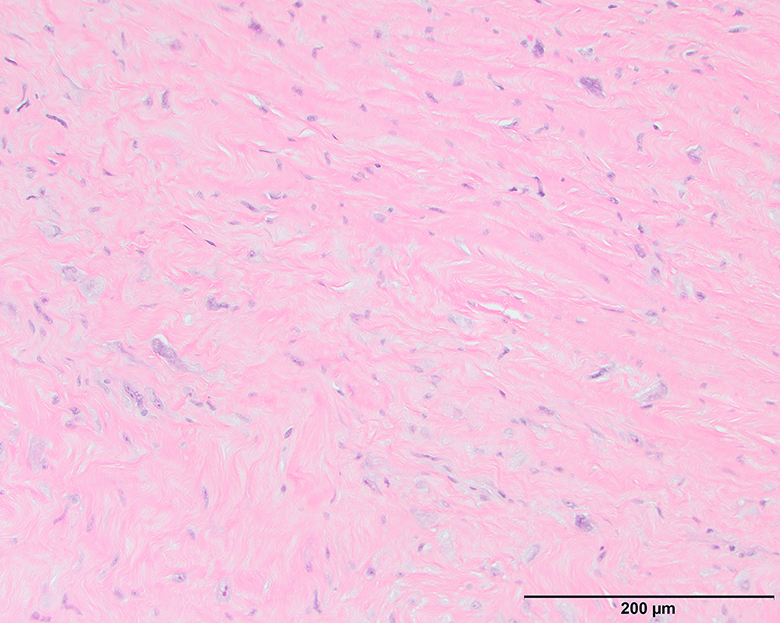
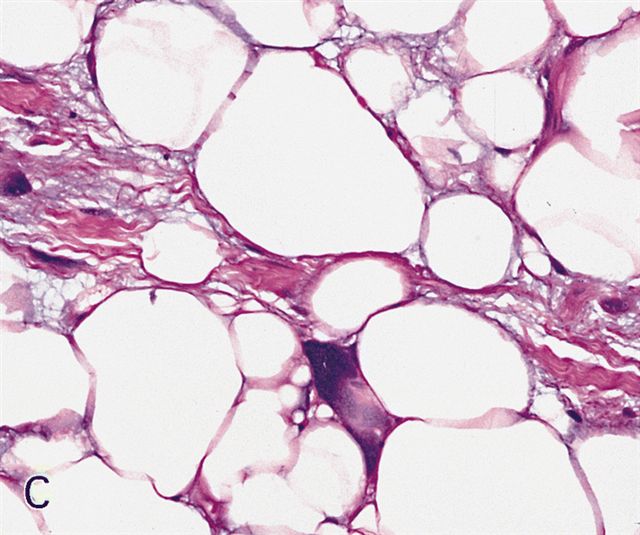
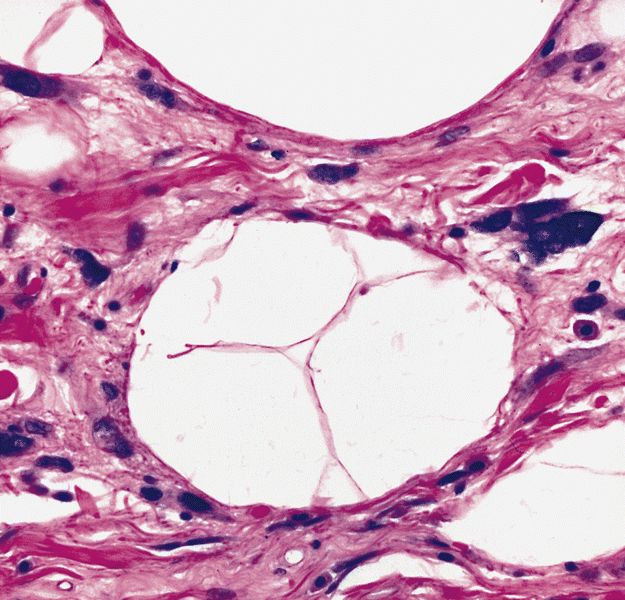
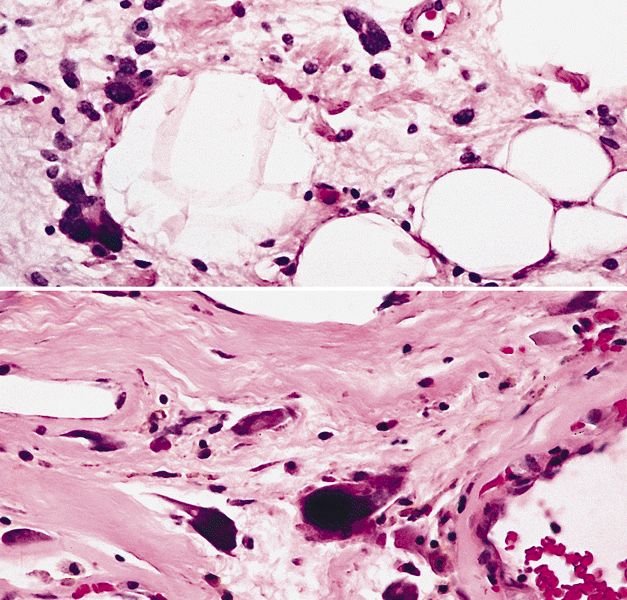
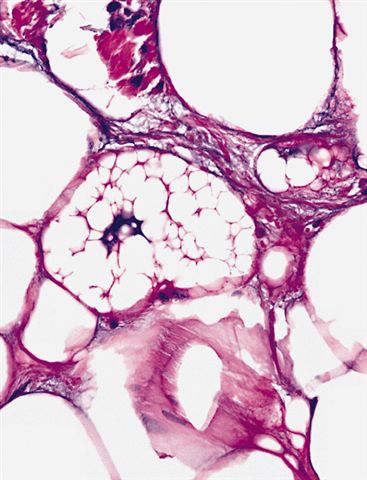
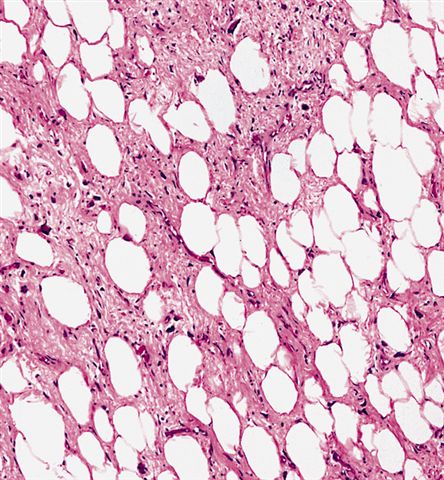
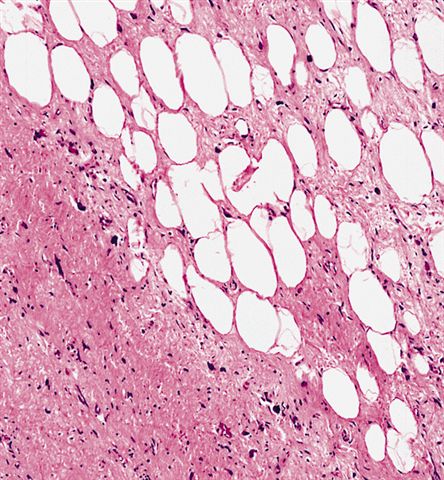
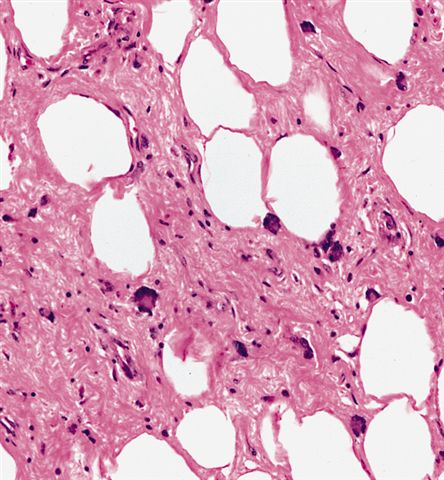
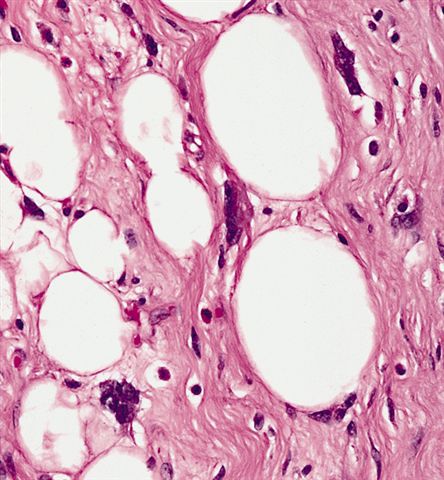
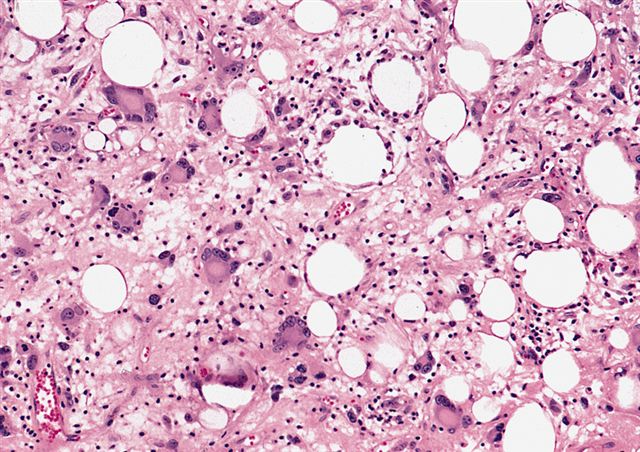
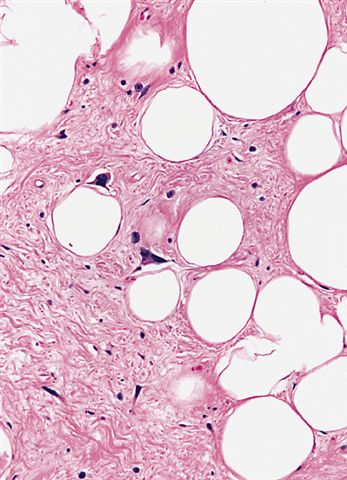
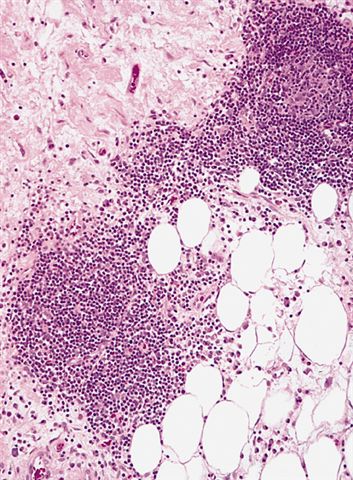
Microscopic (histologic) description
- Depends on subtype, generally composed of mature fat with variably sized adipocytes and bands of fibrotic stroma containing spindle cells with enlarged, hyperchromatic nuclei
- Can be markedly atypical
- Cellularity is low and mitotic figures are uncommon
- Atypical cells are more commonly found in fibrous septa and in a perivascular distribution
- Rarely display heterologous differentiation (Hinyokika Kiyo 2010;56:697)
- There are 3 histologic subtypes that have limited clinical significance (Semin Diagn Pathol 2001;18:258, Ann Surg Oncol 2004;11:78)
- Lipoma-like subtype
- Most common subtype
- Scattered atypical cells may be diffuse or exceedingly rare
- Frequently contains lipoblasts
- Grossly, can be indistinguishable from lipoma
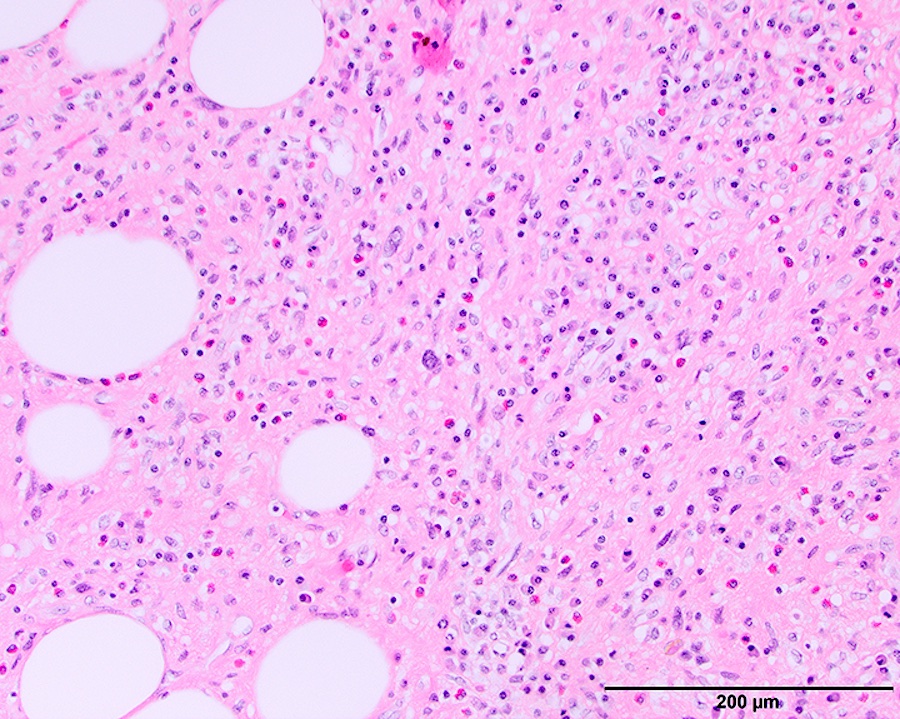
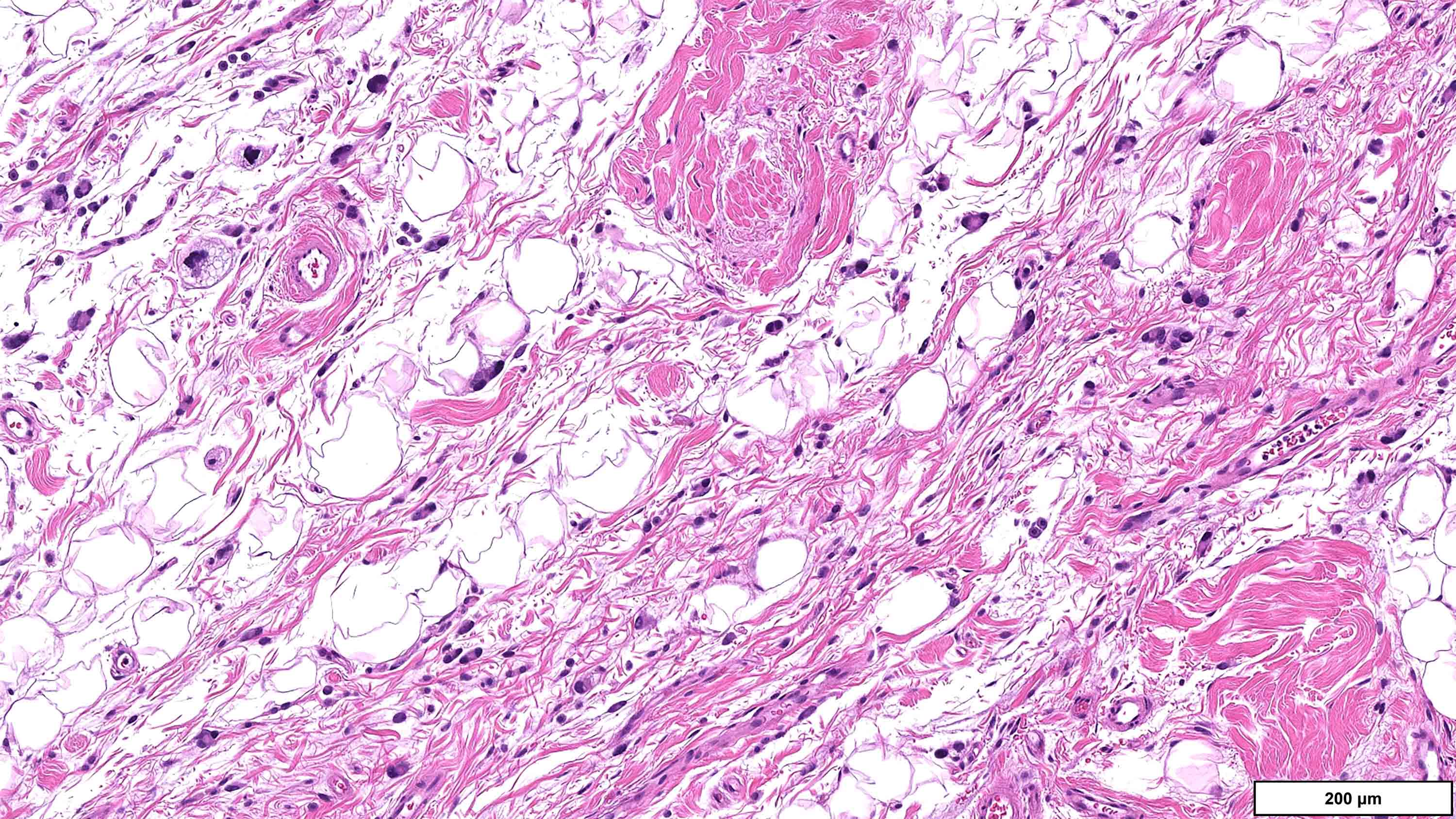
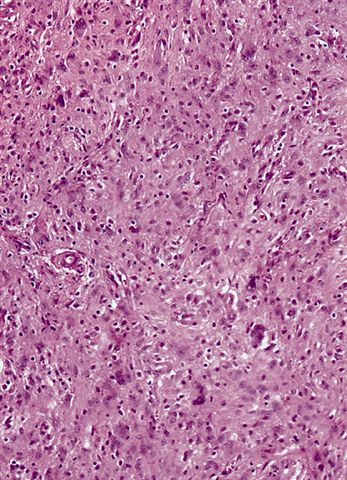
- Sclerosing subtype
- Second most common subtype
- Predilection for retroperitoneal or paratesticular location
- Collagenous fibrous tissue with scattered adipocytes and atypical multinucleated stromal cells
- Scant lipogenic component may be missed in small samples
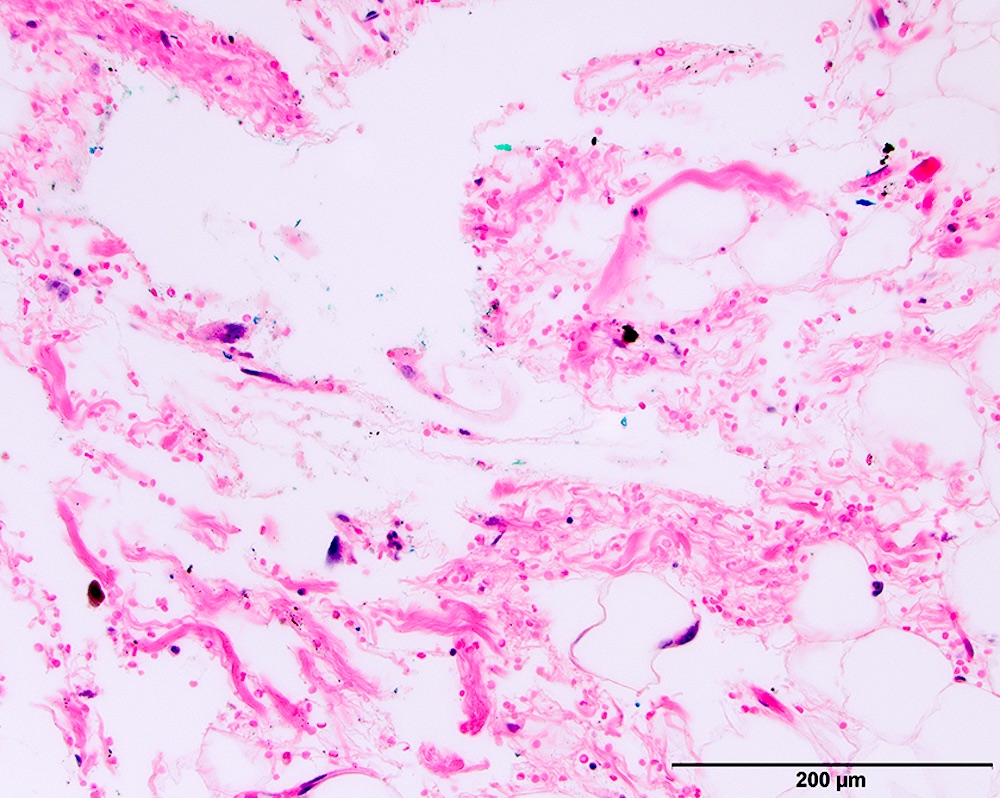
- Inflammatory subtype
- Rare
- Almost always in the retroperitoneum where it is confused with nonlipogenic tumors
- Chronic inflammatory cells (B > T cells) with occasional lymphoid follicles scattered in a cellular fibrocollagenous stroma with sparse multinucleated atypical cells
- May obscure adipocytes
- Lipoma-like subtype
- Mixed subtype
- Not uncommon to see an admixture of these subtypes with sufficient sampling
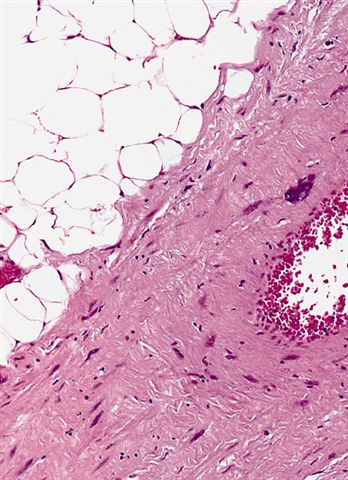
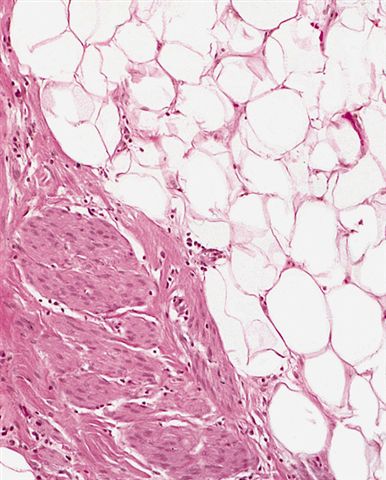
- Rarest variants
- Lipoleiomyosarcoma
- Liposarcoma with leiomyosarcomatous differentiation
- Both components are low grade
- Variable amount of the smooth muscle component, which can be seen in association with large vascular walls
- Similar biology and can dedifferentiate
- ALT / WDL with low grade osteosarcoma-like areas
- In contrast to osseous metaplasia, these lesions have foci reminiscent of parosteal osteosarcoma or low grade central osteosarcoma (Am J Surg Pathol 2010;34:1361)
- Lipoleiomyosarcoma
- Pitfalls and tips
- Nuclei with sharply outlined vacuoles (Lochkern cells) are enlarged and can appear hyperchromatic but are normal adipocytes cut in cross section
- These do not qualify for the diagnosis; the same goes for atrophic skeletal muscle fibers, which can simulate atypia on an otherwise typical lipoma
- Histiocytes in areas of fat necrosis can simulate atypical cells
- Lipoblasts are neither necessary nor sufficient for diagnosis
- When present they are generally multivacuolated versus the signet ring lipoblasts commonly seen in myxoid liposarcoma
- Fatty differentiation may be very focal and difficult to differentiate from background adipocytes; when in doubt test molecularly (see Molecular / cytogenetics description)
- Lipomas do occur in the retroperitoneum and the distinction with WDL may require molecular testing (BMC Res Notes 2015;8:75)
- Retroperitoneal WDL typically shows fat with an abnormal appearance on MRI (stranding) that represents the thick fibrous bands
- Avoid using subtypes as diagnoses (i.e., inflammatory liposarcoma); the preferred terminology would be well differentiated liposarcoma, with the addition of inflammatory subtype (or that information conveyed in the comment)
- Nuclei with sharply outlined vacuoles (Lochkern cells) are enlarged and can appear hyperchromatic but are normal adipocytes cut in cross section
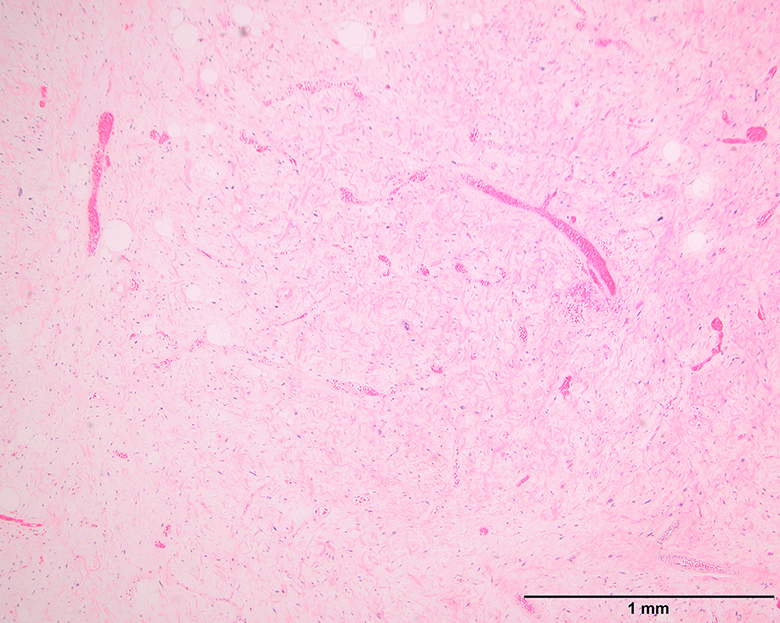
Microscopic (histologic) images
Contributed by Michael Clay, M.D., Melanie Bourgeau, M.D. and AFIP
Morphologic variability:
Metaplastic change:
Virtual slides
Cytology description
- Large cells with multilobulated nuclei and mature appearing adipocytes
- May have bizarre tumor cells (Acta Cytol 2000;44:459)
Positive stains
- MDM2, CDK4 and p16 together have 71% sensitivity and 98% specificity for detecting WDL and DDL (Am J Surg Pathol 2012;36:462, Appl Immunohistochem Mol Morphol 2009;17:51)
- Pitfalls
- MDM2 and CDK4 can falsely stain endothelial cells, foamy macrophages and multinucleated giant cells; this means fat necrosis may be positive
- Care should be taken in problematic well differentiated lipomatous tumors (lipoma-like WDL versus lipoma), where sensitivity is particularly low; in such cases, FISH testing is preferred by some (Am J Surg Pathol 2016;40:1647)
- S100 (adipocytes in ~66% of cases)
- CD34 (some spindle cells)
- Desmin (rare cells are often identified)
Negative stains
Molecular / cytogenetics description
- Ring or giant marker / rod chromosomes derived from 12q13-15 in almost all cases
- Amplifications of the 12q12-21 (Virchows Arch 2012;461:67)
- MDM2 and CDK4, by FISH or real time PCR, can differentiate from other sarcomas (Hum Pathol 2006;37:1123, Am J Surg Pathol 2007;31:1476)
- See Am J Surg Pathol 2015;39:1433 for recommendations on when to utilize FISH in well differentiated tumors
- Carboxypeptidase M amplification has also been reported (Mod Pathol 2009;22:1541)
- Other rearrangements include amplifications of 10p11-14 and complex rearrangements involving chromosomes 8 and 12 (Virchows Arch 2012;461:67, Oncol Rep 2005;13:649)
Videos
Well differentiated liposarcoma / atypical lipomatous tumor mimicking lipoma
Well differentiated liposarcoma / atypical lipomatous tumor
Sample pathology report
- Retroperitoneal mass, resection:
- Well differentiated liposarcoma (7.5 cm) (see comment)
- No evidence of dedifferentiation
- Peripheral resection margins are positive for tumor
- Comment: Histologic sections of this retroperitoneal mass show a well differentiated fatty neoplasm with fibrotic bands containing rare enlarged, hyperchromatic cells. The malignant cells show strong nuclear expression of MDM2 by immunohistochemistry, supporting the diagnosis.
Differential diagnosis
- Inflammatory subtype of ALT / WDL
- Castleman disease:
- No well differentiated liposarcomatous component
- Absence of 12q13-15 amplification
- Hodgkin lymphoma:
- Inflammatory myofibroblastic tumor:
- No well differentiated liposarcomatous component
- Usually a highly cellular proliferation of SMA positive myofibroblasts associated with a dense lymphoplasmacytic infiltrate is seen
- Predilection for children and lack MDM2 gene amplification
- Nearly 50% are positive for ALK immunostaining secondary to ALK gene rearrangements (Mod Pathol 2001;14:569)
- Sclerosing mesenteritis or idiopathic retroperitoneal fibrosis:
- No well differentiated liposarcomatous component, lacks MDM2 gene amplification
- Beware fat necrosis, which can give the false impression of liposarcoma in this setting
- Look for increased IgG4 positive plasma cells to evaluate for IgG4 related disease (Mod Pathol 2012;25:1181)
- Castleman disease:
- Lipoma-like subtype of ALT / WDL
- Lipoblastoma:
- Usually age 3 or younger (Virchows Arch 2002;441:299)
- Lobular growth pattern with delicate branching vessels and myxoid change are characteristic
- Negative for 12q13-15 amplification; harbors PLAG1 rearrangements (Cancer Res 2000;60:4869)
- Classic lipoma:
- Typically superficial, lack atypical nuclei
- Use FISH in deep seated lesions where atypia may be sparse
- Molecular confirmation is particularly useful (Am J Surg Pathol 2015;39:1433):
- Recurrent tumors
- Deep extremity lesions > 10 cm in patients > 50 years old
- Cases with equivocal cytologic atypia
- Lesions in the retroperitoneum, pelvis or abdomen
- Molecular confirmation is particularly useful (Am J Surg Pathol 2015;39:1433):
- Lipomatous angiomyolipoma:
- HMB45+ epithelioid cells, negative for 12q13-15 amplification (Pathol Int 2006;56:638)
- Massive localized lymphedema:
- Clinically very different, localized in the proximal thigh of morbidly obese individuals (Mod Pathol 2016;29:75)
- Fat separated by widened edematous fibrous septa, with no cytologic atypia
- Other areas of compromised lymphatic drainage is also seen, such as lymphangiectasia in the overlying skin
- Lacks molecular findings of ALT / WDL (Am J Surg Pathol 1998;22:1277)
- Myxoid liposarcoma:
- Morphology may be similar but negative for 12q13-15 amplification (Mod Pathol 2009;22:223)
- Tends to have more lobular growth, delicate plexiform vasculature and signet ring lipoblasts
- Characterized by DDIT3 gene rearrangements
- Paraffinoma:
- History of paraffin injection, no atypical nuclei, negative for 12q13-15 amplification (Br J Radiol 2003;76:264)
- Silicone granuloma as a mimicker of ALT (Mod Pathol 2016;29:75, Int J Gynecol Pathol 2020;39:456)
- Perinephric myxoid pseudotumor of fat (Mod Pathol 2009;22:1196, Hum Pathol 2019;87:37)
- Spindle cell / pleomorphic lipoma:
- Frequently seen in the head and neck or other superficial soft tissues, look for ropey collagen and the absence of fibrillary stroma
- Have deletions of 16q / 13q and do not have amplification of 12q13-15 (Am J Surg Pathol 2012;36:1119)
- Loss of RB1 by IHC staining (Am J Surg Pathol 2012;36:1119)
- Lipoblastoma:
- Sclerosing subtype of ALT / WDL
- Atypical spindle cell lipomatous tumor (Am J Surg Pathol 2017;41:234)
- Dedifferentiated liposarcoma:
- Nonlipogenic high grade sarcoma that still retains molecular characteristics of WDL
- Typically shows abrupt transition between well differentiated and dedifferentiated components
- Rarely can have homologous lipoblastic differentiation where the dedifferentiated component morphologically resembles pleomorphic liposarcoma (Histopathology 2013;62:702)
- Concept of low grade dedifferentiation is controversial but generally has cellularity between that seen in WDL and DDL (Pathol Int 2001;51:392)
- Lipomatous hemangiopericytoma (solitary fibrous tumor with fatty differentiation) (Am J Surg Pathol 1999;23:1201):
Practice question #1
Practice answer #1
E. Well differentiated liposarcoma. Given the findings of a retroperitoneal mass composed of a proliferation of variably sized adipocytes intermixed with rare atypical cells characterized by enlarged, hyperchromatic nuclei, the best diagnosis is well differentiated liposarcoma. Evidence of MDM2 amplification by FISH testing supports the diagnosis. A is incorrect, since although deep seated and large lipomas can occur, these lesions lack atypical nuclei and do not have 12q13-15 amplification. B is incorrect because myxofibrosarcomas are extremely rare in the retroperitoneum and although low grade lesions have scattered cells with enlarged, hyperchromatic nuclei, they do not have 12q13-15 amplification. C is incorrect because myxoid liposarcoma tumor cells lack significant atypia, are typically evenly distributed in a prominent myxoid stroma with delicate branching vasculature and do not have 12q13-15 amplification. D is incorrect because pleomorphic lipomas are most frequently seen in the head and neck region and do not have 12q13-15 amplification.
Comment Here
Reference: Atypical lipomatous tumor / well differentiated liposarcoma
Comment Here
Reference: Atypical lipomatous tumor / well differentiated liposarcoma
Practice question #2
Which of the following is true about atypical lipomatous tumor / well differentiated liposarcomas (ALT / WDL)?
- Frequently present in the upper trunk / back of the neck in adults
- Have genomic alterations at 8q11-13
- Lack the ability to metastasize
- Must contain lipoblasts
- Show a predilection to metastasize to other soft tissue sites
Practice answer #2
C. Lack the ability to metastasize. ALT / WDL cannot metastasize unless it progresses to a dedifferentiated liposarcoma. A is incorrect because spindle cell lipomas show this predilection. B is incorrect because lipoblastomas have PLAG1 gene fusions, which is located at 8q11-13. D is incorrect since ALT / WDL neither need nor always have lipoblasts. E is incorrect because myxoid liposarcoma shows the unusual predilection among fatty tumors to metastasize to other soft tissue sites.
Comment Here
Reference: Atypical lipomatous tumor / well differentiated liposarcoma
Comment Here
Reference: Atypical lipomatous tumor / well differentiated liposarcoma