Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Virtual slides | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Malhotra S, Bhattarai N, Crane GM. BCL2. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsbcl2.html. Accessed October 5th, 2025.
Definition / general
- BCL2 gene: proto-oncogene located at chromosome 18q21.33 composed of 4 exons
- BCL2 protein: 25 kDa protein product of BCL2 gene
- Located in intracellular membranes, including the outer mitochondrial membrane, endoplasmic reticulum and nuclear envelope (Cell Death Differ 2013;20:785, Cancer Res 1993;53:4701)
- Serves antiapoptotic function by preventing leakage of cytochrome c and other apoptotic triggers into the cytoplasm
Essential features
- BCL2 gene encodes the BCL2 protein, which is a prosurvival protein that inhibits apoptosis
- BCL2 dysregulation can provide a survival advantage to neoplastic cells, as in follicular lymphoma, where t(14;18) results in juxtaposition of the IGH and BCL2 genes and overactivation of the BCL2 gene
- Certain antineoplastic drugs, such as venetoclax, act by inhibiting BCL2 protein function and are used in many hematologic neoplasms
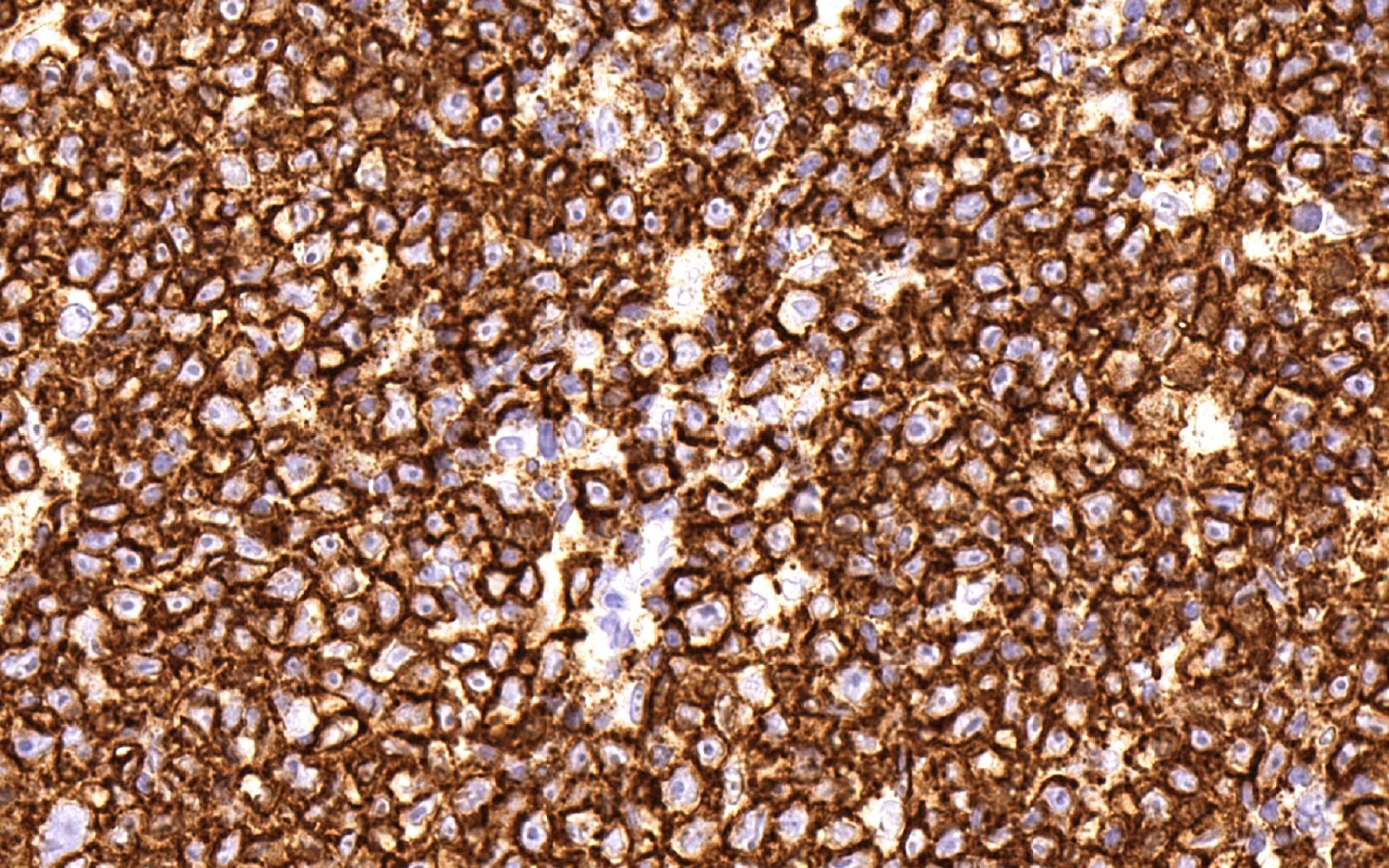
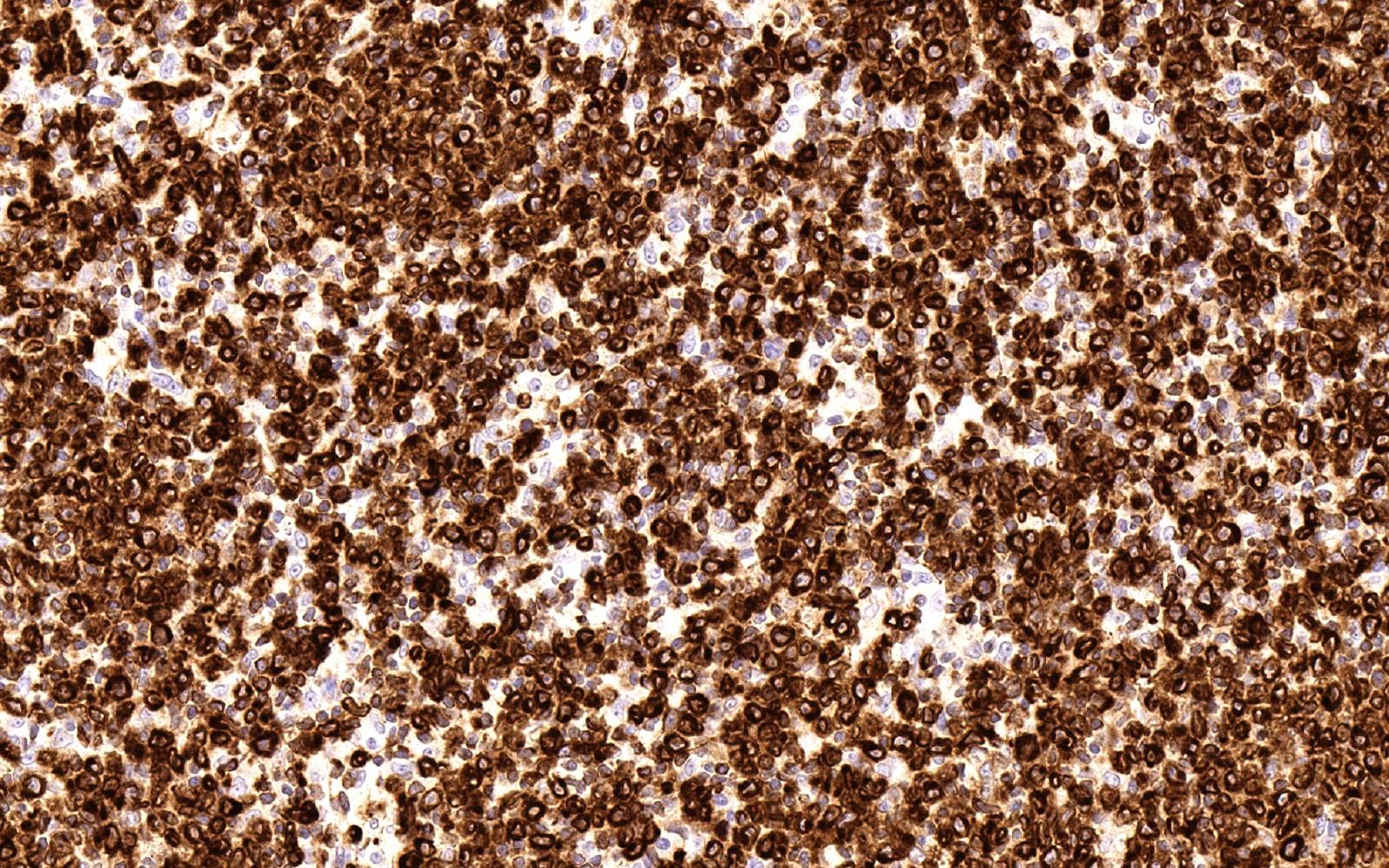
- BCL2 shows cytoplasmic and membranous positivity; expression in > 50% of large B cell lymphoma cells may be interpreted as positive
Terminology
- B cell lymphoma 2
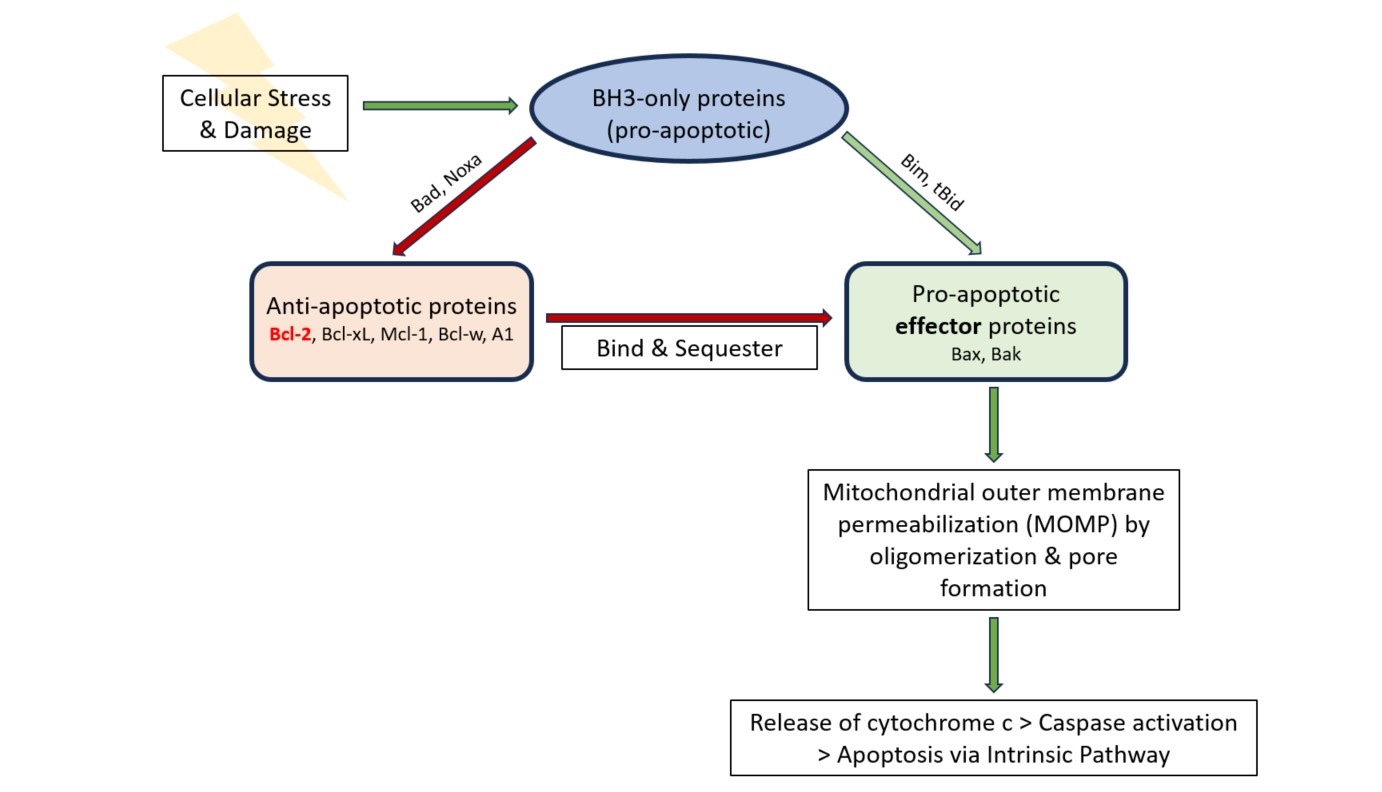
Pathophysiology
- BCL2 is a key member of the Bcl2 family of apoptosis regulating proteins, which also includes BCL-XL, BCL-W, MCL1, A1, BCL-B (Apoptosis 2023;28:20)
- Prosurvival proteins, such as BCL2, bind and suppress proapoptotic proteins, Bim, Bax and Bak
- In the absence of this suppression, the Bax / Bak proteins form pores in the mitochondrial membrane, resulting in the release of proapoptotic molecules such as cytochrome c
- Cytochrome c activates multiple downstream caspases that harbor proteolytic activity and eventually lead to cell death
- Downstream effect of Epstein-Barr virus latent membrane protein 1 (LMP1) is enhancement of BCL2 expression, leading to prolonged lifespan for B cells (Cancer Manag Res 2020;12:8801, J Virol 1994;68:5602)
- See Diagrams / tables
Clinical features
- Originally described 6 hallmarks of cancer include (Cancer Discov 2022;12:31, Cell 2011;144:646)
- Sustaining proliferative signaling
- Evading growth suppressors
- Activating invasion and metastasis
- Enabling replicative immortality
- Inducing angiogenesis
- Resisting cell death
- In cancer cells, accumulation of DNA damage with rapid proliferation and signaling imbalances can act as intracellular apoptosis triggers
- Several of the apoptosis regulating proteins interact through shared BH3 (BCL2 homology domain 3) domains / motifs; BH3 mimetics, such as venetoclax, exert anticancer effect by liberating the proapoptotic proteins (such as Bax and Bak) from their binding sites with prosurvival proteins (such as BCL2), thus allowing apoptosis to proceed (Cancers 2020;12:3353)
- BCL2 dysregulation occurs in various hematologic malignancies through different mechanisms (see table below)
- BCL2 dysregulation has also been described in myelodysplastic syndrome (MDS), acute myeloid leukemia (AML) and multiple myeloma with t(11;14) (Leukemia 2016;30:761)
- Venetoclax is used as a therapeutic drug in some of these entities (such as myelodysplastic syndrome and acute myeloid leukemia) and is being investigated for use in others (Am J Hematol 2023;98:1307, Hematology 2024;29:2343604, Curr Oncol 2022;29:4117)
- Several other drugs with a similar mechanism of action are also being investigated for potential clinical use (Blood 2021;138:1120)
Adapted from Int J Mol Sci 2021;22:10157Disease Molecular mechanism(s)
of BCL2 dysregulationProportion of patients
with the aberrationFollicular lymphoma t(14;18)(q32;q21) 90% BCL2 mutations Diffuse large B cell lymphoma,
germinal center B cell typet(14;18)(q32;q21) 30% BCL2 mutations 10% Hypermutation of BCL2 promoter Diffuse large B cell lymphoma,
activated B cell type18q21 amplifications 20% t(14;18)(q32;q21) 5% Mantle cell lymphoma 18q21 gain 20% Chronic lymphocytic leukemia 13q14 deletion with loss of negative
regulatory miRNA-15a / 16-1 of BCL250%
Interpretation
- Membranous and cytoplasmic (Hematol Rep 2011;3:e26)
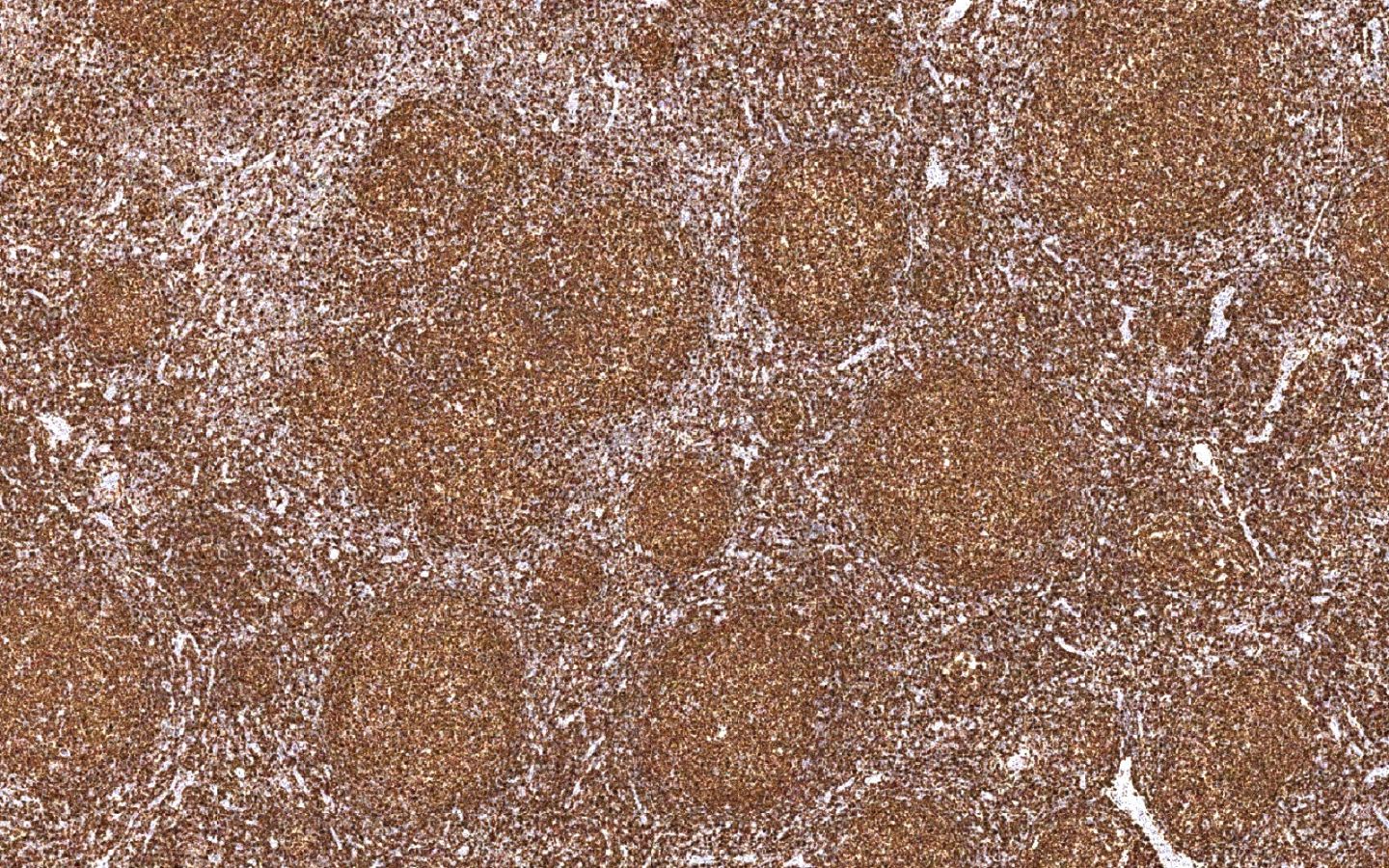
- Threshold to call positive in large B cell lymphomas is ≥ 50%
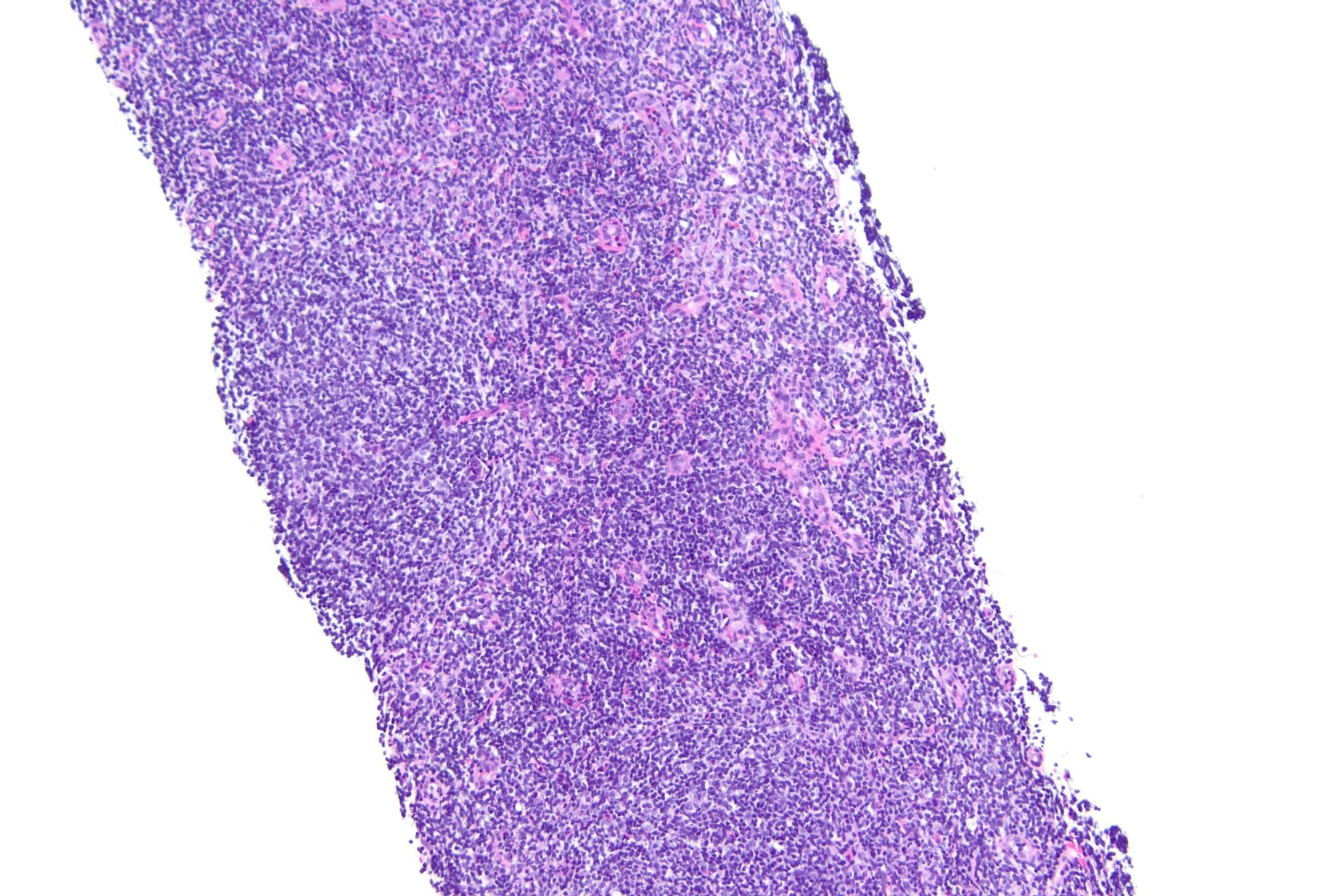
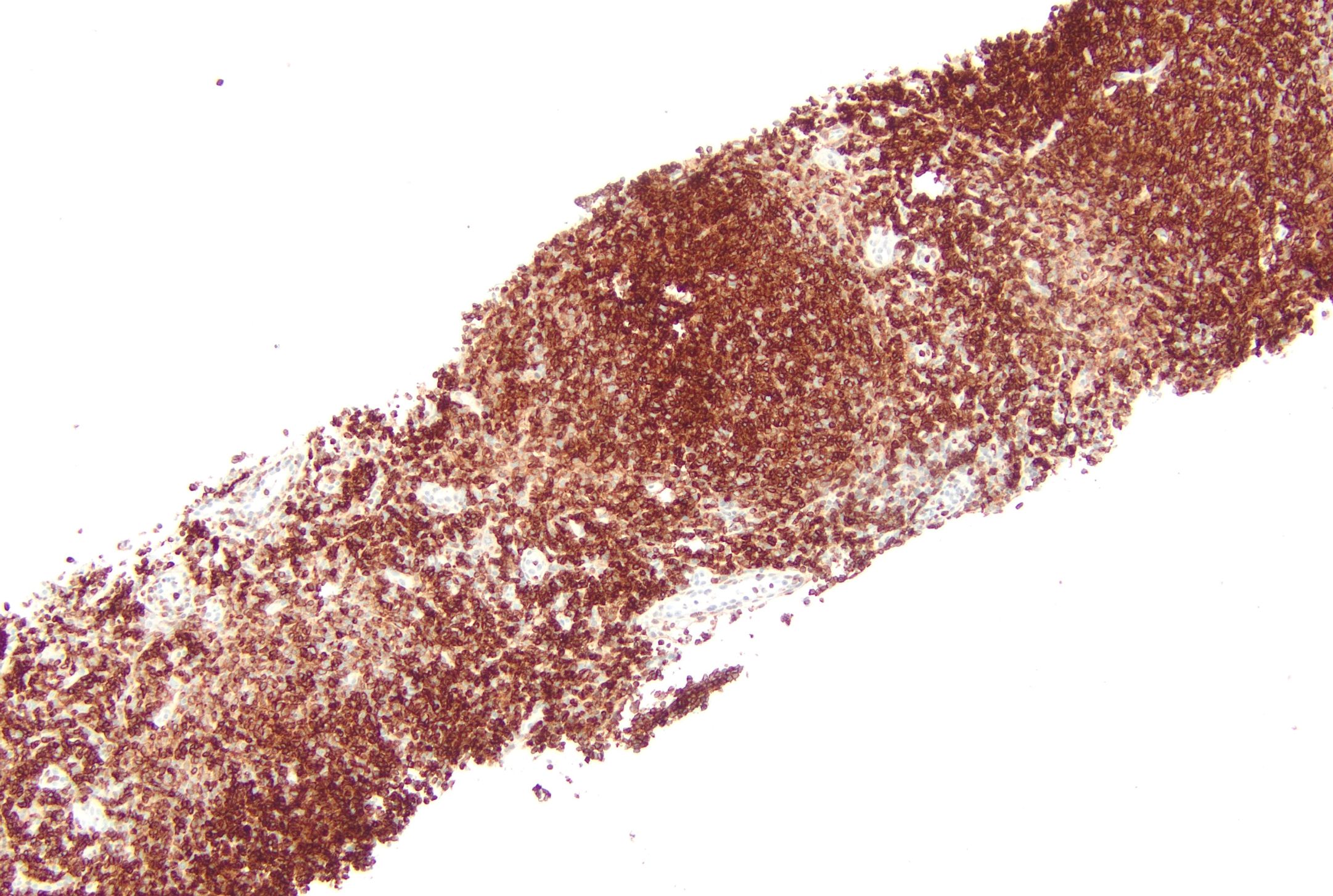
Uses by pathologists
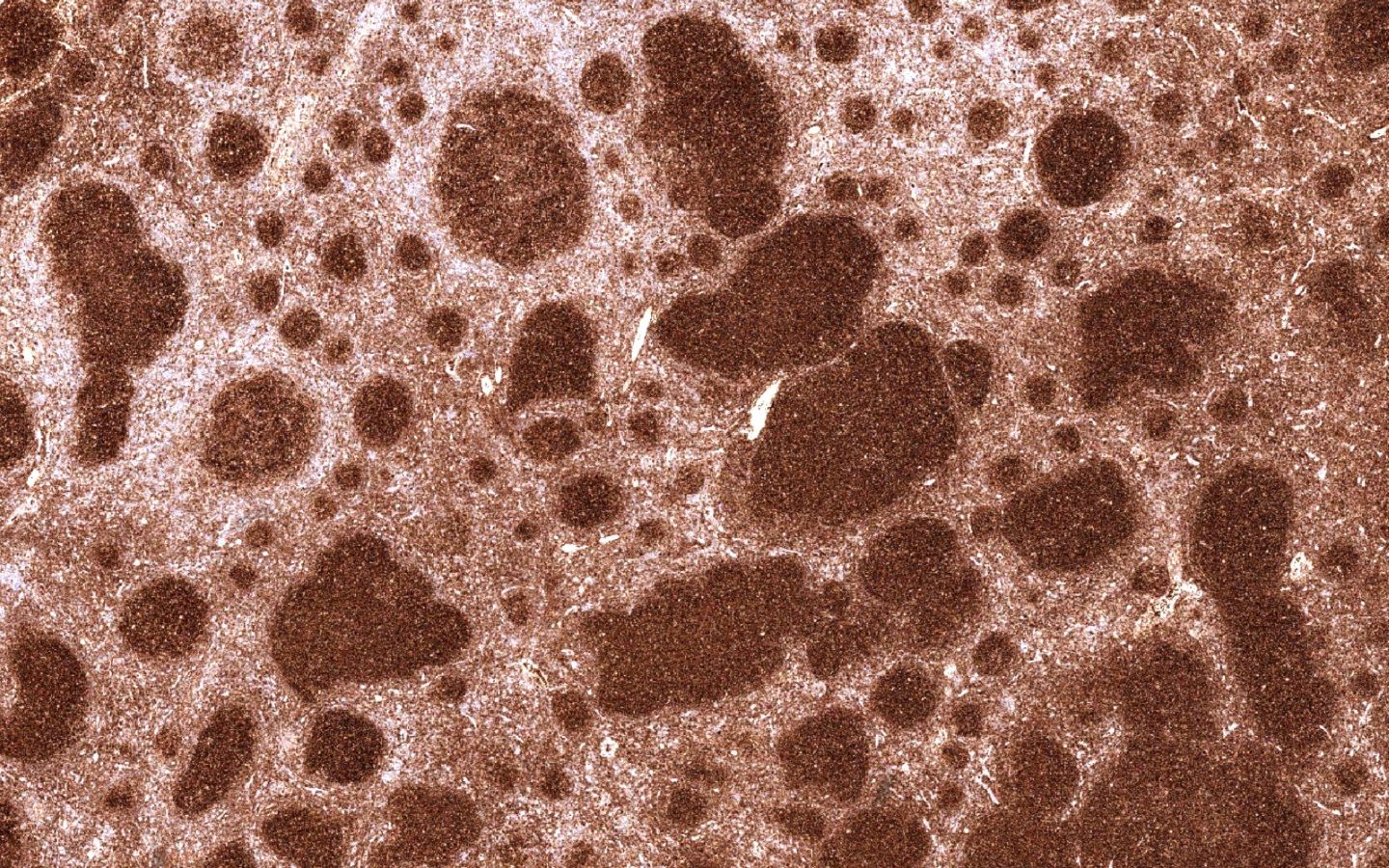
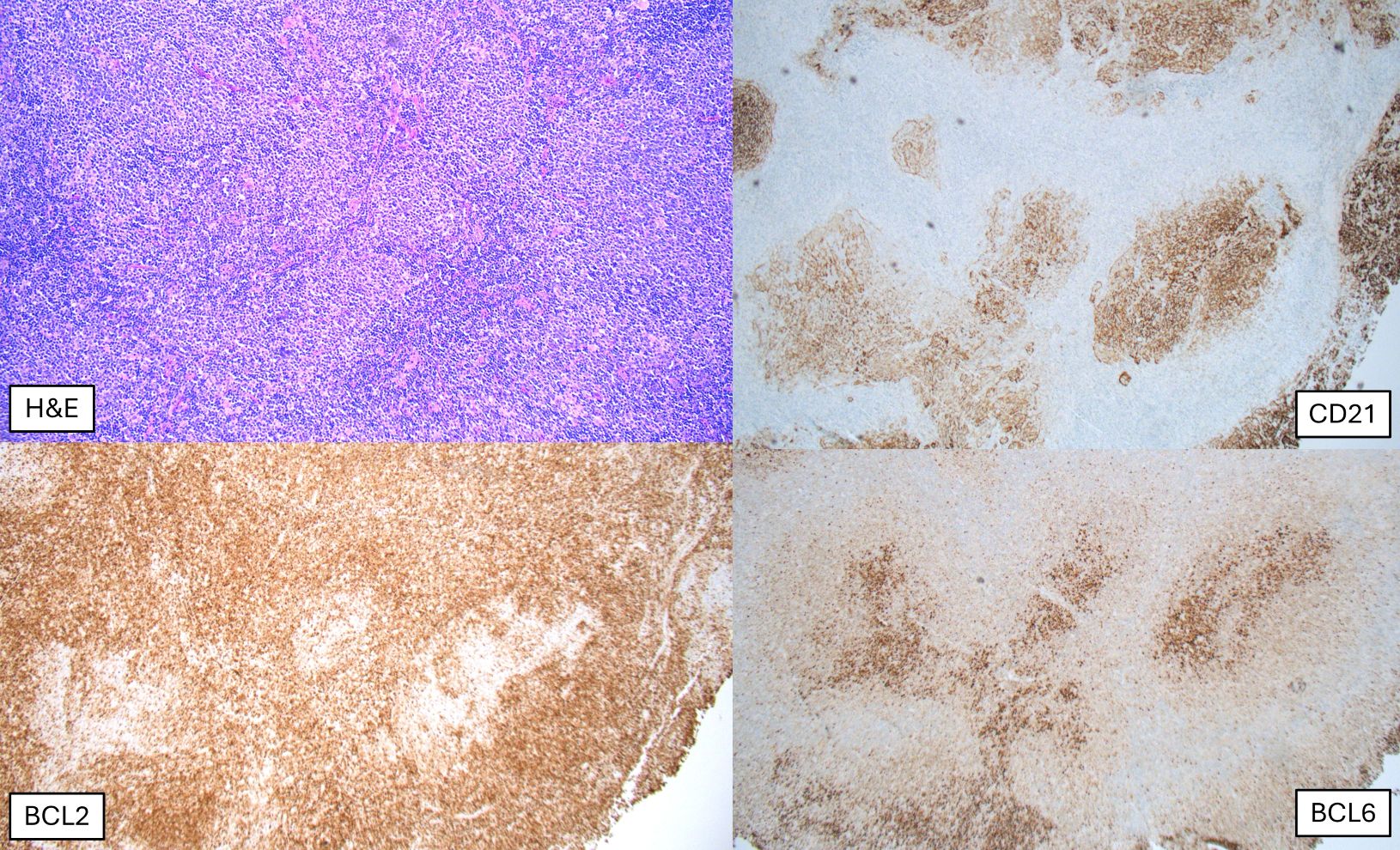
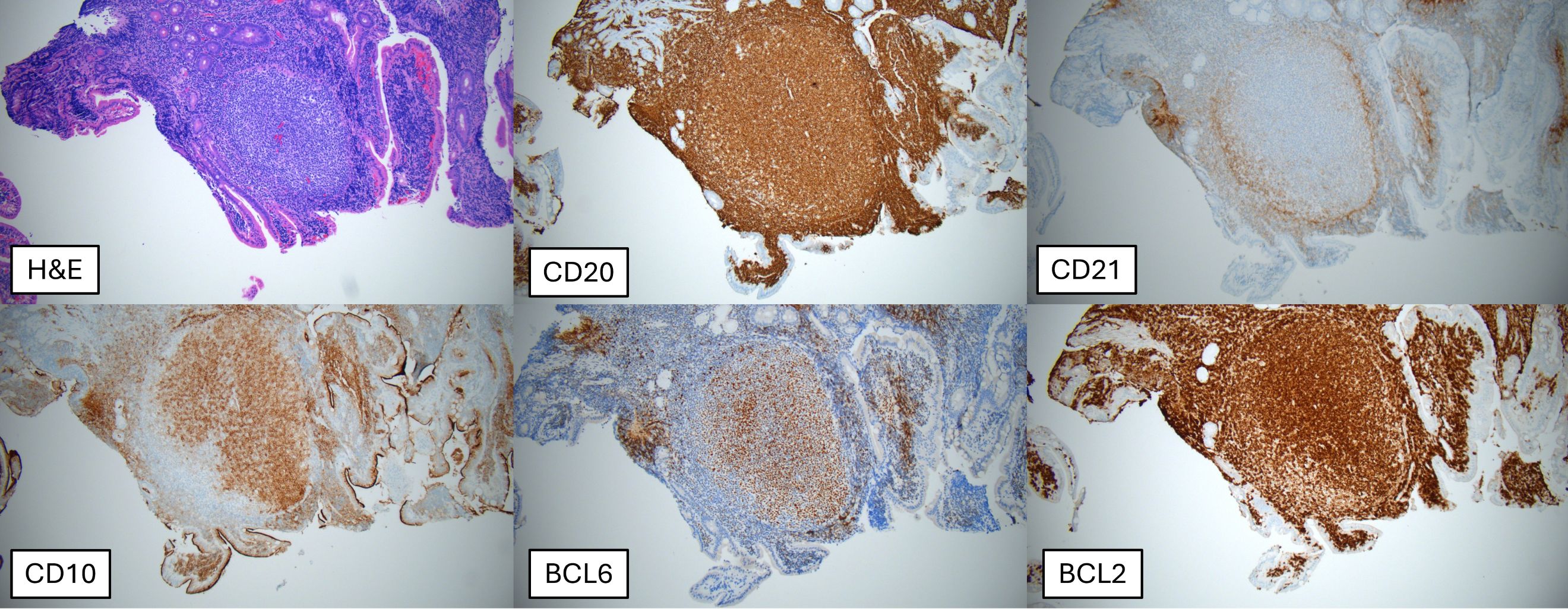
- Diagnosing follicular lymphoma: coexpression of BCL2 with germinal center markers such as BCL6, CD10, MEF2B, HGAL, GCET1 or LMO2 supports the diagnosis of follicular lymphoma over follicular hyperplasia
- Diagnosing diffuse large B cell lymphomas (DLBCL) / high grade B cell lymphomas (HGBCL) with MYC and BCL2 rearrangements (WHO 5th edition)
- Alternatively named high grade B cell lymphoma, double hit (HGBCL DH BCL2) (ICC 2022): immunohistochemical coexpression of BCL2 (≥ 50%) and MYC (≥ 40%) proteins (double expressors) in diffuse large B cell lymphomas is suggestive of concurrent MYC and BCL2 gene rearrangements (Mod Pathol 2018;31:1470)
- Diagnosing high grade B cell lymphomas, triple hit (HGBCL TH), which are aggressive large B cell lymphomas with coexisting MYC, BCL2 and BCL6 gene rearrangements
- Diagnosing T cell lymphomas: loss of BCL2 expression may be seen in T cell lymphomas (Appl Immunohistochem Mol Morphol 2014;22:99)
- Detecting immature enteric ganglion cells in pediatric intestinal pseudo-obstruction (Am J Surg Pathol 2005;29:1017)
- Ruling out Burkitt lymphoma: strong BCL2 expression is not compatible with a diagnosis of Burkitt lymphoma (Cytometry B Clin Cytom 2020;98:412)
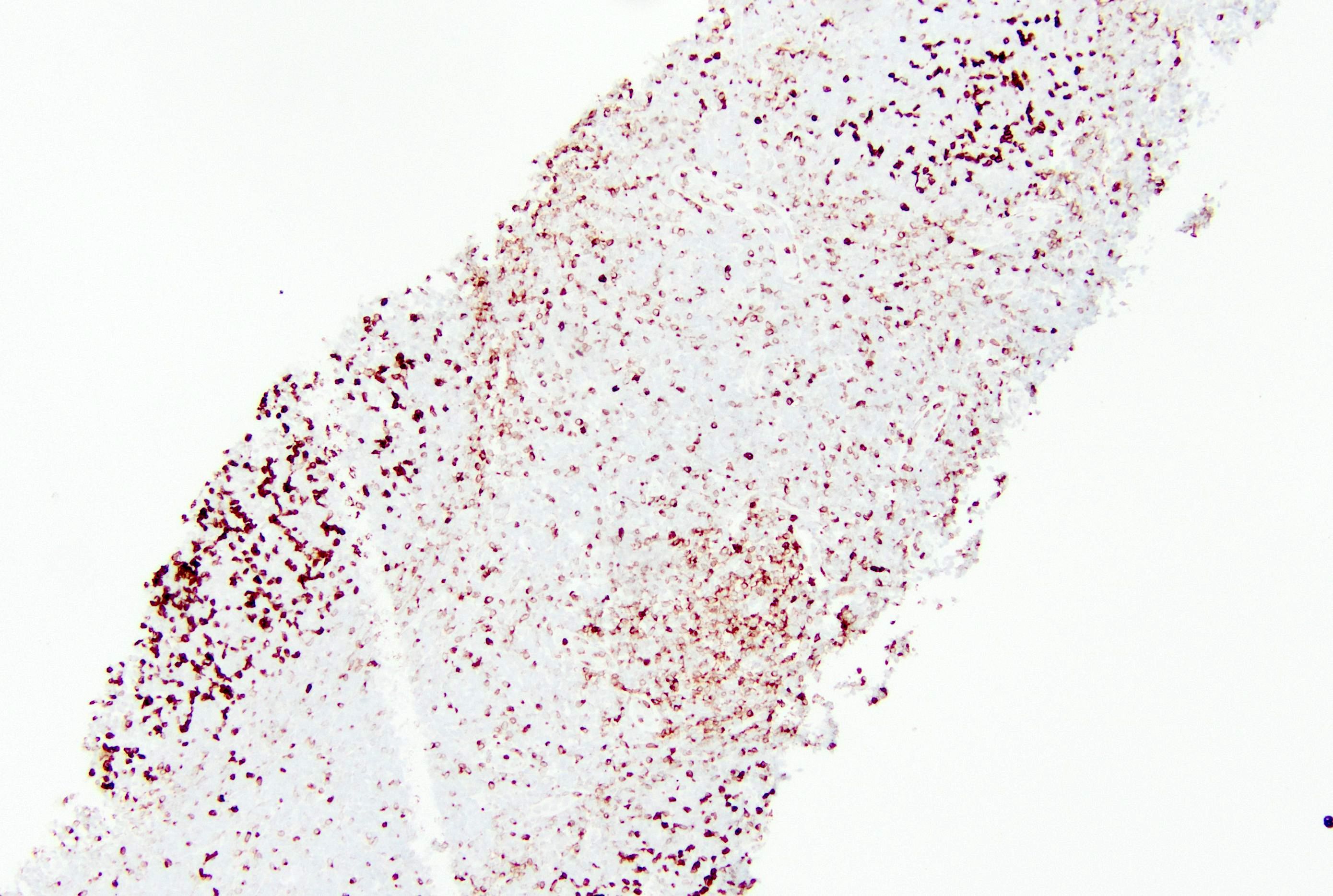
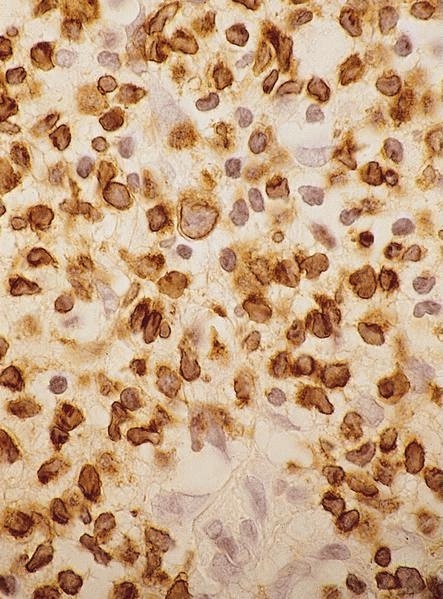
- Using an alternate BCL2 antibody clone may be useful in some cases of suspected follicular lymphomas that do not demonstrate BCL2 expression on initial immunohistochemical studies, which is usually due to mutations in BCL2 gene (Hum Pathol 2023;135:84)
- In particular, multiple antibody clones are available for immunohistochemical assessment of BCL2; these include (Hum Pathol 2013;44:1817)
- Clone 124 (mouse monoclonal antibody): one of the first to be used clinically and raised against amino acids 41 to 54 of the BCL2 protein; may yield false negative results due to epitope masking as a result of the translocation or mutations in the BCL2 gene impacting the protein structure (Pathology 2010;42:212)
- E17 (raised to an adjacent region of BCL2, corresponding to amino acids 61 - 76), EP36 and SP66 (rabbit monoclonal antibodies) may detect a subset of apparently BCL2- cases by the 124 clone and in DLBCL (Hum Pathol 2021;107:1, Pathology 2010;42:212, Hum Pathol 2014;45:2144, Hum Pathol 2023;135:84)
Prognostic factors
- Grading follicular lymphoma: BCL2 gene rearrangement supports diagnosis of grade 3A follicular lymphoma over grade 3B follicular lymphoma (Best Pract Res Clin Haematol 2011;24:111)
- Prognostication of breast cancer: BCL2 expression (strong positivity in > 10% of neoplastic cells) is a favorable prognostic factor in ER+ / HER2- breast cancers (J Breast Cancer 2017;20:54)
- High grade B cell lymphomas, double hit / triple hit, have an aggressive clinical course (Blood 2020;135:1759)
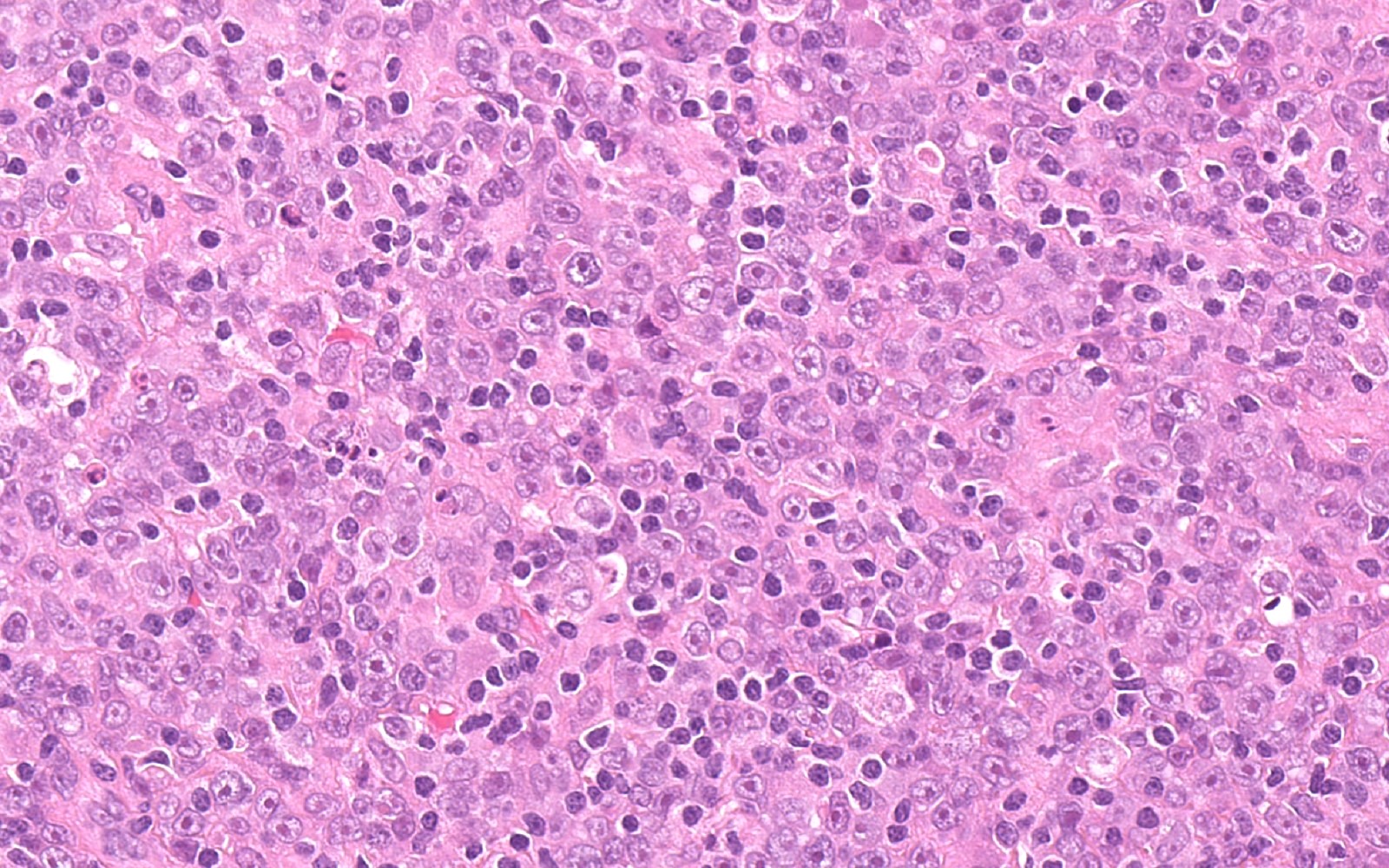
Microscopic (histologic) images
Contributed by Shikha Malhotra, M.B.B.S., M.D., Genevieve M. Crane, M.D., Ph.D. and AFIP
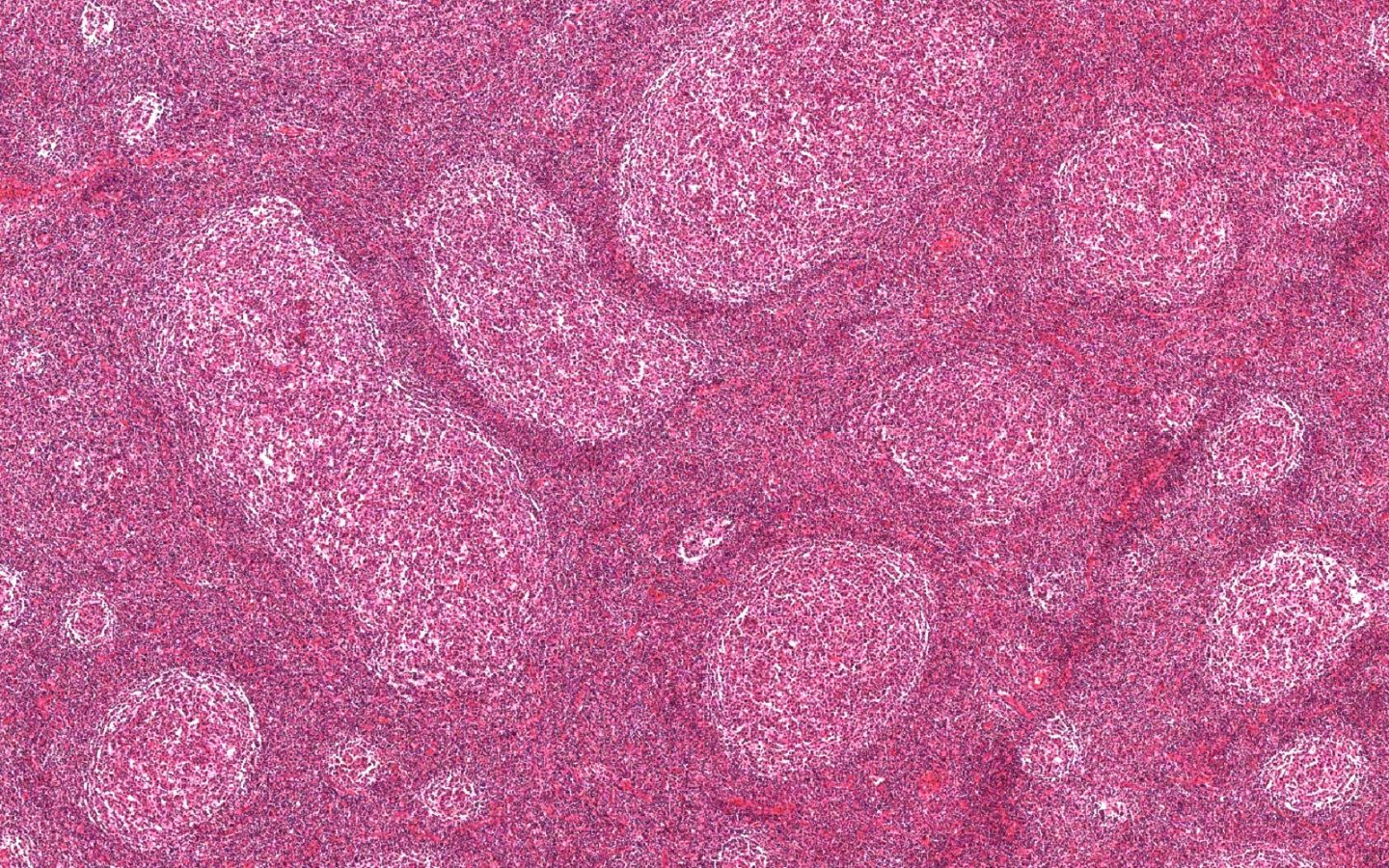
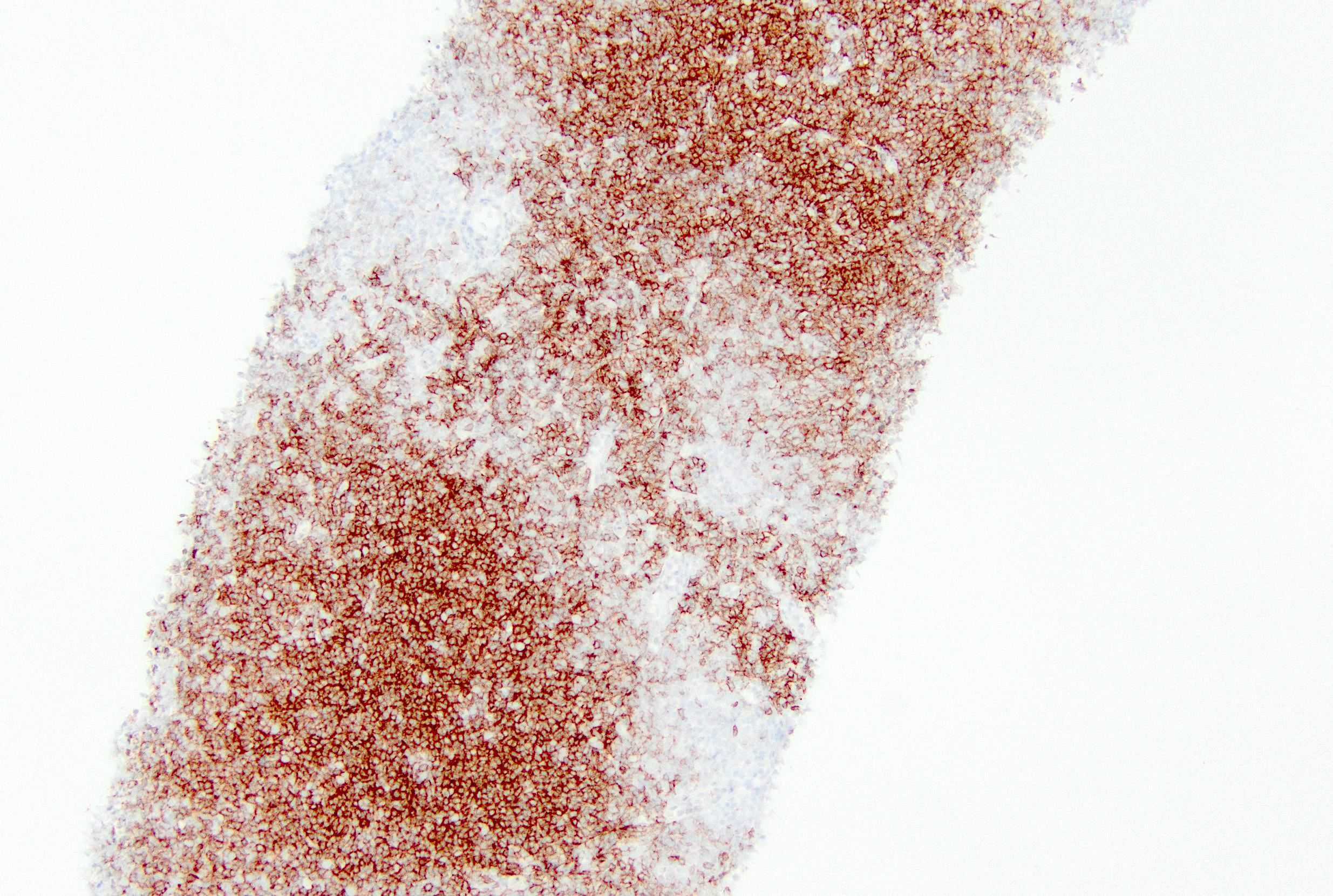
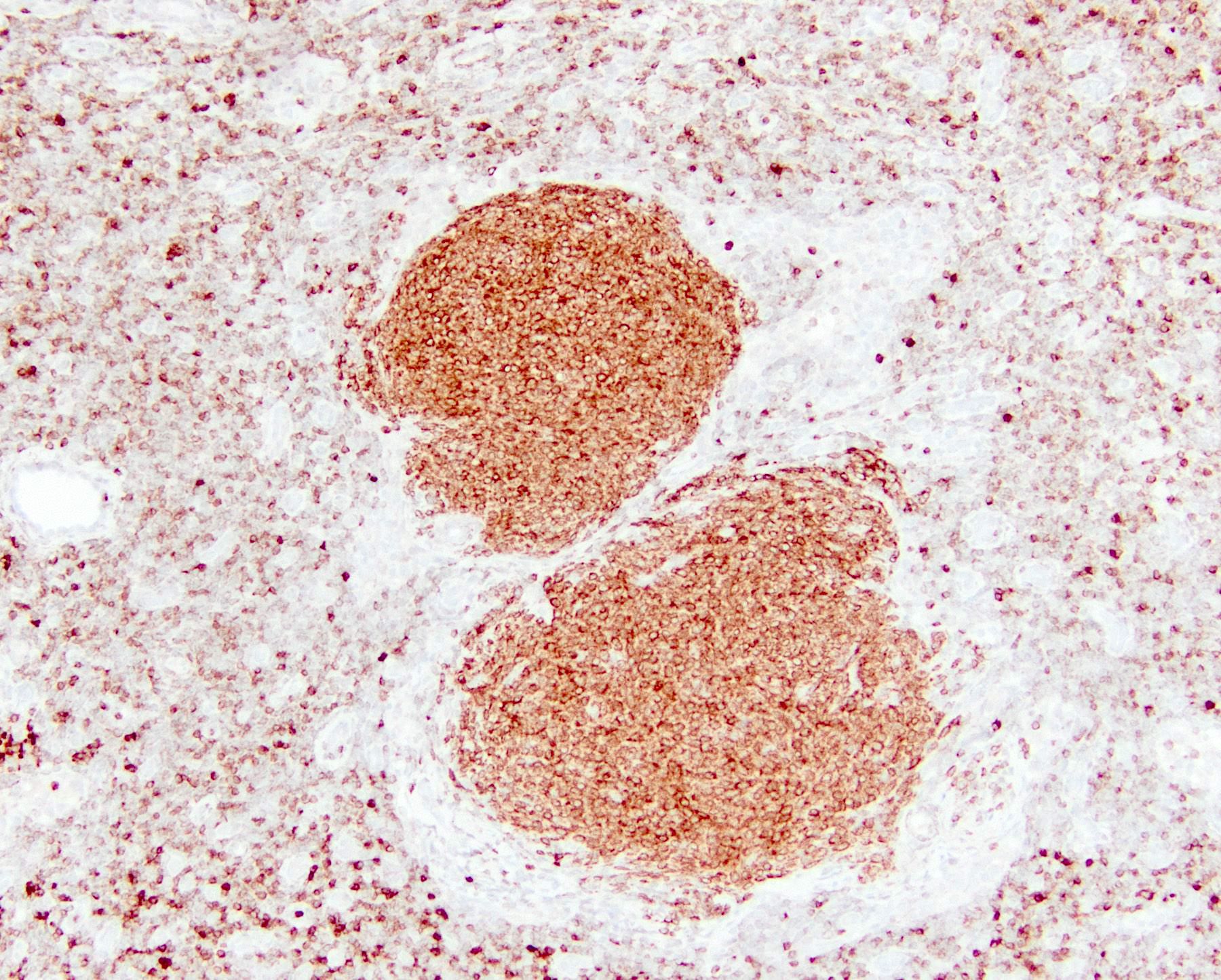
Positive staining - normal
- Lymph node: T cells; B cells of primary follicles, mantle zone B cells and interfollicular B cells
- Adrenal cortex and medulla
- Melanocytes
- Medullary thymocytes
- References: Blood 2017;130:489, Leuk Res 2011;35:256
Positive staining - disease
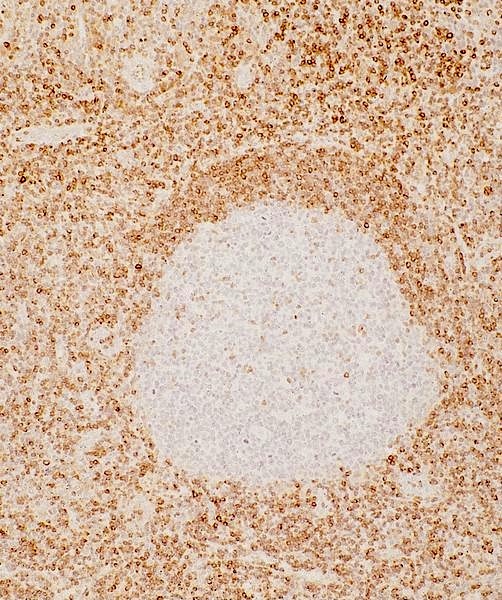
- In situ follicular B cell neoplasm (ISFN): this entity is defined as partial or complete colonization of reactive germinal centers by neoplastic follicular B cells with IGH::BCL2 fusion and hence shows strong aberrant BCL2 expression in the germinal centers of the involved follicles (see In situ follicular B cell neoplasm)
- B cell lymphomas (see Uses by pathologists) (Hum Pathol 2014;45:2144, Hum Pathol 2023;135:84)
- Certain spindle cell tumors including spindle cell lipoma, dendritic fibromyxolipoma, Kaposi sarcoma, solitary fibrous tumors, gastrointestinal stromal tumors and spindle cell component of synovial sarcoma (Histopathology 1998;33:508, Am J Surg Pathol 1998;22:863)
- Medullary thyroid carcinoma (79% of cases): positivity defined as expression in > 25% of neoplastic cells
- Absence of BCL2 expression is associated with poor prognosis (Hum Pathol 1995;26:945)
- Parathyroid adenomas (96% of cases): positivity defined as expression in > 50% neoplastic cells (Mod Pathol 1997;10:12)
- Adrenal tumors: both cortical and medullary tumors may demonstrate positivity (Mod Pathol 2003;16:591)
- Basal cell carcinomas: diffuse pattern (Am J Dermatopathol 1999;21:332)
Negative staining
- Certain spindle cell tumors such as desmoid fibromatosis, nodular fasciitis, fibromatosis and dermatofibroma, benign and malignant smooth muscle proliferations (Prz Gastroenterol 2019;14:79, Am J Surg Pathol 1998;22:863)
- Trichoepitheliomas: may show staining of outermost epithelial layer (Am J Dermatopathol 1999;21:332)
- Parathyroid carcinomas are mostly negative for BCL2 (Mod Pathol 1997;10:12)
Molecular / cytogenetics description
- Translocations involving 18q21.33 on karyotyping should raise suspicion for BCL2 gene rearrangements
- IGH::BCL2 fusion probes may be used in fluorescence in situ hybridization (FISH) studies aimed at recognizing the IGH::BCL2 fusion occurring due to t(14;18)(q32;q21) classically described in follicular lymphoma
- BCL2 gene rearrangement can be confirmed by interphase FISH studies using a BCL2 break apart probe, which is commonly included in most large B cell lymphoma FISH panels
- Using a break apart probe may help identify BCL2 gene rearrangement with partners other than IGH, such as IGK and IGL
- BCL2 mutations may lead to acquisition of resistance to BH3 mimetics / BCL2 inhibitors such as venetoclax
- References: Blood 2017;130:489, Leuk Res 2011;35:256
Molecular / cytogenetics images
Sample pathology report
- Lymph node, retroperitoneal, biopsy:
- Involvement by aggressive B cell lymphoma, germinal center B cell type (Hans criteria), pending ancillary testing (see comment)
- Comment: The findings are consistent with involvement by a CD10 positive aggressive B cell lymphoma. Additional testing is underway to exclude a possible double hit lymphoma and the diagnosis will be clarified in an addendum. Given the focal nodularity in the process as well as interspersed sclerosis, the possibility that this may have arisen from an underlying follicular lymphoma cannot be excluded. Please also correlate with concurrent flow cytometry.
- Biomarker results
- Cell of origin (Hans classifier): germinal center
- MYC expression (% tumor cells by IHC): < 40%
- BCL2 expression (% tumor cells by IHC): > 50%
- Ki67 expression (% tumor cells by IHC): 70 - 80%
Additional references
- NLM: BCL2 Apoptosis Regulator [Homo Sapiens (Human)] [Accessed 20 February 2025], Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Dabbs: Diagnostic Immunohistochemistry - Theranostic and Genomic Applications, 6th Edition, 2021, Swerdlow: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissue, Revised 4th Edition, 2017, WHO Classification of Tumours Editorial Board: Haematolymphoid Tumours, 5th Edition, 2024, Mod Pathol 2018;31:313, J Clin Oncol 2017;35:2515, Histol Histopathol 2001;16:1005
Practice question #1
Practice answer #1
B. Follicular lymphoma (FL). > 90% of follicular lymphoma is associated with an IGH::BCL2 rearrangement or t(14;18). This is termed classic follicular lymphoma in the WHO 5th edition. Follicular lymphoma is thought to arise from a germinal center B cell, which is normally negative for BCL2 expression. Aberrant expression by this rearrangement promotes survival. Answers A and D are both incorrect because these entities are not associated with the IGH::BCL2 rearrangement and are characteristically negative for BCL2 by immunohistochemistry, although weak or partial expression may be seen in some cases. Answer C is incorrect because the cells from which mantle cell lymphoma (MCL) arises are nongerminal center cells and normally express BCL2. In addition, mantle cell lymphoma is associated with the IGH::CCND1 rearrangement. Answer E is incorrect because small lymphocytic lymphoma may show a range of genetic alterations but is generally not associated with IGH::BCL2 rearrangement. These small lymphoid cells typically express BCL2 but not as an aberrant marker.
Comment Here
Reference: BCL2
Comment Here
Reference: BCL2
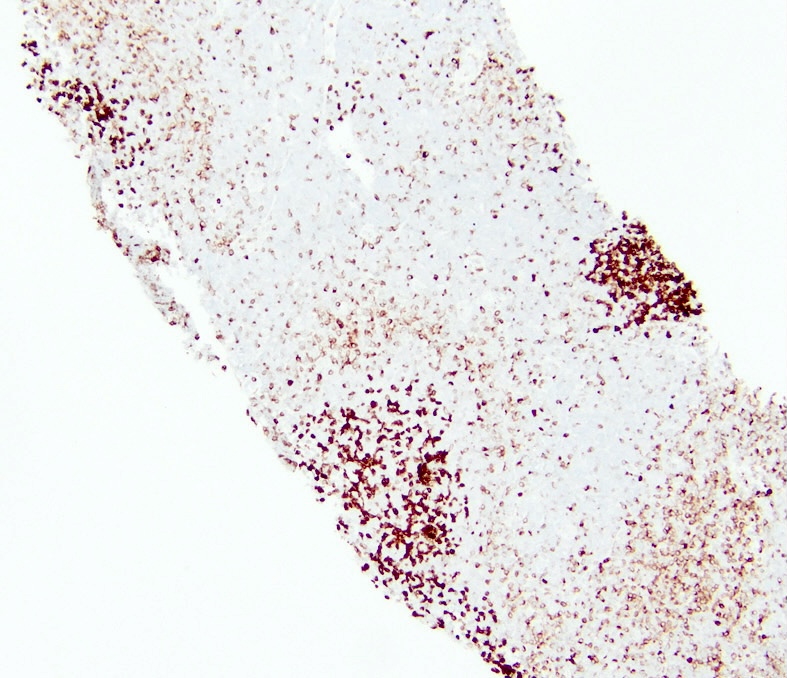
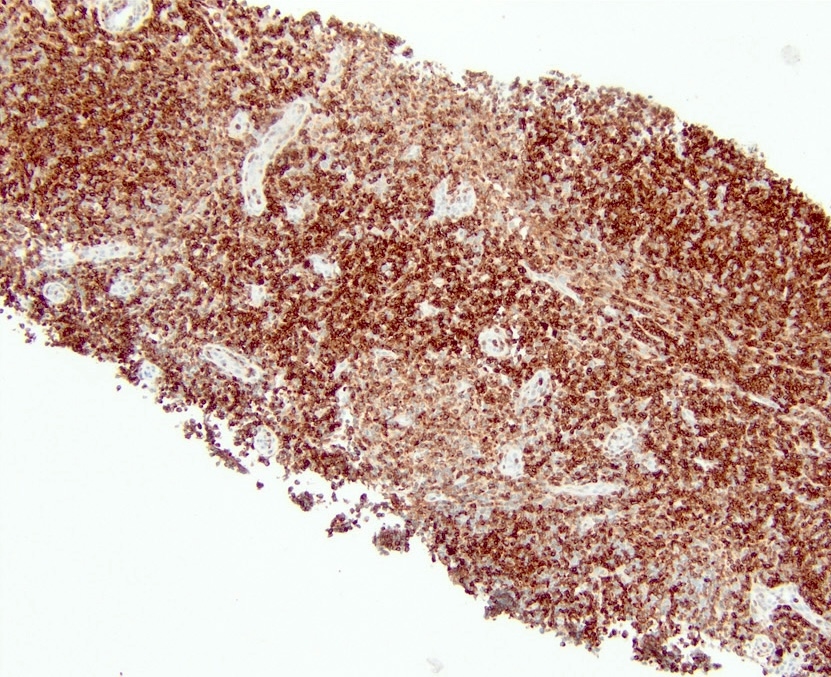
Practice question #2
Practice answer #2
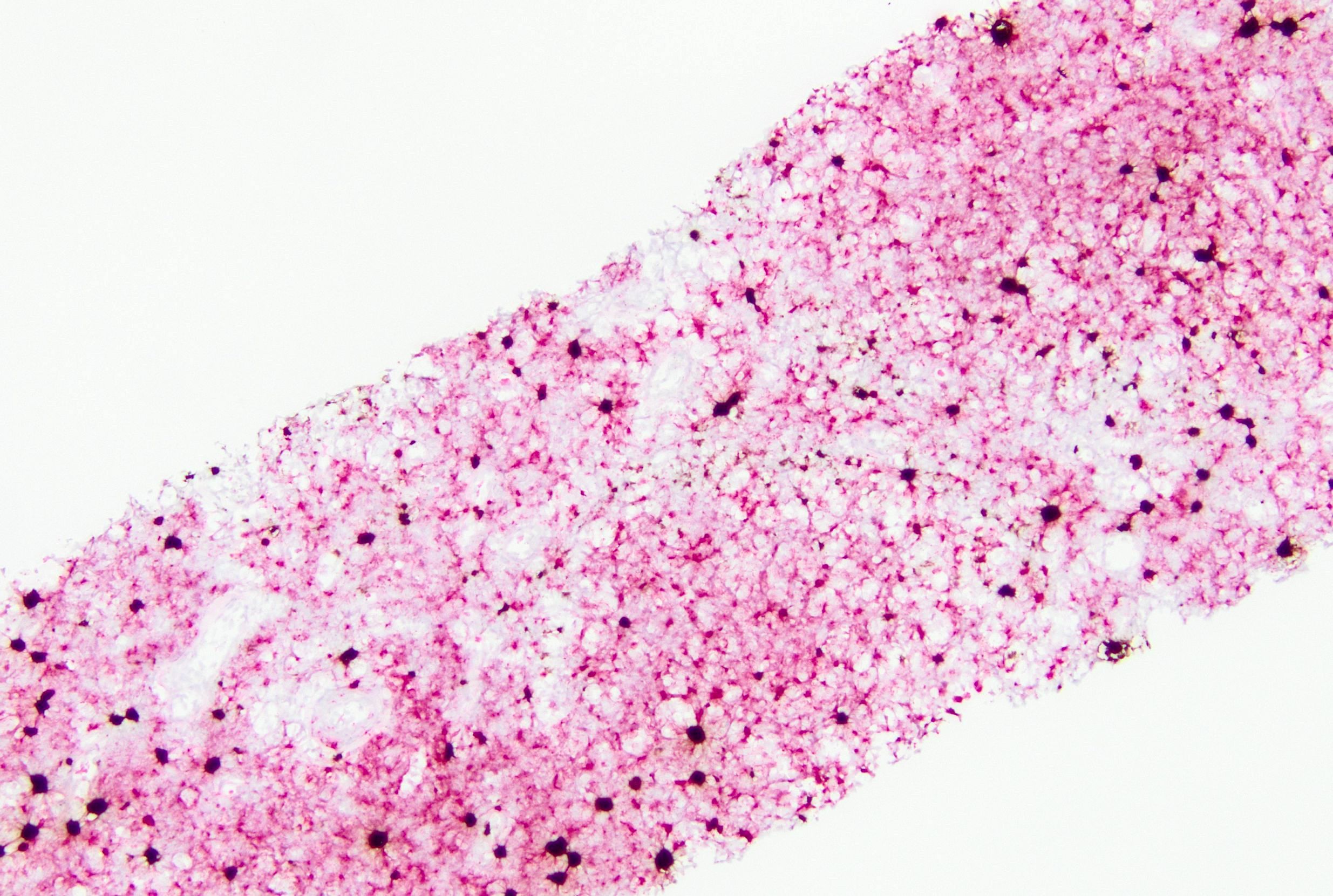
C. Mutations in the BCL2 gene or masking of BCL2 epitopes are common. Various studies report different frequencies of BCL2 gene mutations in follicular lymphoma, ranging from 12% to ~50% of total cases (Blood 2015;125:658, Blood Cancer J 2023;13:81). A subset of these mutations can result in alteration of the antibody clone binding site. Hence, follicular lymphoma may be positive for one BCL2 antibody clone but undetectable by another, as shown in the above images. Answers A, B and D are incorrect because while other issues with detection may occur, this phenomenon is not typically related to isoforms, variability in manufacture of the antibodies or cross reaction with BCL6. In particular, BCL6 is nuclear while BCL2 shows a cytoplasmic pattern.
Comment Here
Reference: BCL2
Comment Here
Reference: BCL2