Testis & paratestis
General
Staging
Last author update: 2 May 2022
Last staff update: 1 June 2023
Copyright: 2002-2024, PathologyOutlines.com, Inc.
PubMed Search:
Testis staging
Page views in 2023: 7,165
Page views in 2024 to date: 2,295
Cite this page: Zynger DL. Staging. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisstaging.html. Accessed April 19th, 2024.
Definition / general
- All testicular postpubertal germ cell tumors and malignant sex cord stromal tumors are covered by this staging system
- These topics are not covered: spermatocytic tumor, nonmalignant sex cord stromal tumor, prepubertal germ cell tumor, hematopoietic tumors and paratesticular tumors
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
Primary tumor (pT)
- pTX: cannot be assessed
- pT0: no evidence of primary tumor
- pTis: germ cell neoplasia in situ
- pT1: nonpure seminoma confined to testis / tunica albuginea / rete and no lymphovascular invasion (LVI)
- pT1a: seminoma < 3 cm confined to testis / tunica albuginea / rete and no LVI
- pT1b: seminoma ≥ 3 cm confined to testis / tunica albuginea / rete and no LVI
- pT2: lymphovascular, hilar fat, epididymal or tunica vaginalis invasion
- pT3: direct spermatic cord soft tissue invasion
- pT4: direct scrotum invasion
Notes:
- Size
- Largest aggregate tumor size should be obtained, encompassing all adjacent nodules, even with different gross appearances rather than regarding nodules as separate smaller tumors
- Seminoma is subclassified as pT1a / b based on a 3 cm threshold but nonpure seminoma is not
- LVI
- Freshly cut or minimally fixed testicular germ cell tumors have frequent tissue displacement artifact ("butter"), which confounds the diagnosis of true LVI (classified as pT2) (Am J Clin Pathol 2016;145:341)
- Care must be taken when grossing to decrease the amount of tissue displacement artifact and overnight fixation of a bivalved specimen may be helpful
- Histologic features supporting true LVI are tumor emboli that are cohesive, have smooth contours and adhere to the vessel wall (Am J Clin Pathol 2016;145:341)
- LVI of the spermatic cord is pT2 not pT3
- pT2
- Involvement of the tunica albuginea does not impact pT classification
- Tumor involvement of the tunica vaginalis is classified as pT2 and is rare (4/170, 2% seminoma; 0/148, 0% nonseminoma) (Histopathology 2018;73:741, Mod Pathol 2013;26:579)
- Epididymal invasion is uncommon (6% seminoma, 8% nonseminoma) and is classified as pT2; however, it is not associated with a higher clinical stage (Histopathology 2018;73:741, Mod Pathol 2013;26:579)
- Tumor within the soft tissue below the level of the epididymal head is considered hilar fat invasion and is classified as pT2
- pT3
- Tumor within the soft tissue beyond the angle between the epididymis and spermatic cord is classified as pT3
Regional lymph nodes (pN)
- pNX: cannot be assessed
- pN0: no regional lymph node metastasis
- pN1: 1 - 5 involved nodes with node size ≤ 2 cm
- pN2: > 5 involved nodes or extranodal extension or involved nodes > 2 cm and ≤ 5 cm
- pN3: lymph node mass > 5 cm
Notes:
- Regional lymph nodes = interaortocaval, para / periaortic, paracaval, preaortic, precaval, retroaortic and retrocaval nodes
- The size used to classify untreated lymph nodes is the overall lymph node size rather than the size of the metastatic deposit
- Per the AJCC chapter 1 regarding classification post therapy, "necrotic cells currently play no role in assigning the ypT and ypN"
- Therefore, size of the metastatic deposit rather than overall lymph node is recommended for use in classifying lymph nodes after therapy
- Additionally, most literature describes residual viable tumor size in lymph nodes post treatment rather than overall lymph node size (World J Urol 2021;39:1969, World J Urol 2021;39:839)
AJCC prognostic stage groups
- Stage group 0:pTis N0 M0 S0
- Stage group I:pT1 - 4 N0 M0 SX
- Stage group IA:pT1 N0 M0 S0
- Stage group IB:pT2 - 4 N0 M0 S0
- Stage group IS:pT1 - 4,X N0 M0 S1 - 3
- Stage group II:pT1 - 4,X N1 - 3 M0 SX
- Stage group IIA:pT1 - 4,X N1 M0 S0 - 1
- Stage group IIB:pT1 - 4,X N2 M0 S0 - 1
- Stage group IIC:pT1 - 4,X N3 M0 S0 - 1
- Stage group III:pT1 - 4,X N0 - 3 M1 SX
- Stage group IIIA:pT1 - 4,X N0 - 3 M1a S0 - 1
- Stage group IIIB:pT1 - 4,X N1 - 3M0 S2;pT1 - 4,XN0 - 3M1aS2
- Stage group IIIC:pT1 - 4,X N1 - 3M0S3; pT1 - 4,XN0 - 3 M1aS3; pT1 - 4,X N0 - 3M1bS0 - 3
Notes:
- While discontinuous spermatic cord invasion is classified as pM1 per the AJCC thus rendering the patient stage III, the National Comprehensive Cancer Network (NCCN) guidelines do not agree with the designation of discontinuous spermatic cord invasion as pM1 but instead as pT3 (J Natl Compr Canc Netw 2019;17:1529)
Registry data collection variables
- Serum tumor markers (AFP, hCG, LDH)
Histologic grade (G)
- Germ cell tumors are not graded
Histopathologic type
- Seminoma
- Nonseminoma
- Embryonal carcinoma
- Yolk sac tumor
- Teratoma
- Choriocarcinoma
- Mixed germ cell tumor
- Malignant Leydig cell tumor
- Malignant Sertoli cell tumor
- Malignant sex cord stromal tumors, other types
Notes:
- 60% of testicular germ cell tumors are seminoma
- Within a mixed germ cell tumor, frequency of tumor type is: embryonal carcinoma > teratoma, yolk sac tumor, seminoma > choriocarcinoma > other rare types (Med Oncol 2018;35:21)
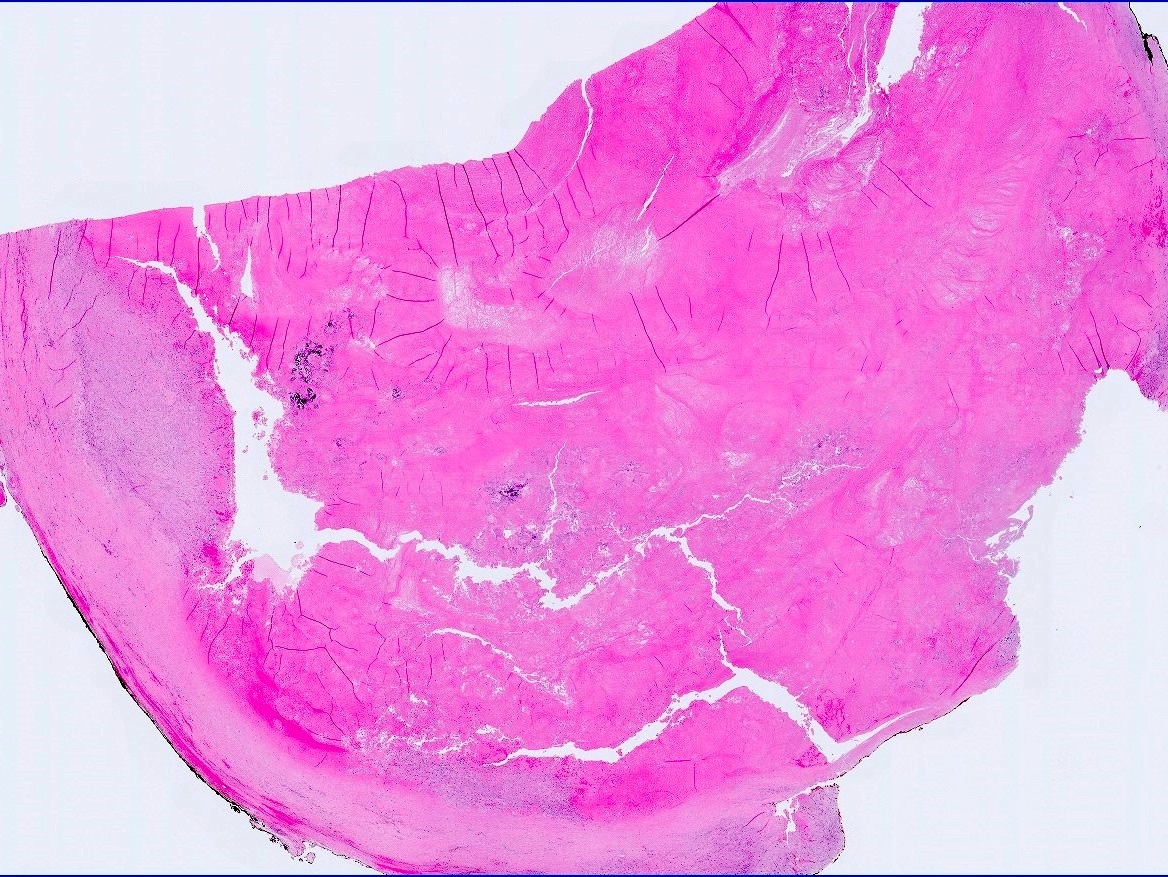
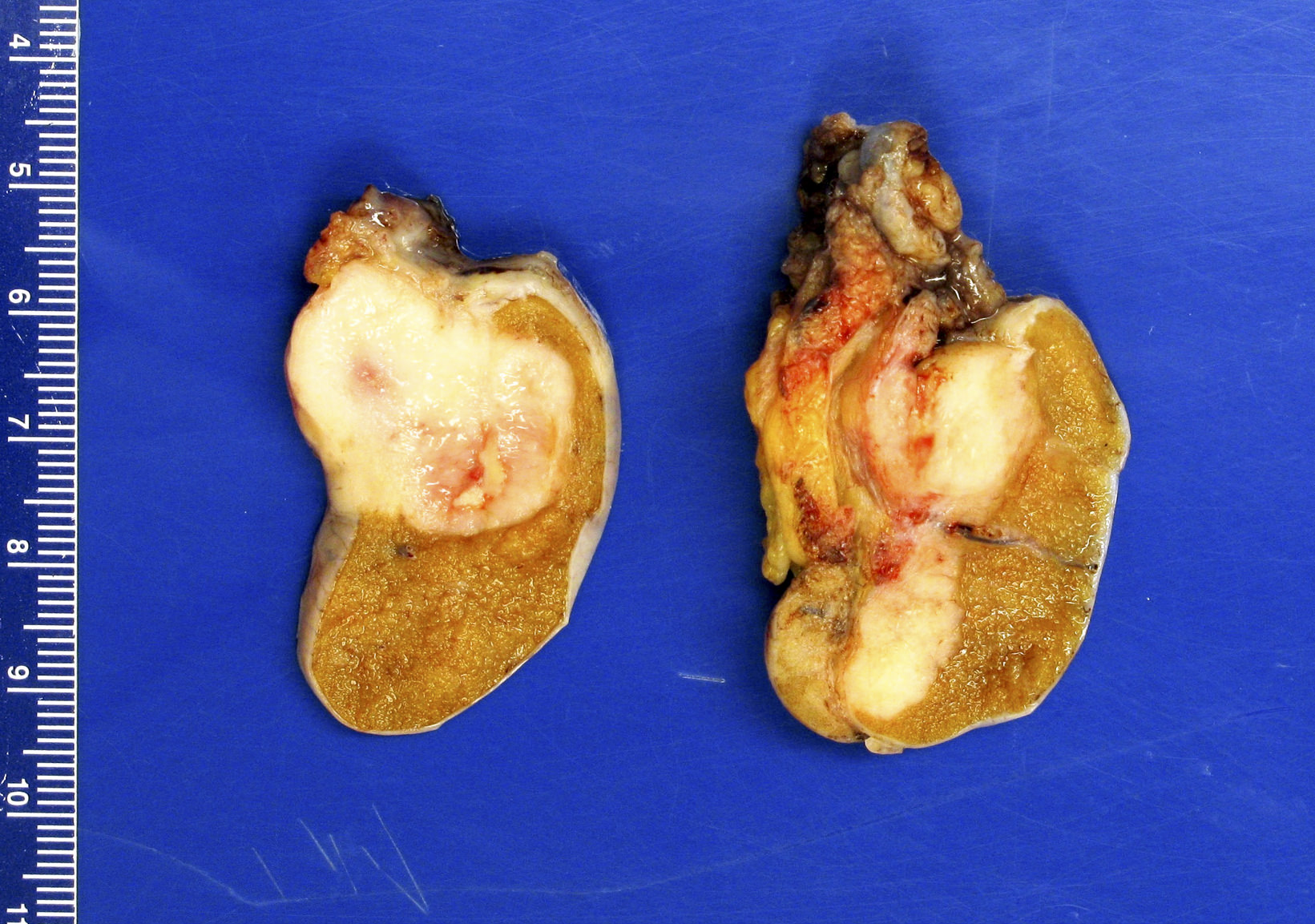
Gross images
Contributed by Debra L. Zynger, M.D.

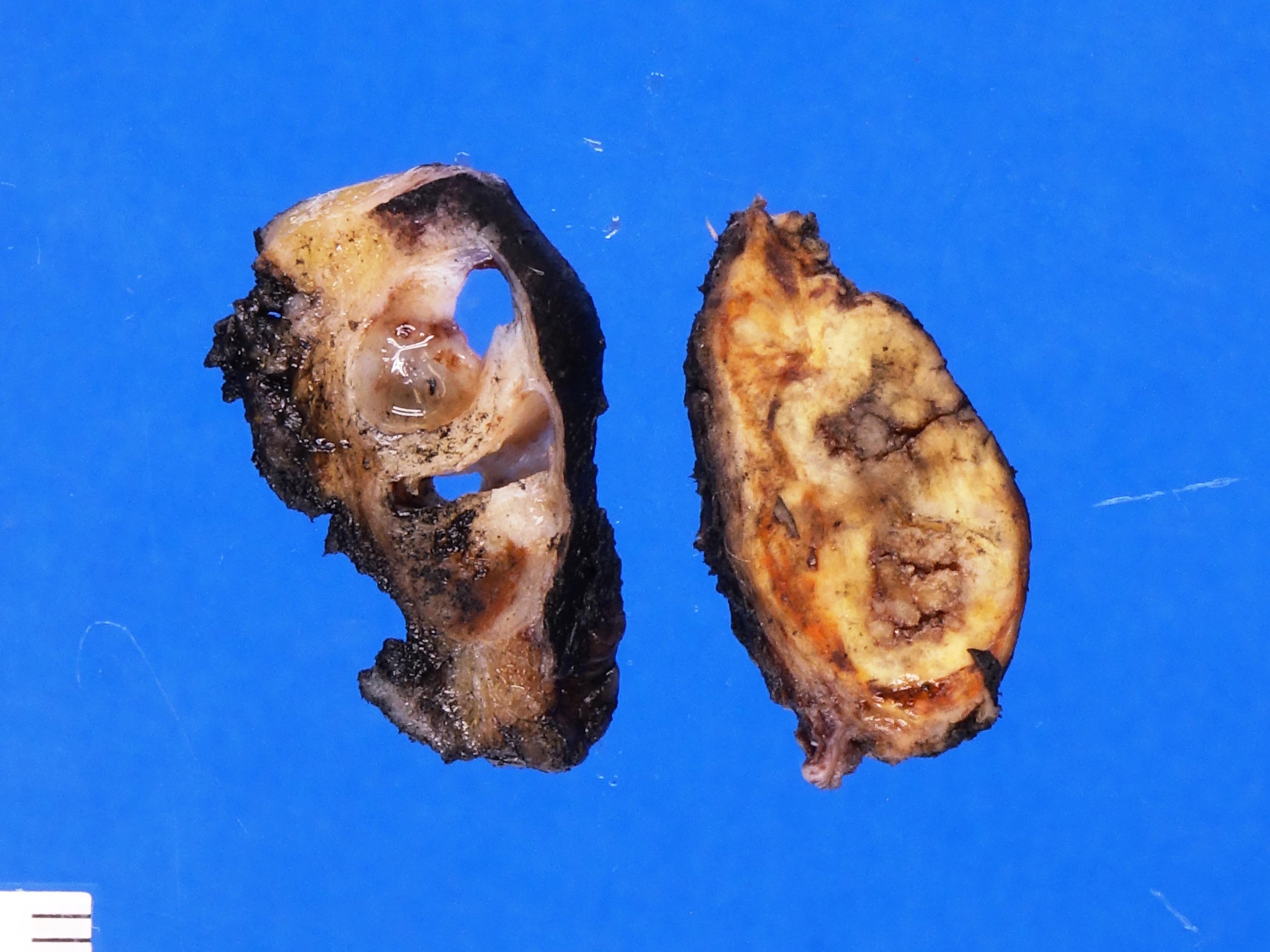
Complete regression (pT0)

Germ cell neoplasia in situ only (pTis)

Partial regression (pT1)

Teratoma (pT1)

Teratoma and EC (pT1)

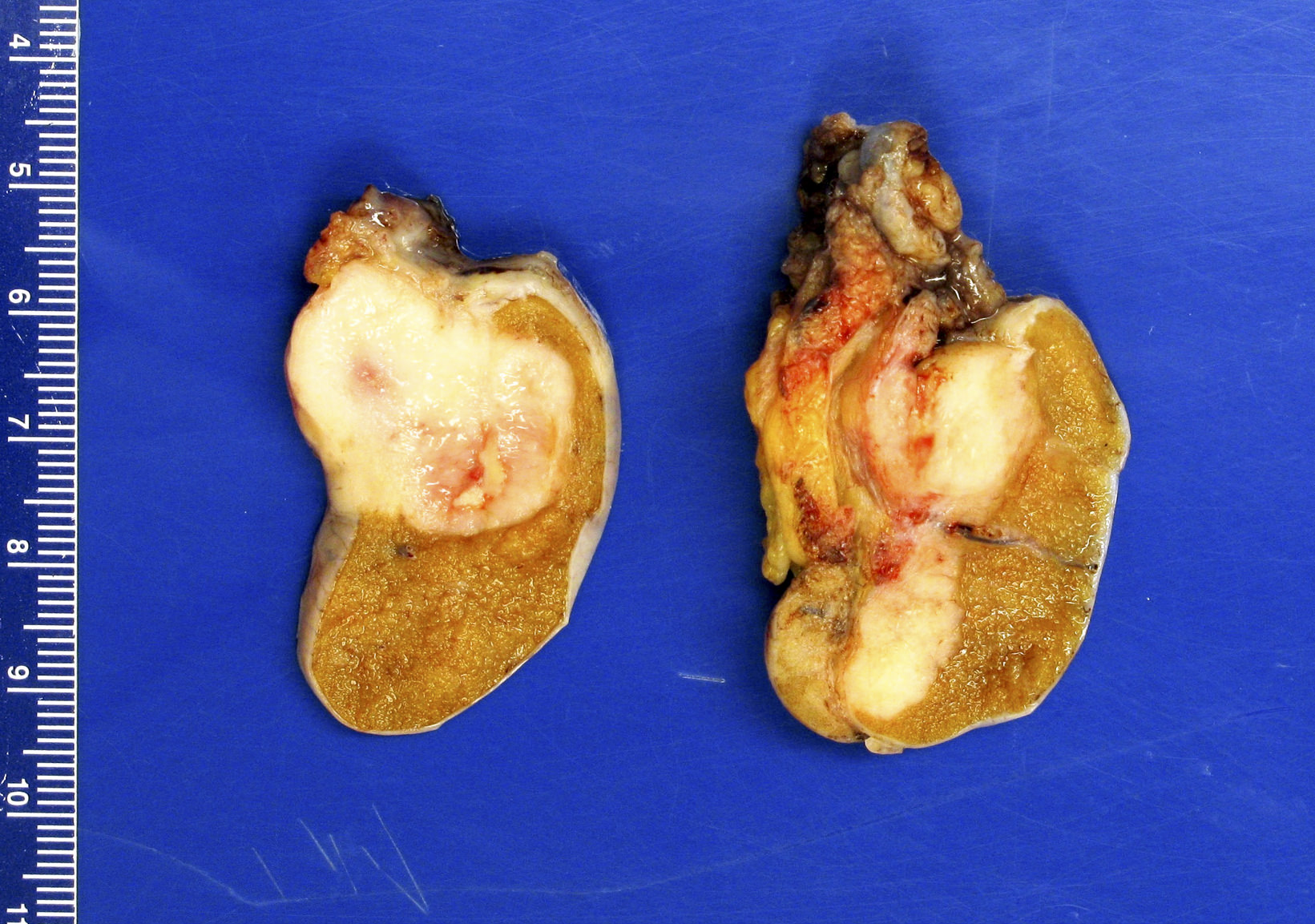
Seminoma (pT1a)
Seminoma (pT1b)

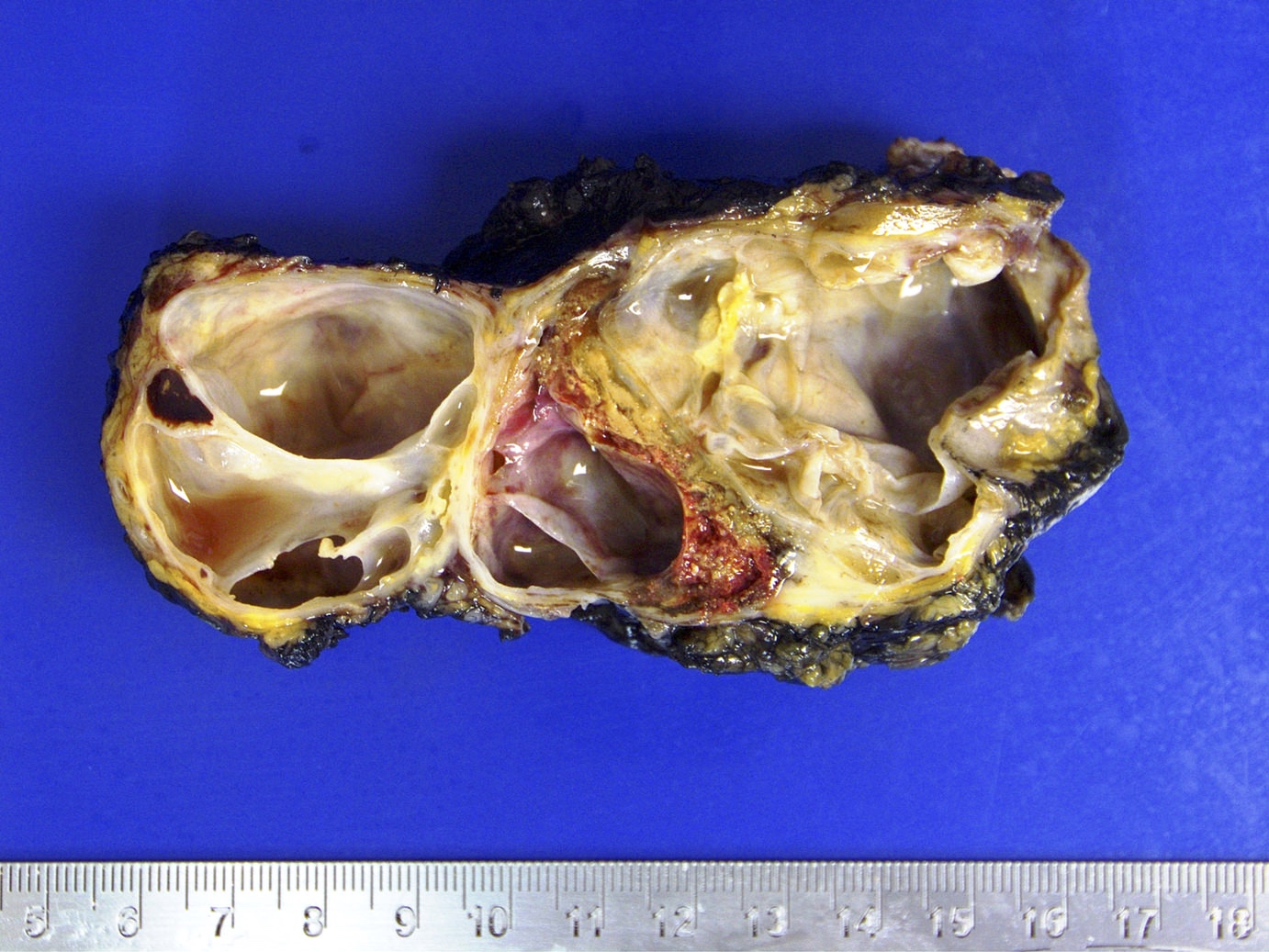
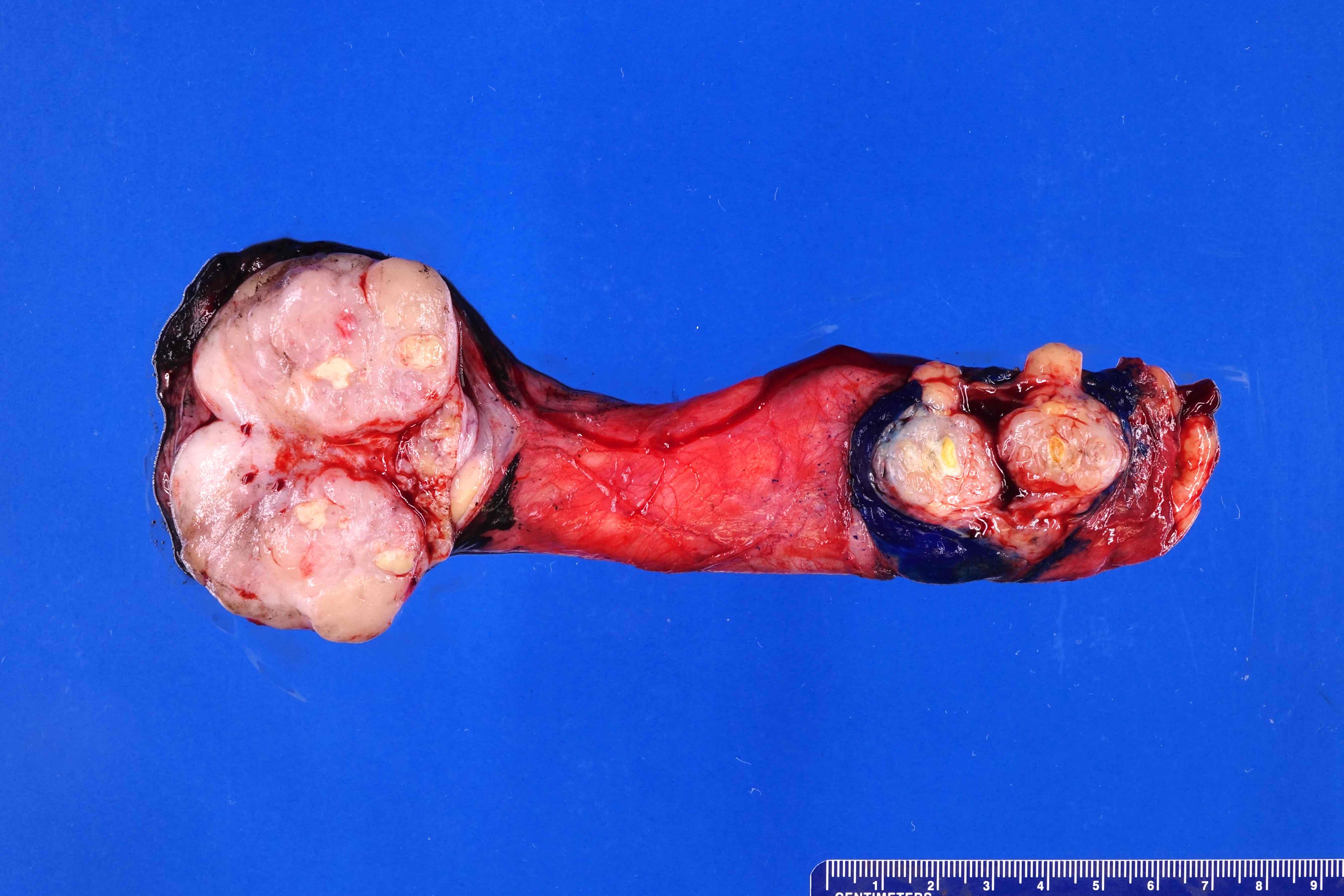
Mixed germ cell tumor (pT2)

Seminoma (pT2)

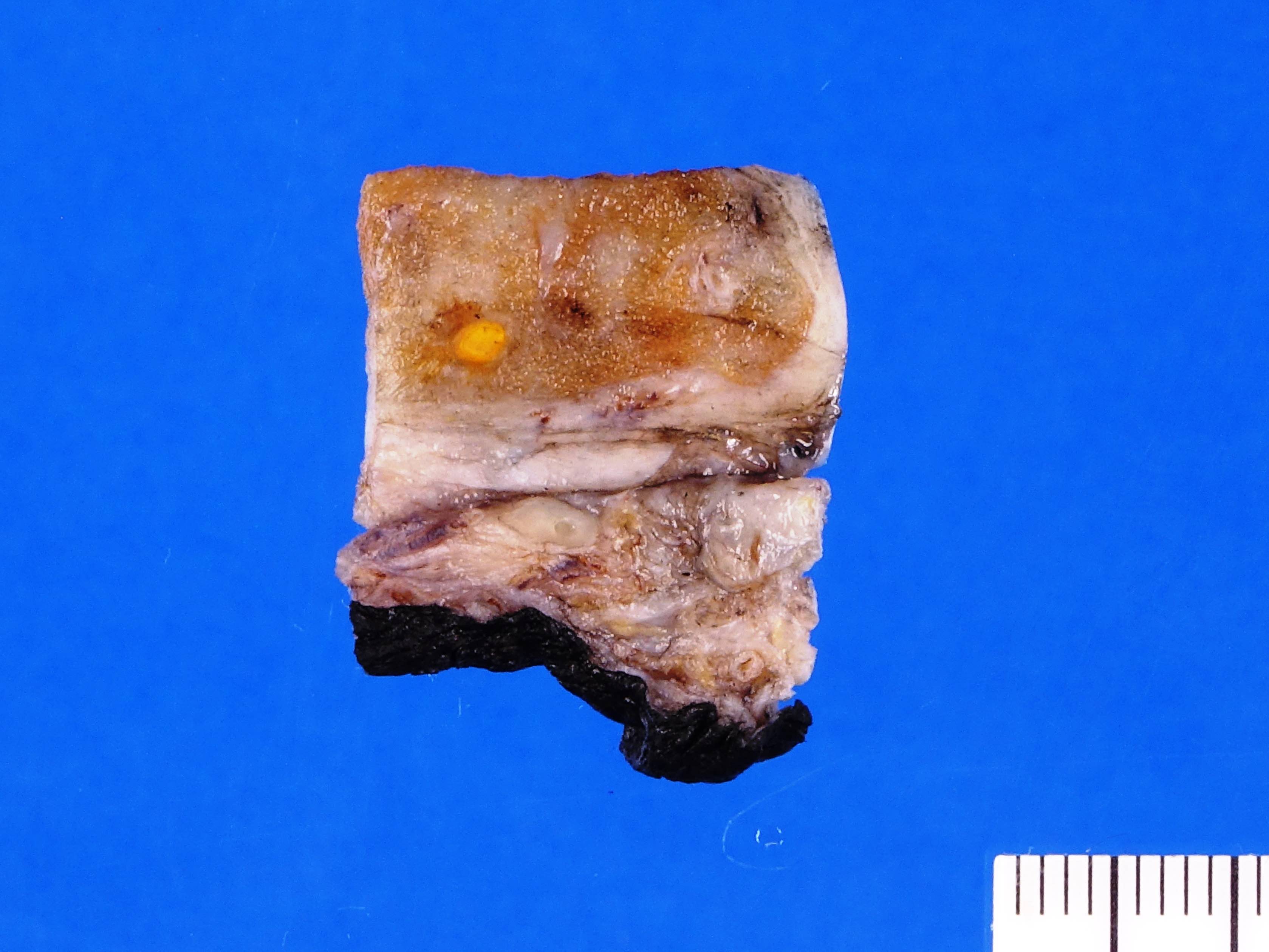
No residual node tumor (ypN0)
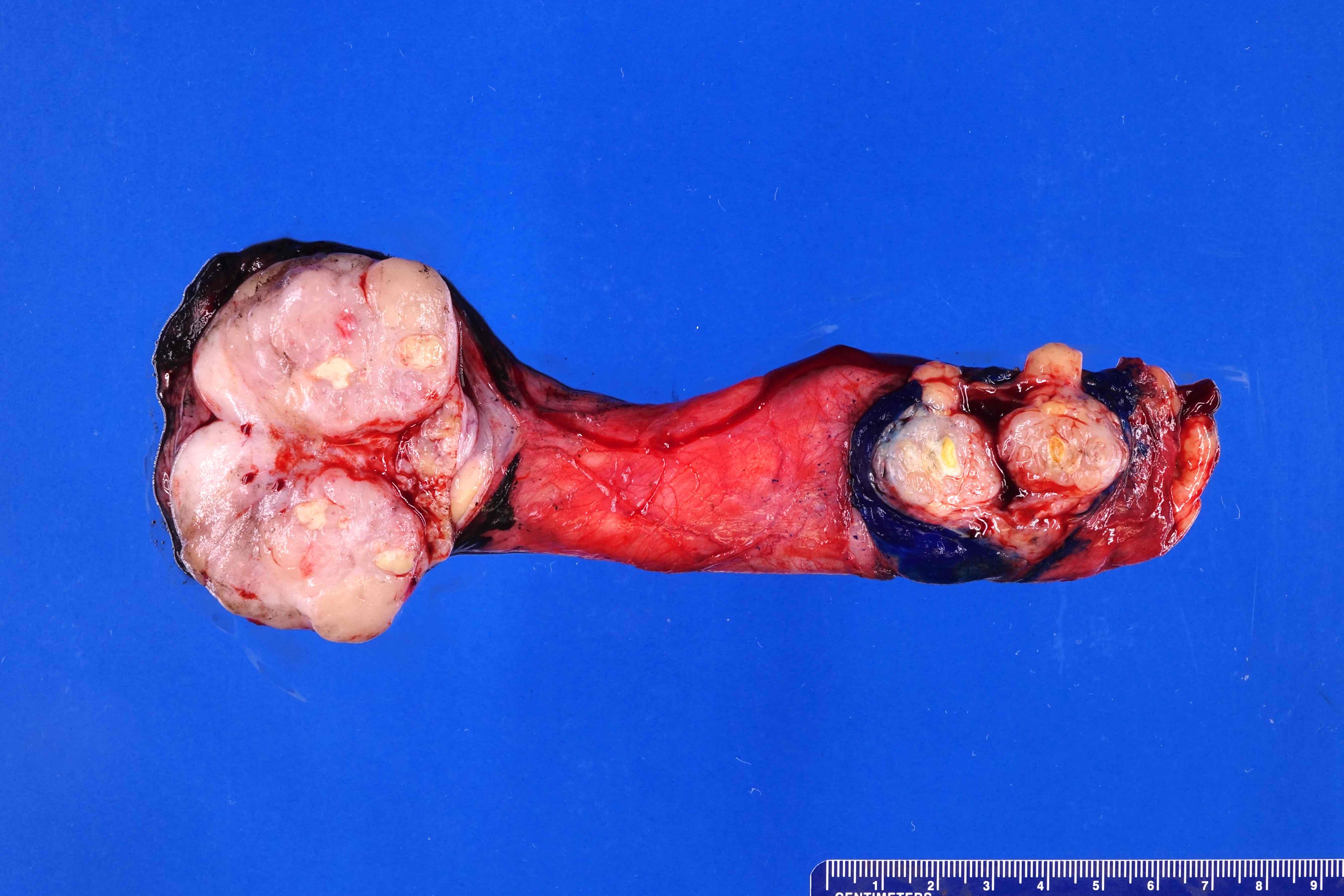
Discontinuous spermatic cord (pM1)
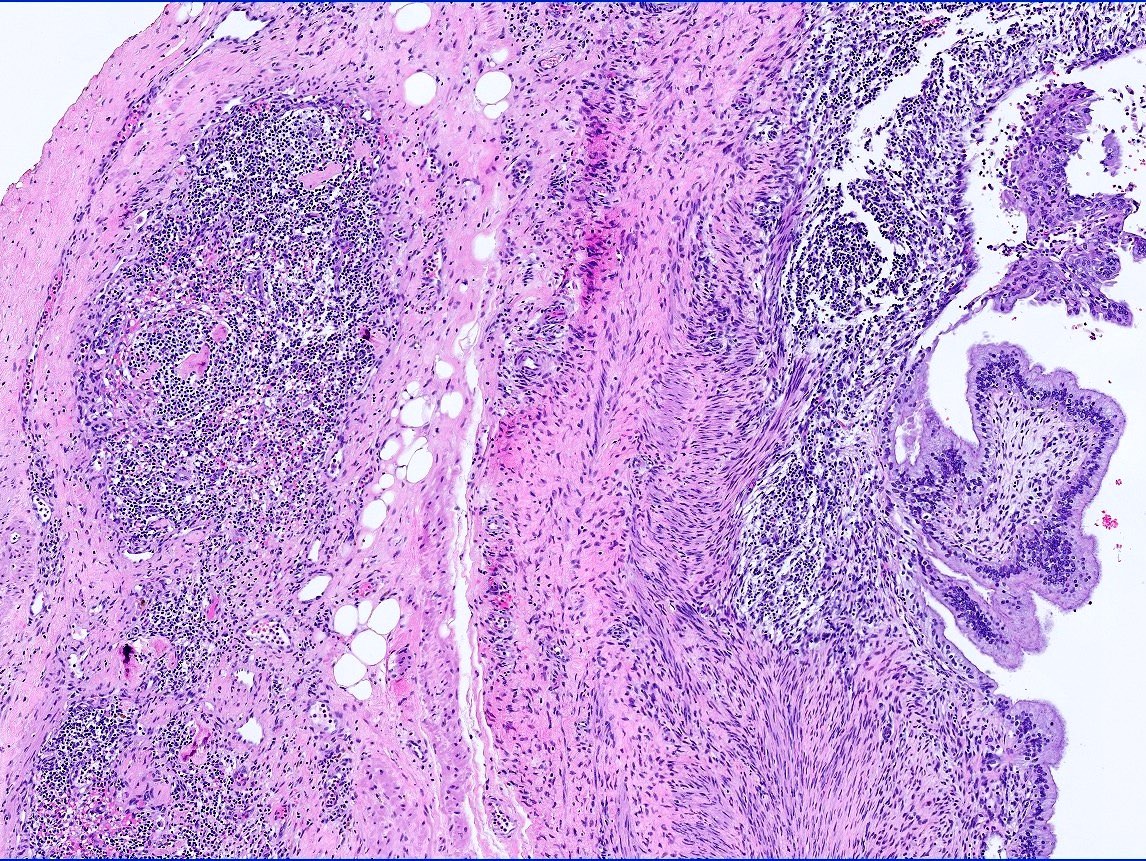
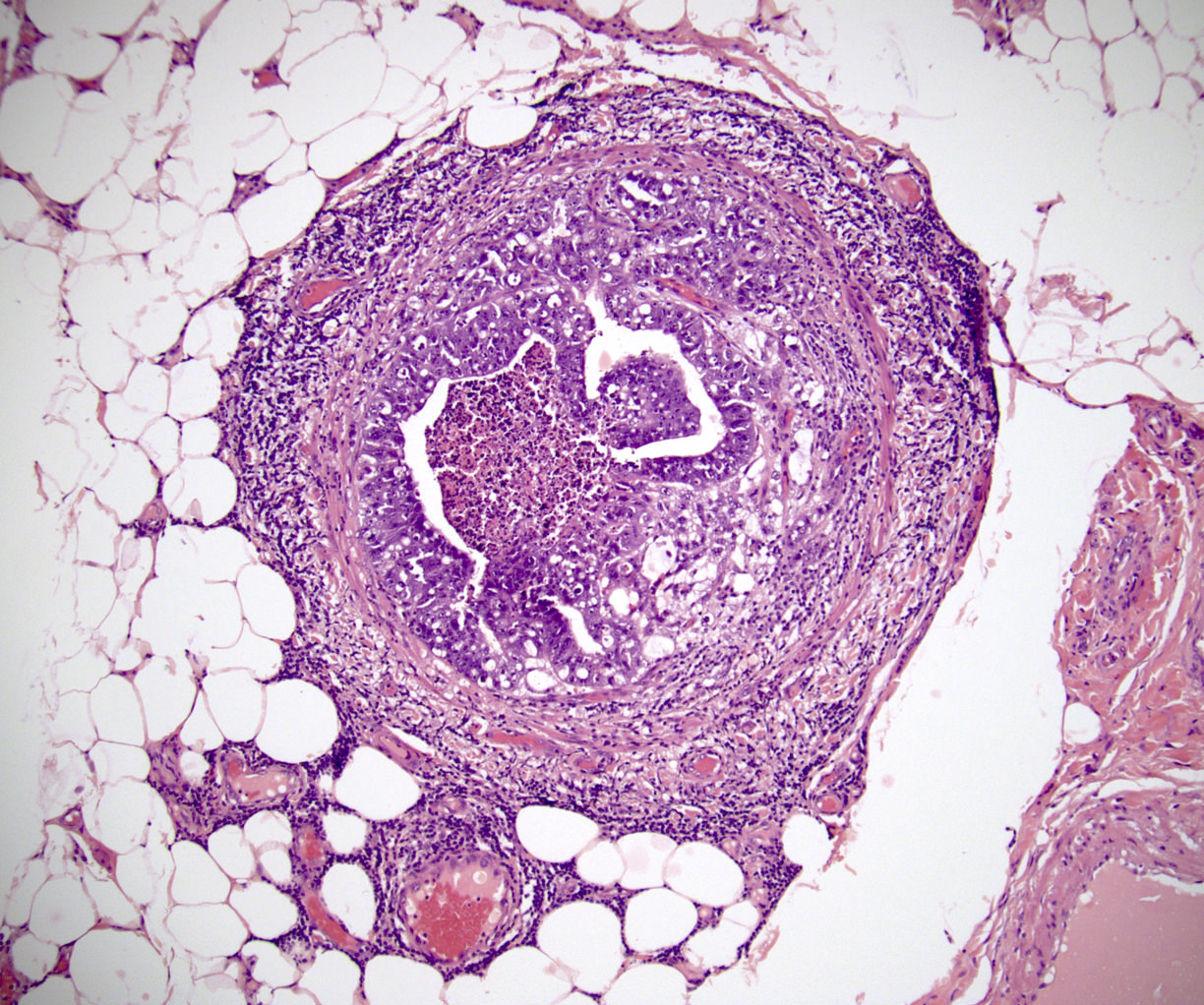
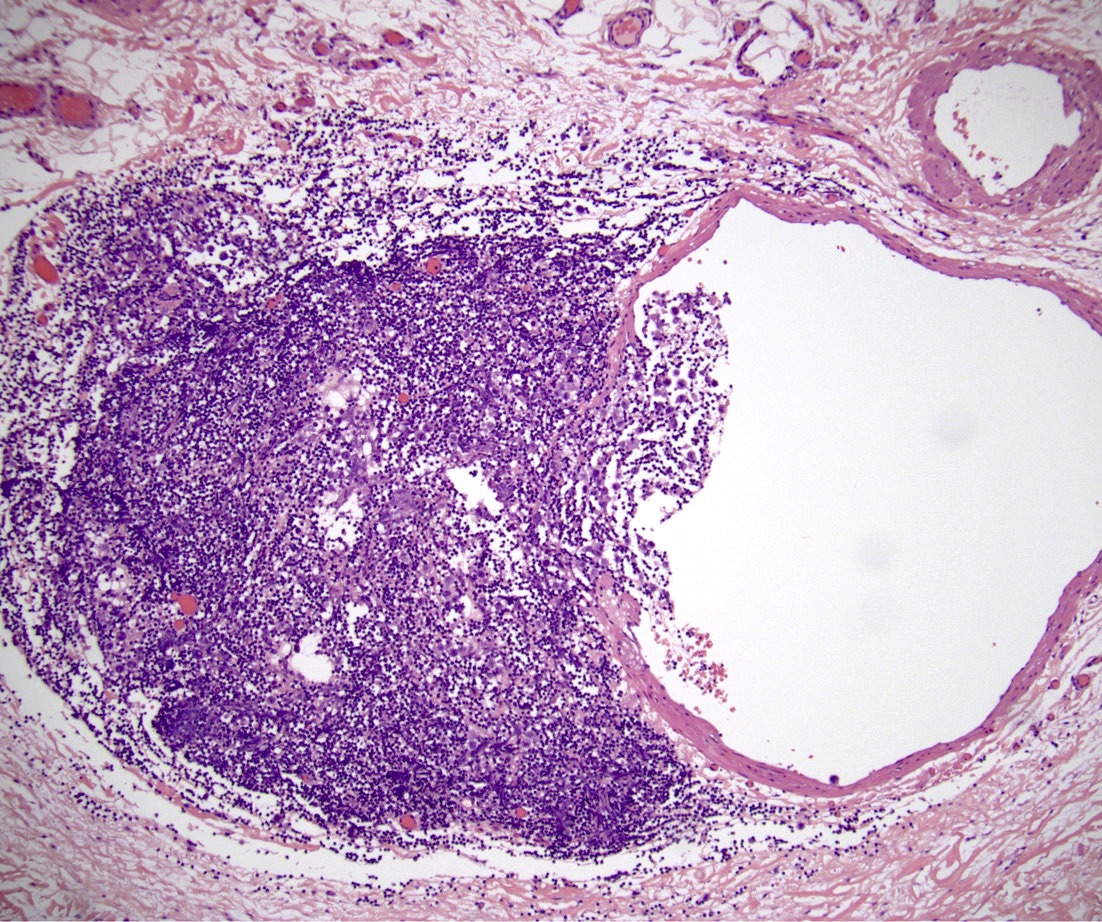
Microscopic (histologic) images
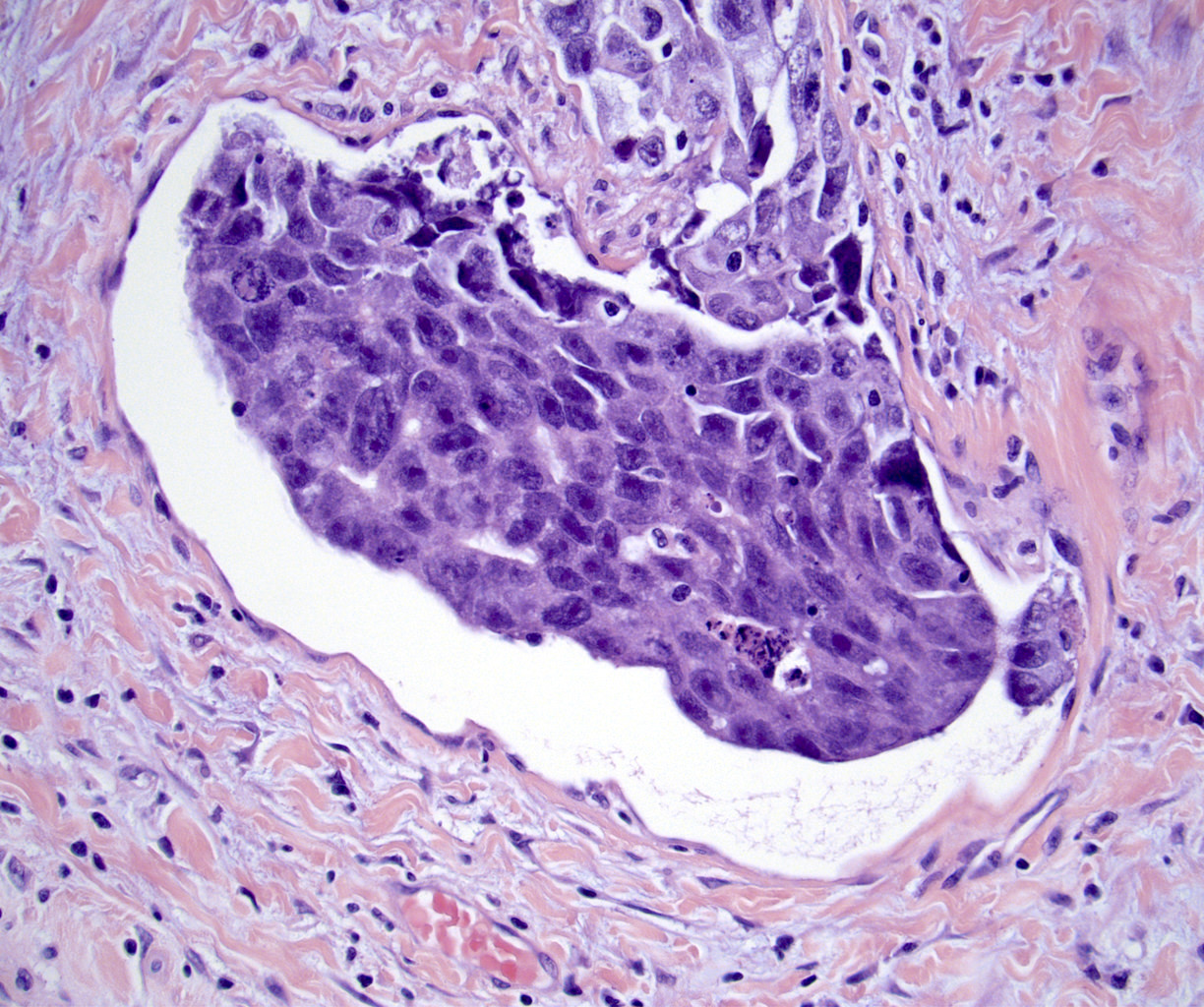
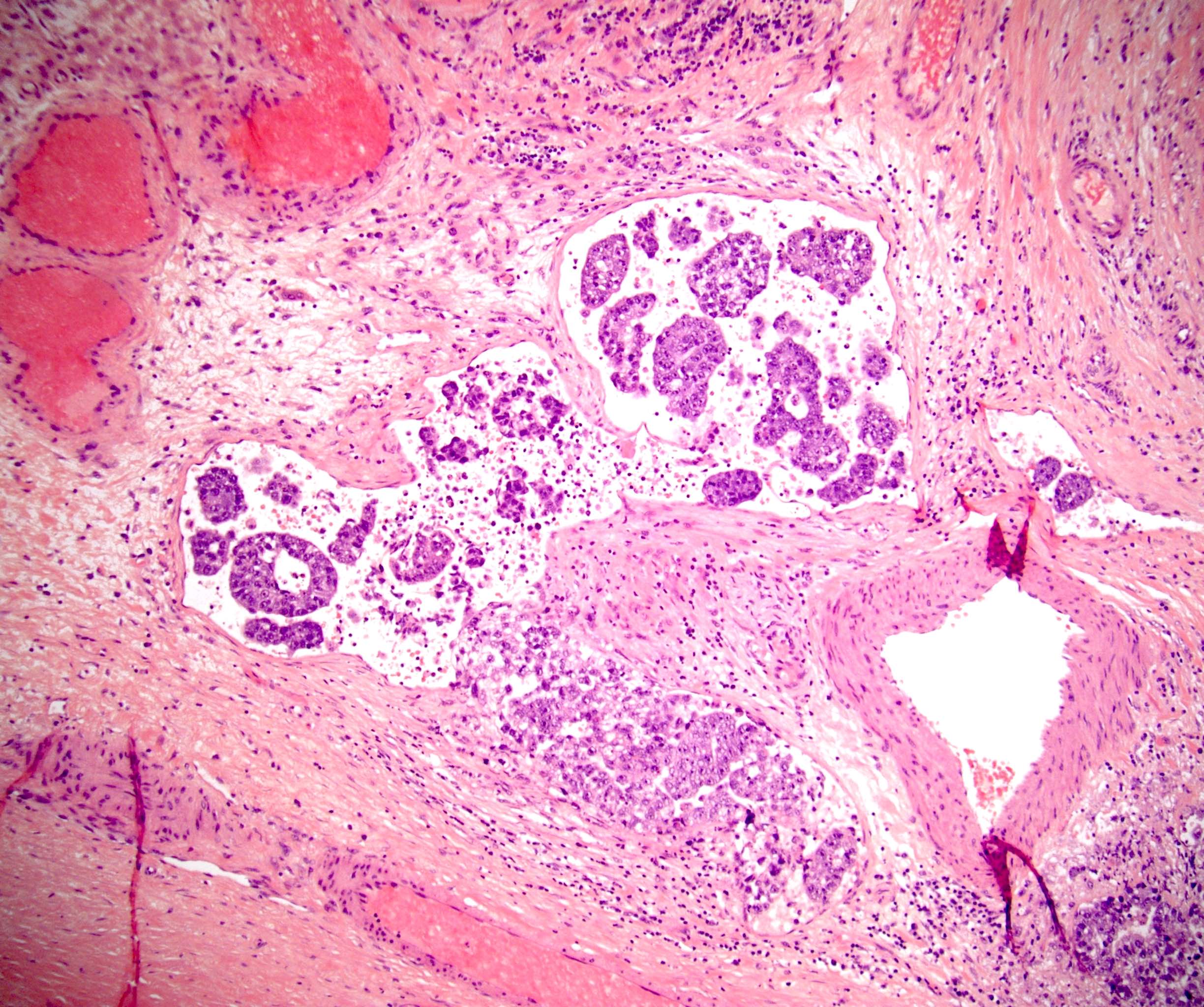
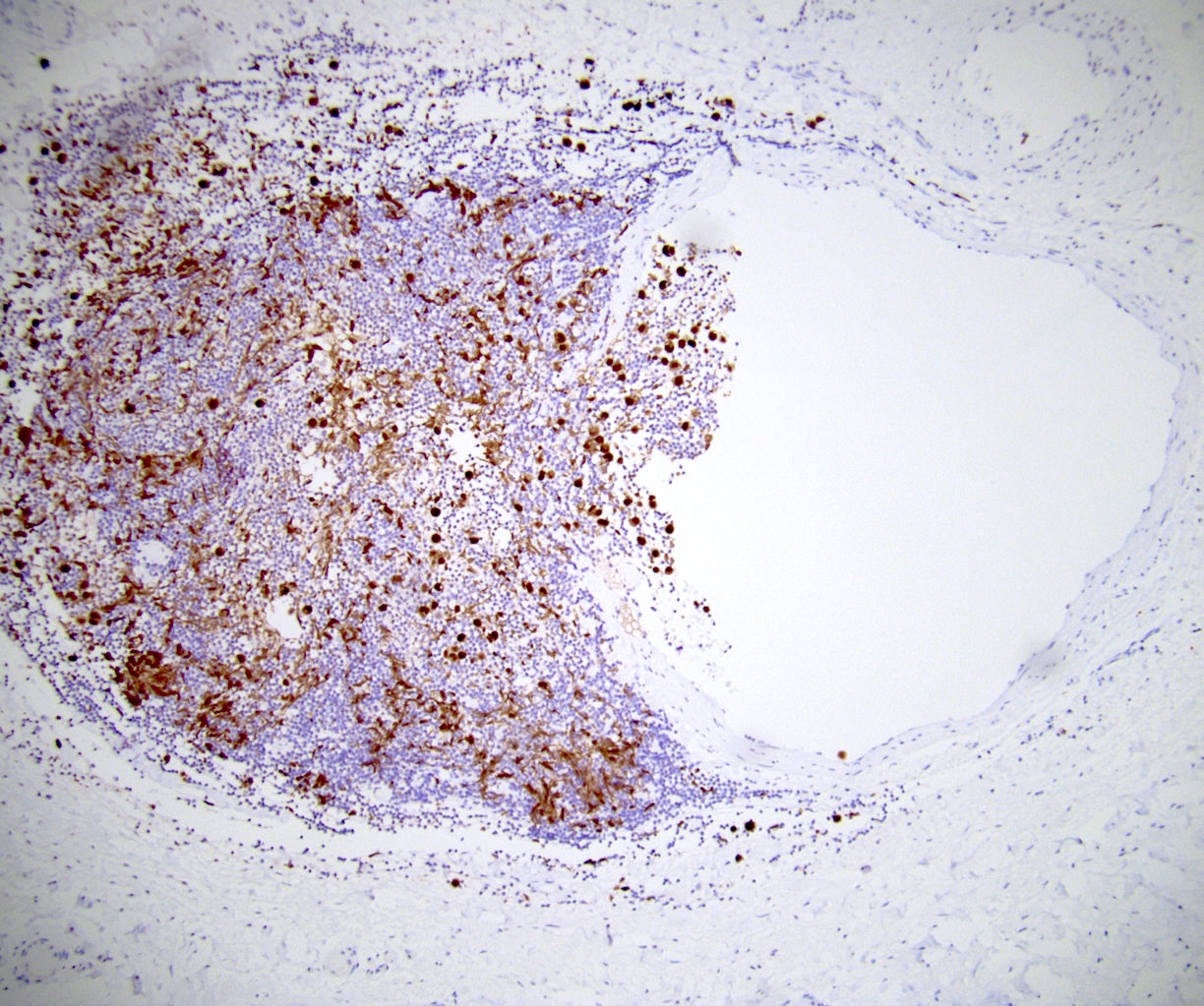
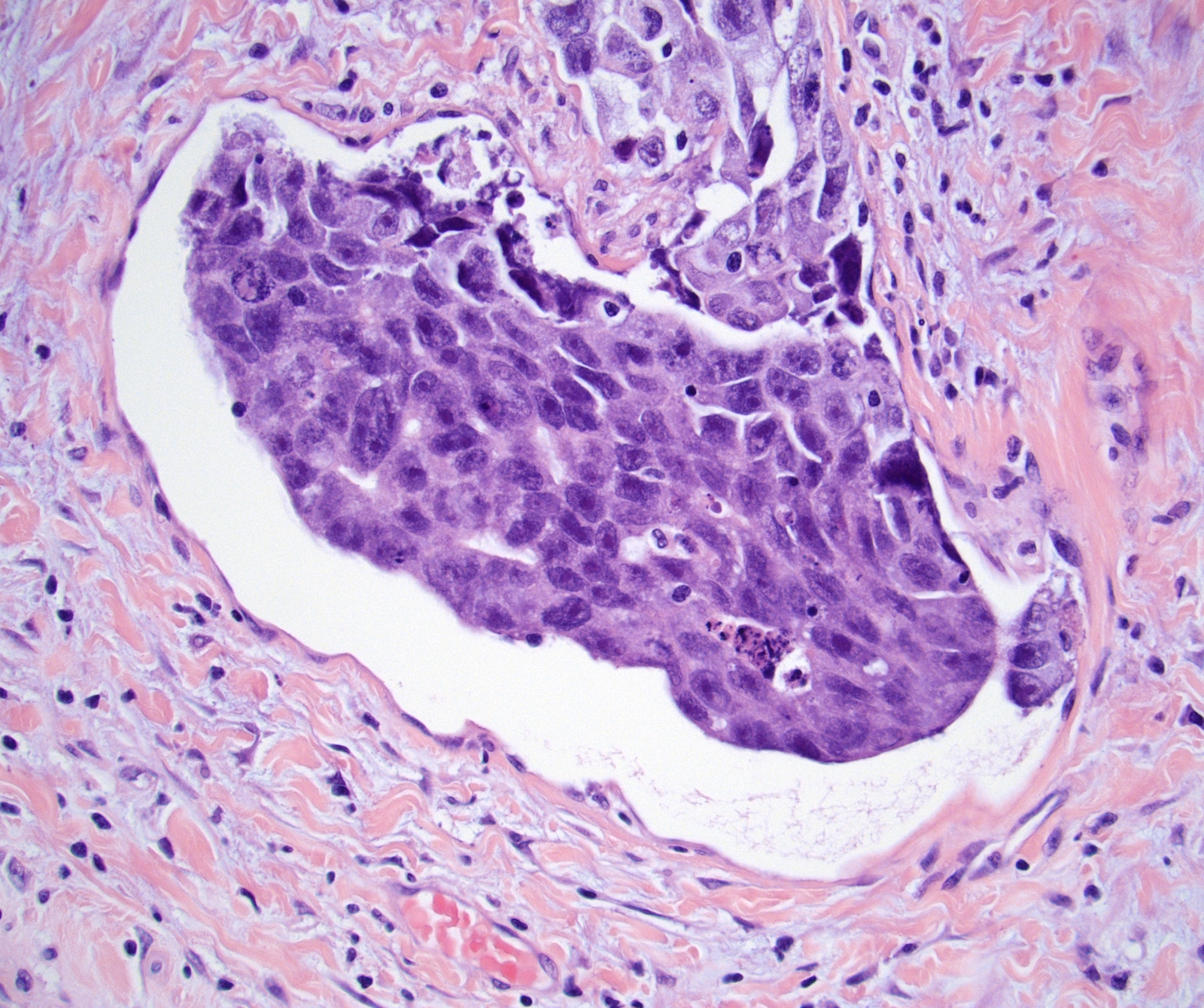
Board review style question #1
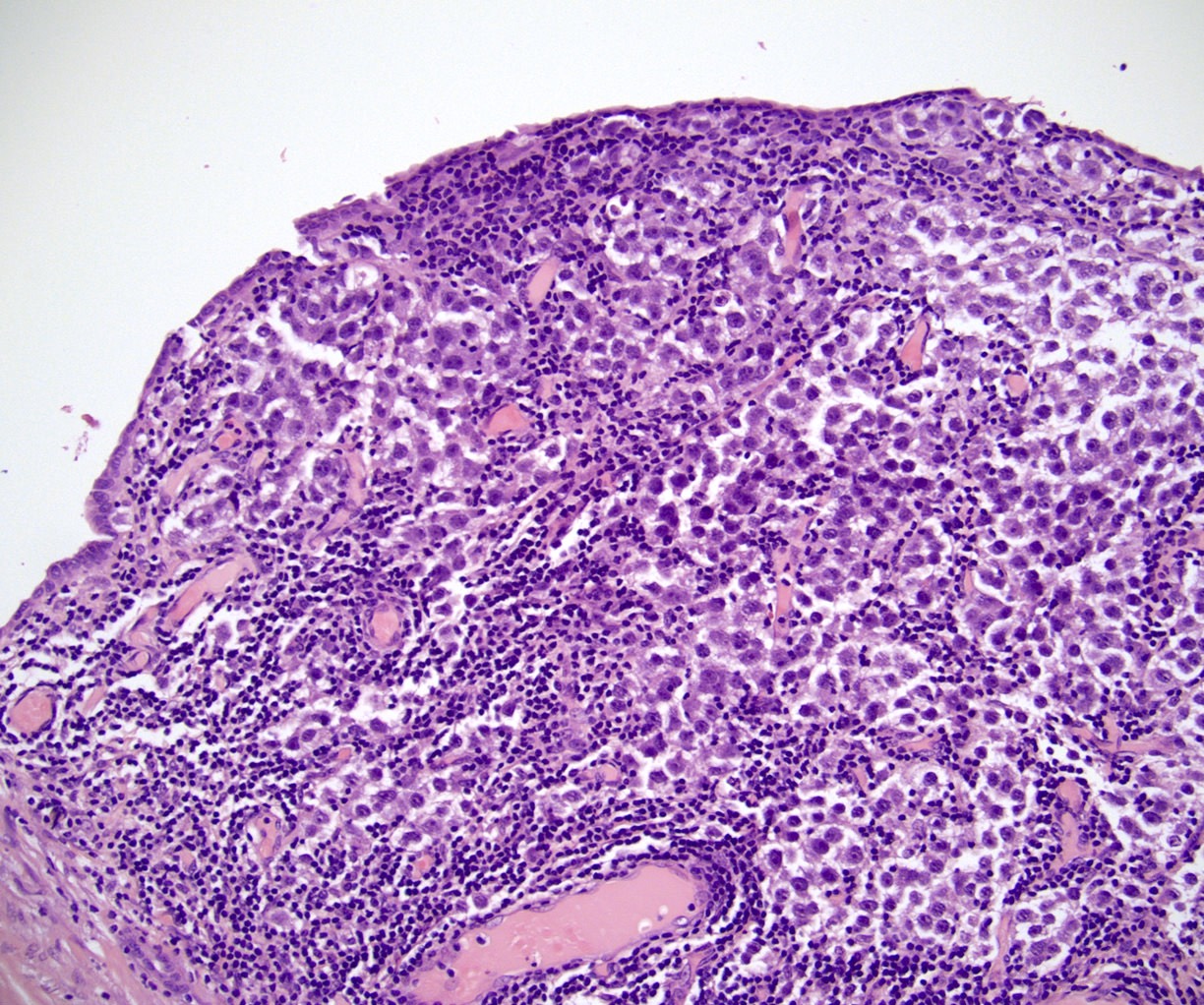
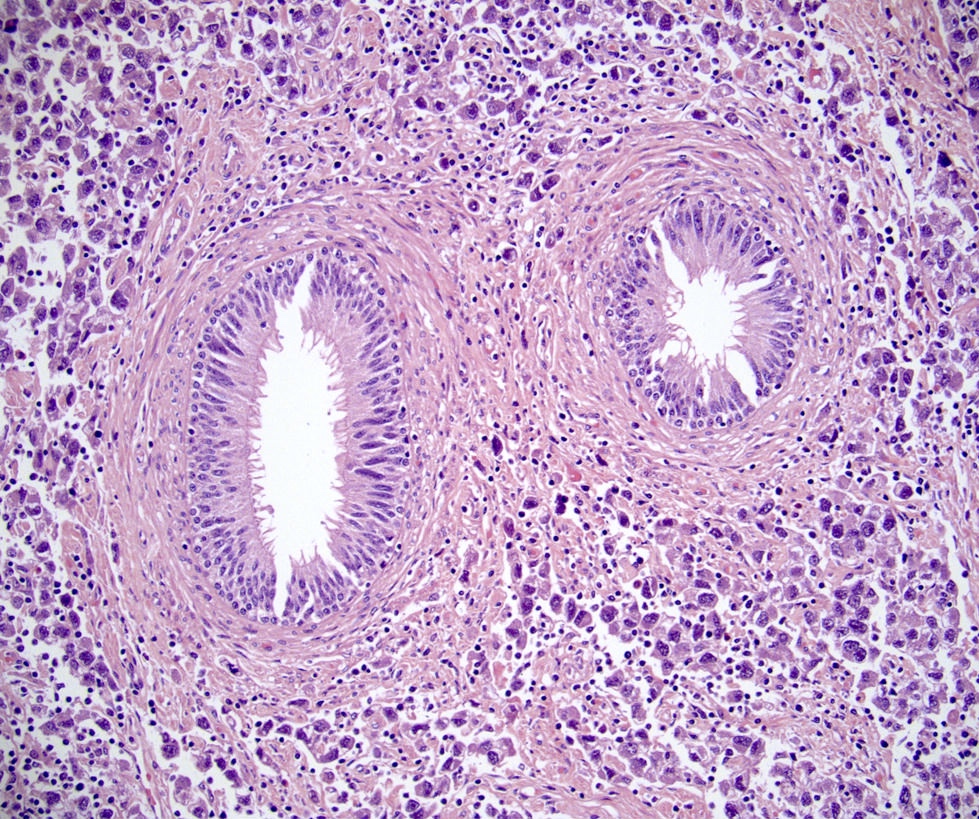
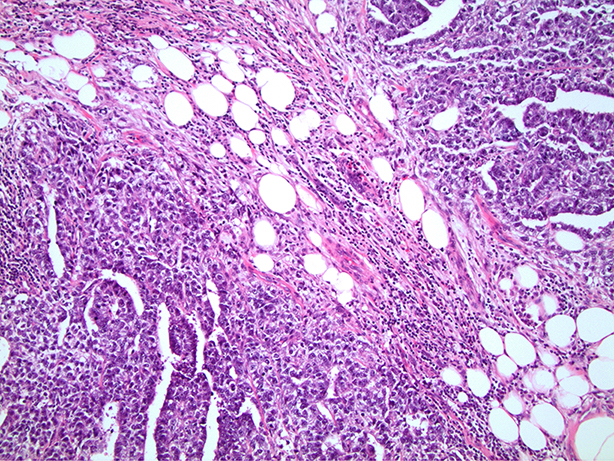
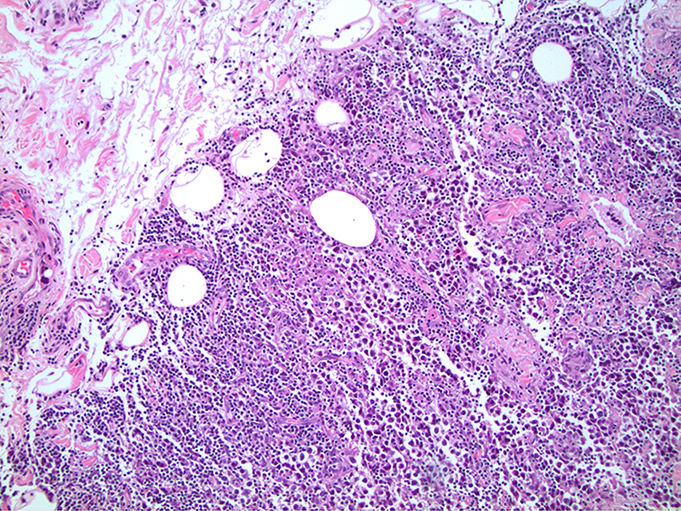
In a postpubertal testicular germ cell tumor, lymphovascular (shown above), hilar fat, epididymal and tunica vaginalis invasion are all a part of which pT category?
- pT1
- pT1a
- pT1b
- pT2
- pT3
Board review style answer #1
D. pT2. Lymphovascular, hilar fat, epididymal and tunica vaginalis invasion are all a part of the pT2 category for testicular germ cell tumors. Lymphovascular invasion by embryonal carcinoma is shown in the image.
Comment Here Reference:
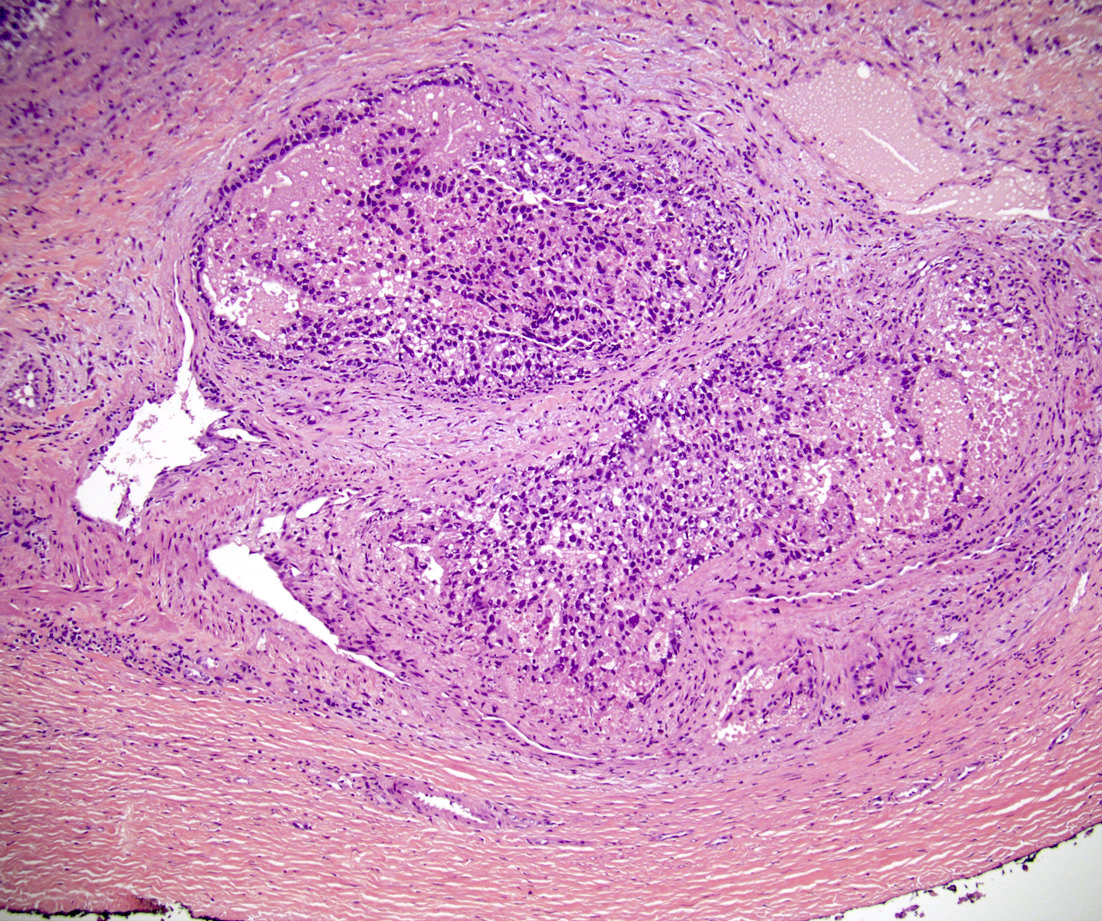
Testis & epididymis - Staging Board review style question #2
The postpubertal teratoma shown in the gross photo is 1.7 cm and is confined to the testis and did not have lymphovascular invasion. Which is the correct pT category?
- pT1
- pT1a
- pT1b
- pT2
- pT3
Board review style answer #2
A. pT1. Postpubertal germ cell tumors that are confined to the testicular parenchyma and lack lymphovascular invasion are pT1, pT1a or pT1b. Pure seminoma is stratified as pT1a and pT1b based on a 3 cm threshold. Nonpure seminomas are not stratified and therefore this tumor is pT1.
Comment Here Reference:
Testis & epididymis - Staging
Back to top