Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Agarwal S. Anaplastic thyroid carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidundiff.html. Accessed September 29th, 2025.
Definition / general
- The most aggressive follicular cell derived thyroid malignancy composed of undifferentiated cells
- Total or near total loss of follicular cell differentiation
- Concomitant with previous history of differentiated thyroid carcinoma
- Clinically, a rapidly enlarging neck mass with survival < 6 months in most cases
Essential features
- Composed of undifferentiated, pleomorphic, mitotically active tumor cells, that may show focal follicular cell differentiation morphologically or immunohistochemically
- Develops from progression of differentiated thyroid carcinoma (DTC) or de novo
- Rapidly growing, widely invasive thyroid mass needing multimodal treatment, still with near 100% disease specific mortality
Terminology
- Synonym: undifferentiated thyroid carcinoma (Endocr Relat Cancer 2022;30:e220293)
ICD coding
Epidemiology
- Rare, 1 - 2% of all thyroid malignancies
- Incidence: 0.9 - 1.2 cases per 1,000,000 population (Am J Transl Res 2019;11:5888, World J Otorhinolaryngol Head Neck Surg 2018;5:34)
- Age: > 50 years in most; median: 68 years (Thyroid 2020;30:1505)
- F:M = 1 - 2:1
Sites
- Either lobe or isthmus of thyroid gland
- Anaplastic transformation can be seen in local and distant metastases of DTC
Pathophysiology
- May arise de novo or from dedifferentiation from DTC, such as papillary thyroid carcinoma, follicular thyroid carcinoma, oncocytic carcinoma of the thyroid
- Accumulation of genetic events, commonly TP53 and TERT promoter
Etiology
- 2 pathways: develops from pre-existing DTC or de novo (Endocr Pathol 2022;33:27)
- Radiation exposure and iodine deficiency in 10% of cases
Diagrams / tables
Clinical features
- Rapidly enlarging, fixed neck mass (Endocrinol Metab Clin North Am 2019;48:269)
- Compression symptoms (e.g., pain, dysphonia, dysphagia, dyspnea, cough)
- Symptoms related to distant metastases, in ~60% of cases (Thyroid 2020;30:1505)
- Prior history of surgery for DTC or concurrent DTC in > 50% of cases (Thyroid 2020;30:1505)
Diagnosis
- Anaplastic thyroid carcinoma (ATC) is a clinicopathological diagnosis to be corroborated with radiology; confirmation on histopathology or cytopathology supplemented by immunohistochemistry or molecular analysis is essential
- Diagnostic workup (Thyroid 2021;31:337)
- Fine needle aspiration cytology (FNAC)
- Can be supplemented by immunohistochemistry and BRAF evaluation
- Core biopsy, if FNAC does not have adequate cellularity for diagnosis or for ancillary testing
- Ultrasonography of neck for evaluation of the thyroid mass and assessment of cervical node involvement
- Staging of disease using 18F FDG PET / CT (whole body); if unavailable, computed tomography (CT) / magnetic resonance imaging (MRI) of neck, chest, abdomen and pelvis
- MRI or CT brain with contrast for brain metastases
- Fine needle aspiration cytology (FNAC)
Laboratory
- Blood tests and biochemistry: complete blood count with differential, blood chemistry, thyroid function tests, Tg and Tb antibody (Thyroid 2021;31:337)
- Part of clinical workup but changes are not specific to ATC
- Optional, liquid biopsy to assess mutational profile or monitor treatment response
Radiology description
- Sonography
- Large, hypoechoic, solid, irregular mass with heterogeneous echogenicity, invading surrounding neck structures (J Ultrasound Med 2016;35:1873)
- Computed tomography scan
- Large ill defined mass, heterogeneous, isodense or slightly hyperdense relative to skeletal muscle, with areas of necrosis, dense amorphous nodular calcification and infiltration of adjoining organs (AJR Am J Roentgenol 1990;154:1079, Acta Radiol 2008;49:321)
Radiology images
Prognostic factors
- Poor prognosis, mortality > 90%
- Median survival: 5 - 6 months
- 1 year survival: 10 - 20%
- 5 year survival: 5 - 10% (Clin Oncol (R Coll Radiol) 2010;22:486, J Natl Compr Canc Netw 2015;13:1140)
- Only marginal improvement with multimodal therapy
- Poor prognostic indicators (Thyroid 2020;30:1505, Thyroid 2021;31:337, Endocr Pathol 2022;33:27)
- Older patient age (> 60 - 65 years)
- Acute symptoms
- Leukocytosis
- Absence of DTC
- Presence of nodal or distant metastasis
- Larger tumor size (> 5 - 7 cm)
- Tumor with gross extrathyroidal extension
- TERT promoter mutations
- Concomitant BRAF / RAS and TERT promoter mutations
- EIF1AX mutation, chromosome 13q loss and 20q gains (Endocr Pathol 2016;27:205)
- Better clinical outcome (Thyroid 2021;31:337, Head Neck 2016;38:E2083, Thyroid 2020;30:1505, Thyroid 2016;26:404)
- Younger age
- Lower comorbidity score (Charlson / Deyo comorbidity score of 0)
- Absent nodal disease and metastasis
- Smaller tumor size
- Minor ATC component: defined arbitrarily as < 10% ATC component along with DTC
- Encapsulation
- Absent extrathyroidal extension
- ATC with excellent outcome is likely to be a misdiagnosed case of PTC with unusual morphology (Endocr J 2016;63:441)
Case reports
- 44 year old woman diagnosed with ATC with rhabdoid phenotype (Diagn Cytopathol 2020;48:1125)
- 44 year old woman with Epstein-Barr virus (EBV) associated lymphoepithelioma-like thyroid carcinoma (Diagn Pathol 2018;13:39)
- 51 year old man with ATC arising from tall cell variant of papillary thyroid carcinoma (Case Rep Endocrinol 2017;2017:4581626)
- 53 year old man with ATC (J Clin Diagn Res 2017;11:ED03)
- 61 year old woman with anaplastic transformation of papillary thyroid carcinoma found at pleural metastasis (Head Neck Pathol 2017;11:162)
- 63 year old man with ATC showing chondrosarcomatous differentiation (Diagn Pathol 2020;15:89)
- 64 year old man with metastatic ATC in complete remission (Endocr Pathol 2020;31:77)
- 67 year old woman with osteoclastic variant of ATC (J Cancer Res Ther 2019;15:704)
- 72 year old man with BRAF V600E positive ATC (Diagn Cytopathol 2021;49:150)
- 75 year old man with a history of malignant melanoma develops ATC with rhabdoid features (Diagn Cytopathol 2019;47:1232)
Treatment
- Based on American Thyroid Association and National Comprehensive Cancer Network guidelines, usually multimodal therapy (Thyroid 2021;31:337, NCCN: NCCN Guidelines - Thyroid Carcinoma [Accessed 14 August 2023])
- Surgery, if resectable
- Radiotherapy with or without chemotherapy
- Targeted therapy
- Dabrafenib and trametenib, if BRAF V600E mutated
- Crizotinib, ceritinib, alectinib, in case of ALK fusions
- Pralsetinib, selpercatinib, in case of RET fusions
- Larotrectinib, entrectinib, in case of NTRK fusions
- Checkpoint inhibitor (e.g., pembrolizumab)
- High PD-L1 expression or ≥ 10 MB mutations/Mb
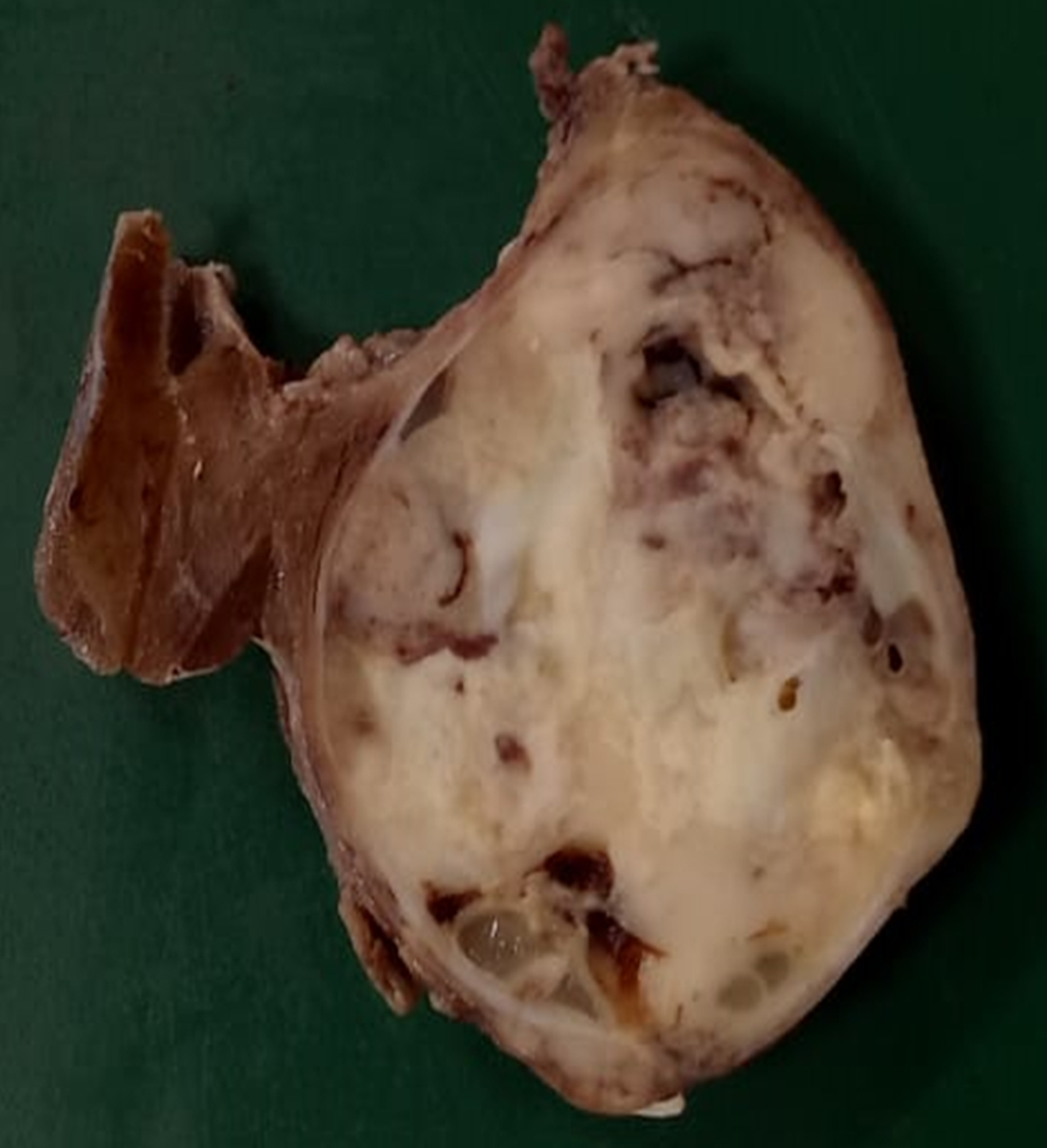
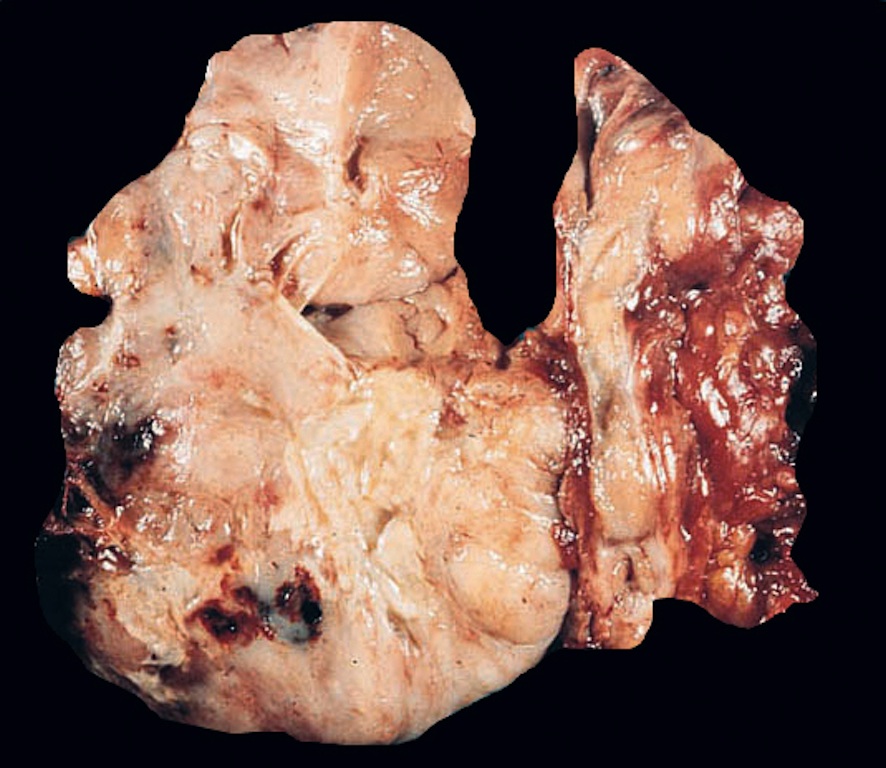
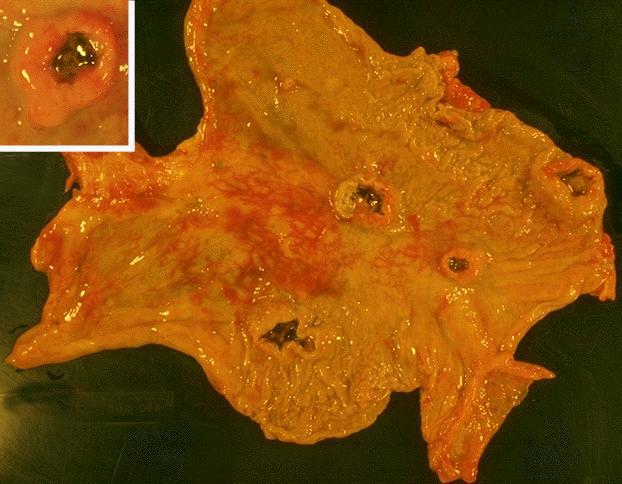
Gross description
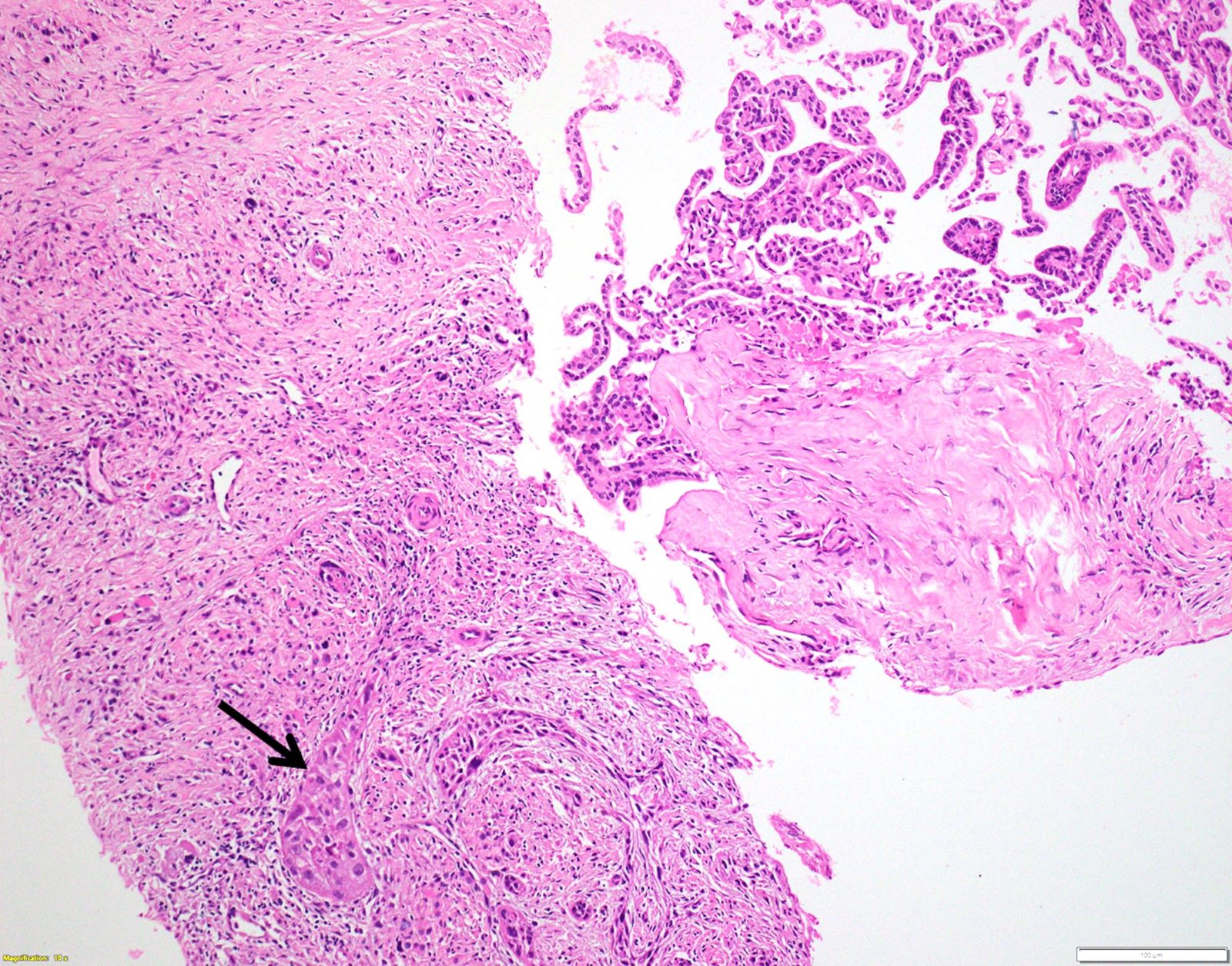
- Large mass (often > 5 cm) with ill defined margins that infiltrate adjoining skeletal muscle and trachea
- Cut surface is tan, fleshy, may be variegated; hemorrhage, necrosis (Endocr Pathol 2022;33:27)
Gross images
Frozen section description
- Rarely used
- Sometimes may be helpful to assess adequacy of diagnostic tissue, besides margins and tumor extent (Thyroid 2021;31:337)
- May not be diagnostic if only necrotic or inflammatory areas are sampled
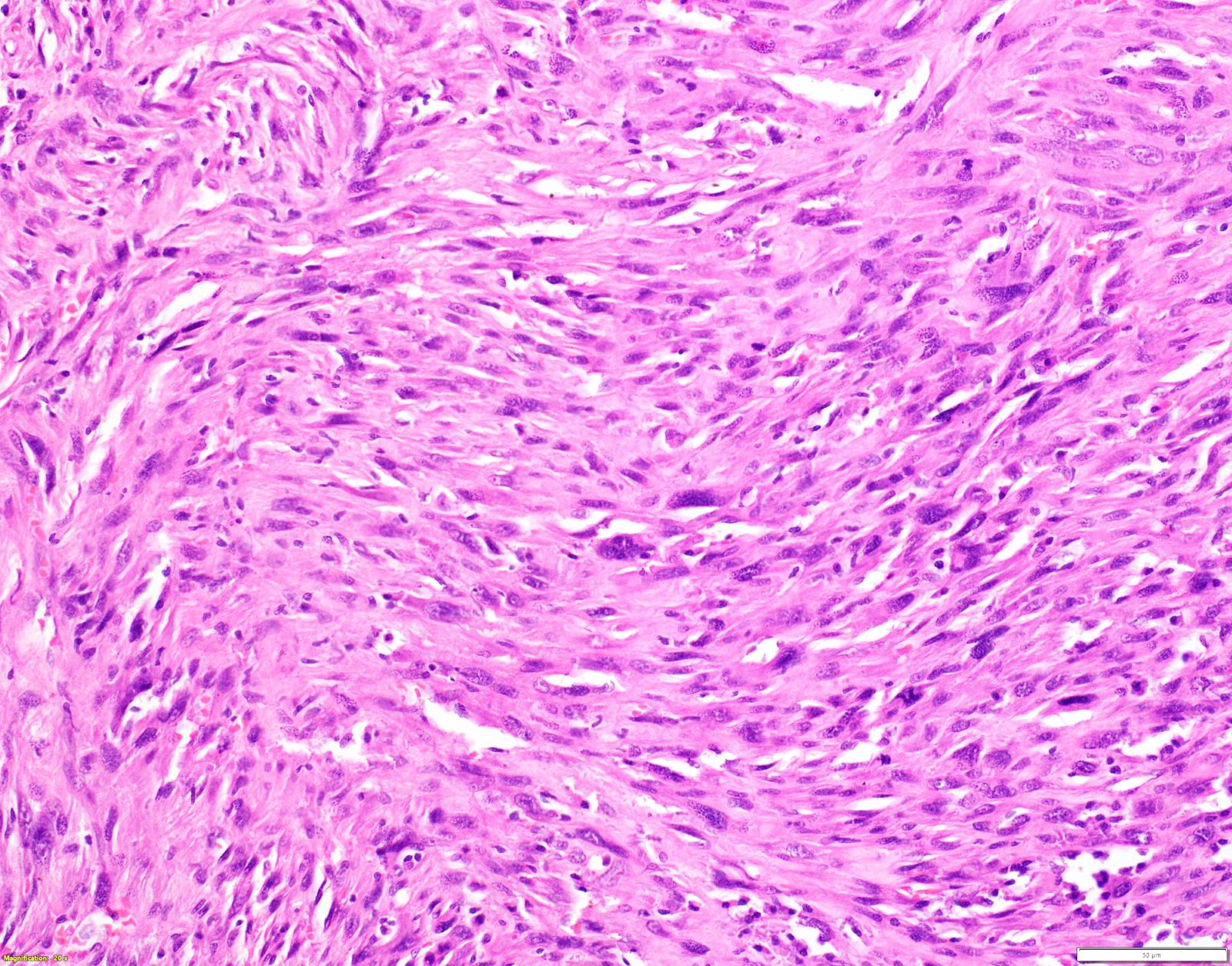
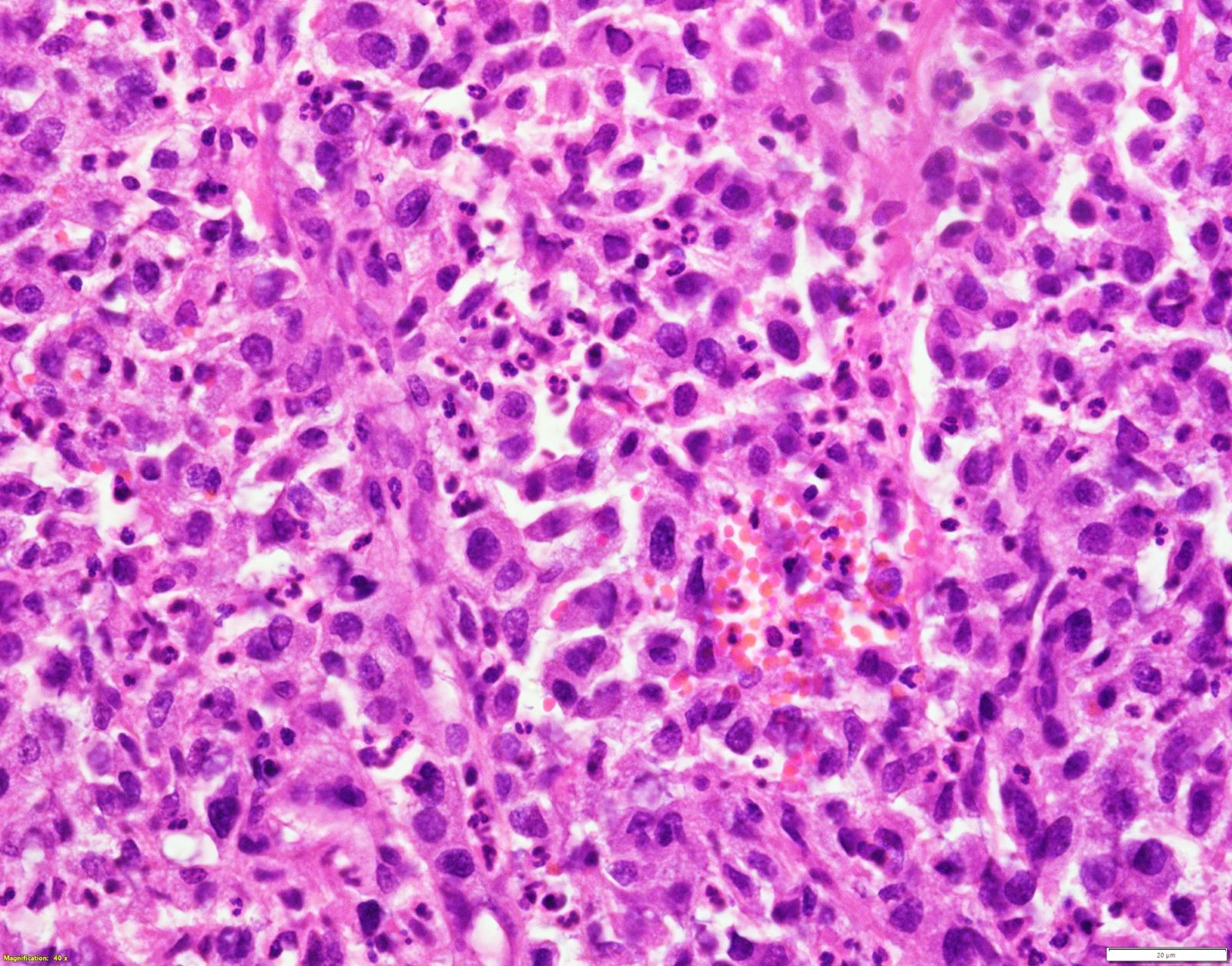
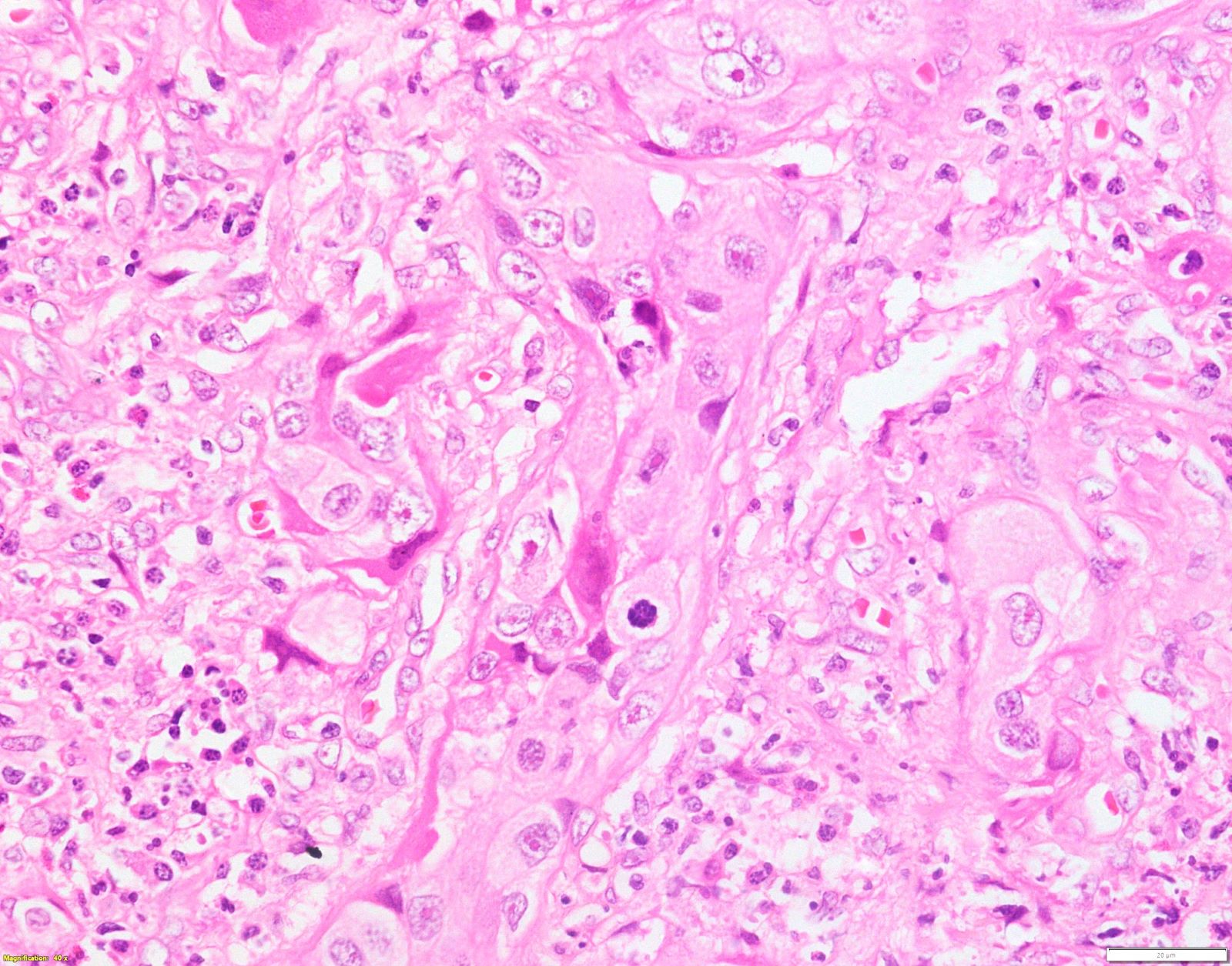
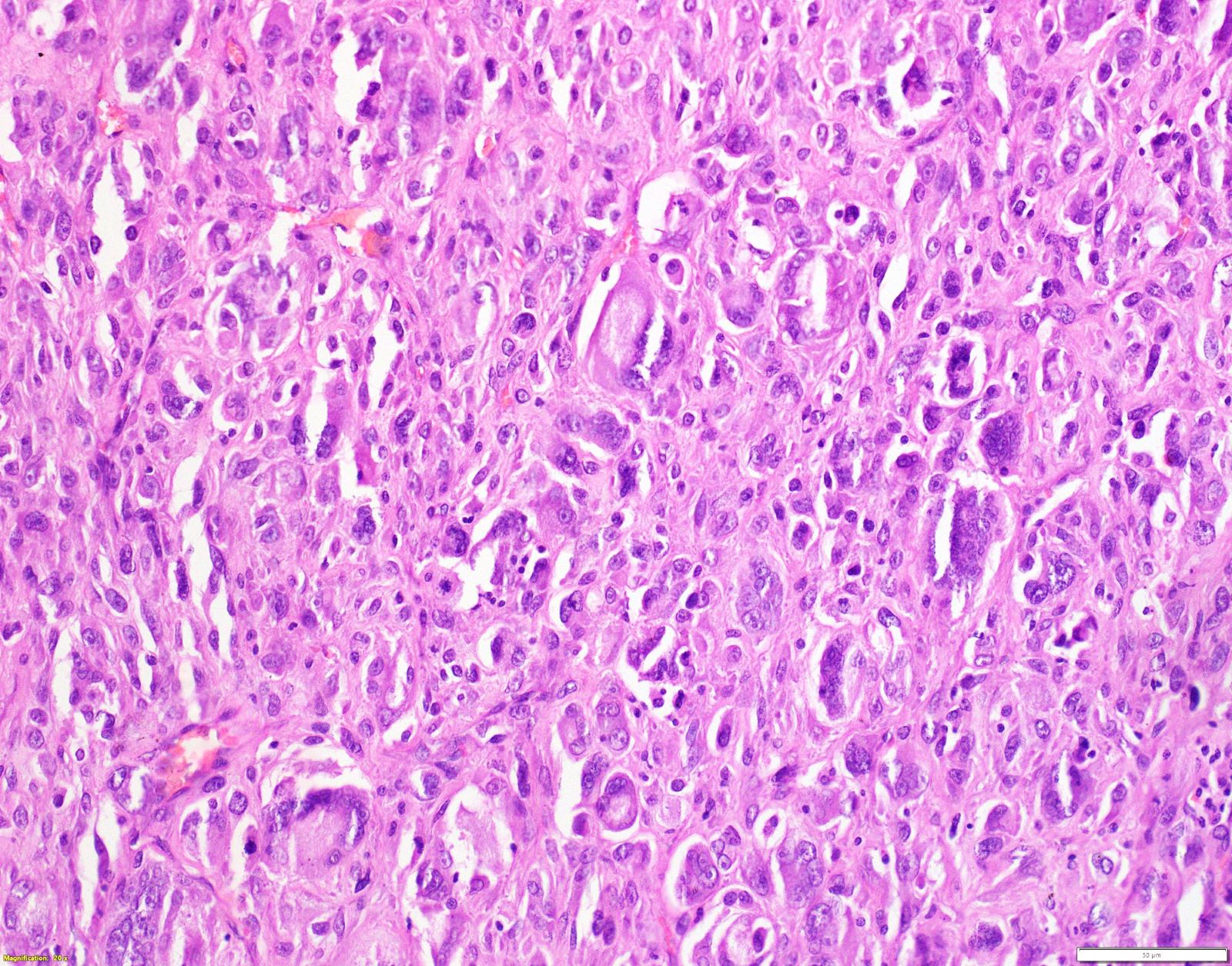
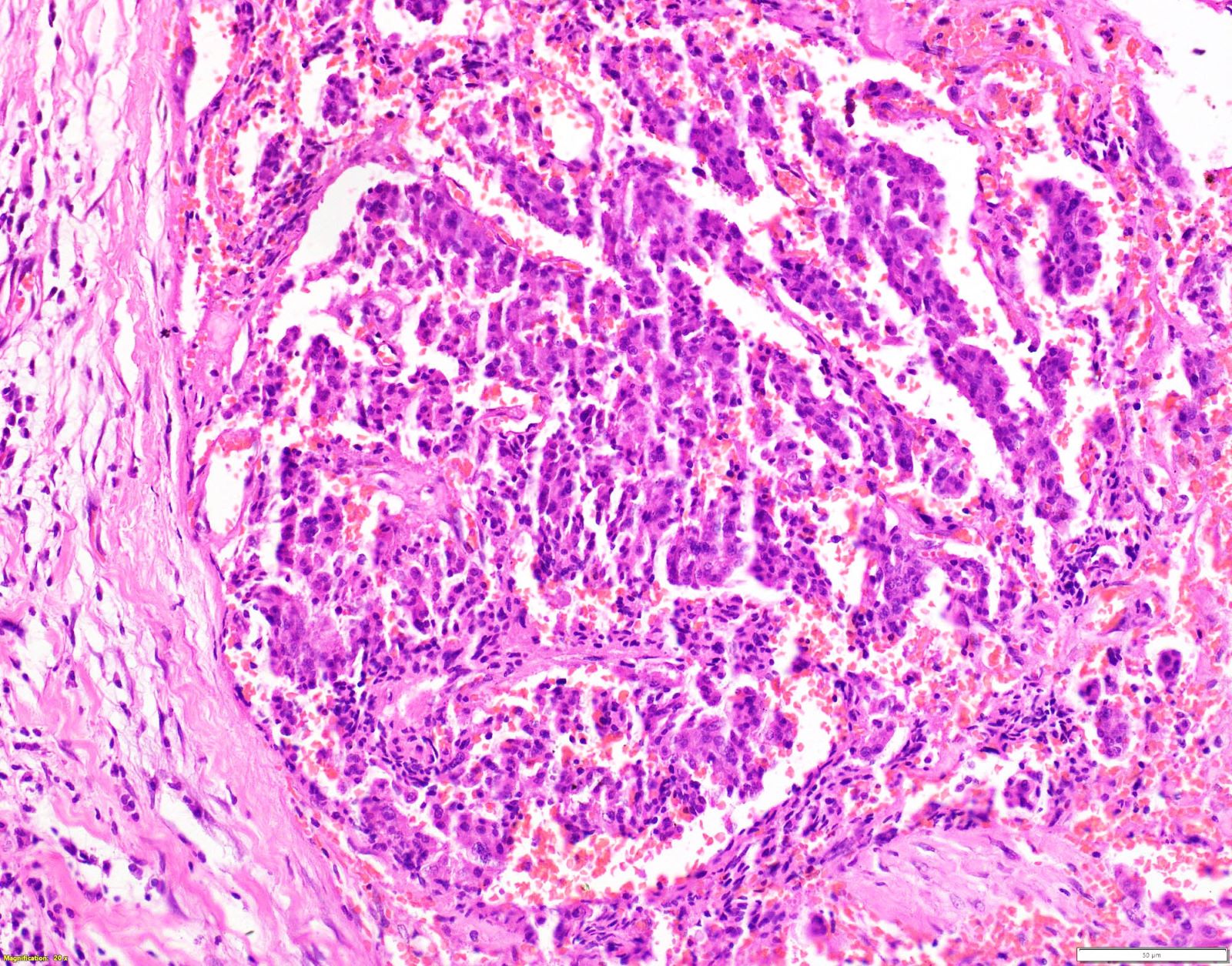
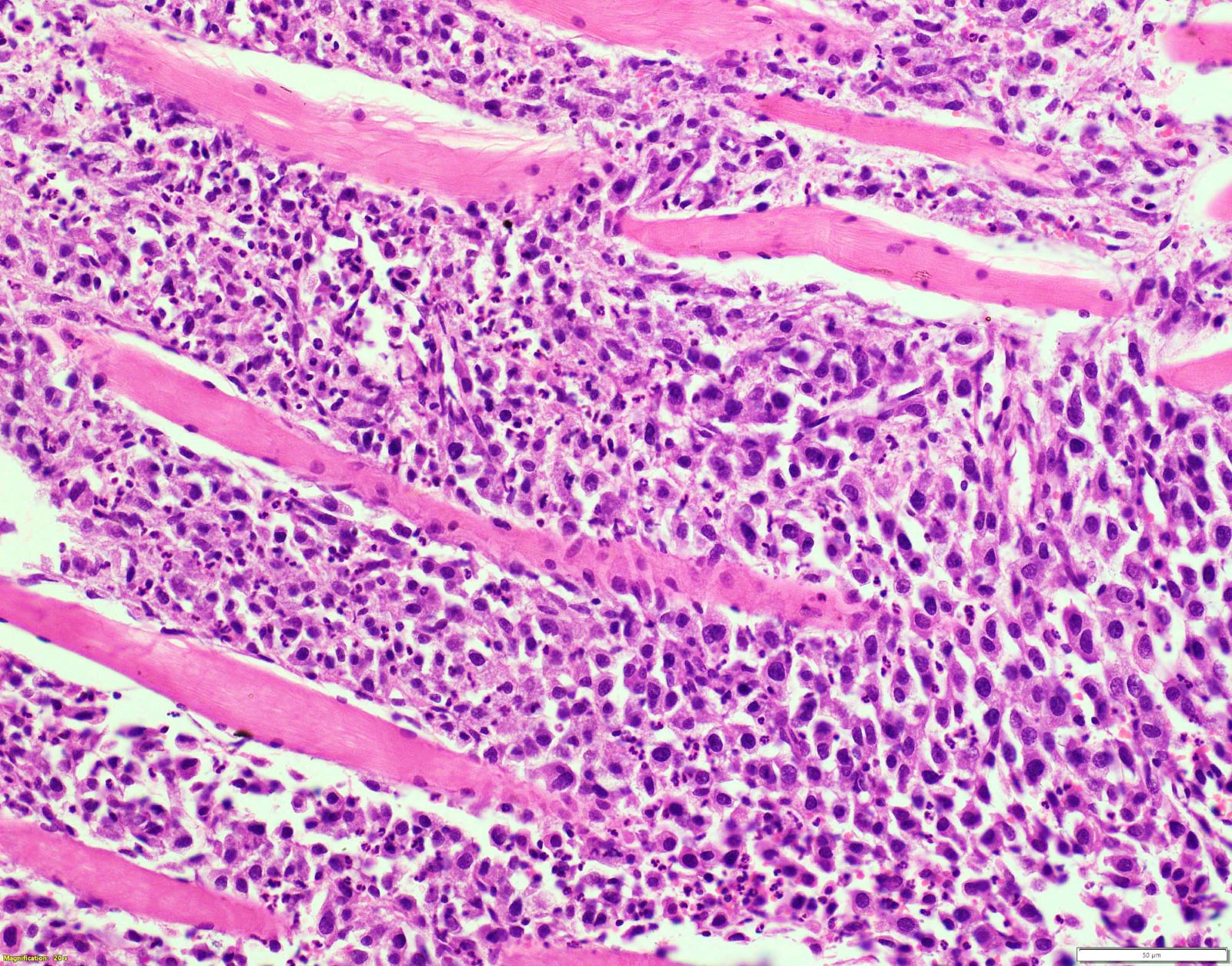
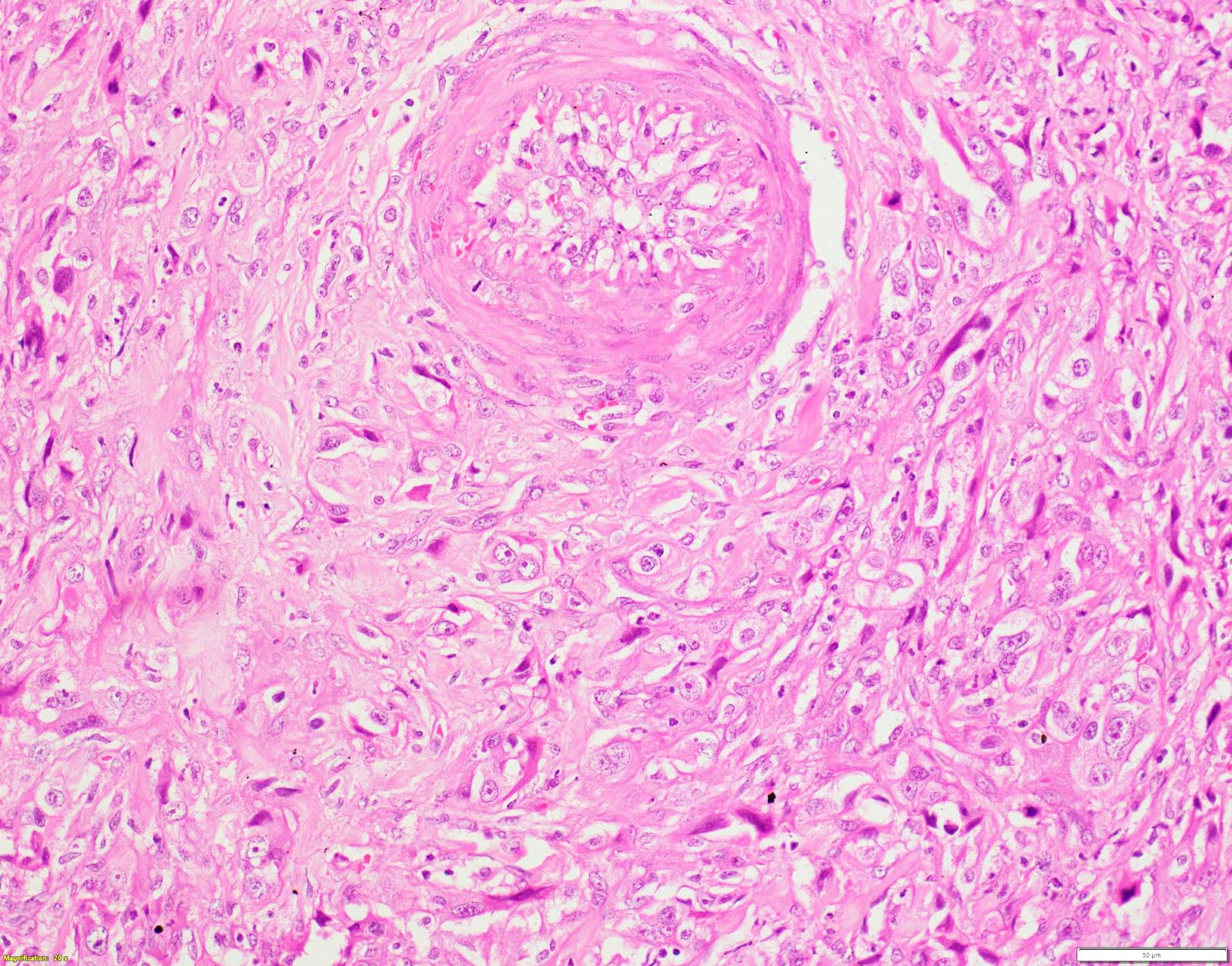
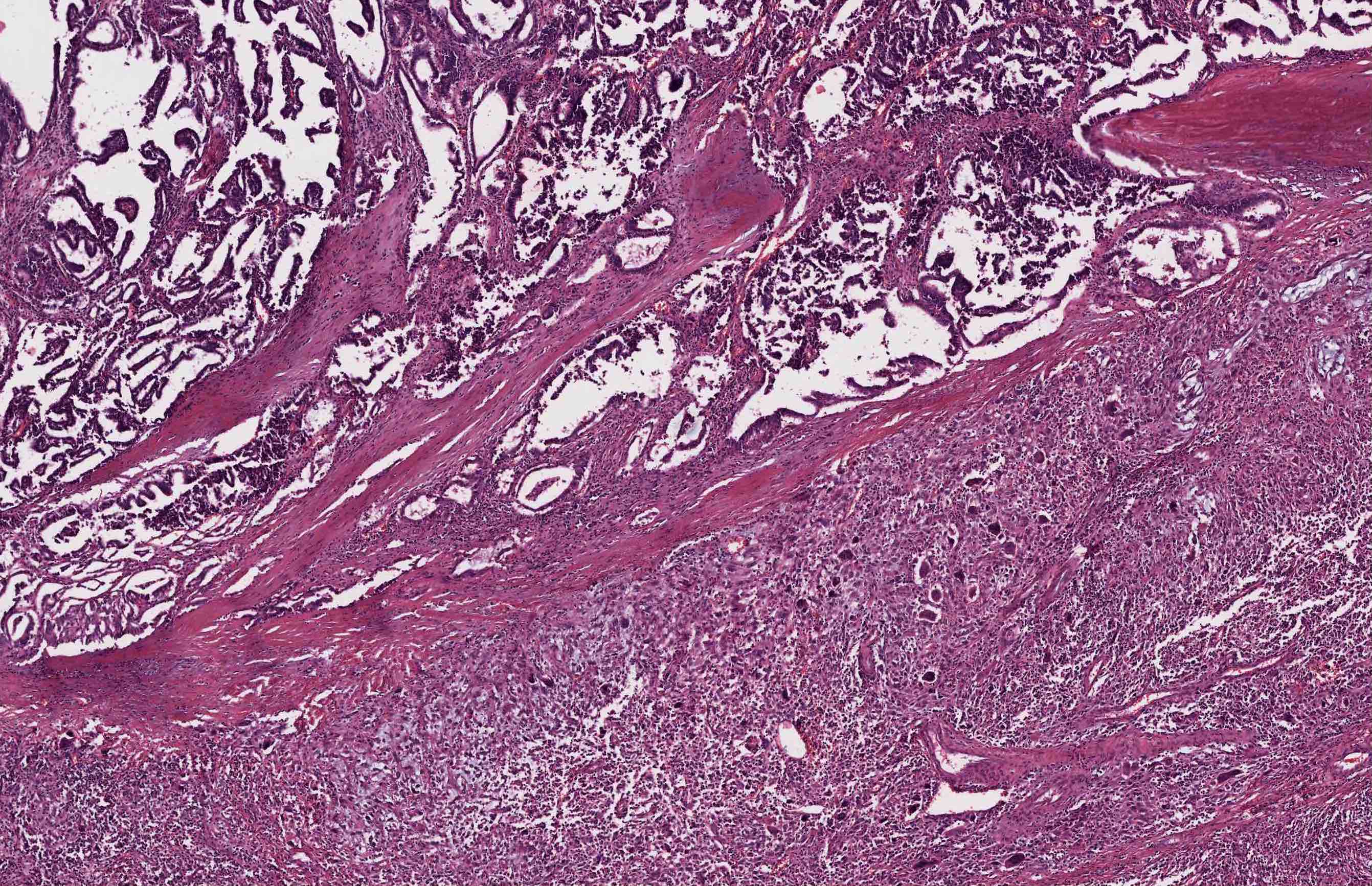
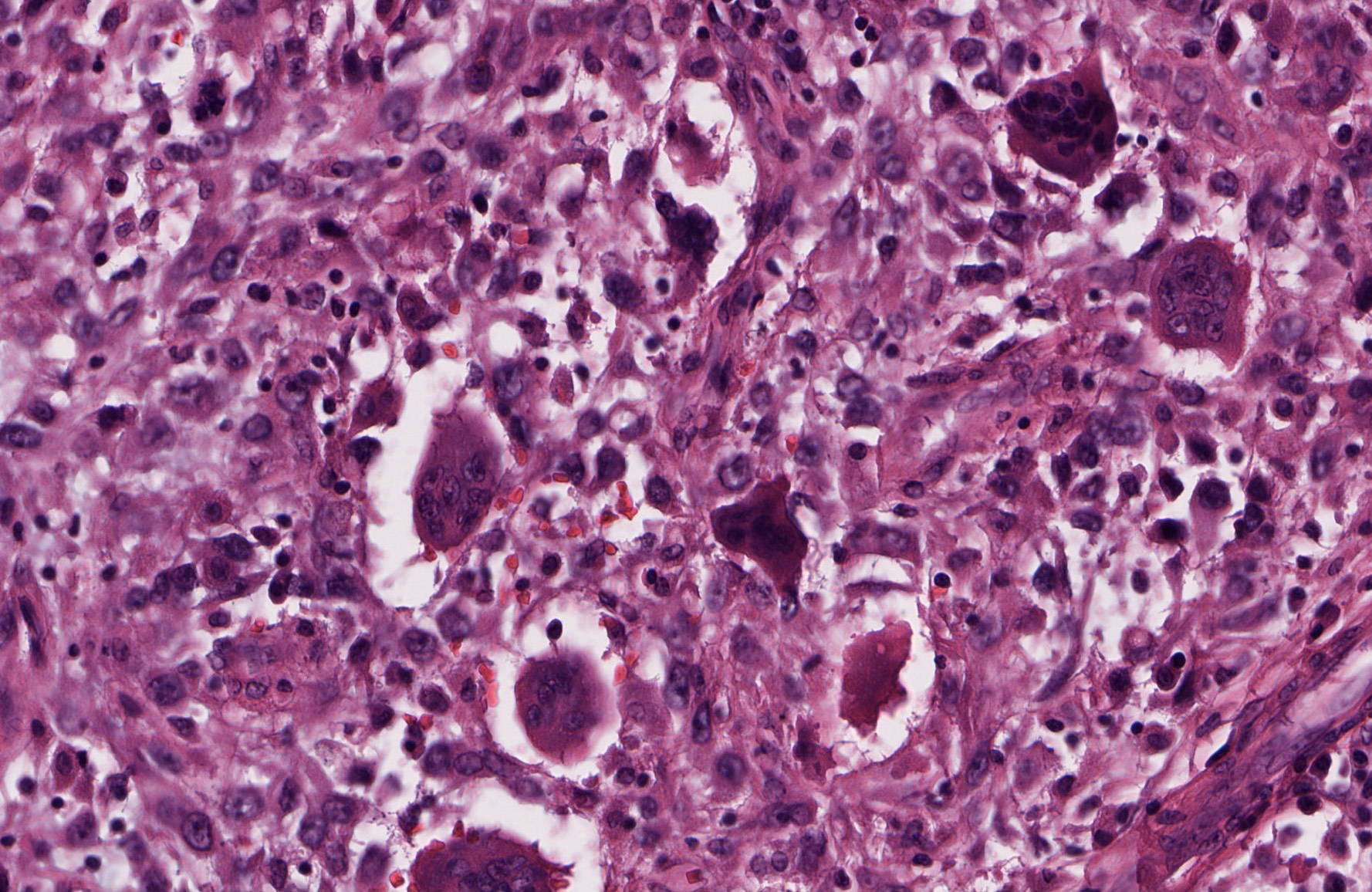
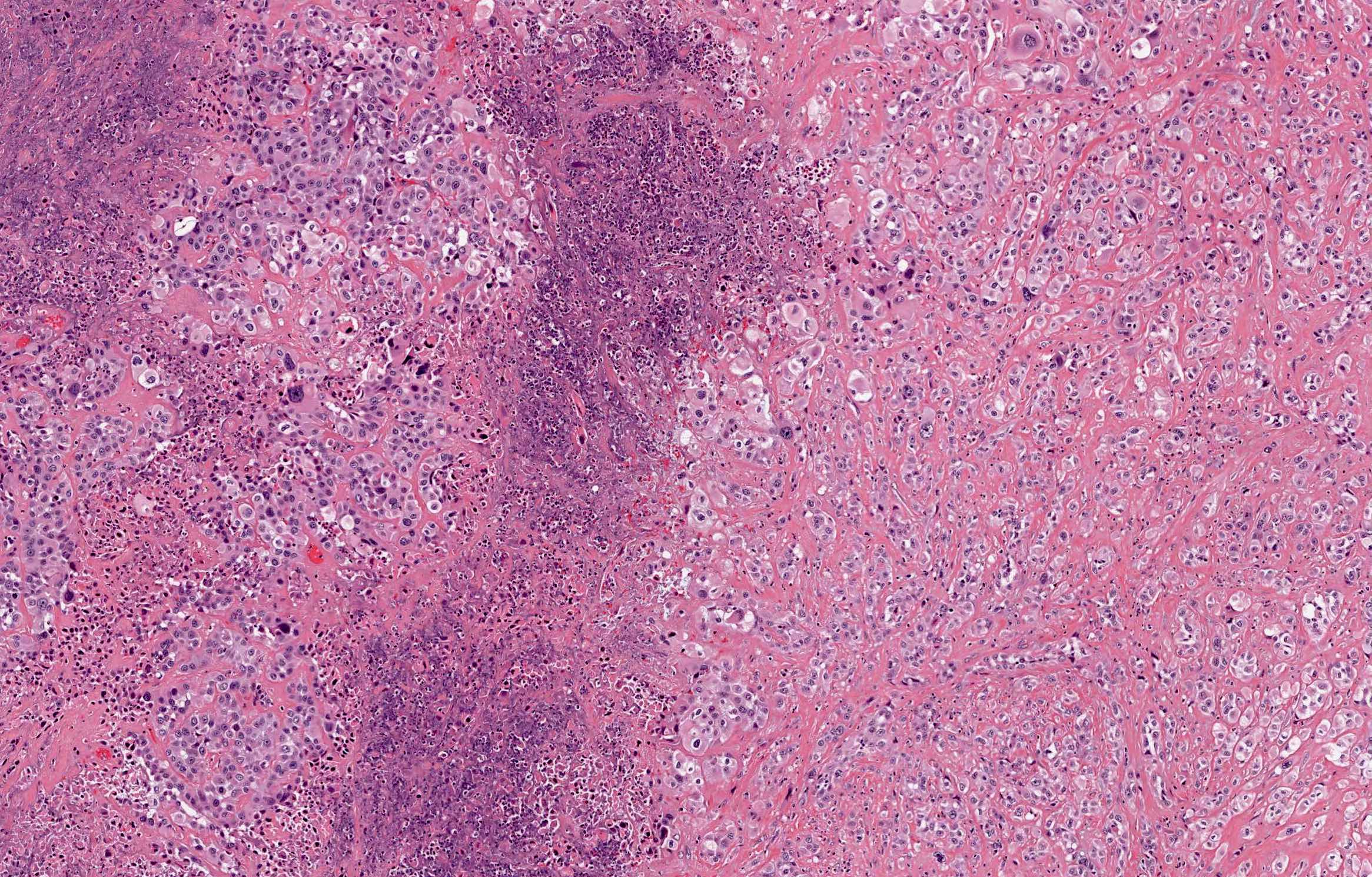
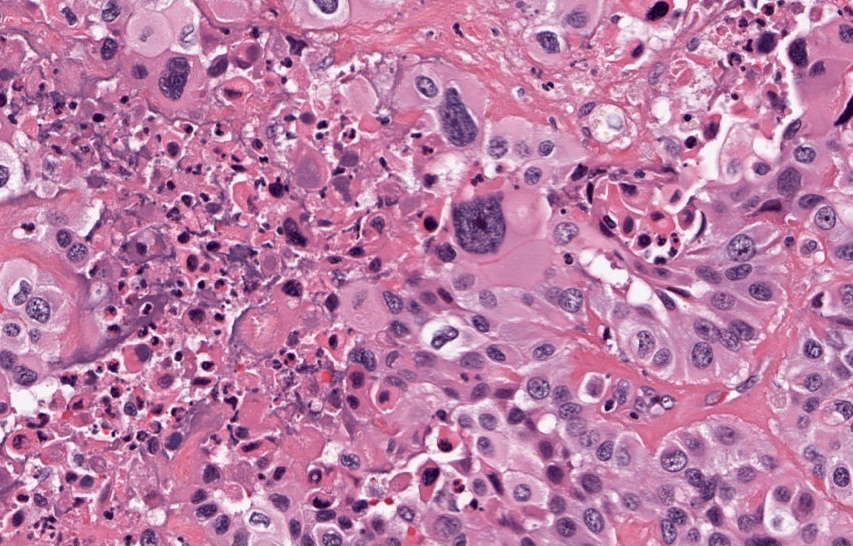
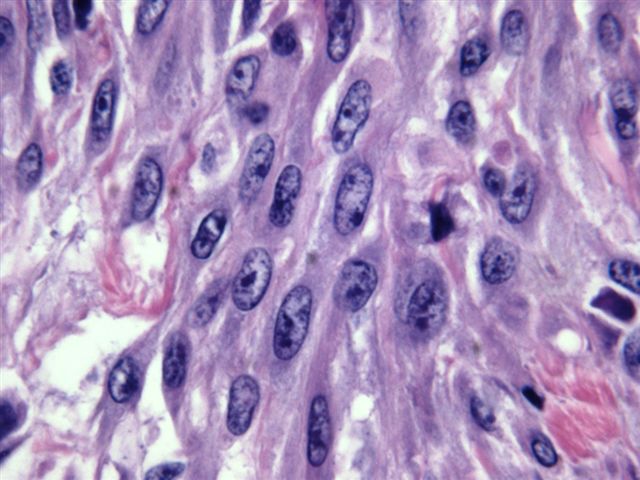
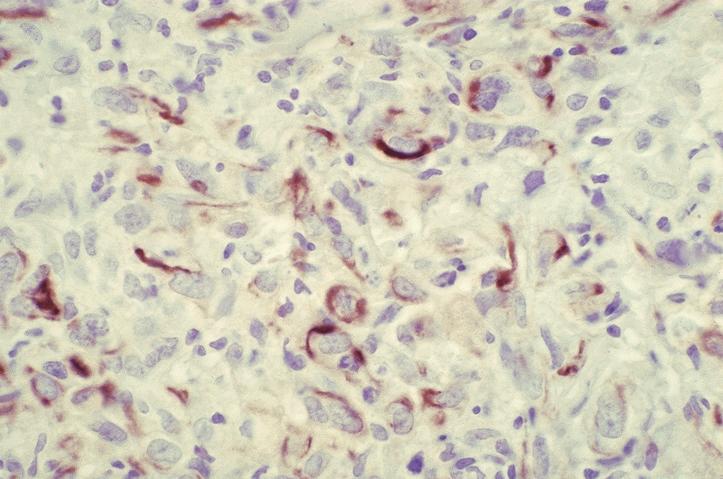
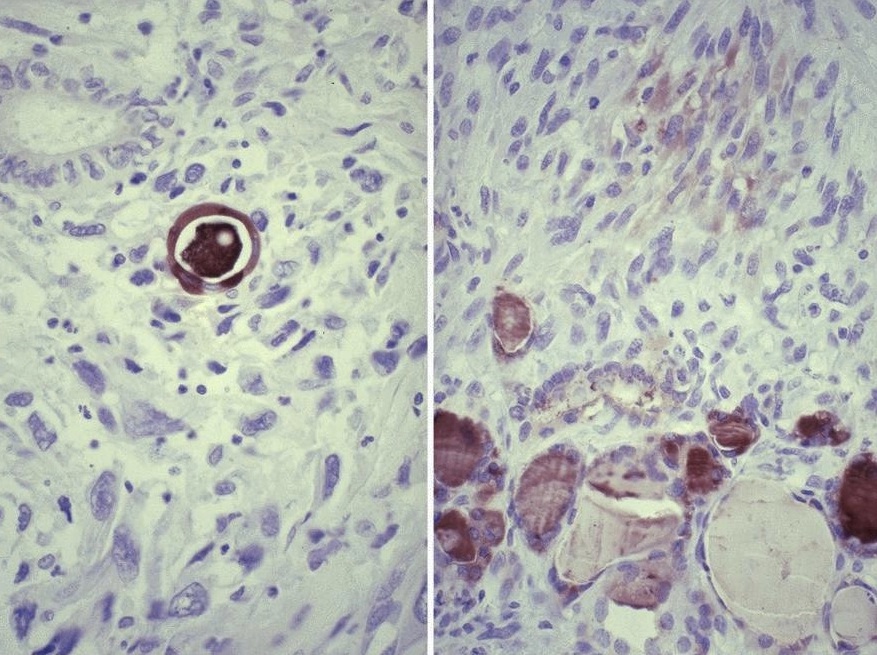
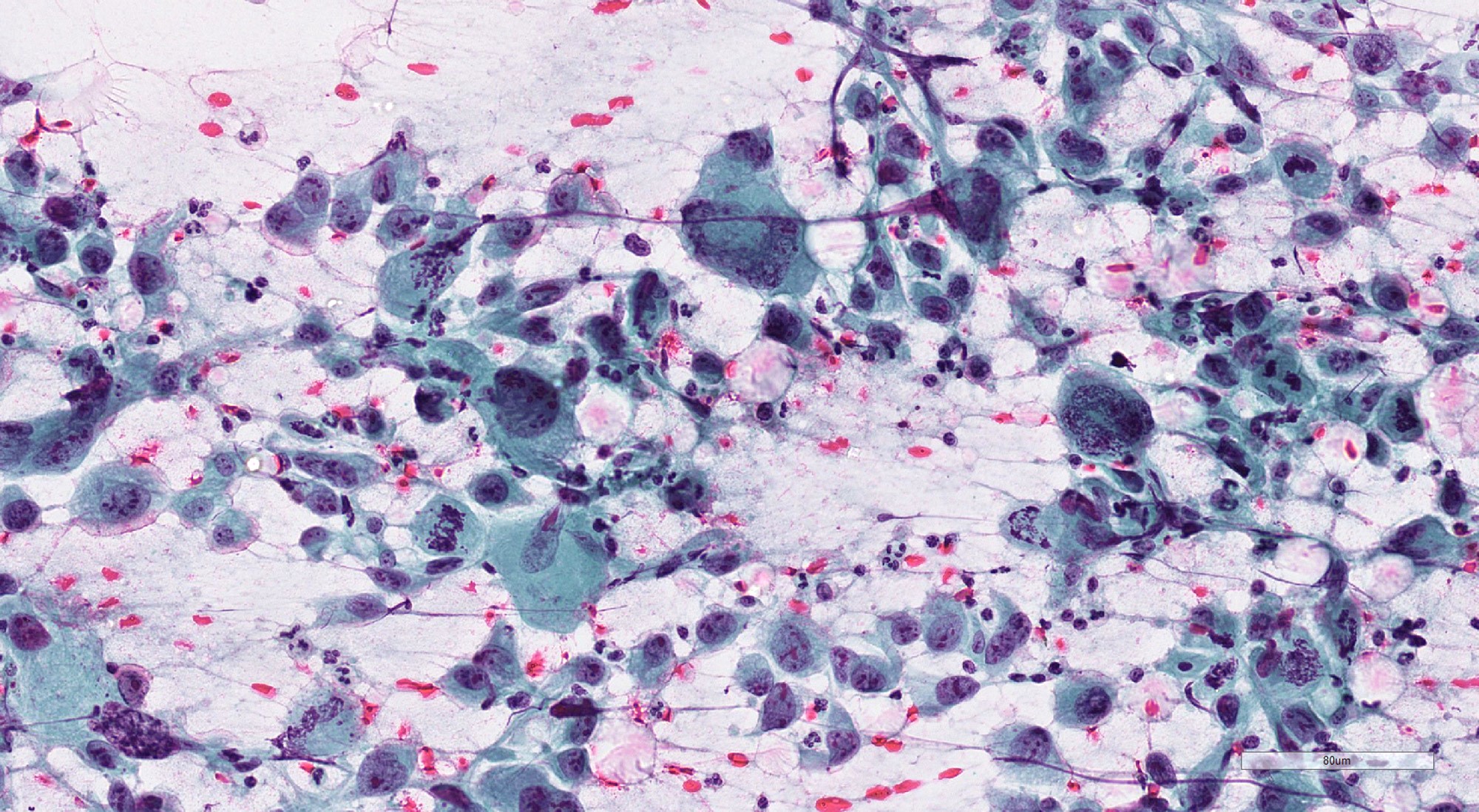
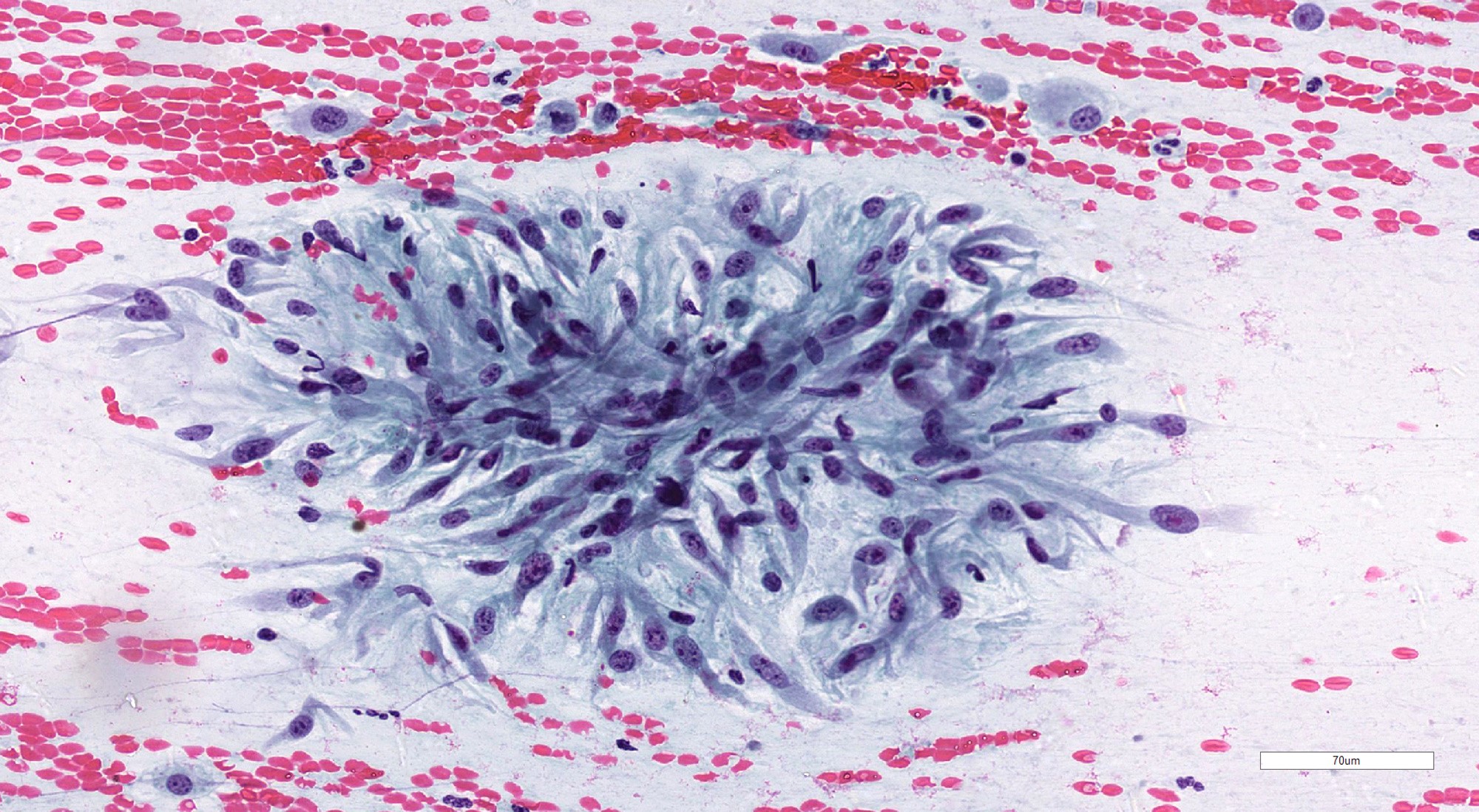
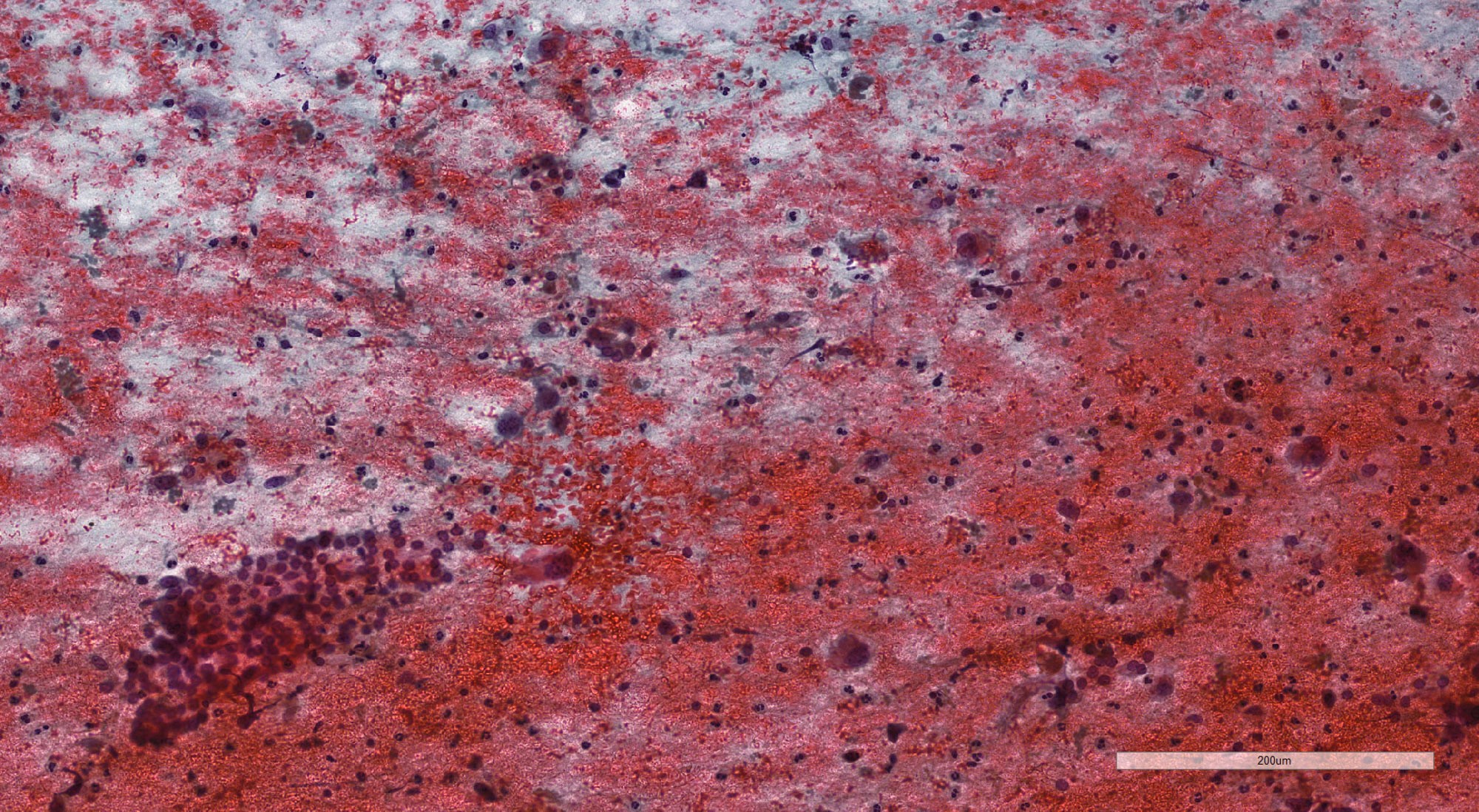
Microscopic (histologic) description
- Marked cellular pleomorphism
- Bizarre, hyperchromatic nuclei
- Prominent mitotic activity
- Atypical mitoses
- Necrosis, usually extensive
- Accompanied by acute inflammatory infiltrate, tumor associated macrophages
- Invasion
- Deep infiltration of adjacent structures such as trachea / larynx and esophagus, fibroadipose tissue and skin
- Vascular invasion
- Very rarely encapsulated (Thyroid 2020;30:1505)
- Coexistent DTC (papillary thyroid carcinoma, follicular thyroid carcinoma, oncocytic carcinoma of thyroid) or poorly differentiated thyroid carcinoma (PDTC) (Thyroid 2020;30:1505, Ann Surg 2000;231:329)
- Heterologous differentiation: bone, with or without cartilage
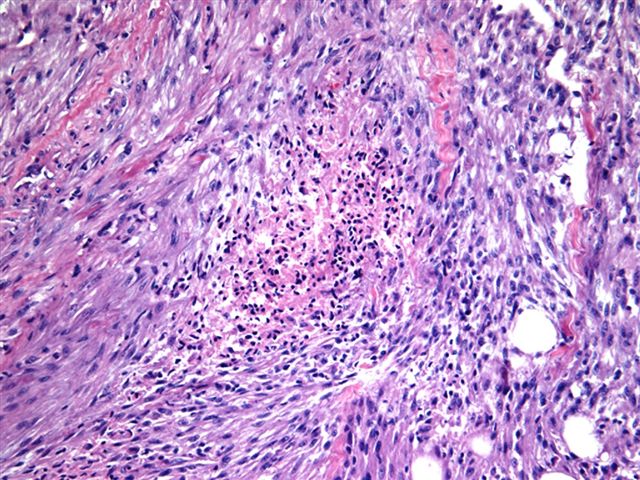
- Common patterns: epithelioid / squamoid, spindle / sarcomatoid, giant cell and pleomorphic; occur singly or in combination (Endocr Pathol 2022;33:27)
- Epithelioid / squamoid: tumor nests with abundant eosinophilic cytoplasm, appear squamoid, may show keratinization
- Spindle / sarcomatoid: malignant spindle cells simulating pleomorphic sarcoma
- Pleomorphic: highly pleomorphic tumor cells, having bizarre nuclei and prominent nucleoli, some with multiple nuclei
- Giant cell: numerous multinucleated giant cells, which can be cancer cells or macrophages
- Rare patterns (Endocr Pathol 2022;33:27)
- Squamous cell carcinoma pattern
- Focal or diffuse squamous phenotype (previously primary squamous cell carcinoma of thyroid) (Endocr Pathol 2022;33:27)
- Paucicellular
- Mimics Riedel thyroiditis
- Abundant fibrotic stroma, chronic inflammatory cell infiltrate
- Few atypical spindle cells
- Angiomatoid
- Irregular channels within tumor cell islands mimicking blood vessels
- May contain red blood cells
- Mimics angiosarcoma
- Rhabdoid
- Rhabdoid cells
- Eccentric nucleus, paranuclear inclusion, prominent nucleoli
- Lymphoepithelioma-like
- Sheets of tumor cells infiltrated by dense infiltrate of lymphocytes and plasma cells (Int J Endocrinol 2014;2014:790834)
- Mimics intrathyroidal thymic carcinoma
- Squamous cell carcinoma pattern
Microscopic (histologic) images
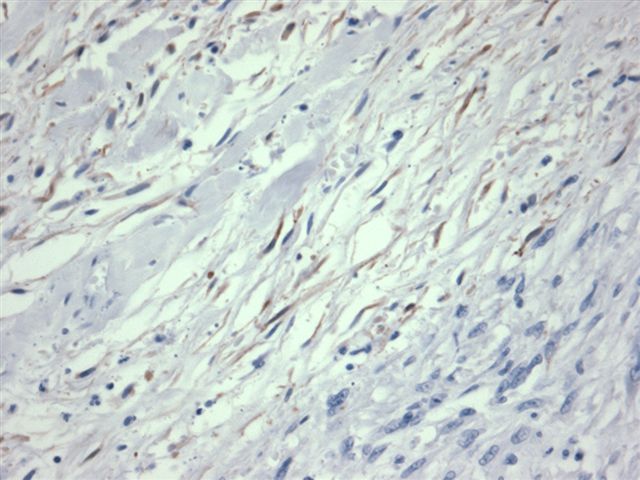
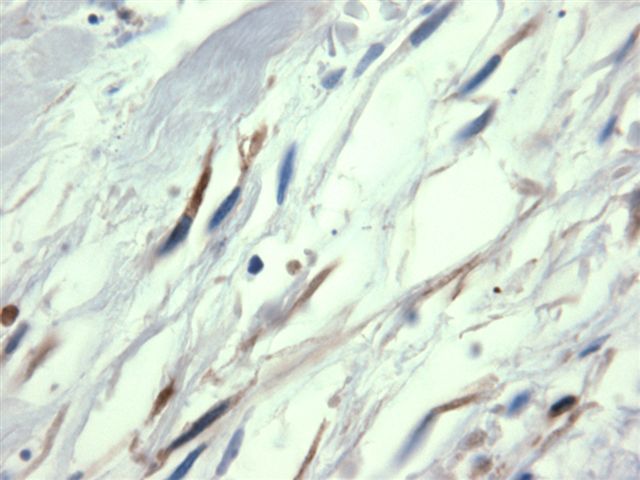
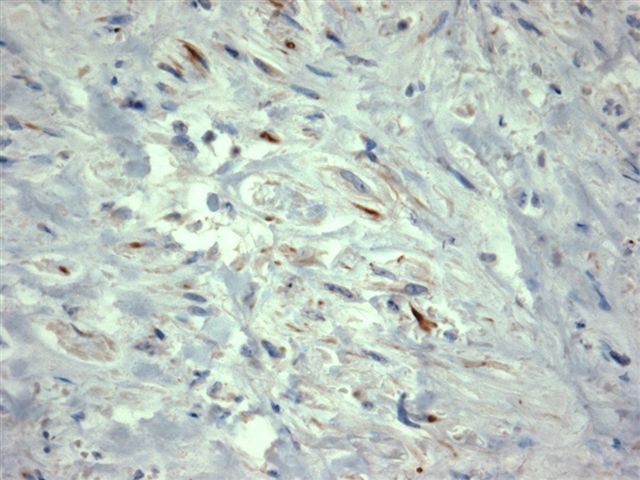
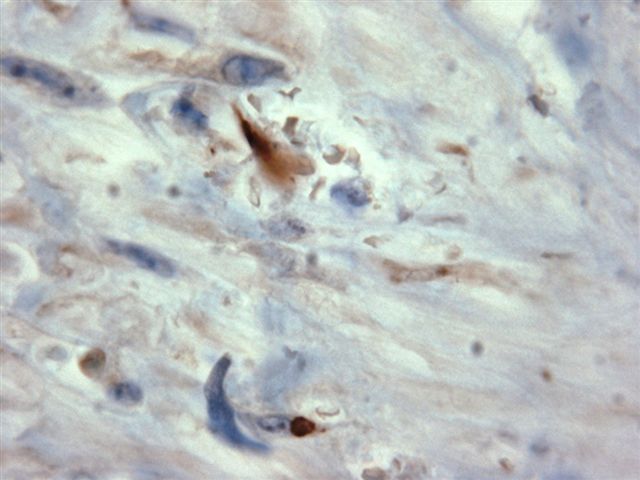
Contributed by Shipra Agarwal, M.D., Shuanzeng Wei, M.D., Ph.D., Stephen J. Schultenover, M.D. and AFIP
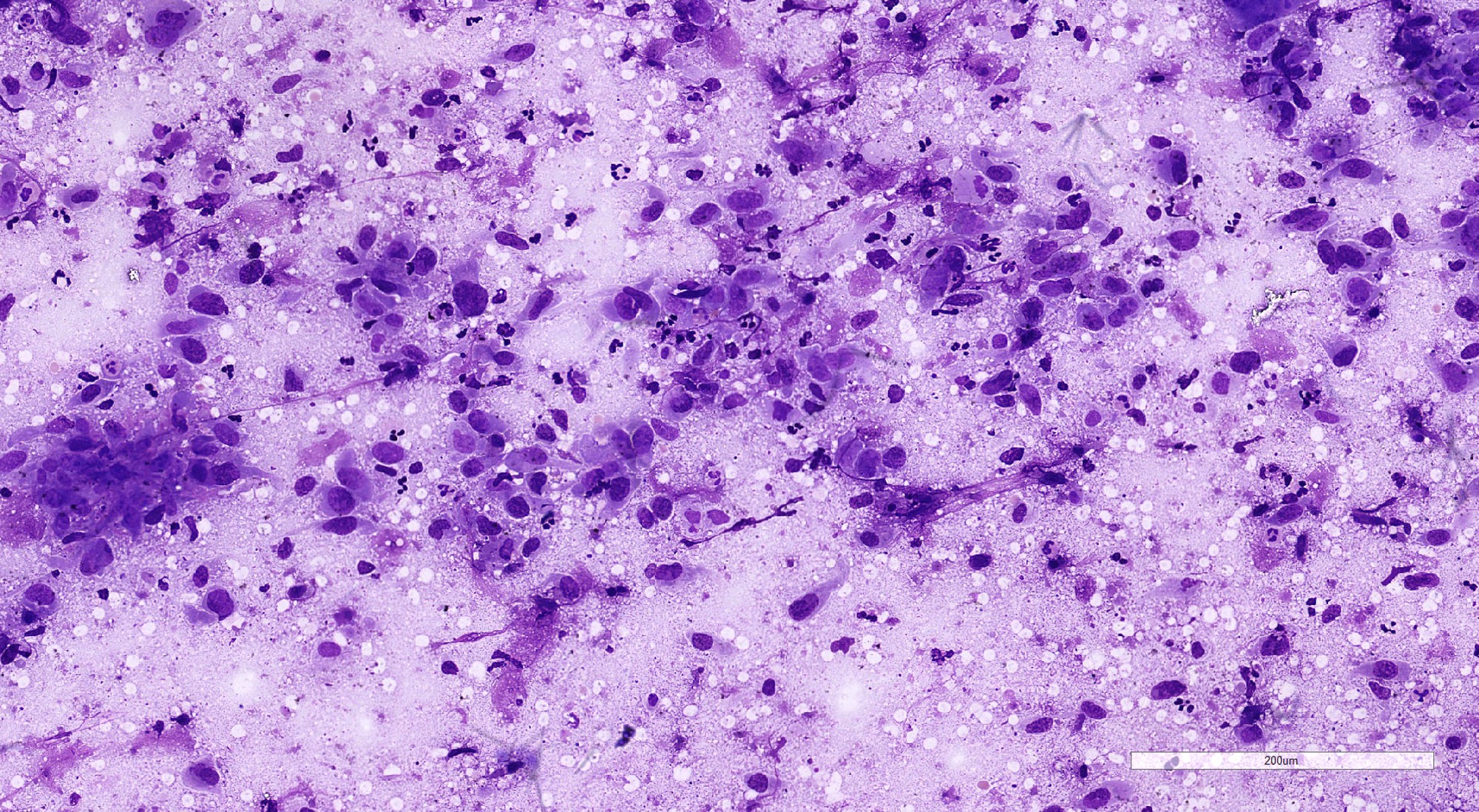
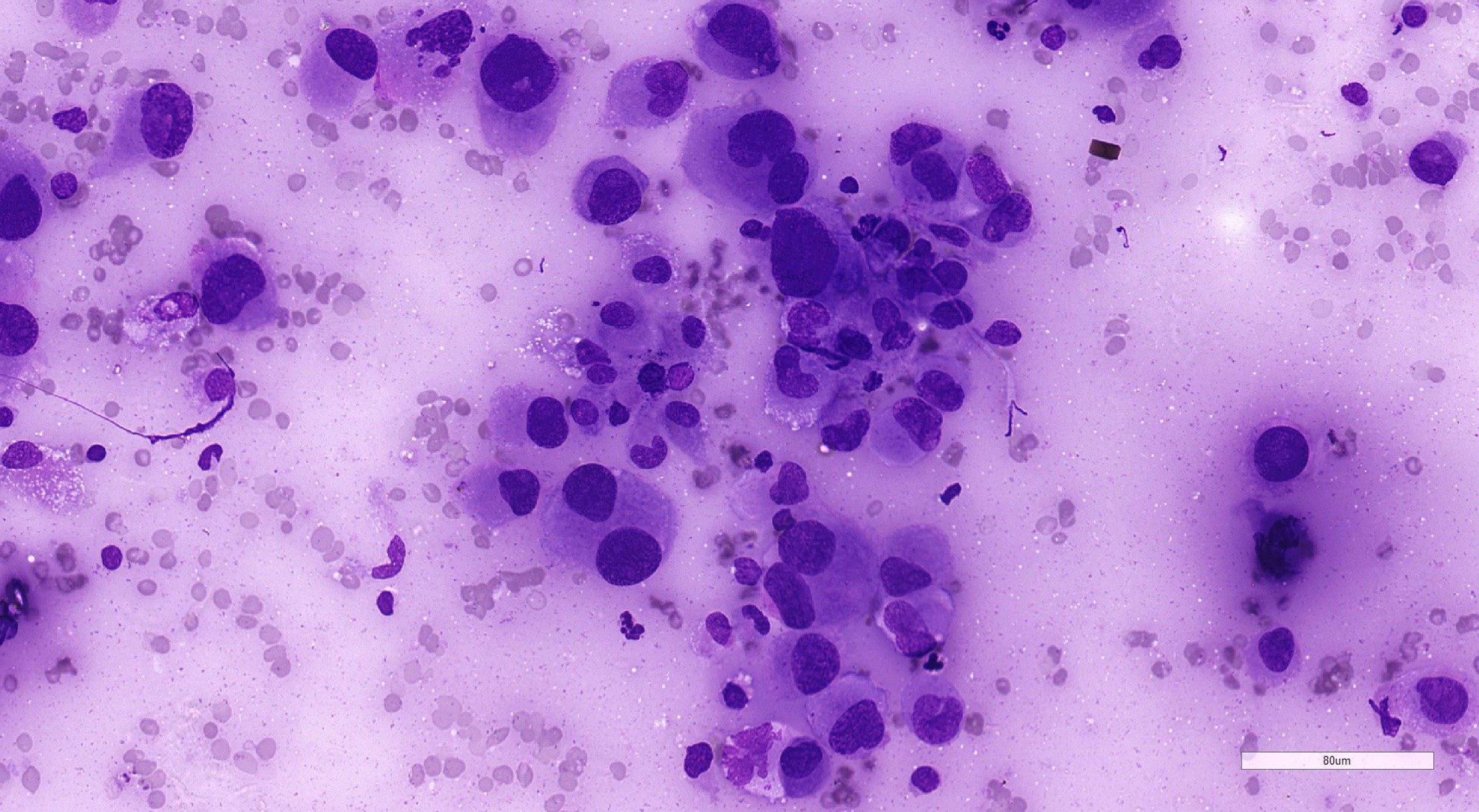
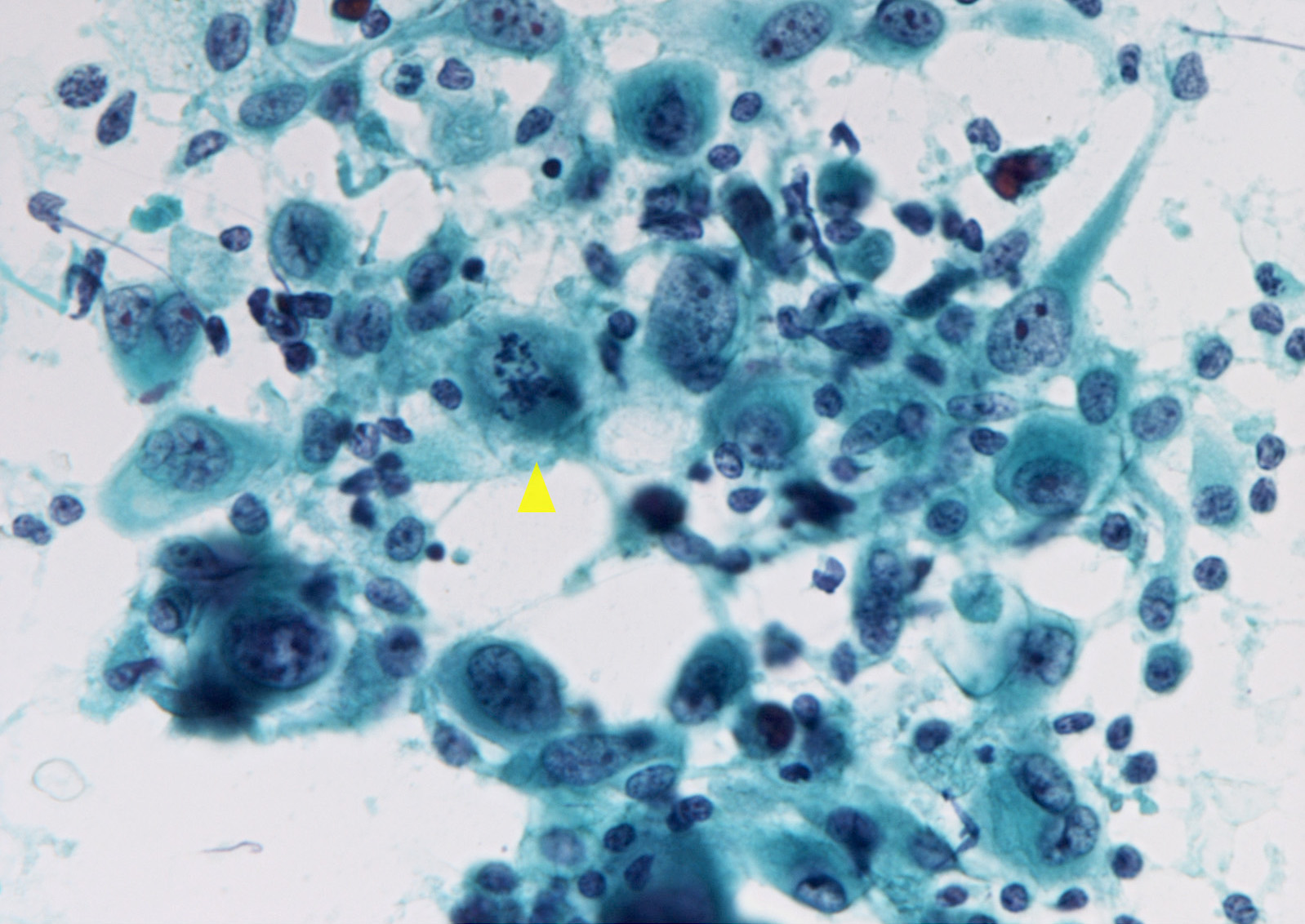
Cytology description
- Cellular or less commonly, sparse aspirate (Endocr Pathol 2022;33:27)
- Marked nuclear pleomorphism
- Epithelioid and spindle cells, osteoclast-like tumor giant cells
- Necrosis
- Mixed with acute inflammatory cells
- DTC component may be present
- Usually classified as Bethesda VI
Cytology images
Positive stains
- PAX8
- Immunopositivity varies with the histologic pattern: up to 100% of the squamoid and 50 - 60% of the sarcomatoid (Semin Diagn Pathol 2015;32:305)
- More likely to be positive in the presence of a DTC component
- Higher rate of positivity (60 - 80%) with less specific polyclonal antibody (Hum Pathol 2011;42:1873)
- ~50 - 60% when using monoclonal antibody (Virchows Arch 2020;476:431)
- Cytokeratin (50 - 70%) (Thyroid 2020;30:1505)
- Aberrant p53 expression (Thyroid 2020;30:1505)
- BRAF VE1 antibody detects BRAF V600E mutant protein (Cancers (Basel) 2020;12:596)
- Ki67 labeling index > 30%, often > 50%
- Epithelial membrane antigen and vimentin are frequently positive but have no role in diagnostic workup
Negative stains
- Markers of thyroid follicular cells: TTF1 and thyroglobulin
- Positive in coexisting DTC and PDTC, if present
- Markers of parafollicular cells: calcitonin, chromogranin, synaptophysin
- CD45
- S100, HMB45, melanA
- CK20
- Reference: Semin Diagn Pathol 2015;32:305
Molecular / cytogenetics description
- Genes involved in MAP kinase pathway
- BRAF V600E (40 - 70%) (Thyroid 2021;31:337)
- RAS mutations (15 - 40%)
- TERT promoter mutations (55 - 75%) (Endocrinol Metab Clin North Am 2019;48:269)
- E1F1AX mutation (10%) (Thyroid 2021;31:337)
- Mutations of MMR genes (MLH1, PMS2, MSH2 and MSH6) (5 - 10%) (Thyroid 2021;31:337)
- Mutations of DNA repair genes: ATM mutation (10%) (Thyroid 2020;30:1505, Thyroid 2021;31:337)
- Mutations involving tumor suppressor genes
- TP53 mutation (30 - 70%) (Endocrinol Metab Clin North Am 2019;48:269, Thyroid 2021;31:337, Endocr Pathol 2016;27:205)
- NF2 mutation (12%) (Thyroid 2020;30:1505, Clin Cancer Res 2018;24:3059)
- NF1 mutation (10%)
- RB1 mutation (10%)
- MEN1 mutation
- Alterations in cell cycle genes (CDKN2A, CDKN2B, CCNE1) (Thyroid 2020;30:1505, Clin Cancer Res 2018;24:3059)
- Mutations in genes of PI3K / AKT pathway
- PIK3CA mutations (10 - 20%) (Endocr Pathol 2022;33:27, Thyroid 2021;31:337)
- PTEN mutation (10 - 15%)
- AKT1, AKT2 mutations (< 5%)
- Gene fusions: RET, NTRK
- ALK mutations, ALK fusions
Molecular / cytogenetics images
Videos
Cytology of ATC
Management of ATC
Sample pathology report
- Thyroid, total thyroidectomy:
- Anaplastic thyroid carcinoma, epithelioid pattern, 12 cm, replacing the entire specimen (see synoptic report)
- It is dedifferentiating from papillary thyroid carcinoma, classical subtype
- Gross extrathyroidal extension into adjoining skeletal muscles
- Multiple lymphovascular emboli and perineural invasion are present
- 4 of the 5 lymph nodes dissected from the specimen are involved by tumor
- AJCC stage IVB (pT3bN1Mx)
- Immunohistochemically, the tumor cells are positive for pan-CK, PAX8, VE1 and p53 but are negative for TTF1 and TG; the Ki67 labeling index is 35%
- Thyroid, needle biopsy:
- Anaplastic thyroid carcinoma, spindle cell pattern
- Immunohistochemically, the tumor cells are positive for pan-CK, vimentin and p53 but are negative for PAX8, p40 and VE1; the Ki67 labeling index is 55%
- Findings corroborate with but are not specific for the above diagnosis; a clinicoradiological correlation is advised
- Thyroid, fine needle cytology:
- Malignant (Bethesda diagnostic category VI): anaplastic thyroid carcinoma, pleomorphic pattern
- Immunohistochemistry performed on cell block shows that the tumor cells are positive for pan-CK and PAX8 but are negative for VE1
- The findings corroborate with but are not specific for the above diagnosis; a clinicoradiological correlation is advised
Differential diagnosis
- Poorly differentiated thyroid carcinoma (Thyroid 2021;31:337, Nat Rev Endocrinol 2017;13:644):
- Small uniform cells arranged as nests and trabeculae
- Lesser nuclear pleomorphism, atypia and mitotic activity
- Patchy necrosis thyroglobulin, TTF1 positive
- Riedel thyroiditis:
- Absent atypia, mitoses
- Squamous cell carcinoma of head and neck:
- Absent DTC component
- Site specific clinical features and radiology
- PAX8 negative
- Medullary thyroid carcinoma:
- Amyloid
- Stippled chromatin
- Chromogranin, synaptophysin, calcitonin, carcinoembryonic antigen immunopositivity
- Non-Hodgkin lymphoma:
- LCA positive and cytokeratin negative
- Lineage specific immunoprofile
- Absent DTC component
- Squamous metaplasia in differentiated thyroid tumors and chronic thyroiditis:
- Absence of nuclear pleomorphism, mitosis, necrosis and a large invasive front
- Low Ki67 index, usually < 5%
- Angiosarcoma:
- PAX8 negative
- Absent DTC component
- Pleomorphic sarcoma:
- Cytokeratin and PAX8 negative
- Lineage specific immunoprofile
- Absent DTC component
- Spindle epithelial tumor with thymus-like differentiation (SETTLE):
- Less pleomorphism
- Smooth muscle actin positive
- Intrathyroid thymic carcinoma (CASTLE; carcinoma showing thymus-like element):
- Metastatic carcinoma:
- Metastatic malignant melanoma:
Practice question #1
- A 72 year old woman presented with a hoarse voice and rapid enlargement of neck mass of 3 months' duration. Radiology revealed lumbar vertebral metastases. Cytological examination from the low anterior neck mass showed a tumor composed of mitotically active pleomorphic polygonal and spindle cells in a necrotic and inflammatory background. Incisional biopsy revealed a malignant spindle cell tumor. What is the most likely diagnosis?
- Anaplastic thyroid carcinoma
- Follicular thyroid carcinoma
- Metastatic carcinoma to thyroid gland
- Papillary thyroid carcinoma
- Spindle epithelial tumor with thymus-like differentiation
Practice answer #1
A. Anaplastic thyroid carcinoma. Anaplastic thyroid carcinoma typically presents with a short duration history of a rapidly enlarging neck mass, with symptoms secondary to compression of adjacent structures, such as pain, dysphonia, dysphagia, dyspnea and cough. Lymph node and distant metastases are common. Cytological examination reveals a pleomorphic tumor cell population, including bizarre forms, dispersed in a necrotic and inflammatory background. Mitotic activity is frequent and atypical mitotic forms common. Answer B is incorrect because follicular thyroid carcinoma, on cytology, shows a microfollicular architecture and lacks marked cellular pleomorphism and extensive necrosis. Answer C is incorrect because the clinical presentation of hoarseness of voice, a rapidly enlarging neck mass and radiology revealing distant metastases are indicative of a thyroid primary. Answer D is incorrect because papillary thyroid carcinoma, on cytological evaluation, lacks cellular pleomorphism and extensive necrosis. Instead, classic papillary thyroid carcinoma shows follicular cells arranged as papillae, sheets and fragments showing typical nuclear features. Answer E is incorrect because spindle epithelial tumor with thymus-like elements is characterized by low grade spindle cells and an amyloid-like material with or without an epithelial component.
Comment Here
Reference: Anaplastic thyroid carcinoma
Comment Here
Reference: Anaplastic thyroid carcinoma
Practice question #2
- Which of the following immunohistochemical profiles best defines anaplastic thyroid carcinoma?
- TTF1 negative, thyroglobulin negative, CD5 positive, CD117 positive
- TTF1 negative, thyroglobulin negative, PAX8 positive, cytokeratin positive
- TTF1 negative, thyroglobulin negative, S100 positive, HMB45 positive
- TTF1 positive, thyroglobulin negative, PAX8 negative, calcitonin positive
- TTF1 positive, thyroglobulin positive, PAX8 positive, vimentin negative
Practice answer #2
B. TTF1 negative, thyroglobulin negative, PAX8 positive, cytokeratin positive. Anaplastic thyroid carcinoma (ATC) is usually immunonegative for TTF1 and thyroglobulin but expresses PAX8; cytokeratin is variably positive. Answer E is incorrect because vimentin can also be variably positive in ATC but in this case thyroglobulin is positive as well. Answer D is incorrect because calcitonin is immunopositive in medullary thyroid carcinoma. Answer A is incorrect because CD5 and CD117 are positive in intrathyroidal thymic carcinoma. Answer C is incorrect because S100 and HMB45 are positive in malignant melanoma.
Comment Here
Reference: Anaplastic thyroid carcinoma
Comment Here
Reference: Anaplastic thyroid carcinoma