Table of Contents
Definition / general | Essential features | Epidemiology | Diagrams / tables | Etiology | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Wei S. Follicular thyroid carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidfollicular.html. Accessed October 3rd, 2025.
Definition / general
- Thyroid carcinoma with follicular differentiation but no papillary nuclear features (Hürthle cell (oncocytic) carcinoma is discussed separately)
- Comprises 6 - 10% of thyroid carcinomas
- Insufficient dietary iodine is a risk factor
- Usually solitary "cold" nodule on radionuclide scan
- Extensive sampling of capsule is recommended (Am J Surg Pathol 1992;16:392)
- Three types (Lloyd: WHO Classification of Tumours of Endocrine Organs, 2017):
- Minimally invasive follicular carcinoma
- With capsular invasion only
- Encapsulated angioinvasive:
- Tumors with limited vascular invasion (< 4) have a better prognosis than those with extensive vascular invasion
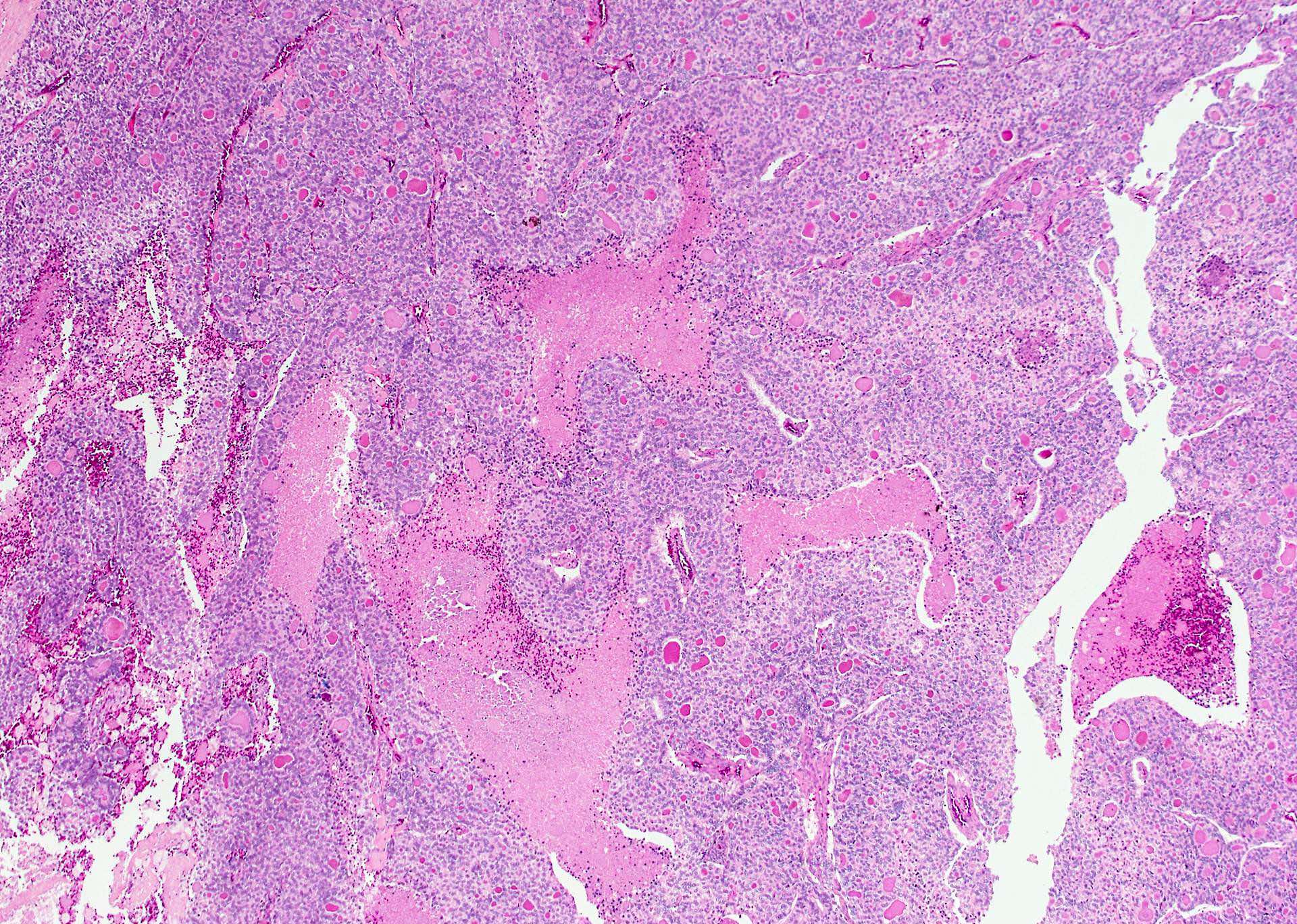
- Widely invasive:
- Extensive invasion of thyroid and extrathyroidal soft tissue
- Minimally invasive follicular carcinoma
- Two types (ARP: Tumors of the Thyroid and Parathyroid Glands, 2016):
- Minimally invasive follicular carcinoma
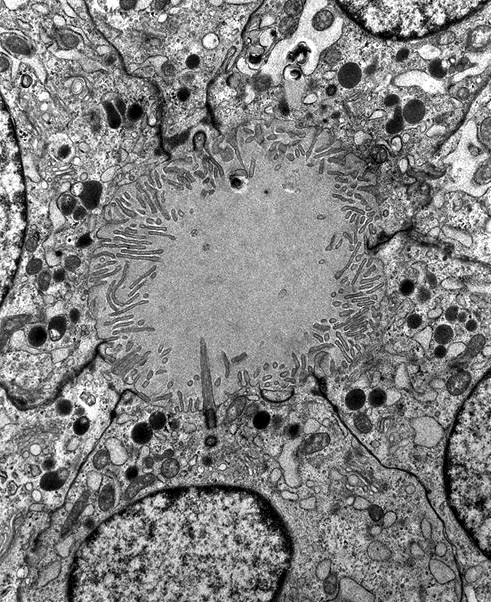
- With capsular invasion (not obvious, need to search)
- With limited (fewer than 4 vessels) vascular invasion
- With extensive (4+ vessels) vascular
- Widely invasive
- Minimally invasive follicular carcinoma
Essential features
- Follicular lesion with capsular or vascular invasion but without papillary nuclear features
Epidemiology
- 75% women
- Older age than papillary carcinoma, peak age: 40 - 60
- Rarely in children
Diagrams / tables
Etiology
- Iodine deficiency and irradiation exposure, older age
Clinical features
- Usually "cold" on radionuclide scan
- May arise from preexisting adenoma
- Does not metastasize through lymphatics but does spread to lungs, liver, bone, brain via blood vessels
- Less than 5% with ipsilateral lymphadenopathy
- Up to 69% distant metastasis: lung and bone (common in widely invasive carcinoma)
Radiology description
- Ultrasound: solid hypoechoic nodule with a peripheral halo (fibrous capsule); irregular or poorly defined margins may be suggestive of carcinoma
Prognostic factors
- Minimally invasive follicular carcinoma: very low long term mortality (Cancer 2001;91:505)
- Widely invasive: 50% long term mortality
- Poor prognostic factors: tumor size greater than 4 cm, distant metastases, age greater than 45 years, large size, extensive vascular invasion, extrathyroidal extension (World J Surg 2007;31:1417)
Case reports
- 33 year old pregnant woman with lung and bone metastases (Hormones (Athens) 2006;5:295)
- 61 year old woman with tumor dissemination along fine needle aspiration track (Surg Today 2007;37:34)
- 76 year old woman with multiple giant scalp metastases (World J Surg Oncol 2008;6:82)
Treatment
- T3 / T4 to suppress endogenous TSH, thyroidectomy and radioactive iodine
- No nodal dissection is needed
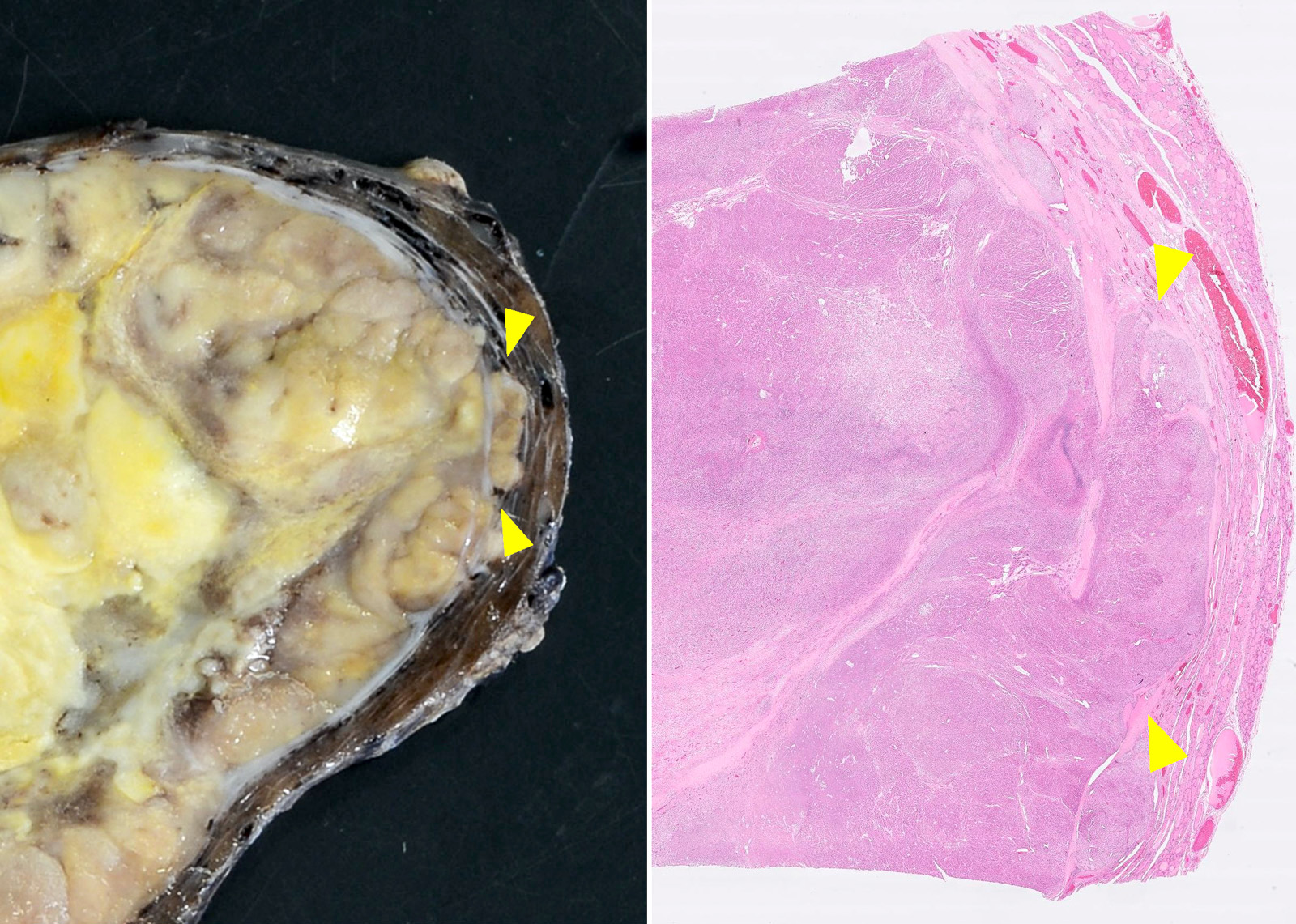
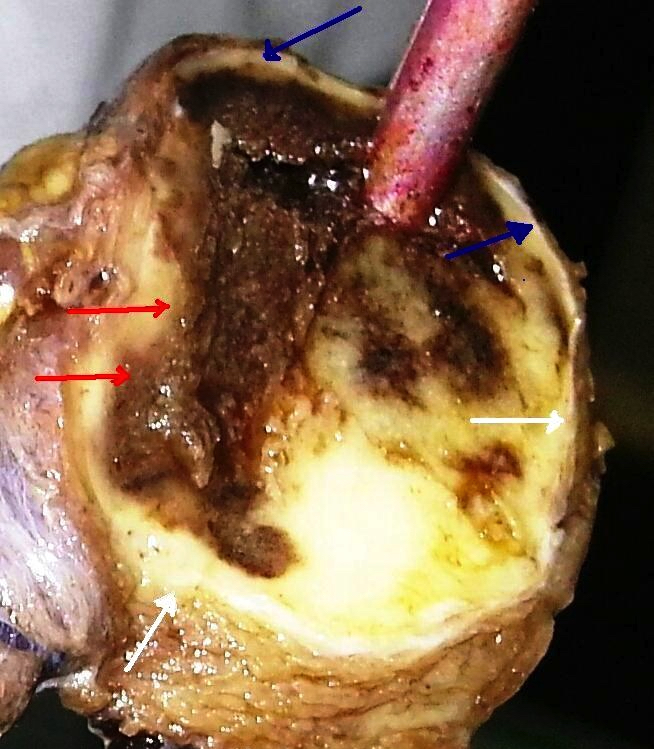
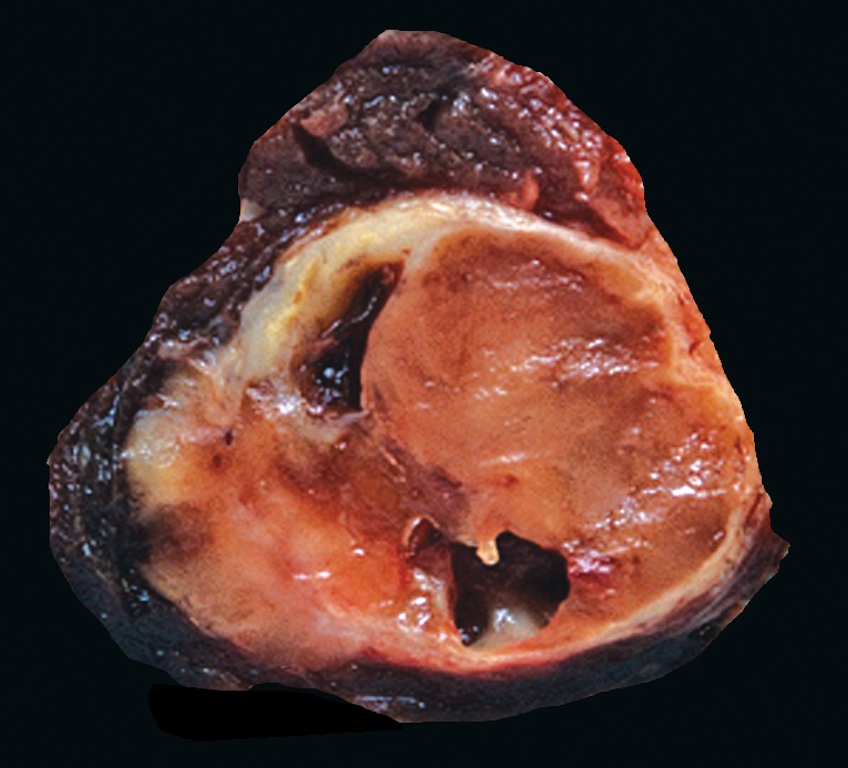
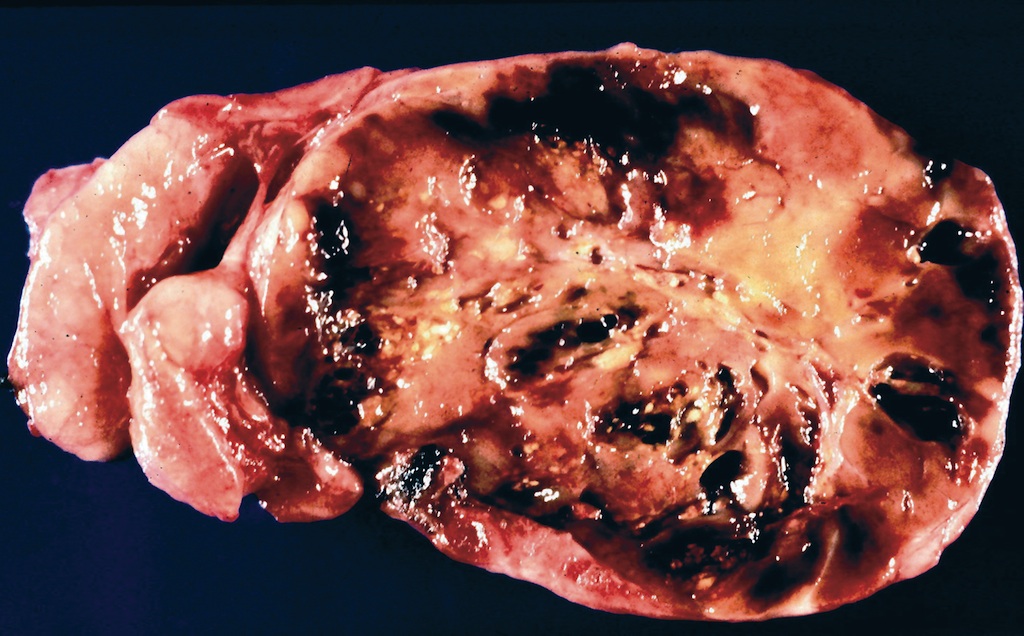
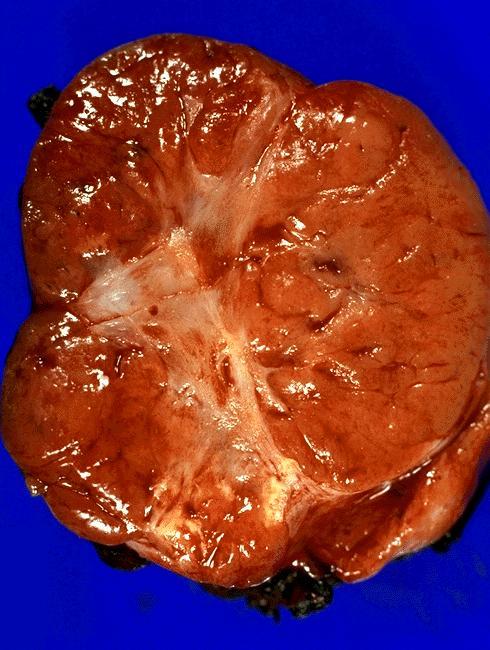
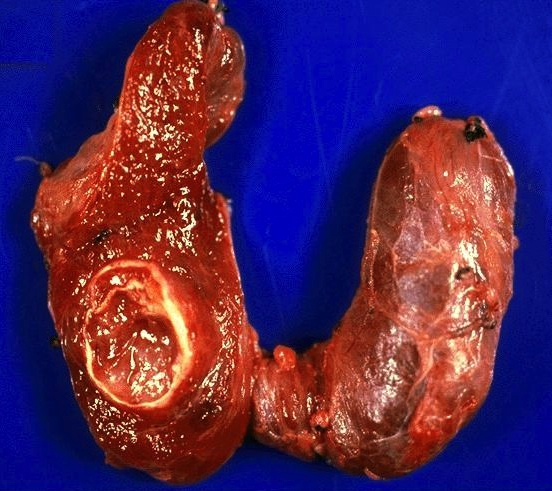
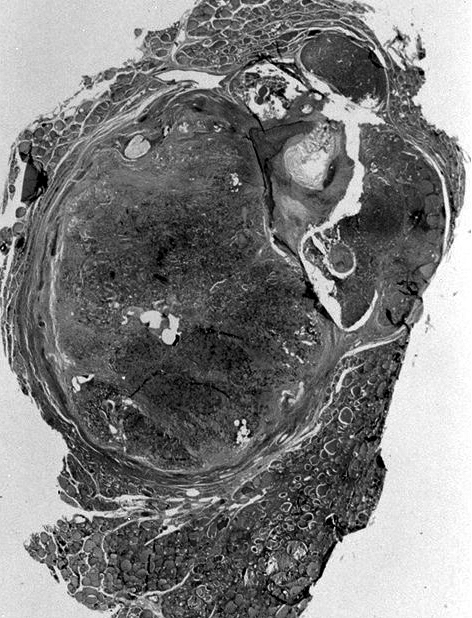
Gross description
- Tan to brown solid cut surface, can have cystic changes and hemorrhage
- Minimally invasive: usually single encapsulated nodule, with thickened and irregular capsule
- Widely invasive: extensive permeation of capsule or no capsule
- All capsule with adjacent tissue needs to be submitted for histological evaluation
Gross images
Contributed by Andrey Bychkov, M.D., Ph.D., Wafaey Fahmy Badawy Mohamed, M.D., Mark R. Wick, M.D. and AFIP
Images hosted on other servers:
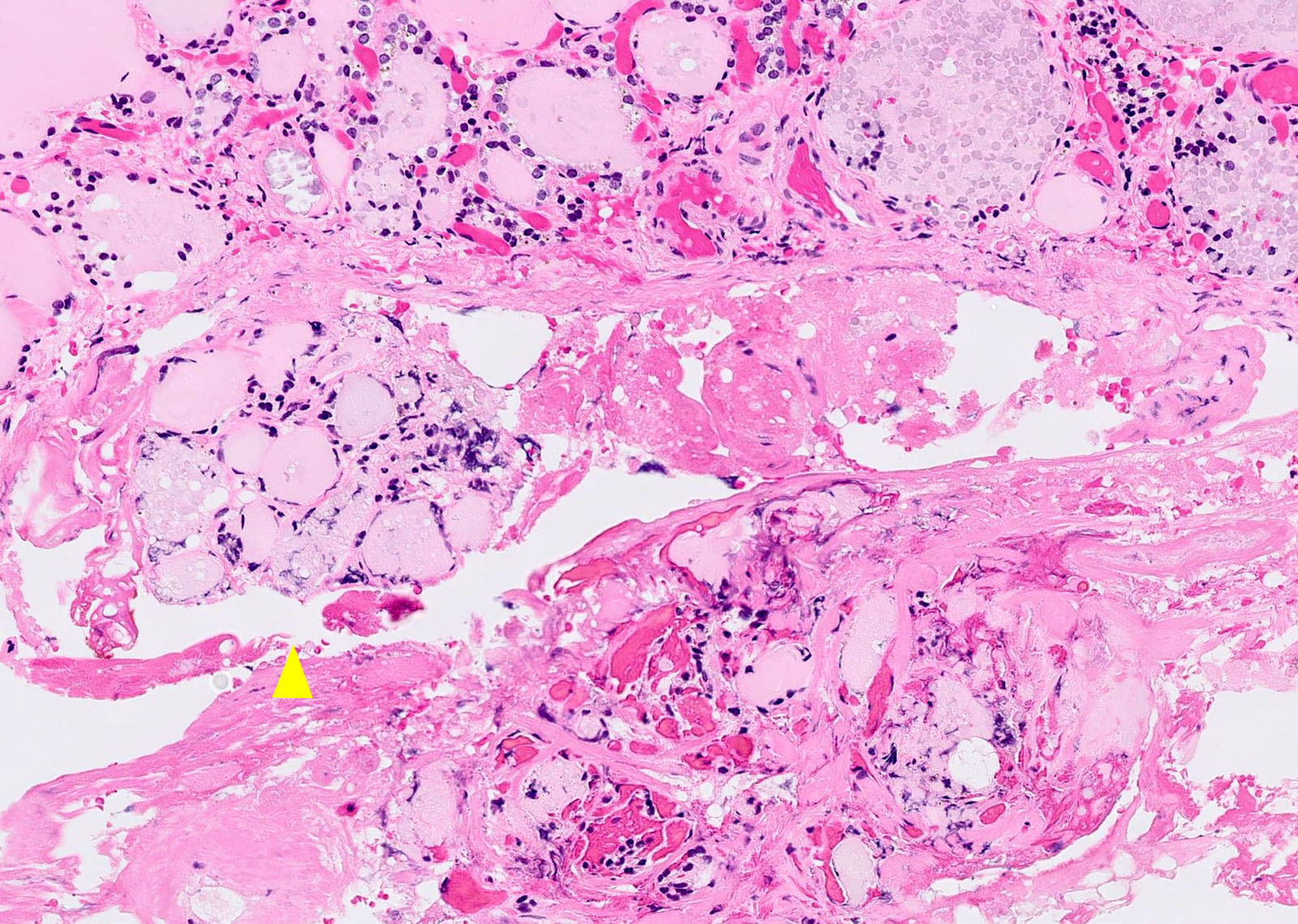
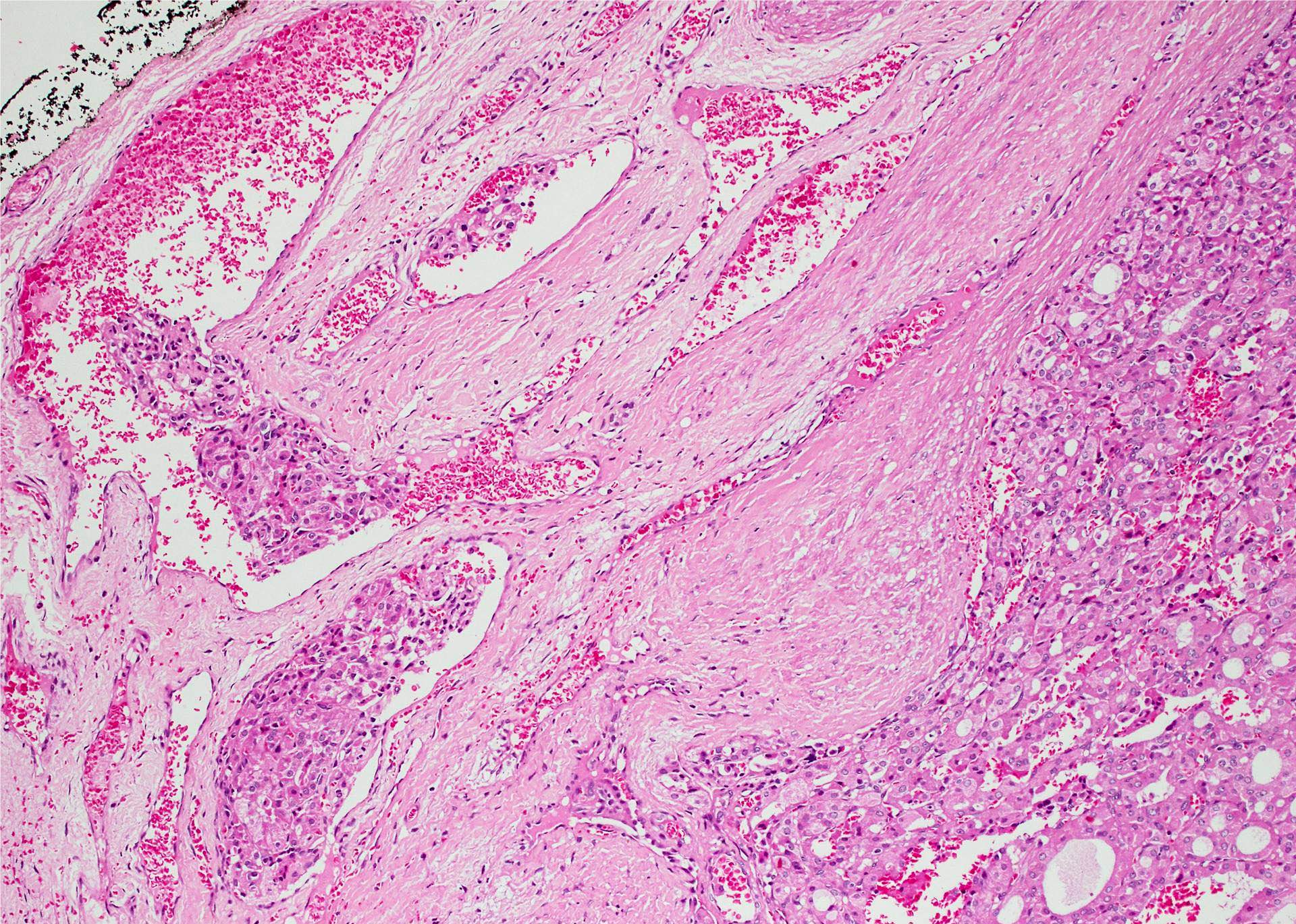
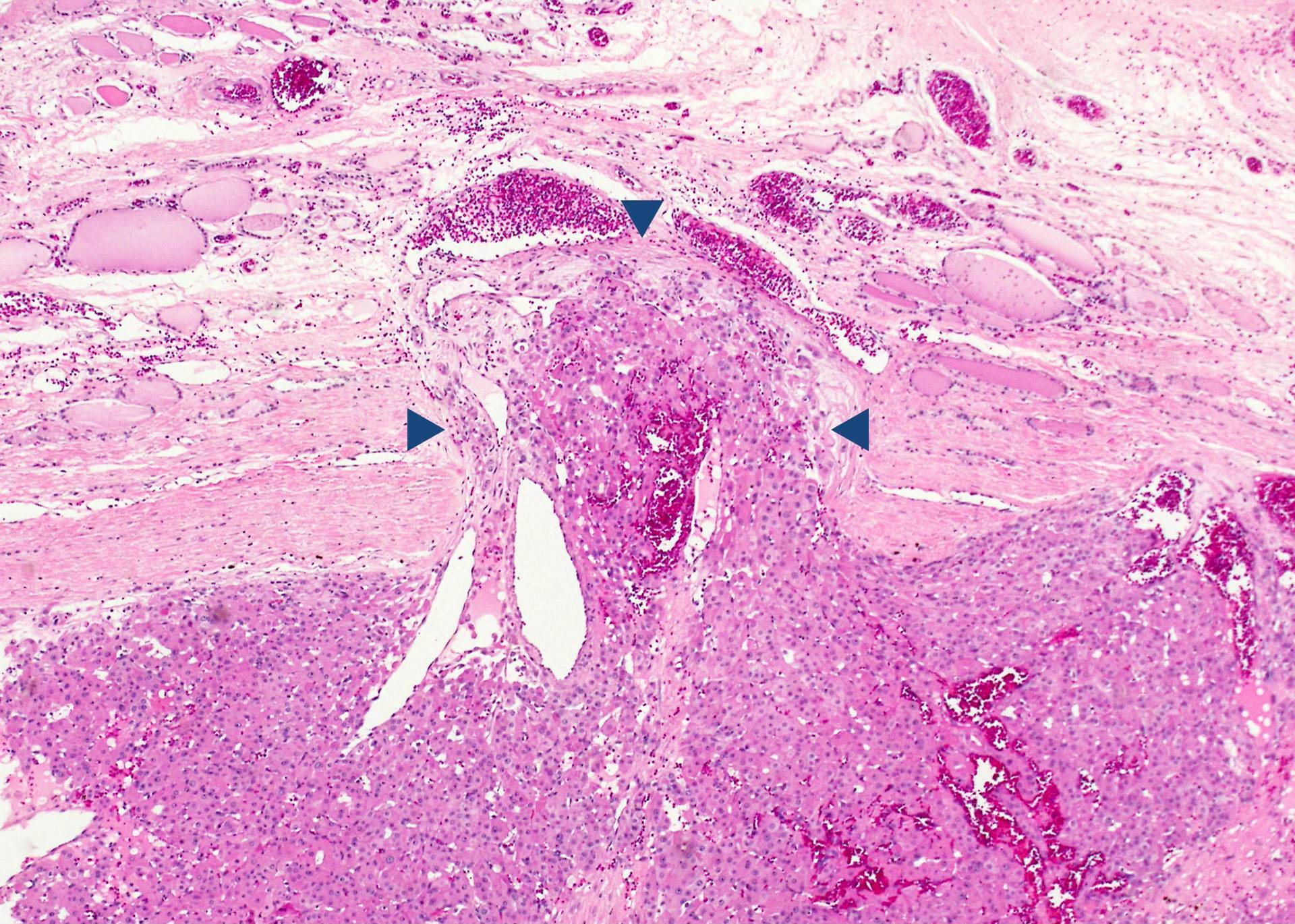
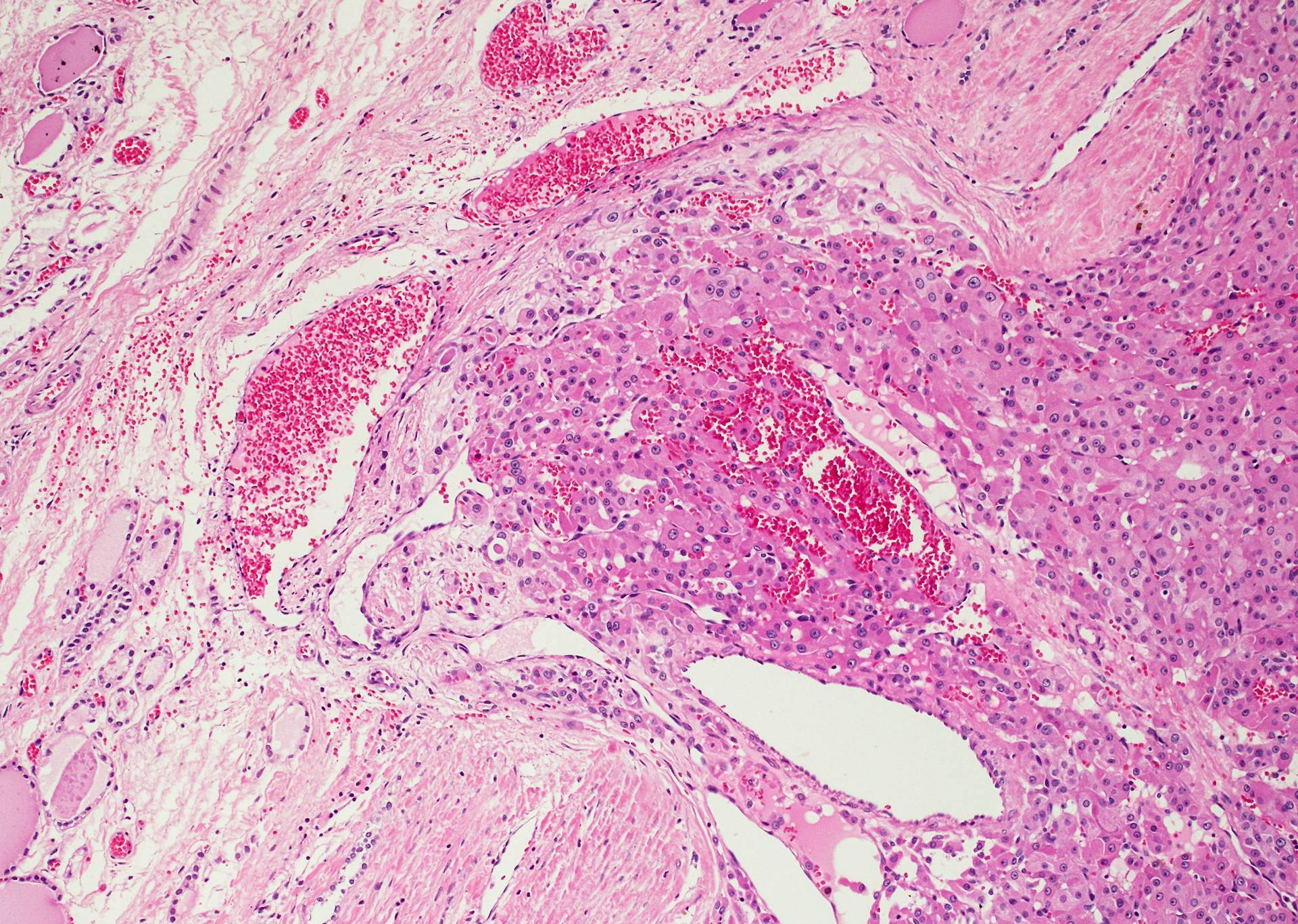
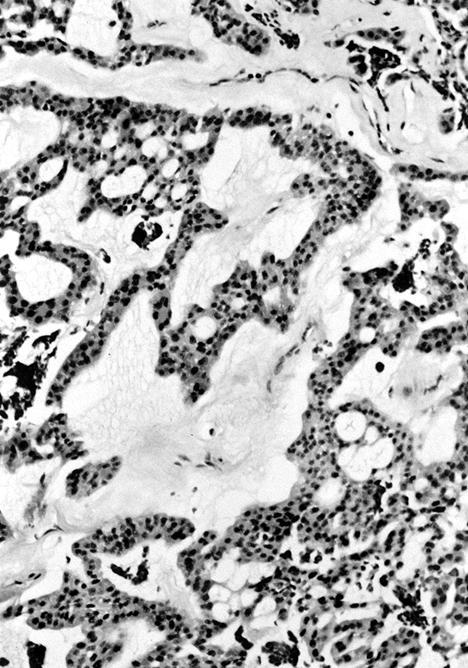
Microscopic (histologic) description
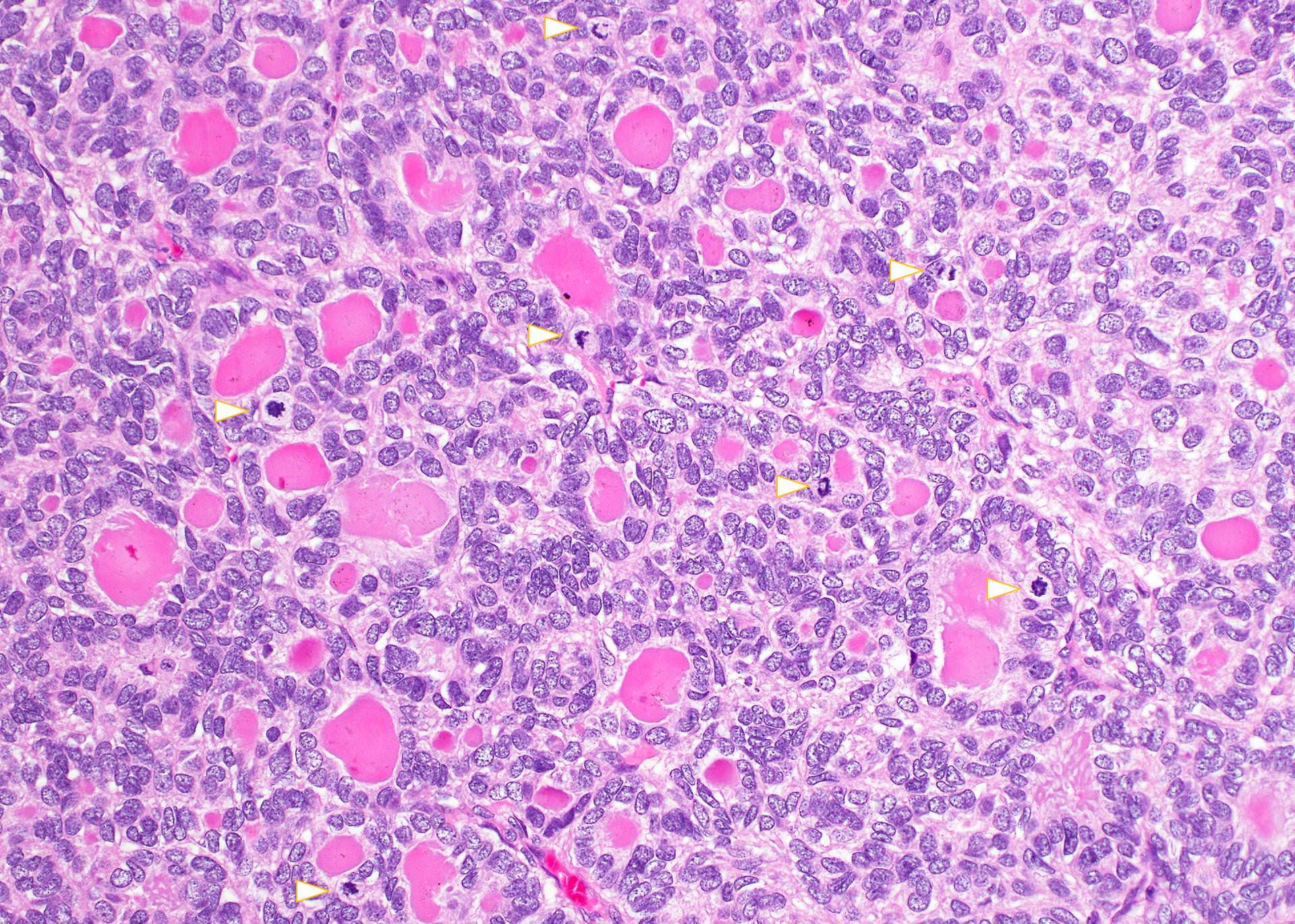
- Trabecular or solid pattern of follicles (small, normal sized or large - microfollicular, normofollicular or macrofollicular respectively)
- No nuclear features of papillary thyroid carcinoma
- Invasion of adjacent thyroid parenchyma, capsule (complete penetration) or blood vessels (in or beyond the capsule)
- Capsular invasion: capsule is typically thickened and irregular, needs penetration through the capsule (full thickness), may have reactive pseudocapsule around the invasion edge, exclude FNA site
- Vascular invasion: vessel within or beyond capsule, tumor covered with endothelium, attached to the wall or with thrombus
- May have nuclear atypia, focal spindled areas, mitotic figures (< 3/10HPF)
- No necrosis
- Usually no squamous metaplasia, no psammoma bodies, no / rare lymphatic invasion
- Metastatic follicular carcinoma can mimic normal thyroid tissue
Microscopic (histologic) images
Contributed by Andrey Bychkov, M.D., Ph.D., Mark R. Wick, M.D. and AFIP
Images hosted on other servers:
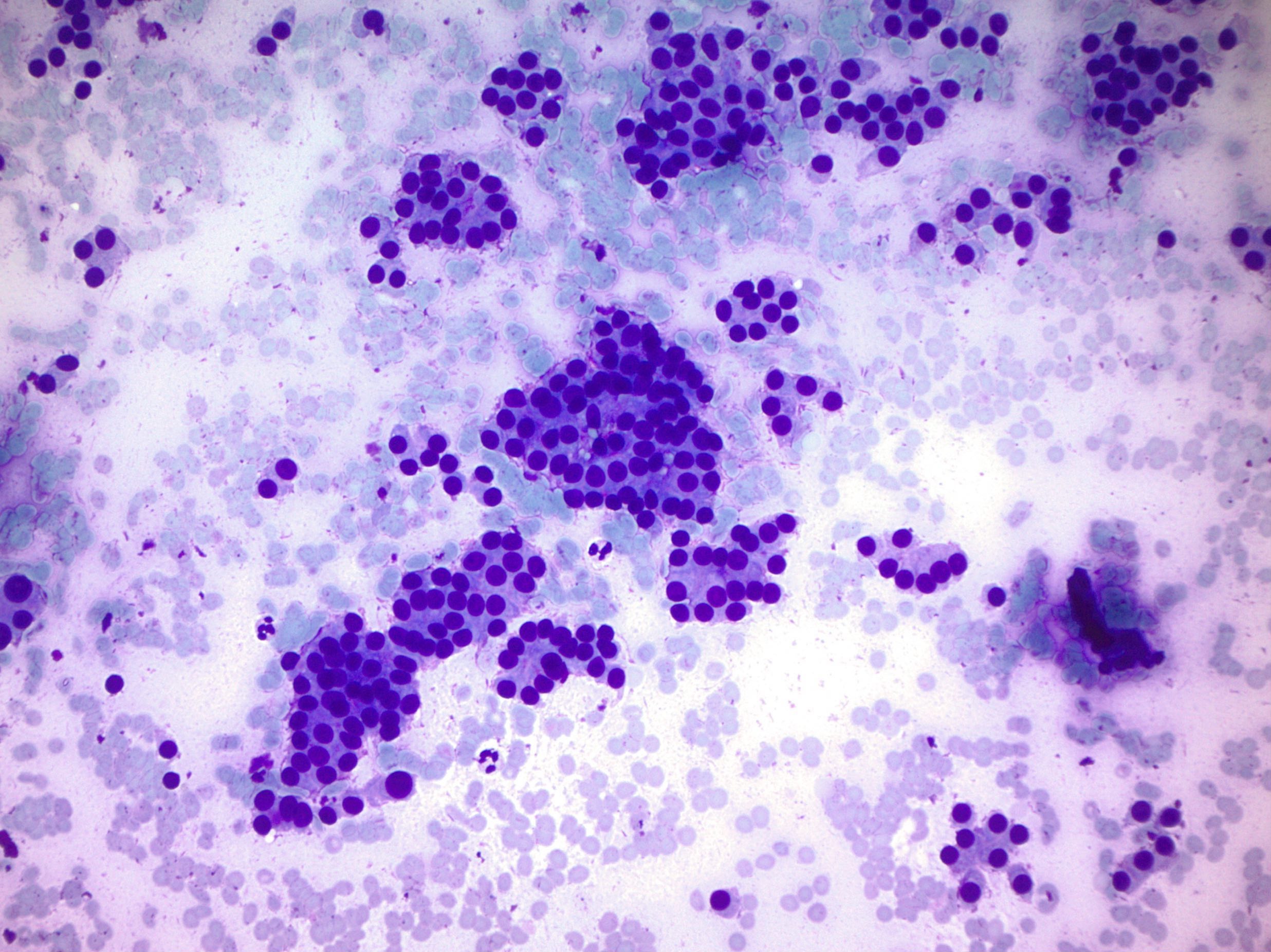
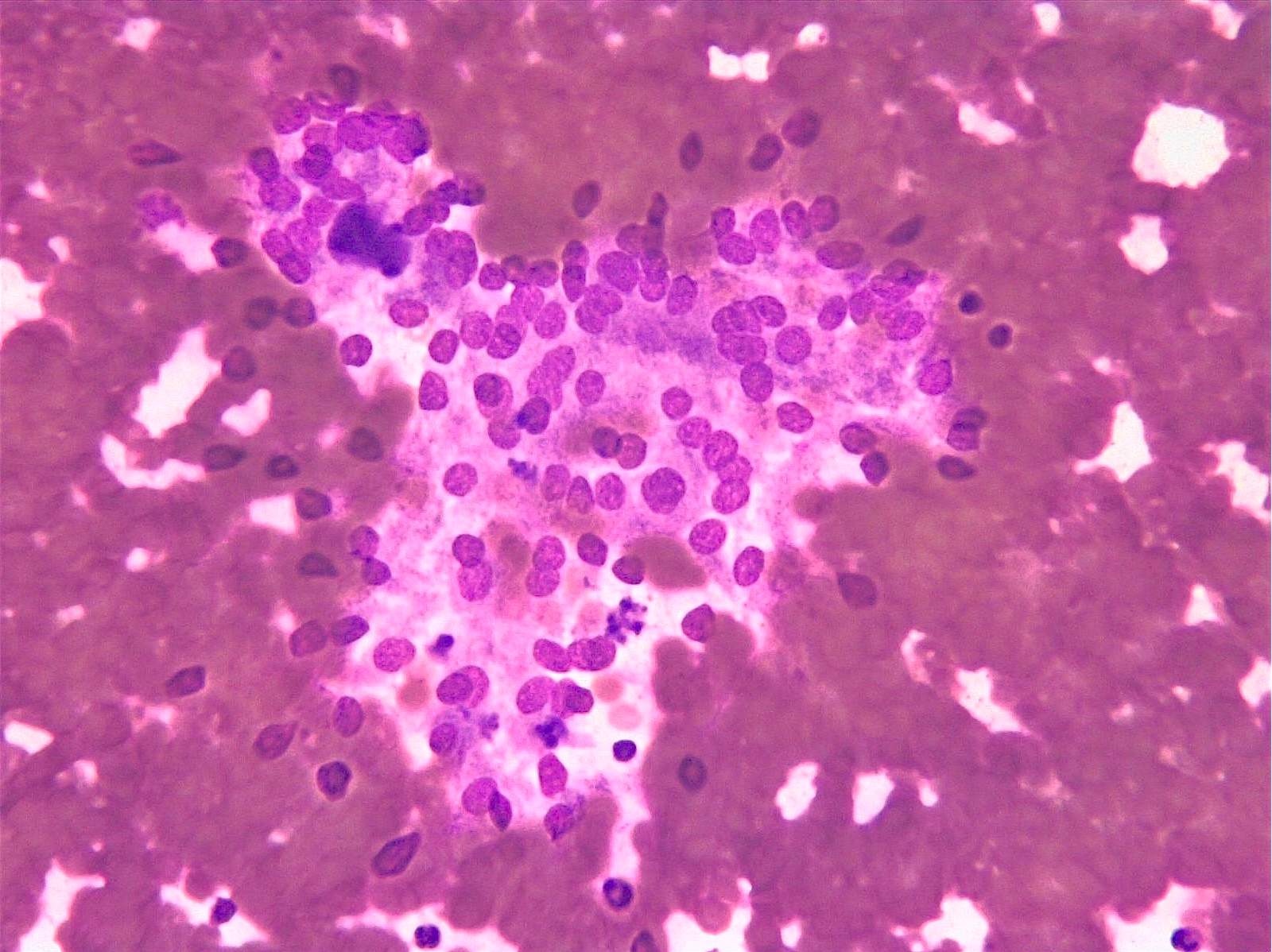
Cytology description
- Microfollicules (6 - 12 nuclei) with nuclear enlargement, overlapping and crowding
- No or scant colloid
- Nuclear atypia is not specific for malignancy
- Cannot distinguish between follicular adenoma and carcinoma by fine needle aspiration since there needs to be evidence of capsular invasion, vascular invasion or invasion of adjacent parenchyma
Cytology images
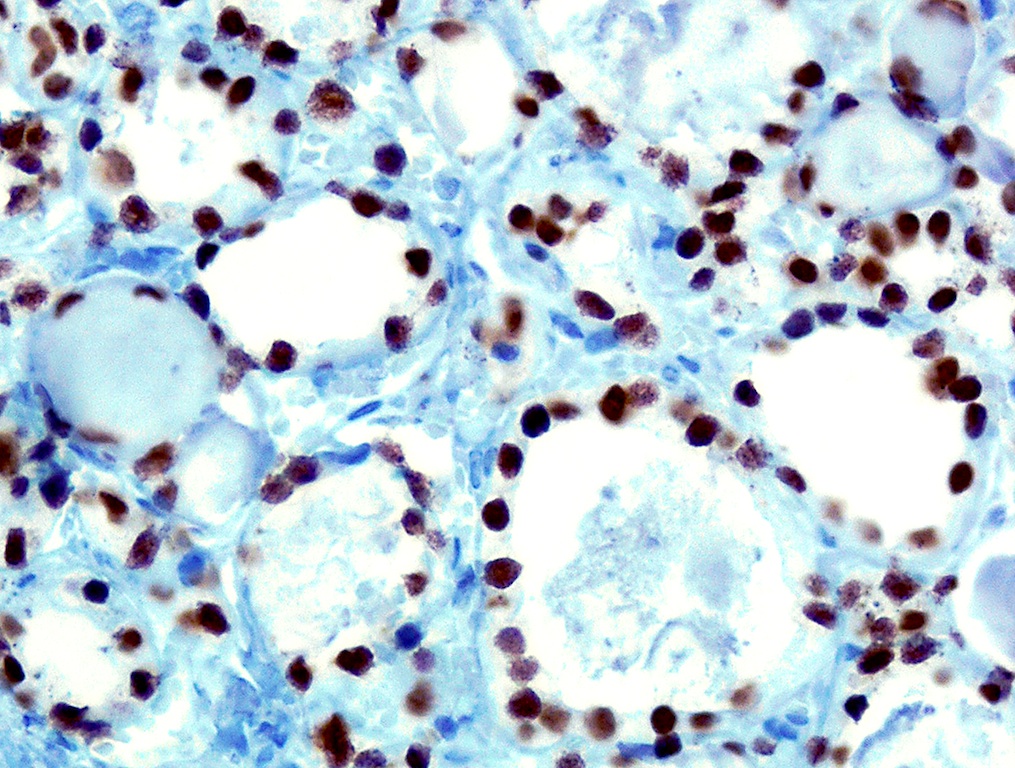
Positive stains
Molecular / cytogenetics description
- Activated PI3K / AKT or RAS of the receptor tyrosine kinase signaling pathway
- NRAS and HRAS mutations in 49%, PAX8 and PPAR gamma rearrangements in 36% (J Clin Endocrinol Metab 2003;88:2318)
- PI3CA and PTEN mutations in 5 - 10%
- Tumors with rearrangement tend to be overtly invasive versus minimally invasive without this rearrangement (Am J Surg Pathol 2002;26:1016)
- Widely invasive carcinomas have higher frequency of allelic loss than minimally invasive carcinomas (Hum Pathol 2003;34:375)
Videos
Thyroid carcinoma: gross and micro
Histopathology thyroid: follicular carcinoma
Differential diagnosis
- Metastatic clear cell renal cell carcinoma vs. clear cell follicular carcinoma: the latter is TTF1+ and thyroglobulin+
- Parathyroid carcinoma: PTH+
- Poorly differentiated thyroid carcinoma: solid, trabecular and insular growth patterns, necrosis, mitotic figure ≥ 3/10 HPF, convoluted nuclei (many previously diagnosed widely invasive follicular carcinoma could be this category)
- Well differentiated thyroid carcinoma, NOS: encapsulated follicular derived neoplasm with tumor capsular or vascular invasion and questionable nuclear features of papillary carcinoma
Additional references
Practice question #1
- Which statement for thyroid follicular carcinoma is false?
- Cannot have necrosis or increased mitotic figures (≥ 3/10 HPF)
- Commonly metastases to bone, lung, not lymph node
- Detecting RAS mutations and PPAX8-PPAR gamma rearrangements can be used to distinguish follicular carcinoma from adenoma
- Nuclear atypia does not indicate malignancy
- Risk factors include iodine deficiency and irradiation exposure
Practice answer #1
C. Detecting RAS mutations and PAX8-PPAR gamma rearrangements can be used to distinguish follicular carcinoma from adenoma. RAS mutations and PAX8-PPAR gamma rearrangements can be found in follicular adenoma.
Comment Here
Reference: Follicular
Comment Here
Reference: Follicular