Table of Contents
Definition / general | Essential features | Clinical features | Diagnosis | Case reports | Treatment | Cytology description | Cytology images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Suzuki A, Bychkov A. Malignant. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidmalignant.html. Accessed April 20th, 2024.
Definition / general
- Bethesda category VI malignant is used when cytologic features strongly suggest malignancy (Thyroid 2017;27:1341)
Essential features
- Used when cytology is strongly suggesting malignancy
- Frequency 5 - 10%, resection rate 65 - 78%, risk of malignancy 99% (when noninvasive follicular thyroid neoplasm with papillary-like nuclear features [NIFTP] is included in malignant) or 94 - 96% (NIFTP is excluded from malignant)
- Most common histological diagnosis is papillary thyroid carcinoma (PTC)
Clinical features
- Meta analysis data (Cancer Cytopathol 2020;128:238)
- Frequency: 7.4% (5.4 - 9.3%)
- Resection rate: 72.1% (65.3 - 77.9%)
- Risk of malignancy: 99% when NIFTP is included in malignant, 94 - 96% when NIFTP is excluded from malignant (Ali: Bethesda System for Reporting Thyroid Cytopathology, 2nd Edition, 2018)
Diagnosis
- Includes the following malignancies: papillary thyroid carcinoma, poorly differentiated thyroid carcinoma, anaplastic thyroid carcinoma, medullary thyroid carcinoma, lymphoma, intrathyroid thymic carcinoma, mucoepidermoid carcinoma, squamous cell carcinoma and metastatic carcinoma to the thyroid
- Follicular thyroid carcinoma does not belong to this category (usually Bethesda category IV)
- A few cases of NIFTP, a nonmalignant thyroid tumor, may reside in this category, owing to nuclear features of papillary thyroid carcinoma (Endocr Pract 2019;25:491)
- If interpreted as malignant, it is implied that the sample is adequate for evaluation irrespective of quantitative criteria of adequacy
- Mention the subtype, if identified
Case reports
- Primary malignancies:
- 41 year old man with primary thyroid diffuse large B cell lymphoma coexistent with papillary thyroid carcinoma (Head Neck 2015;37:E109)
- 42 year old woman with poorly differentiated carcinoma of the thyroid (J Cancer Res Ther 2018;14:1142)
- 61 year old woman with synchronous papillary thyroid carcinoma and breast ductal carcinoma (Medicine (Baltimore) 2017;96:e6114)
- 62 year old woman with primary squamous cell carcinoma of the thyroid (Rom J Morphol Embryol 2016;57:831)
- 66 year old woman with anaplastic thyroid carcinoma with rapid thyrotoxicosis (Endokrynol Pol 2018;69:28)
- 74 year old man with mucinous carcinoma of the thyroid (Ann Endocrinol (Paris) 2017;78:70)
- Metastatic malignancies:
- 53 year old man with metastasis of colon cancer to medullary thyroid carcinoma (J Korean Med Sci 2014;29:1432)
- 55 year old man with thyroid metastasis from small cell lung carcinoma (J Med Case Rep 2015;9:231)
- 62 year old woman with breast cancer metastases to the thyroid gland (J Med Case Rep 2017;11:269)
- 68 year old man with thyroid metastasis from p16+ oropharyngeal squamous cell carcinoma (Endocr J 2018;65:479)
Treatment
- Usual management is total thyroidectomy or lobectomy (Clin Endocrinol (Oxf) 2014;81:1)
- For nodules indicating metastatic tumor rather than a primary thyroid malignancy, surgery may not be indicated
- Papillary thyroid carcinoma:
- Extent of surgery (lobectomy versus total thyroidectomy) depends on the patient's age, overall health status and the size and sonographic characteristics of the tumor
- For low risk cases (≤ 1 cm, without extrathyroidal extension and clinical metastasis), active surveillance is an option (Thyroid 2018;28:23)
- Medullary thyroid carcinoma:
- Serum calcitonin level and genetic testing for germline RET mutations are performed (Endocr J 2017;64:1099, Thyroid 2015;25:567)
- Surgical treatment is usually total thyroidectomy with neck dissection
- Poorly differentiated thyroid carcinoma:
- If no distant metastasis, external beam radiotherapy in addition to surgery is recommended
- Anaplastic thyroid carcinoma:
- Complete surgical resection, with or without preoperative hyperfractionated radiotherapy or chemotherapy (Nat Rev Endocrinol 2017;13:644)
- If potentially incurable, surgery is combined with postoperative radiation or chemotherapy
- Lymphoma:
- Combined modality therapy (2 or more of surgery, radiotherapy and chemotherapy)
Cytology description
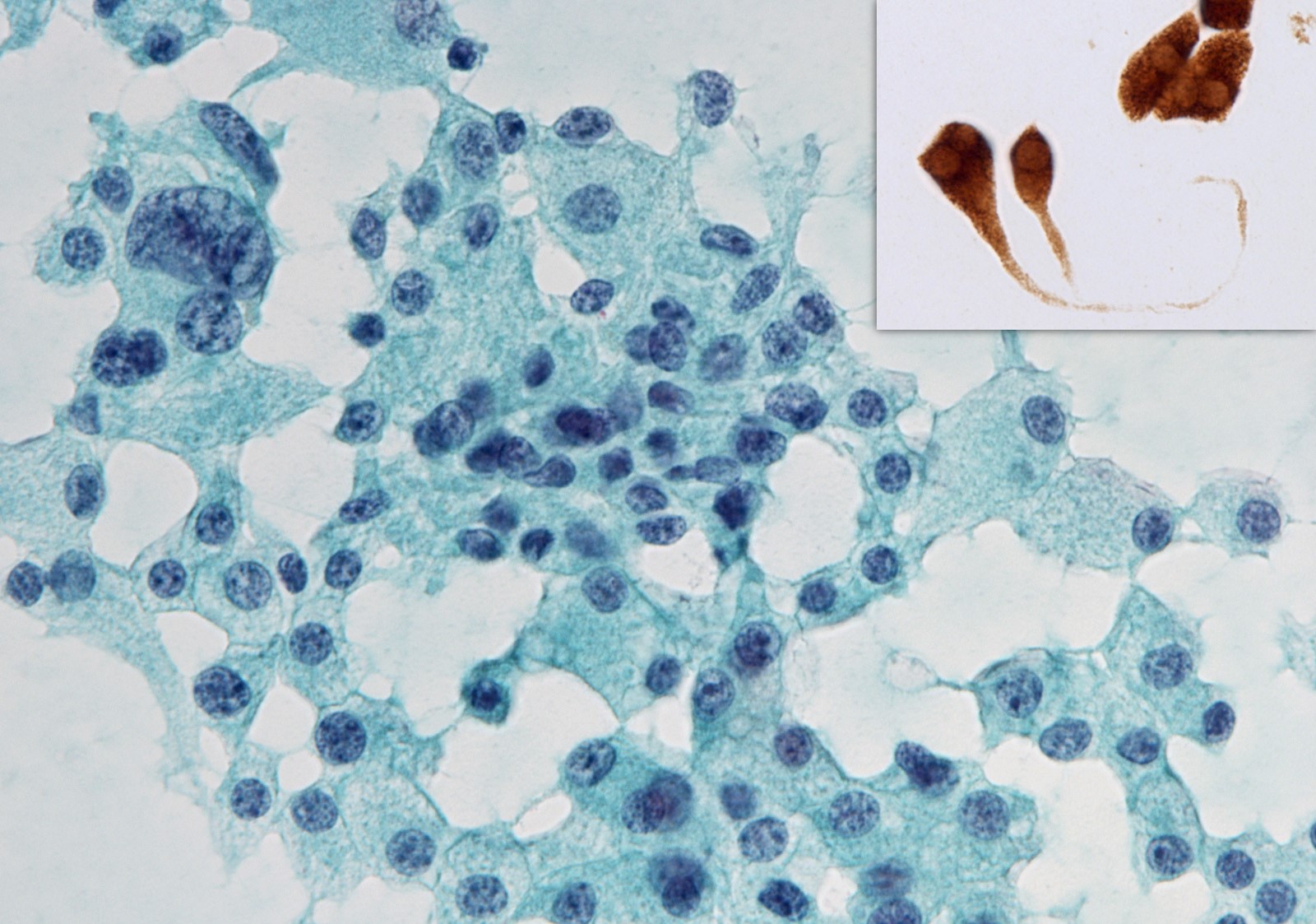
- Papillary thyroid carcinoma (PTC):
- Arrangement: papillae, monolayers, cellular swirls (Acta Cytol 2010;54:939)
- Cytoplasm: hobnail cells, oncocytic metaplasia, squamoid metaplasia, histiocytoid cells
- Nuclei:
- Enlarged, crowded, molded, oval or irregularly shaped
- Longitudinal grooves, pseudoinclusions
- Pale nuclei with powdery chromatin, thick nuclear membranes, marginally placed micronucleoli
- Background: psammoma bodies, multinucleated giant cells, ropy colloid
- Liquid based cytology specimens: convoluted nuclei, eosinophilic nucleoli, perinucleolar halo, intercellular spaces (Diagn Cytopathol 2015;43:108)
- PTC variants:
- Follicular variant and NIFTP: small to medium sized follicles lined by cells with variable nuclear features of PTC, absence of papillary fragments, multinucleated giant cells, pseudoinclusions, psammoma bodies and marked cystic change
- Cystic variant: sheets, papillae, follicles, ball-like clusters, septate intracytoplasmic vacuoles, histiocytoid cells, macrophages
- Oncocytic variant: oncocytic cells arranged in papillae, sheets, microfollicles, diagnostic nuclear changes of PTC
- Warthin-like variant: oncocytic cells arranged in papillae, lymphoplasmacytic background, nuclear changes of PTC
- Tall cell variant: polygonal with centrally located nuclei but can be elongated and cylindrical with an eccentrically placed nucleus (tail-like cells or tadpole cells), granular cytoplasm with prominent cytoplasmic borders, nuclear changes of PTC
- Columnar cell variant: lacking colloid, arranged as papillae, clusters and flat sheets, small tubular structures, elongated and pseudostratified nuclei, hyperchromatic, nuclear features of PTC are much less prominent
- Solid variant: lack colloid, appear as cohesive, syncytial type 3 dimensional tissue fragments, microfollicles / trabeculae, discohesive, single cells, typical nuclear features of PTC, scant true papillae
- Diffuse sclerosing variant: scant or absent colloid, arranged in 3 dimensional ball-like clusters and cohesive clusters intermingled with inflammatory cells
- Cribriform morular variant: absent colloid, tall, columnar cells having papillary arrangement, round to oval slit-like empty spaces formed by spindle to ovoid cells within cell clusters (cribriform pattern), cell clusters with eddy formation (morules), pale staining nuclei with thickened nuclear membranes (peculiar nuclear clearing), nuclear grooves, pseudoinclusions, hyaline material within cell clusters, absence of psammoma bodies and multinucleated giant cells, positive for β catenin (nuclear and cytoplasmic), estrogen receptor, progesterone receptor
- Hobnail variant: loss of polarity and cohesiveness, single cells with eccentric nuclei and tapering cytoplasm (comet-like or teardrop-like cells), apically or eccentrically placed nucleus (hobnail features) in papillary or micropapillary clusters, multiple soap bubble-like pseudoinclusions, typical nuclear features of PTC
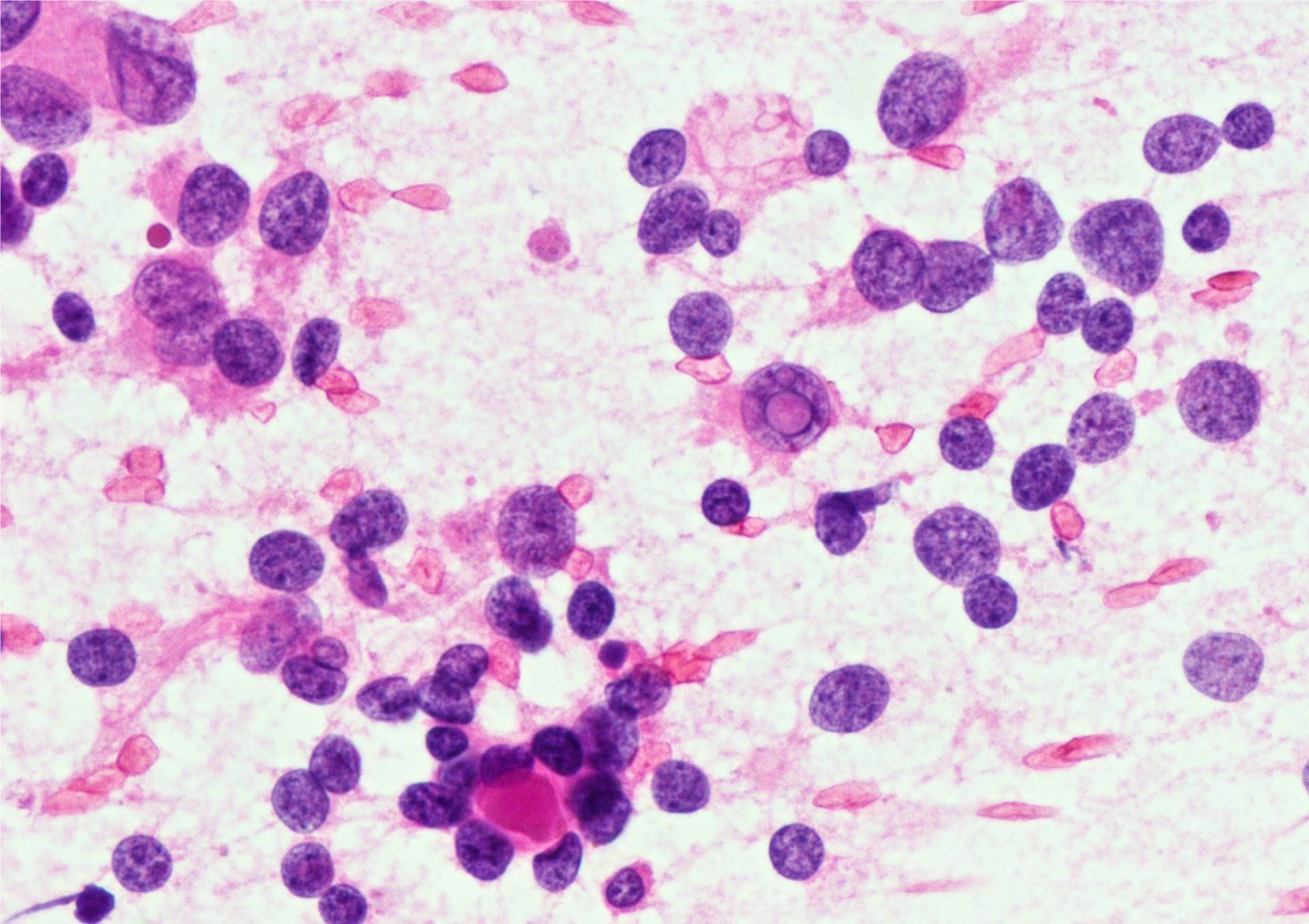
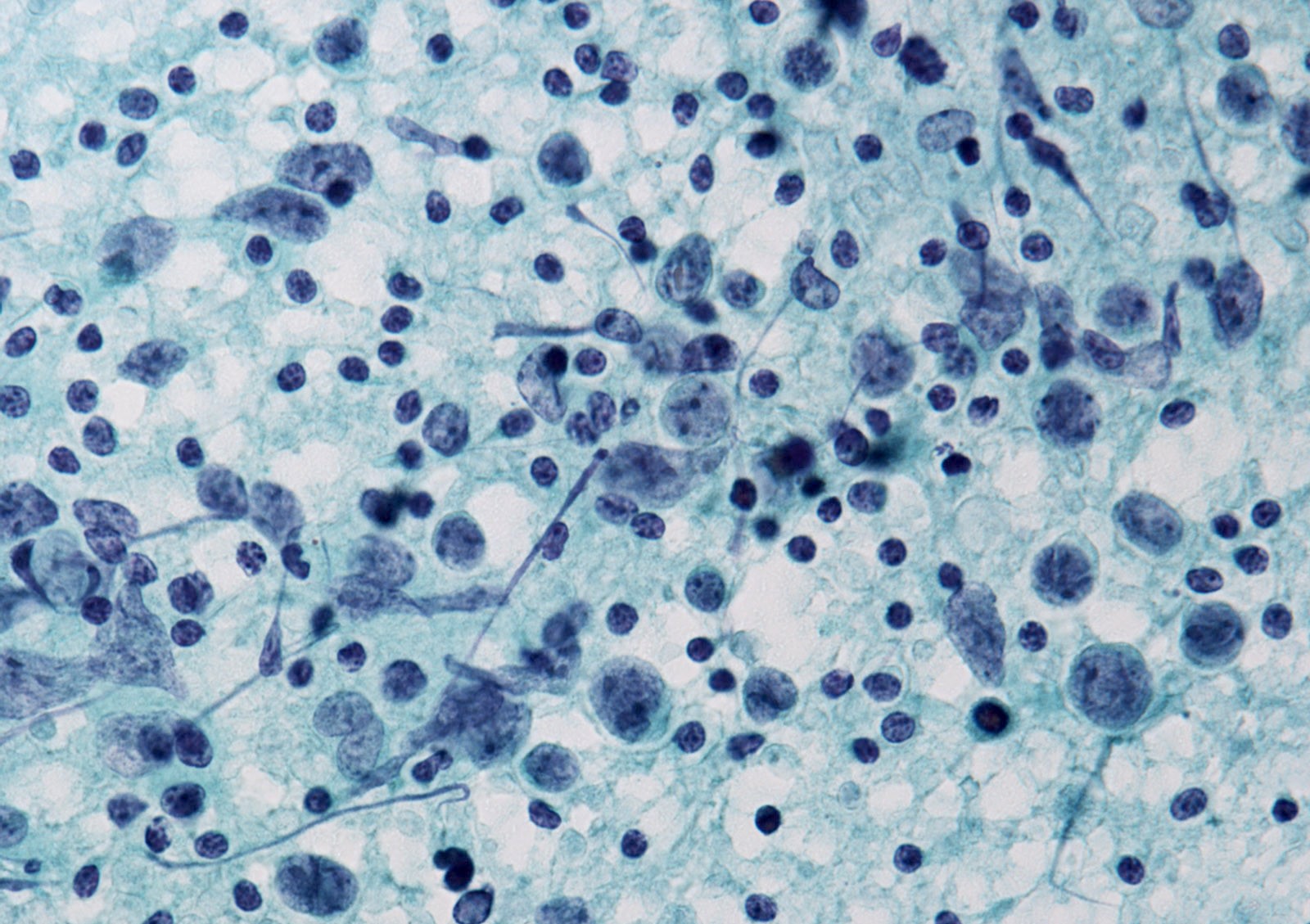
- Medullary thyroid carcinoma:
- Arrangement: numerous isolated cells, weakly cohesive clusters
- Cell shape: plasmacytoid, polygonal, round or spindle shaped, long cell processes, bizarre giant cells
- Cytoplasm: granular, small red-purple granules (Romanowsky stains)
- Nuclei: round, oval, elongated, eccentrically placed, finely or coarsely granular (salt and pepper) chromatin, binucleation or multinucleation
- Background: amyloid
- Immunostaining:
- Positive: calcitonin, CEA, neuroendocrine markers (chromogranin, synaptophysin) and TTF1
- Negative: PAX8 and thyroglobulin
- Measurement of calcitonin levels in needle washout fluid can be helpful (Endocr J 2017;64:1099)
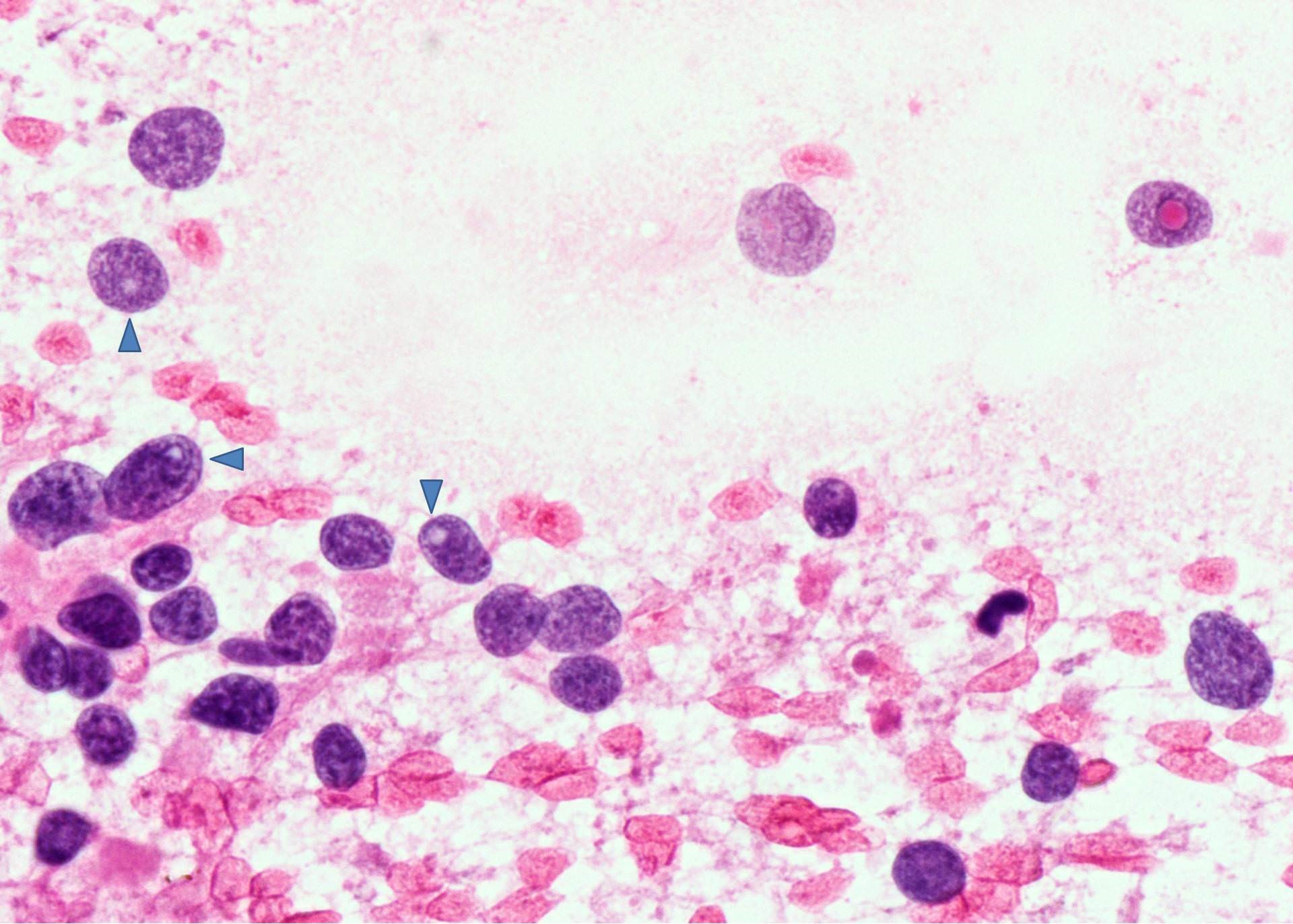
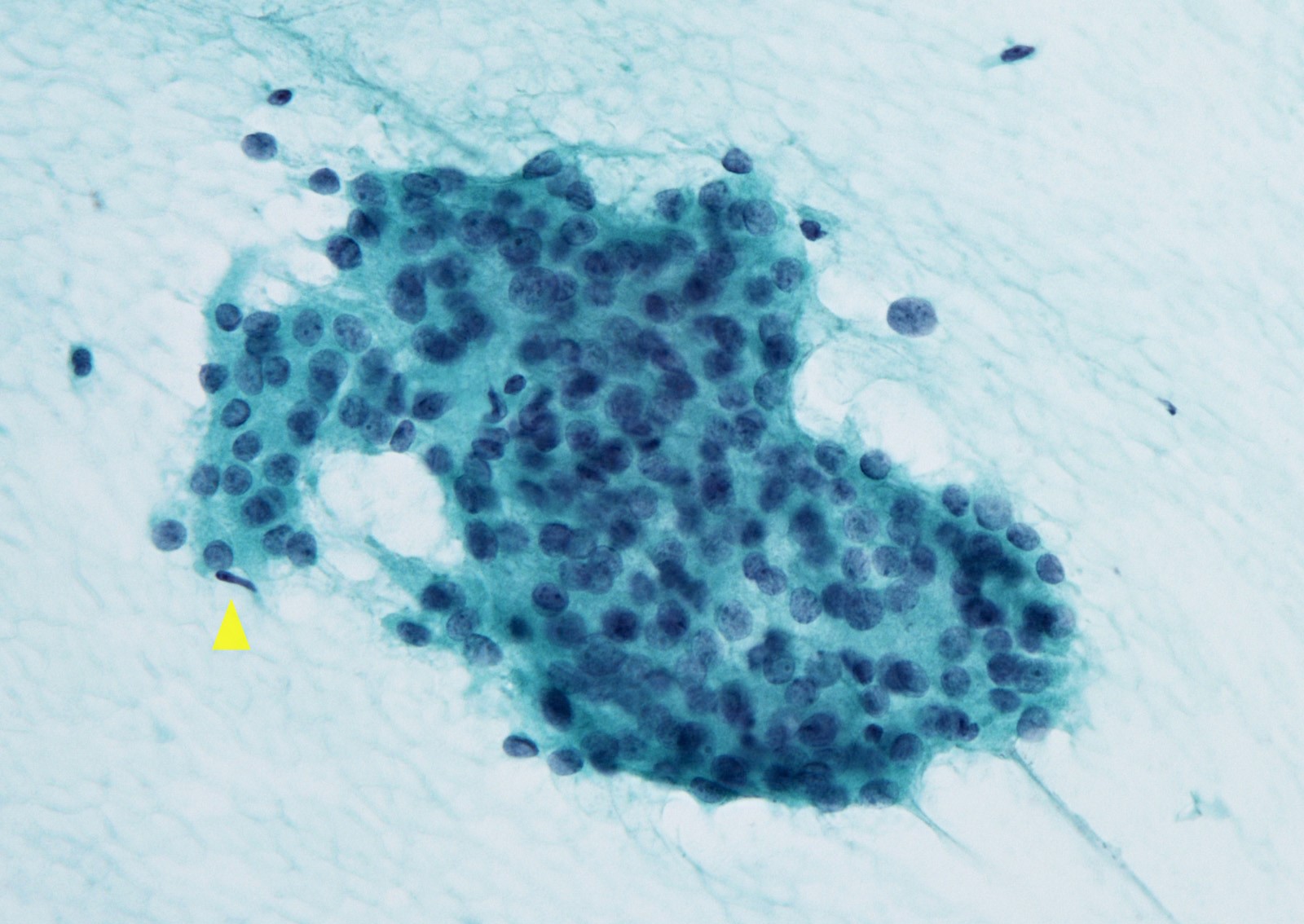
- Poorly differentiated thyroid carcinoma (Cancer Cytopathol 2015;123:82):
- Arrangement: insular, solid or trabecular pattern
- Nuclei: high nuclear/cytoplasmic (N/C) ratio with variable nuclear atypia
- Background: scant colloid, apoptosis and mitotic activity, necrosis
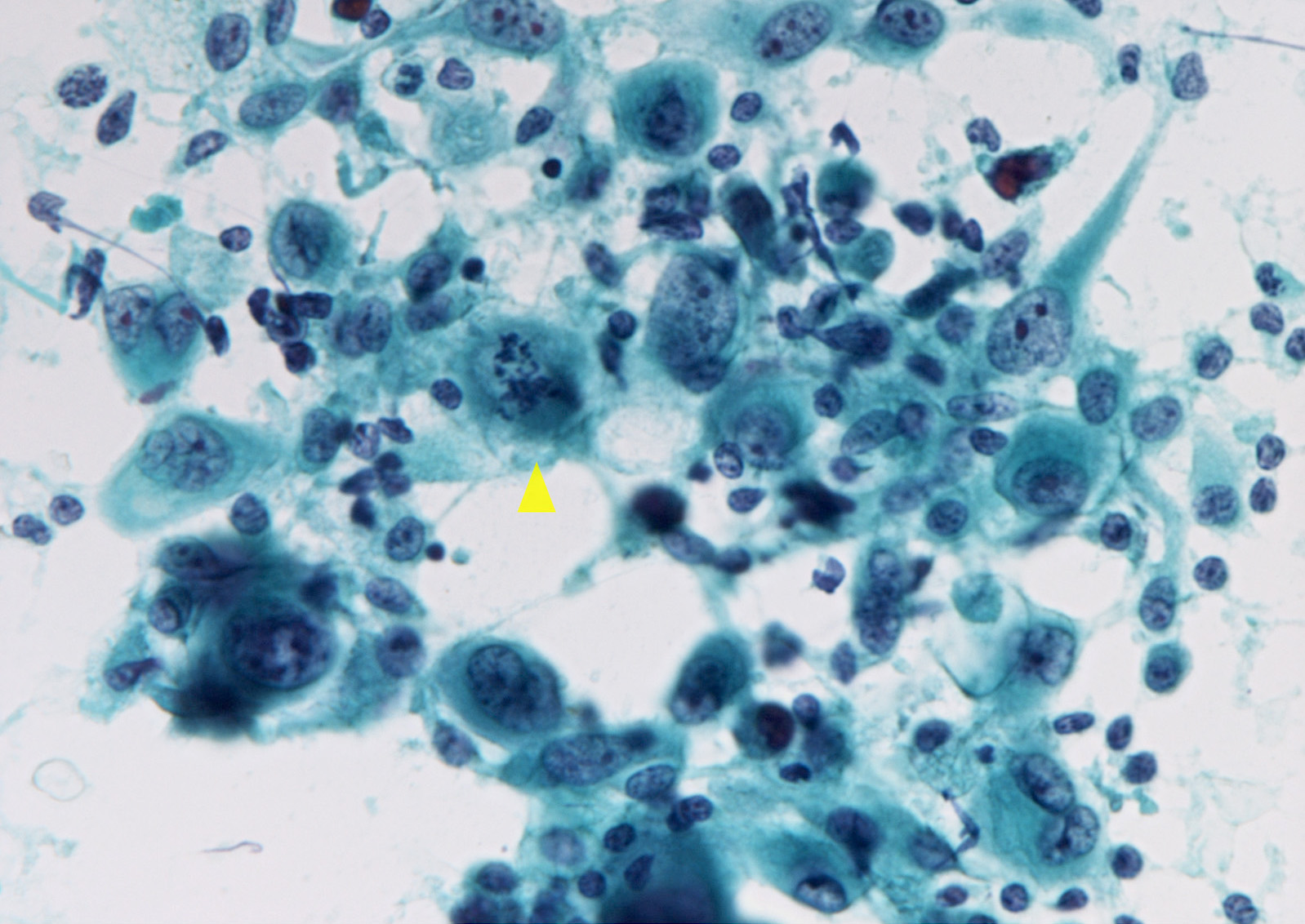
- Anaplastic thyroid carcinoma:
- Arrangement: isolated cells or in variably sized groups
- Cell shape: epithelioid, spindle shaped, range in size, could be plasmacytoid, rhabdoid
- Nuclei: enlargement, irregularity, extreme pleomorphism, mitotic figures, multinucleation
- Background: necrosis, extensive inflammation, sometimes osteoclast-like giant cells
- Immunostaining:
- Positive: pankeratins, PAX8, vimentin (focal)
- Negative: TTF1, thyroglobulin (Hum Pathol 2018;82:140)
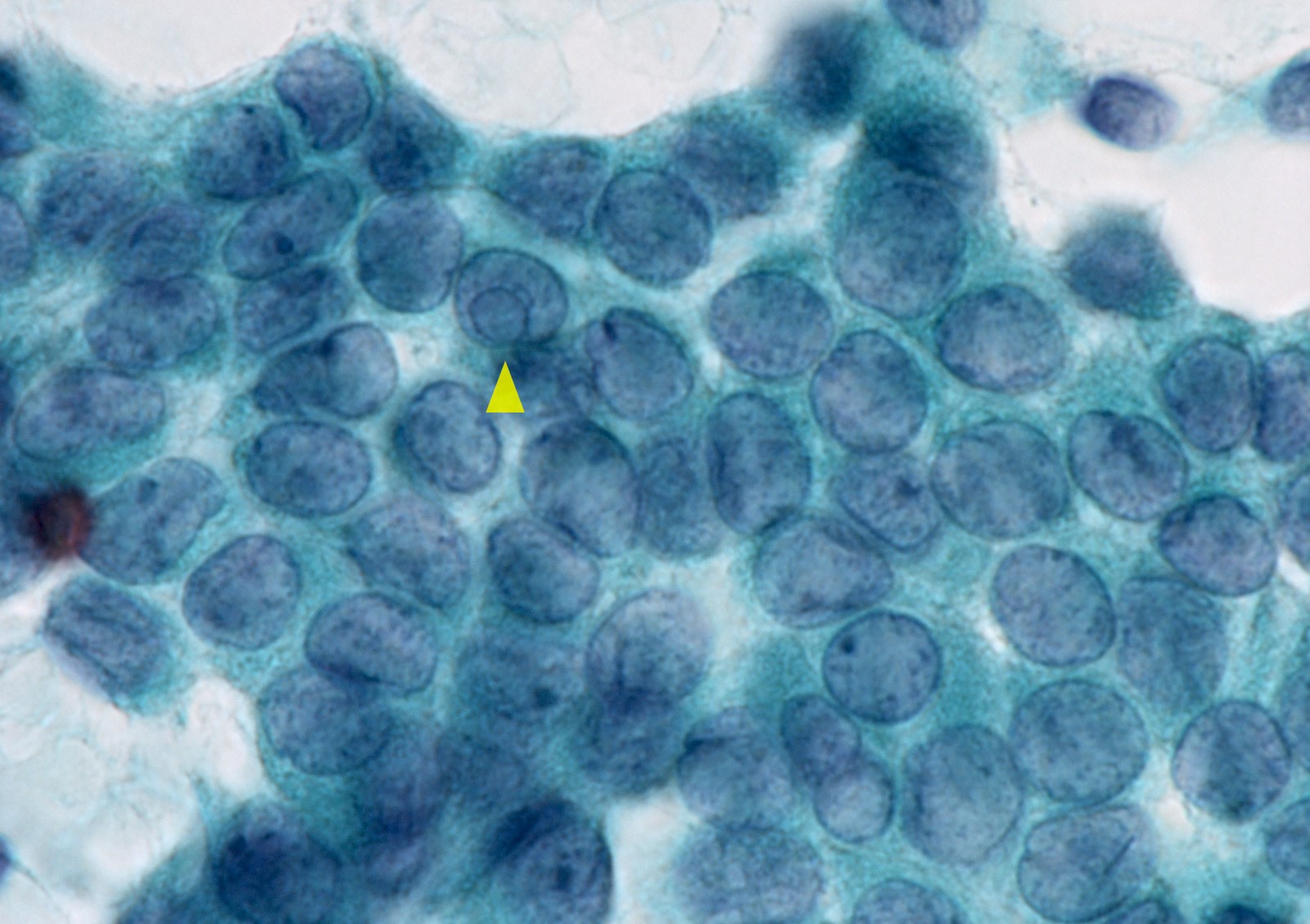
- Lymphoma:
- Arrangement: discohesive round to slightly oval cells
- Cell shape: twice the size of a small mature lymphocyte (marginal zone lymphoma), moderate to abundant basophilic cytoplasm (diffuse large B cell lymphoma)
- Nuclei:
- Vesicular chromatin, small nucleoli (marginal zone lymphoma)
- Coarse chromatin with 1 or more prominent nucleoli (diffuse large B cell lymphoma)
- Reed-Sternberg cells, plasma cells, eosinophils, histiocytes, fibroblasts and capillaries (Hodgkin lymphoma)
- Liquid based cytology specimens: large nuclei, elongated nuclei, degenerative nuclei (specific) (Acta Cytol 2018;62:93)
- Squamous cell carcinoma:
- Composed exclusively of large, pleomorphic keratinized cells
- Metastatic renal cell carcinoma:
- Arrangement: dispersed individually and in small clusters, fragmented papillae, sheets
- Cytoplasm: abundant pale, finely granular, clear, vacuolated
- Nuclei: round to oval, large nucleoli
- Background: bloody
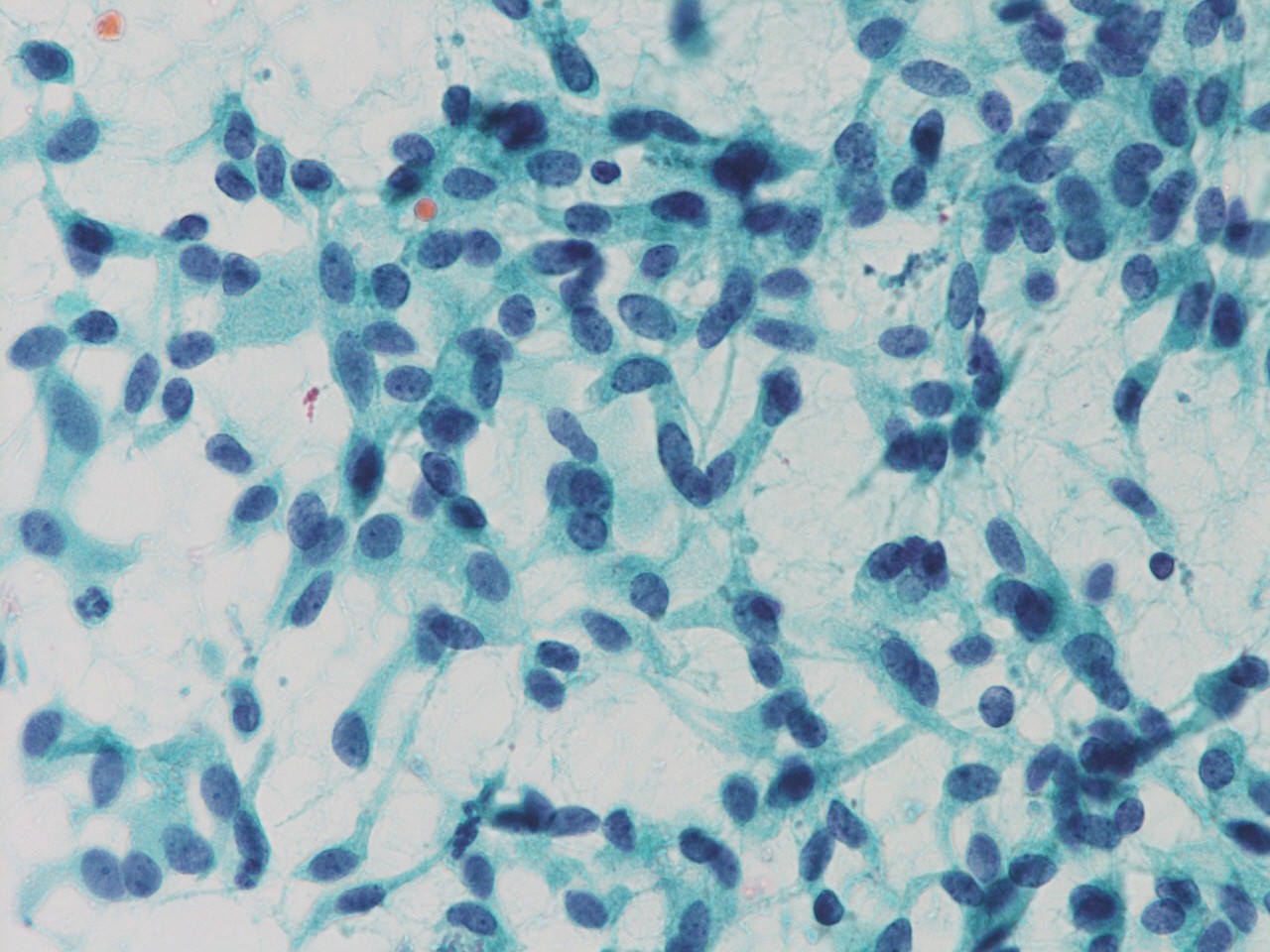
Cytology images
Videos
Thyroid cytopathology
Sample pathology report
- Dx / category: malignant
- Papillary thyroid carcinoma, favor tall cell variant
- Dx / category: malignant
- Medullary thyroid carcinoma
- The malignant cells are positive for calcitonin.
- Dx / category: malignant
- Poorly differentiated thyroid carcinoma
- Highly cellular aspirate with atypical follicular cells, necrosis and scant colloid, most consistent with poorly differentiated thyroid carcinoma.
Differential diagnosis
- Nodular goiter:
- Monolayered sheet-like cluster may mimic papillary thyroid carcinoma (PTC); however, no PTC nuclear features are seen
- Hyalinizing trabecular tumor:
- Nuclear grooves and abundant nuclear pseudoinclusions resemble PTC; however, hyaline material inside the clusters and yellow bodies are specific for this low risk neoplasm
- Chronic thyroiditis:
- Nuclear changes of follicular cells with focal enlargement, grooves, prominent nucleoli and chromatin clearing mimic PTC; however, no PTC nuclear features are seen
- Benign cyst:
- Histiocytes with septate intracytoplasmic vacuoles so-called histiocytoid cells may mimic PTC; however, no PTC nuclear features are seen (Diagn Cytopathol 2003;29:243)
- Hürthle cell (oncocytic) neoplasms:
- Discohesive cells with abundant granular cytoplasm resembles medullary thyroid carcinoma; however, no salt and pepper chromatin and amyloid background are seen
- Parathyroid adenoma:
- Insular pattern with scant colloid mimics poorly differentiated thyroid carcinoma; however, no irregularity of nuclear membrane is seen
Board review style question #1
Board review style answer #1
C. Medullary thyroid carcinoma. Numerous isolated spindle cells indicate medullary thyroid carcinoma.
Comment Here
Reference: Malignant
Comment Here
Reference: Malignant
Board review style question #2
- Which thyroid malignancy is included in the malignant category of the Bethesda system for reporting thyroid cytopathology?
- Chronic thyroiditis
- Follicular carcinoma
- Hyalinizing trabecular tumor
- Nodular goiter
- Poorly differentiated thyroid carcinoma
Board review style answer #2
E. Poorly differentiated thyroid carcinoma. Nodular goiter and chronic thyroiditis belong to the benign category, the follicular carcinoma belongs to follicular neoplasm / suspicious for a follicular neoplasm category and hyalinizing trabecular tumor belongs to the suspicious for malignancy category.
Comment Here
Reference: Malignant
Comment Here
Reference: Malignant