Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Agarwal S. Fibromatosis / fasciitis-like. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidnodularfasciitis.html. Accessed April 20th, 2024.
Definition / general
- Rare histological variant of papillary thyroid carcinoma (PTC)
- Characterized by an abundant stroma resembling nodular fasciitis / fibromatosis / other myofibroblastic proliferative processes
- First described by Ostrowski as PTC with fibromatosis-like stroma and by Chan et al. as PTC with nodular fasciitis-like stroma (Am J Clin Pathol 1991;95:309)
Essential features
- Prominent myofibroblastic proliferation histomorphologically similar to fibromatosis or nodular fasciitis of soft tissue
- Varying proportion of PTC component
- CTNNB1 (beta catenin) mutation frequent in mesenchymal component
Terminology
- PTC with fibromatosis / fasciitis-like stroma
- PTC with desmoid type fibromatosis (Mod Pathol 2017;30:236)
ICD coding
Epidemiology
- Exceedingly rare, with less than 50 well documented cases reported (Mod Pathol 2017;30:236)
- Estimated 0.04 - 0.5% of all PTC cases (Mod Pathol 2017;30:236, Am J Clin Pathol 1991;95:309)
- 20 - 82 years (mean: 44.5 years); F:M = 3:1 (J Laryngol Otol 2006;120:338)
Sites
- Either lobe or isthmus of thyroid gland
Pathophysiology
- Stromal proliferation mechanism:
- Activated Wnt / APC / beta catenin signaling pathway (Mod Pathol 2017;30:236)
- Downstream signaling induced by BRAF mutation (Virchows Arch 2019;475:519)
- Reactive, remains to be proved (Am J Clin Pathol 1991;95:309, Histopathology 1992;21:577)
Clinical features
- Asymptomatic / palpable firm neck mass (Endocr J 2017;64:1017)
- May manifest with cervical nodal metastasis or obstructive symptoms
Diagnosis
- Diagnostic workup is similar to any thyroid mass / nodule
- Ultrasound with fine needle aspiration cytology (FNAC)
- CT scan may be useful to evaluate extrathyroidal extension and lymph node metastases
- Final diagnosis is rendered on histopathological examination of resected tumor
- Accurate diagnosis of PTC with fibromatosis / fasciitis-like stroma is usually not possible on FNAC; however, preoperative recognition of this variant among other PTC variants does not influence treatment decisions (Endocr J 2017;64:1017)
Radiology description
- Sonography:
- Similar to classical PTC (Ultrasound Int Open 2018;4:E39)
- Classified as intermediate or high suspicion nodule
- Irregular shape
- Heterogeneous echogenicity
- Taller than wide sign (85%)
- Usually lacks microcalcification (76.9%), macrocalcification (> 2 mm) in 31%
- Mesenchymal component: heterogeneous (62.5%), more hypoechoic (71.4%) than PTC areas; lacks microcalcification
- Doppler ultrasound:
- No or mild flow signal (75.0%)
- Ultrasound elastography:
- Mesenchymal component: not stiff; more elastic than PTC areas
Radiology images
Prognostic factors
- Prognosis similar to classic PTC of similar size and stage (J Laryngol Otol 2006;120:338)
- Risk stratification as per American Thyroid Association 2015 (Thyroid 2016;26:1)
Case reports
- 20 year old man with desmoid type fibromatosis postthyroidectomy (Int J Surg Case Rep 2019;63:5)
- 38 year old woman with left side neck swelling (Indian J Pathol Microbiol 2017;60:390)
- 44 year old woman with neck swelling (Int J Surg Pathol 2015;23:305)
- 48 year old woman with desmoid type fibromatosis postthyroidectomy (Int J Clin Exp Pathol 2018;11:2879)
- 58 year old patient with SOX11 expression in a case of PTC with fibromatosis / fasciitis-like stroma containing BRAF c.1799_1801delTGA and CTNNB1 c.133T>C mutations (Virchows Arch 2019;475:519)
Treatment
- Based on American Thyroid Association and NCCN guidelines, usually surgical excision (Thyroid 2016;26:1, J Natl Compr Canc Netw 2018;16:1429)
- Response of radioactive iodine on the mesenchymal component not proven (Mod Pathol 2017;30:236)
Gross description
- Size: 1.6 - 9 cm (J Laryngol Otol 2006;120:338, Ultrasound Int Open 2018;4:E39)
- Usually well circumscribed but not encapsulated, firm, homogeneous, whitish nodule (Endocr J 2017;64:1017)
- Mesenchymal area: translucent, rubbery elastic, tan in color (Endocr J 2017;64:1017)
Frozen section description
- May not be diagnostic if demonstrates only mesenchymal component (Indian J Pathol Microbiol 2017;60:390)
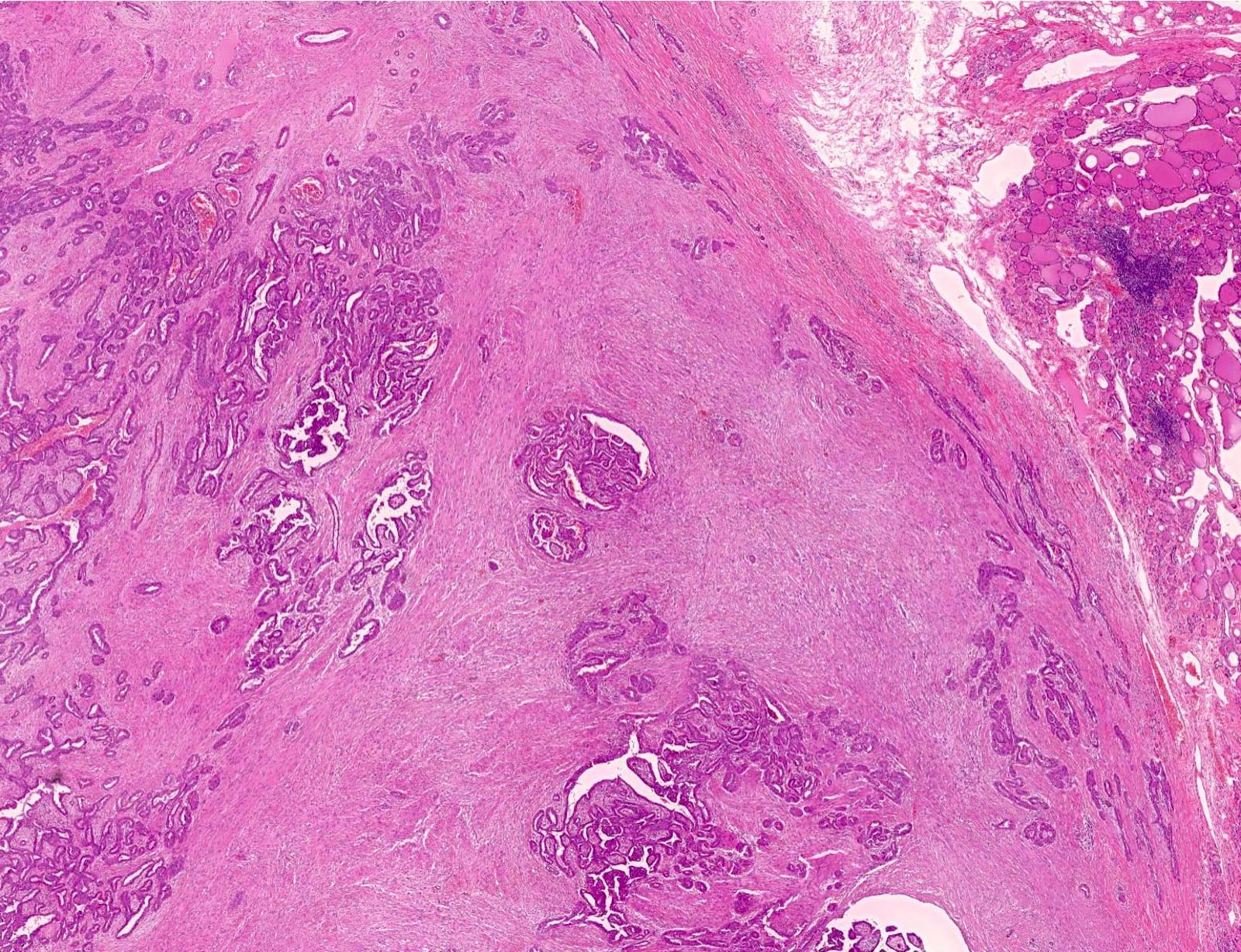
Microscopic (histologic) description
- Mixed epithelial-mesenchymal tumor
- Epithelial component:
- PTC (usually classical PTC; follicular variant of PTC also documented) (Mod Pathol 2020;33:1702)
- Mesenchymal component:
- 20 - 95% of tumor area (Endocr J 2017;64:1017, Ultrasound Int Open 2018;4:E39)
- Myofibroblastic proliferation similar to fibromatosis / nodular fasciitis / other myofibroblastic proliferative processes
- Fibromatosis type stroma: dense hypocellular collagenous connective tissue
- Nodular fasciitis-like stroma: edematous, extravasated red blood cells, inflammatory cells; reminiscent of granulation tissue
- May infiltrate surrounding neck structures
- May metastasize to lymph nodes along with the epithelial cell component (Endocr J 2017;64:1017)
Microscopic (histologic) images
Cytology description
- Usually Bethesda V (suspicious for PTC) or VI (diagnostic of PTC) (Endocr J 2017;64:1017)
- Aspirate may show stromal fragments containing spindle cells in a myxoid background
- May be misdiagnosed as nonneoplastic or benign / malignant spindle cell neoplasm or anaplastic thyroid carcinoma
- Aspirate may be biphasic
- Admixed epithelial and stromal fragments
- May be hypocellular / unsatisfactory (Mod Pathol 2020;33:1702)
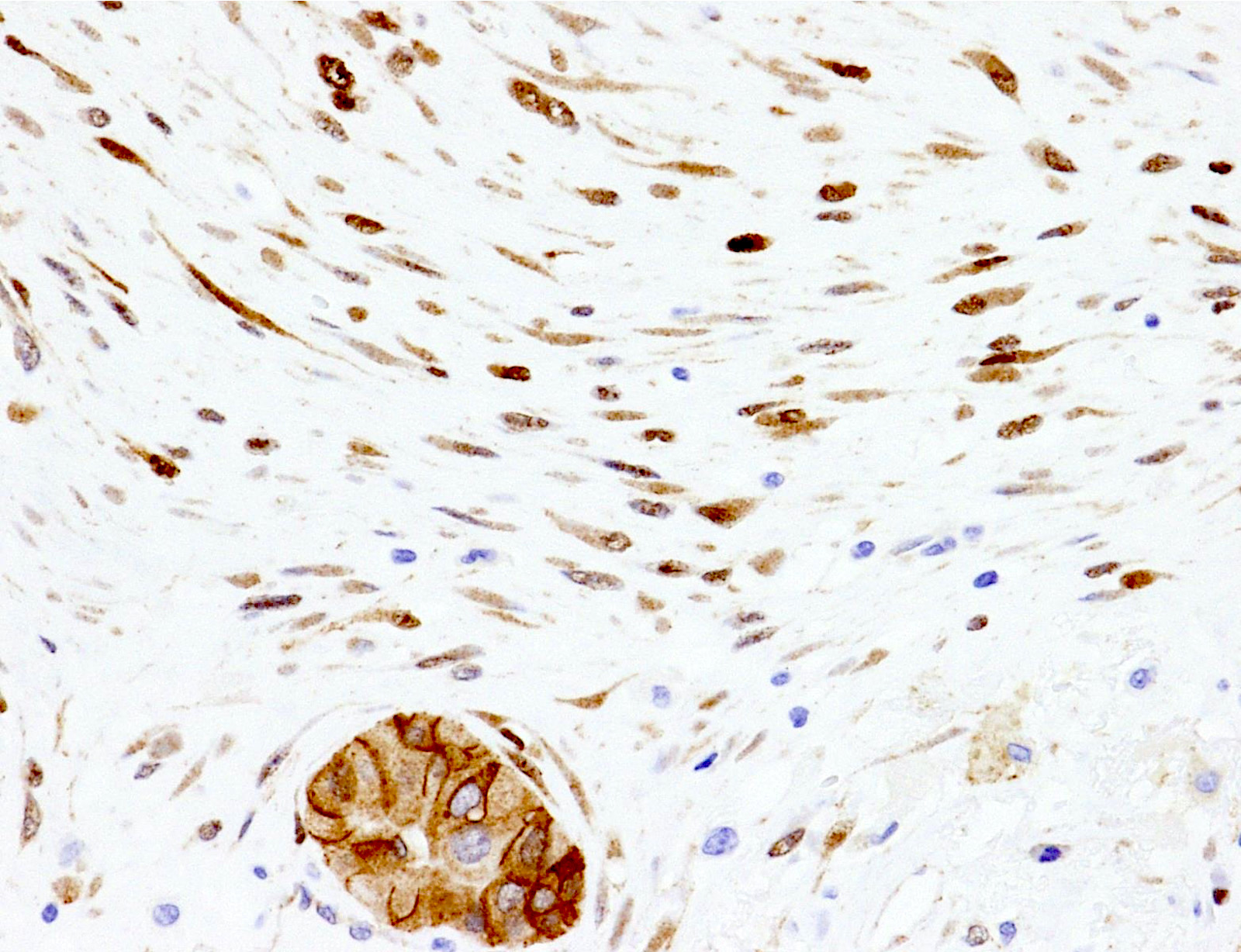
Positive stains
- PTC component:
- Cytokeratins: AE1 / AE3, CK7, CK19
- Thyroid specific markers: TTF1, thyroglobulin, PAX8
- Galectin3, HBME
- Membranous beta catenin staining
- Mesenchymal component:
- Nuclear and cytoplasmic staining for beta catenin in cases with fibromatosis-like stroma (Mod Pathol 2020;33:1702, Pathobiology 2018;85:300)
- Focal cytoplasmic beta catenin staining in nodular fasciitis-like variant
- Vimentin, alpha smooth muscle actin, desmin
- MIB1 < 5%
Negative stains
- CK20, calcitonin, S100, p53
Electron microscopy description
- Collagen fibers in proximity of mesenchymal cells (Mod Pathol 2017;30:236)
- Abundant rough endoplasmic reticulum
Molecular / cytogenetics description
- PTC: BRAF V600E mutation most common, rarely NRAS mutation (Mod Pathol 2020;33:1702)
- Mesenchymal component: CTNNB1 (beta catenin) mutations
- Absent USP6 gene rearrangement (limited evidence)
Differential diagnosis
- Hashimoto thyroiditis, fibrous variant:
- Absent PTC component
- No extrathyroidal extension / metastases
- Dense lymphocytic infiltrate, oncocytic metaplasia
- No beta catenin expression (nuclear or cytoplasmic) in stroma
- Riedel thyroiditis:
- Absent PTC component
- No lymph node metastases
- Lymphoplasmacytic infiltrate
- No beta catenin expression (nuclear or cytoplasmic) in fibroblasts
- Postoperative spindle cell nodules:
- Previous history of surgery
- Absent PTC component
- No metastases
- No beta catenin expression (nuclear or cytoplasmic) in fibroblasts
- Diffuse sclerosing variant of PTC:
- Diffuse involvement of one lobe or entire gland
- Stroma rich in lymphocytic infiltrate
- Numerous psammoma bodies
- Squamous metaplasia, squamous morules
- Rare fibroblastic proliferation
- No beta catenin expression (nuclear or cytoplasmic) in fibroblasts
- Anaplastic thyroid carcinoma:
- Marked atypia of spindle cells
- No beta catenin expression (nuclear or cytoplasmic) in fibroblasts
- May be positive for cytokeratin, PAX8 and p53
- Medullary thyroid carcinoma:
- Amyloid
- Stippled chromatin
- Calcitonin and pancytokeratin immunopositivity
- No beta catenin expression (nuclear or cytoplasmic) in fibroblasts
- Mesenchymal spindle cell neoplasms like solitary fibrous tumor, sarcoma:
- Specific immunoprofile
- Absent PTC component
Board review style question #1
How is the variant of papillary thyroid carcinoma shown in the image distinct from other variants?
- BRAF V600E mutation in epithelial component
- EWSR1 fusions
- CTNNB1 (beta catenin) mutation in mesenchymal component
- HRAS mutation in epithelial component
- CTNNB1 (beta catenin) mutation in epithelial component
Board review style answer #1
C. CTNNB1 (beta catenin) mutation in mesenchymal component
CTNNB1 (beta catenin) mutations have been documented in the mesenchymal component of papillary thyroid carcinoma (PTC) with fibromatosis / fasciitis-like stroma. The PTC (epithelial) component of this tumor lacks CTNNB1 mutation; it instead usually harbors BRAF V600E mutation and less commonly HRAS mutation. BRAF and HRAS mutations are, however, not specific for PTC with fibromatosis / fasciitis-like stroma. CTNNB1 mutations are seen in cancer cells of cribriform-morular variant of PTC. EWSR1 gene fusions are a hallmark of Ewing sarcoma.
Comment Here
Reference: Fibromatosis / fasciitis-like
CTNNB1 (beta catenin) mutations have been documented in the mesenchymal component of papillary thyroid carcinoma (PTC) with fibromatosis / fasciitis-like stroma. The PTC (epithelial) component of this tumor lacks CTNNB1 mutation; it instead usually harbors BRAF V600E mutation and less commonly HRAS mutation. BRAF and HRAS mutations are, however, not specific for PTC with fibromatosis / fasciitis-like stroma. CTNNB1 mutations are seen in cancer cells of cribriform-morular variant of PTC. EWSR1 gene fusions are a hallmark of Ewing sarcoma.
Comment Here
Reference: Fibromatosis / fasciitis-like
Board review style question #2
Which of the following is true about papillary thyroid carcinoma with fibromatosis / fasciitis-like stroma?
- Aggressive clinical course
- Fibromatosis may recur postthyroidectomy
- Only the epithelial component can metastasize
- Membranous expression of beta catenin in both epithelial and mesenchymal elements
- Stroma always mimics desmoid type fibromatosis
Board review style answer #2
B. Fibromatosis may recur postthyroidectomy
Clinical course of papillary thyroid carcinoma (PTC) with fibromatosis / fasciitis-like stroma is usually similar to classical PTC. The tumor is characterized by a prominent myofibroblastic proliferation reminiscent of fibromatosis or nodular fasciitis, hence the name. Stromal component of tumors with fibromatosis-like stroma commonly harbors CTNNB1 (beta catenin) mutation, which on immunohistochemistry is depicted by nuclear positivity and loss of membranous staining. The PTC component retains normal membranous beta catenin immunoreactivity. The tumor is also unique in that the patients can develop recurrence of fibromatosis postthyroidectomy. Metastases can show both mesenchymal and epithelial components similar to the primary tumor.
Comment Here
Reference: Fibromatosis / fasciitis-like
Clinical course of papillary thyroid carcinoma (PTC) with fibromatosis / fasciitis-like stroma is usually similar to classical PTC. The tumor is characterized by a prominent myofibroblastic proliferation reminiscent of fibromatosis or nodular fasciitis, hence the name. Stromal component of tumors with fibromatosis-like stroma commonly harbors CTNNB1 (beta catenin) mutation, which on immunohistochemistry is depicted by nuclear positivity and loss of membranous staining. The PTC component retains normal membranous beta catenin immunoreactivity. The tumor is also unique in that the patients can develop recurrence of fibromatosis postthyroidectomy. Metastases can show both mesenchymal and epithelial components similar to the primary tumor.
Comment Here
Reference: Fibromatosis / fasciitis-like