Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Diagrams / tables | Pathophysiology / etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Flow cytometry description | Differential diagnosisCite this page: Bychkov A. Thymic tissue. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidthymictissue.html. Accessed April 20th, 2024.
Definition / general
- Ectopic thymic tissue within the thyroid gland due to aberrant migration during embryogenesis
- First described by Rossle in 1932 (Virchows Archiv 1932;283:41)
- May give rise to thymoma, SETTLE, CASTLE (Hum Pathol 1991;22:349, Am J Surg Pathol 2006;30:994)
- A survey of the thyroids of 350 infants and children suggests that the presence of thymus and parathyroid tissue within the thyroid is so common as to be classified as normal (J Anat 1976;122:77)
Terminology
- Intrathyroidal thymic tissue, ectopic thymus within thyroid
Epidemiology
- Aberrant thymic tissue may be found in the neck of up to 20% of the general population, but intrathyroid ectopic thymic tissue is more rare and is usually found incidentally (Eur J Pediatr Surg 2002;12:327)
- Usually found in prepubertal pediatric population, rarely in adults due to age related involution
- Detected by ultrasound in 1% of general pediatric population (Thyroid 2015;25:534); increasing use of thyroid ultrasound in children results in an increased detection of intrathyroidal thymic inclusions (Horm Res Paediatr 2011;75:258)
- Portions of thymic tissue are present in 70% of normal thyroid glands of infants studied by serial sectioning techniques (J Anat 1976;122:77), 5% of random sections of fetal thyroid (Pediatr Pathol 1993;13:431); 0.1% - 2.6% on random sections of pediatric thyroid (Pediatr Pathol 1993;13:181, J Anat 1976;122:77)
- 50+ morphologically verified cases have been reported, including < 10 cases in adults; additional 420+ cases were verified by ultrasound
- M = F, mean age is 6.5 years at detection
Sites
- L > R, bilateral in 5%
- Mid to lower portion of thyroid lobes
- Often close to the surface
Pathophysiology / etiology
- The closely related descent of the thyroid and parathyroid glands and thymus explains their ectopic location within each other (J Ultrasound Med 2015;34:1651)
- As most of the thymus and inferior parathyroid glands are derived from the third pharyngeal pouch, they migrate together, and maldescending thymic portions can be trapped within the thyroid (Int J Clin Exp Pathol 2014;7:6375)
- A small and inconstant portion of thymic gland derives from the fourth branchial pouch (thymus IV, accessory thymus), together with the upper parathyroid glands and ultimobranchial body, which may become another source of thymic tissue within thyroid (Pediatr Pathol 1993;13:431)
Clinical features
- Rarely symptomatic and may mimic solid (rarely cystic) thyroid nodule found accidentally on US or CT / MRI
- Most cases occur in prepubertal children, correlating with a period of maximum growth of the thymus
- Adult cases are exceedingly rare, most likely due to age related involution (Arch Pathol Lab Med 2001;125:842)
- Thymic remnants are usually found in an orthotopic (normal) position or around the thyroid gland; an intrathyroidal thymus is rarely contiguous with the mediastinal thymus (Horm Res Paediatr 2011;75:258)
Diagnosis
- US is a sensitive tool because of the unique echogenicity of thymic tissue
- FNAC and flow cytometry may confirm thymic tissue in preoperative settings, although thyroid FNA in children is challenging
- Most of the early cases removed surgically were diagnosed only on histopathology
Radiology description
- US of ectopic thymus is identical to echotexture of the orthotopic thymus:
- Irregular, triangular, polygonal hypoechoic (rarely hyperechoic) area with punctate, granular or linear bright internal echoes surrounded by normal thyroid tissue (J Clin Ultrasound 2012;40:266, Thyroid 2015;25:534)
- Can show accidental and challenging microcalcification representing Hassall corpuscules (J Pediatr Endocrinol Metab 2012;25:997)
- Hypovascular on Doppler (Endocr Pract 2014;20:e241)
- Can be compared with suprasternal thymus in children
- MRI is similar to that of the mediastinal thymus:
- In children, normal thymic tissue is homogeneous and of low signal intensity, though slightly higher than that of muscle on T1-weighted images
- On T2-weighted images, the signal intensity of thymus tissue is less than that of fat, and as the child ages, the thymus becomes infiltrated with more fat, thus increasing the signal of both T1- and T2-weighted images (J Clin Ultrasound 2008;36:443)
- RAI scan: cold nodule (Journal of Pediatric Surgery 2013;1:386)
Prognostic factors
- Pediatric cases rarely become cystic; most resolve at puberty and do not progress (Pediatr Radiol 2010;40:1774)
- Extremely rare to progress to neoplasm
Case reports
- 2 year old girl with incidental finding of a hypodense, homogeneous thyroid lesion (JAMA Otolaryngol Head Neck Surg 2013;139:87)
- 2 year old boy and 4 year old girl with ectopic intrathyroidal thymus (Journal of Pediatric Surgery 2013;1:386)
- 4 year old boy with intrathyroidal thymic tissue mimicking a malignant thyroid nodule (Ultrasonography 2014;33:71)
- 6 year old boy with intrathyroidal thymic tissue (Thyroid 2008;18:377)
- 12 year old boy with ectopic thymus presenting as a thyroid nodule (Thyroid 2009;19:293)
- 16 year old girl with ectopic thymic tissue (Eur J Pediatr Surg 2002;12:327)
- 22 year old woman with ectopic thymus adjacent to thyroid and parathyroid (Arch Pathol Lab Med 2001;125:842)
- 27 year old woman with ectopic intrathyroidal thymus (ISPUB 2008:3(1))
- 29 year old woman with ectopic intrathyroidal thymus accompanied by intrathyroidal parathyroid (Int J Clin Exp Pathol 2014;7:6375)
- 31 year old woman with intrathyroidal thymic tissue (Korean J Pathol 2011;45:547)
- 73 year old man with intrathyroidal multiloculated proliferating thymic cyst (Endocr Pathol 2015;26:45)
Treatment
- US surveillance of nodule without invasive procedures is advocated in children (Horm Res Paediatr 2011;75:258)
- Aggressive approach with surgical excision is uncommon; it is recommended that the presence of a normal mediastinal thymus be confirmed before such surgery to avoid potential immunodeficiency (Journal of Pediatric Surgery 2013;1:386)
Clinical images
Gross description
- Whitish yellow, well demarcated solid nodule, < 1 cm
- May be confused with normal parathyroid gland, if located superficially
- Rarely cystic (Endocr Pathol 2015;26:45)
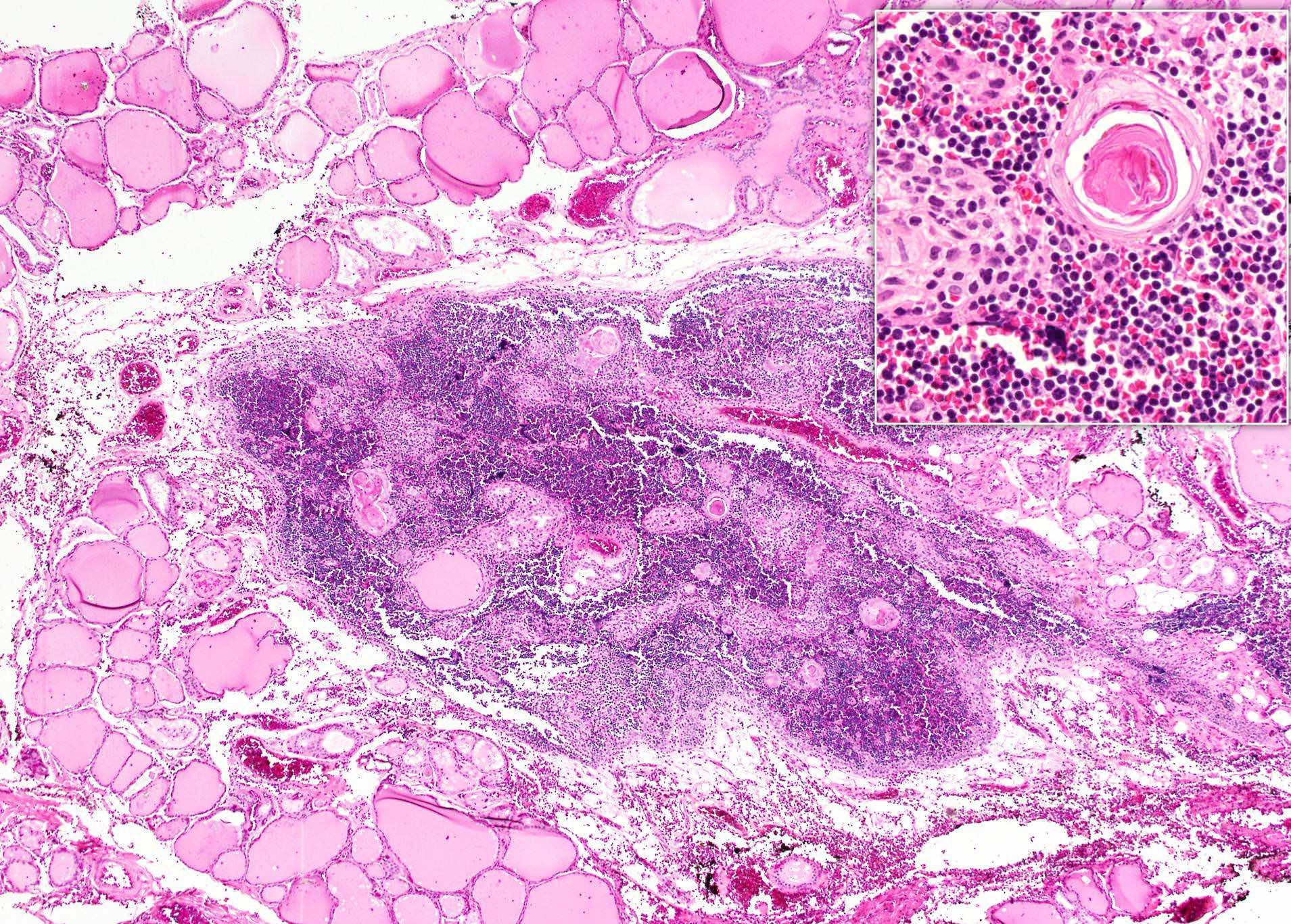
Microscopic (histologic) description
- Mature lymphoid tissue with numerous Hassall corpuscles embedded within thyroid gland
- Extent may vary from a small area of thymic tissue containing one or two Hassall bodies, to complete well differentiated glands with distinct cortex and medulla (J Anat 1976;122:77)
- Marked adipose involution in adults (Neuroradiology 2013;55:1405)
- Small quantities of thyroid follicular epithelial cells can be embedded in the adipose tissue of the heterotopic thymus (Korean J Pathol 2011;45:547)
- Ultimobranchial body remnants or ectopic parathyroid can be found in the vicinity (J Anat 1976;122:77, Thyroid 2008;18:1125)
Microscopic (histologic) images
Cytology description
- Abundant small and medium sized lymphocytes with a mature chromatin pattern, Hassall corpuscles (Thyroid 2009;19:403, J Clin Ultrasound 2012;40:266)
- Relative admixture of epithelial cells and colloid present depends on precise targeting of the nodule (J Pediatr Surg 1997;32:1241, Arch Pathol Lab Med 2001;125:842)
Cytology images
Positive stains
- TdT in thymic lymphocytes
- CK5 / CK6 in thymic epithelial cells (J Ultrasound Med 2015;34:1651)
Negative stains
Flow cytometry description
- Uniformly maturing T cells (Thyroid 2009;19:403):
- CD4 / CD8 coexpression with trailing expression of either CD4 or CD8
- CD5+ T cells
- No clonal B cells
Differential diagnosis
- Histology: Hashimoto thyroiditis
- Cytology
- Ectopic and hamartomatous thymoma, spindle epithelial tumor with thymus-like differentiation, carcinoma showing thymus-like differentiation: atypical cells (Hum Pathol 1991;22:349)
- Hashimoto thyroiditis: degenerated follicular epithelial cells, metaplastic epithelial cells, plasma cells or lymphoplasmacytic cells (Thyroid 2009;19:403)
- Lymphoma: atypical morphology of lymphoid cells, lymphoblasts