Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Case reports | Clinical images | Sample assessment & plan | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Swenson E. Washing & volume reduction. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/transfusionmedwashing.html. Accessed September 17th, 2025.
Definition / general
- Washing of blood products replaces plasma with saline and reduces proinflammatory cells, molecules, additives and minerals
- Washing creates an open system and the unit expiration date is decreased
Essential features
- Blood product modification on red blood cell and platelet units to decrease proinflammatory cells, molecules, additives (mannitol) and minerals by replacing plasma with 0.9% sodium chloride (Transfusion 2011;51:955)
- Creates an open system; therefore, the unit expiration date is decreased to 24 hours or 4 hours, depending on how the unit is stored
- Indications for washing red blood cell (RBC) units include
- Hyperkalemia
- Removal of plasma proteins and inflammatory cells in patients who have had allergic transfusion reactions, including
- IgA deficient patients
- Patients with haptoglobinemia
- Red blood cell units for intrauterine transfusions
- Cryopreserved red blood cell units to remove glycerol
- Indications for washing platelet units
- Patients with allergic transfusion reaction history, unmitigated by antihistamines or steroids
- Decreases the volume of red blood cells and platelets
- Cell salvage - procedure performed in the operating room where shed blood is collected, washed or filtered and returned to the patient to reduce allogeneic transfusion
Terminology
- Washing: an automated or manual blood product modification process by which plasma is removed from platelet and red blood cell units and is replaced with saline solution (Transfusion 2011;51:955)
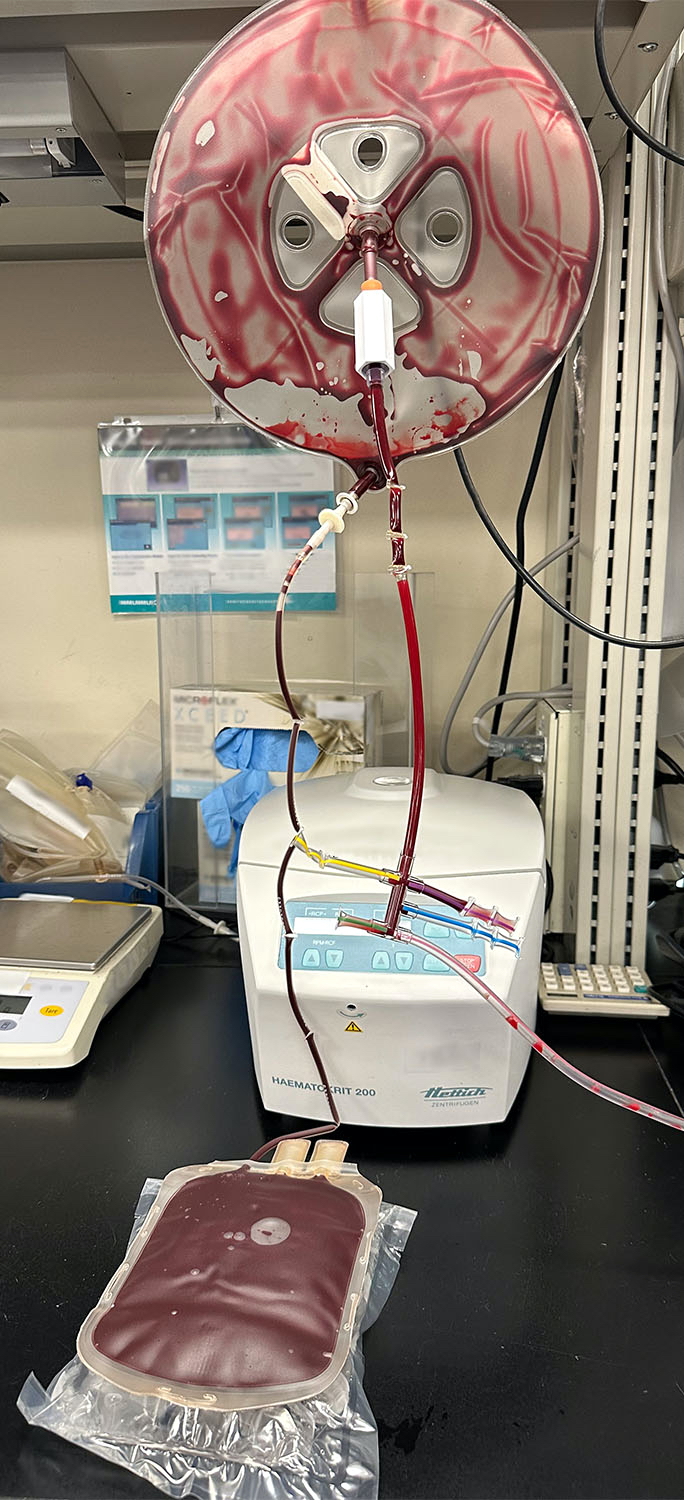
- Cell salvage: a process by which autologous blood is shed by a patient during a surgical procedure, collected, washed and then returned to the patient (Medicine (Baltimore) 2016;95:e4490)
Clinical features
- Washing of RBC can be performed either by manual or automated methods
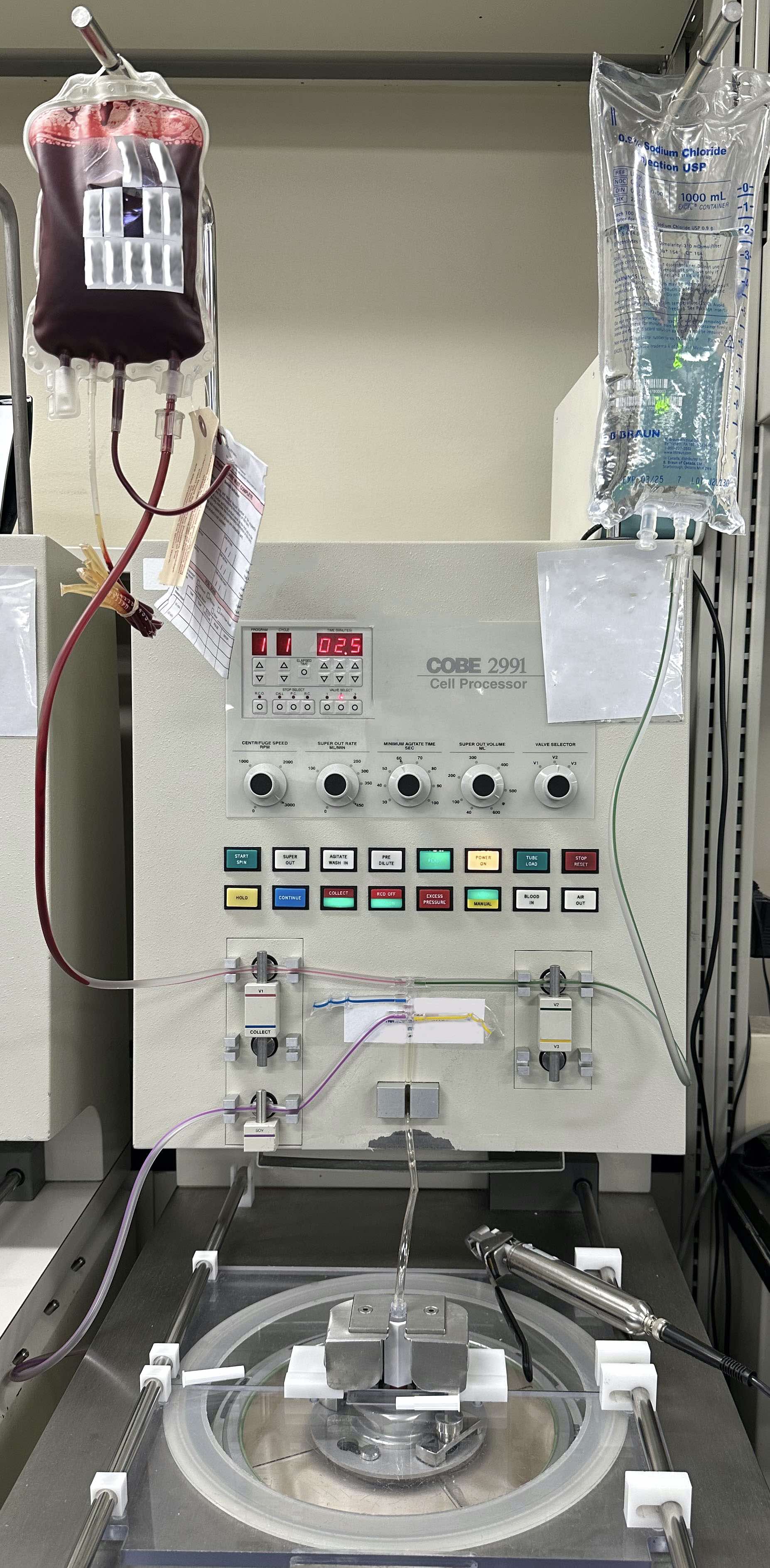
- In a survey of 15 children's hospitals in the United States, 88% of hospitals used the COBE 2991 cell washer (see image below) (Transfusion 2011;51:955)
- In a small study of 8 RBC units, units washed on the COBE 2991 cell washer had the same or higher K+ concentrations at 24 hours after washing compared to prewash values (Transfusion 2011;51:955)
- Creates an open system and increases the risk of bacterial contamination
- Subsequently, the unit expiration date is decreased to
- 24 hours for products stored at 1 - 6 °C
- 4 hours for products stored at 20 - 24 °C
- Subsequently, the unit expiration date is decreased to
- Decreases the volume of a RBC unit by ~20 - 25% and a platelet unit by up to 33%
- Activates platelets and reduces platelet count recovery and survival (Anesth Analg 2004;99:17, Transfusion 2012;52:1221)
- Indications for RBC washing
- Hyperkalemia
- Defined as potassium (K+) concentration > 5.5 mmol/L
- Decreases the resting membrane potential of cardiac myocytes, leading to life threatening arrhythmias and cardiac arrest as K+ levels rise (Circ Arrhythm Electrophysiol 2017;10:e004667)
- Inhibition of the RBC membrane Na-K-ATPase pump in CPD-A or additive solution cold stored red blood cells results in leakage of K+ into the supernatant of red blood cell units
- Irradiation (gamma or Xray) further increases the K+ leak by damaging the red blood cell membrane (Transfus Med Rev 2022;36:133)
- Large volume transfusions in pediatric and adult patients may result in transfusion associated hyperkalemia (Transfus Med Rev 2022;36:133, Transfusion 2021;61:1093)
- Removes the supernatant and replaces it with sodium chloride solution
- Decreases the K+ volume
- Randomized controlled trials show conflicting results (Turk J Med Sci 2017;47:407, Eur J Cardiothorac Surg 2007;31:659)
- History of allergic transfusion reaction (ATR)
- Allergic transfusion reactions: type I hypersensitivity reactions where IgE antibodies interact with an allergen and cause activation of mast cells and basophils
- Biogenic amines, including histamine and adenosine, eosinophil and neutrophil chemotactic factors, bradykinin and proteoglycans mediate ATRs (Transfusion 2011;51:1676)
- Washing RBC and apheresis platelet units reduced the incidence of allergic transfusion reactions from 2.7% to 0.3% and 5.5% to 0.5%, respectively (Transfusion 2011;51:1676)
- In patients with IgA deficiency and haptoglobinemia, prior exposure results in antibodies to IgA or haptoglobin
- Future transfusions, with exposure to IgA or haptoglobin, result in allergic transfusion reactions
- Washing of RBC units and apheresis platelet units can decrease incidence of transfusion reactions (Transfusion 2018;58:2320, Ann Lab Med 2012;32:304, Transfusion 2015;55:2415)
- Allergic transfusion reactions: type I hypersensitivity reactions where IgE antibodies interact with an allergen and cause activation of mast cells and basophils
- Intrauterine transfusion (IUT)
- RBC units used for IUT should be group O, crossmatch compatible with maternal plasma, irradiated to prevent transfusion associated graft versus host disease, cytomegalovirus (CMV) safe (either leukoreduced or from a CMV seronegative donor), lacking Hgb S, collected within 5 - 7 days, washed or concentrated to a hematocrit of 70 - 85%
- In a survey of IUT practices in the U.S., 56% of 32 institutions always washed RBC units (Transfusion 2022;62:2449)
- Part of the deglycerolizing process
- RBC cryopreserved in glycerol (40% concentration) are thawed in a 37 °C water bath and then the glycerol needs to be removed via washing
- Glycerol is replaced with a 0.9% sodium chloride and 2% dextrose solution
- Hyperkalemia
- Indications for platelet unit washing
- Reducing exposure to antibodies against recipient antigens
- In neonatal alloimmune thrombocytopenia (NAIT), maternal antibodies against fetal platelet antigens, most commonly against HPA-1a, can cause severe thrombocytopenia
- Maternal platelets can be used for transfusion in the fetus or neonate and washing of the platelets can remove the maternal anti-HPA-1a antibodies (Transfusion 1982;22:125)
- History of allergic transfusion reaction (in particular, related to IgA deficiency / haptoglobinemia)
- In one study, washing apheresis platelet units reduced the incidence of allergic transfusion reactions from 5.5% to 0.5% (Transfusion 2011;51:1676)
- Reducing exposure to antibodies against recipient antigens
- Intraoperative cell salvage
- Blood shed during operative procedures is collected and either washed or filtered and then returned to the patient
- Cell salvage procedures have been shown to decrease the need for allogeneic RBC transfusions in cardiac, vascular and orthopedic surgery, among others (Medicine (Baltimore) 2016;95:e4490)
Case reports
- Neonate from a B r’r’ mother with anti-c and anti-S antibodies underwent RBC exchange for hyperbilirubinemia using 2 frozen antigen negative RBC units that were thawed and washed (Transfus Med 2019;29:128)
- 44 year old man who underwent emergent multivessel coronary artery bypass grafting requiring extracorporeal membrane oxygenation (ECMO), complicated by heparin induced thrombocytopenia (HIT) and disseminated intravascular coagulopathy (DIC), required massive transfusion as well as 19.7 L washed RBCs from cell salvage (Perfusion 2019;34:337)
- 50 year old woman, with relapsed acute promyelocytic leukemia and anhaptoglobinemia (deletion of Hp gene cluster) and haptoglobin antibodies, received washed apheresis platelet units (Ann Lab Med 2012;32:304)
- 88 year old woman with IgA deficiency, anti-IgA class IgG antibodies and monocytopenia and neutropenia after red blood cell transfusion, managed by red blood cell washing (Transfusion 2018;58:2320)
Sample assessment & plan
- Assessment: Jane Doe is a 78 year old woman with a history of residual / recurrent acute myeloid leukemia and a history of red blood cell transfusions. She developed an anaphylactic transfusion reaction 15 minutes into a red blood cell transfusion, requiring treatment with epinephrine, ICU transfer and ventilator support. Workup found IgA deficiency with anti-IgA class IgG antibodies.
- Plan: The patient presentation and laboratory workup are consistent with a diagnosis of IgA deficiency with anti-IgA antibodies.
- The patient will be supported with washed red blood cell products. Please allow extra time to prepare this product (~2 hours).
- Limiting transfusions of plasma containing products is recommended.
Additional references
Practice question #1
Practice answer #1
A. 24 hours. A washed red blood cell unit expires 24 hours after it has been washed. Answers B - E are incorrect because the 24 hour expiration supersedes all other expiration time points. The shelf life for a unit collected in CPD-A is 35 days. An irradiated unit will expire 28 days after irradiation in Europe and 28 days from the irradiation date or the original expiration date in the U.S., whichever comes earlier. Red blood cell units collected in additive solutions have 42 day shelf lives.
Comment Here
Reference: Transfusion medicine - Washing
Comment Here
Reference: Transfusion medicine - Washing
Practice question #2
For which patient would red blood cell washing be recommended?
- 26 year old man, O positive, with sickle cell disease with anti-C, anti-e, anti-Fyb antibodies who presents for his monthly red blood cell exchange of 6 red blood cell units and the blood bank has 6 antigen negative liquid units available
- 54 year old man with aplastic anemia requiring transfusion support with history of multiple previous mild allergic transfusion reactions
- 78 year old woman on dialysis with recent myocardial infarction and peripheral edema
- Intrauterine transfusion for a fetus with hematocrit of 25% in a mother with anti-D titer of 1:256
- Neonate being placed on extracorporeal membrane oxygenation (ECMO) and fresh red blood cell units are available
Practice answer #2
D. Intrauterine transfusion for a fetus with hematocrit of 25% in a mother with anti-D titer of 1:256. RBCs used for intrauterine transfusion should be group O and crossmatch compatible with maternal plasma, be irradiated to prevent transfusion associated graft versus host disease, be CMV risk reduced (leukoreduced or from a CMV negative donor) and lack hemoglobin S. Units can be washed or concentrated to a hematocrit of 70 - 85%.
Answer A is incorrect because patients with sickle cell disease who have developed multiple alloantibodies may need rare cryopreserved red blood cell units. In this current case, the patient's red blood cell needs can be supported by available liquid units but if he is further alloimmunized and requires rare cryopreserved red blood cell units, cryopreserved units need to undergo washing to remove the glycerol preservative prior to being transfused.
Answer B is incorrect because a 54 year old man with history of mild allergic transfusion reactions does not need washed products at this time. If he has an anaphylactic transfusion reaction, that would be an indication for washed RBC units.
Answer C is incorrect because this patient is exhibiting risk factors for transfusion associated circulatory overload (TACO). Washing of RBCs can mitigate transfusion related acute lung injury (TRALI), possibly by removing proinflammatory cells and molecules stored in RBCs. Washing does not mitigate TACO. Recommended methods for TACO mitigation include judicious transfusion, slow transfusion rate (no greater than 4 hours) and diuresis.
Answer E is incorrect because a neonate on ECMO can be supported with fresh red blood cell units. As red blood cell units age, they leak potassium, which can cause cardiac arrhythmias in neonates. If no fresh red blood cell units are available, washed RBC units can be used.
Comment Here
Reference: Transfusion medicine - Washing
Answer A is incorrect because patients with sickle cell disease who have developed multiple alloantibodies may need rare cryopreserved red blood cell units. In this current case, the patient's red blood cell needs can be supported by available liquid units but if he is further alloimmunized and requires rare cryopreserved red blood cell units, cryopreserved units need to undergo washing to remove the glycerol preservative prior to being transfused.
Answer B is incorrect because a 54 year old man with history of mild allergic transfusion reactions does not need washed products at this time. If he has an anaphylactic transfusion reaction, that would be an indication for washed RBC units.
Answer C is incorrect because this patient is exhibiting risk factors for transfusion associated circulatory overload (TACO). Washing of RBCs can mitigate transfusion related acute lung injury (TRALI), possibly by removing proinflammatory cells and molecules stored in RBCs. Washing does not mitigate TACO. Recommended methods for TACO mitigation include judicious transfusion, slow transfusion rate (no greater than 4 hours) and diuresis.
Answer E is incorrect because a neonate on ECMO can be supported with fresh red blood cell units. As red blood cell units age, they leak potassium, which can cause cardiac arrhythmias in neonates. If no fresh red blood cell units are available, washed RBC units can be used.
Comment Here
Reference: Transfusion medicine - Washing