Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Han L, Bennett JA. High grade endometrial stromal sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusESShighgrade.html. Accessed April 19th, 2024.
Definition / general
- Malignant uterine mesenchymal tumor originating from the endometrial stroma
Essential features
- Cellular tumor with high grade round or spindle cells, sometimes with an associated low grade component
- Variable positivity for BCOR, cyclin D1 and CD10, depending on molecular alteration present; often negative or only focally positive for smooth muscle markers and hormone receptors
- Major subtypes include sarcomas with YWHAE::NUTM2A/B fusions, BCOR rearranged and BCOR internal tandem duplication (ITD)
Terminology
- Undifferentiated endometrial sarcoma, uniform type
- High grade endometrial stromal sarcoma with YWHAE::FAM22 fusions
ICD coding
Epidemiology
- Rare, wide age range
- YWHAE::NUTM2A/B fusions: 28 - 67 (mean 50) years (Am J Surg Pathol 2012;36:641)
- BCOR rearranged: 28 - 71 (median 54) years (Mod Pathol 2018;31:674)
- BCOR ITD: 14 - 55 (median 42) years (Oncology 2019;96:101)
- High grade transformation: 45 - 74 (median 54) years (Mod Pathol 2020;33:1861)
Sites
- Uterine corpus
- Rarely vagina (Mod Pathol 2020;33:1861)
Pathophysiology
- Several alterations have been described (YWHAE::NUTM2A/B fusions, BCOR fusions, BCOR ITD) (Am J Surg Pathol 2012;36:641, Mod Pathol 2018;31:674, Oncology 2019;96:101)
- High grade transformation of low grade endometrial stromal sarcoma (Mod Pathol 2020;33:1861)
Etiology
- Unknown
Clinical features
- Pelvic pain, pelvic mass, abnormal uterine bleeding
Diagnosis
- Hysterectomy needed for definitive diagnosis
- Rarely diagnosed on endometrial biopsy / curettage
Radiology description
- MRI (Cancer Imaging 2019;19:63):
- Solid and occasionally cystic mass
- Feather-like enhancement, hemorrhage and necrosis
Prognostic factors
- Intermediate prognosis between low grade endometrial stromal sarcoma and undifferentiated uterine sarcoma
- Limited number of cases reported with limited followup information to identify favorable / unfavorable prognostic factors
Case reports
- 40 year old woman with a 4 month history of recurrent right sided lower thoracic pain and previous hysterectomy (BMC Cancer 2018;18:92)
- 41 year old woman with a 6 month history of menorrhagia (Int J Gynecol Pathol 2019;38:420)
- 51 year old woman with brown discharge and postcoital bleeding (Virchows Arch 2020;476:615)
Treatment
- Cytoreductive surgery and multimodality therapy (Taiwan J Obstet Gynecol 2016;55:625)
- Anthracycline based chemotherapy for YWHAE::NUTM2A/B sarcomas (Gynecol Oncol 2017;145:531)
- Potential role for MDM2 or CDK4 inhibitors in BCOR rearranged sarcomas with MDM2 amplification or alterations of genes in the cyclin D1 / CDK4 kinase pathway (Gynecol Oncol 2020;157:357, J Pathol Clin Res 2020;6:178)
- Limited role for antihormonal therapy as most lack or have limited ER / PR expression
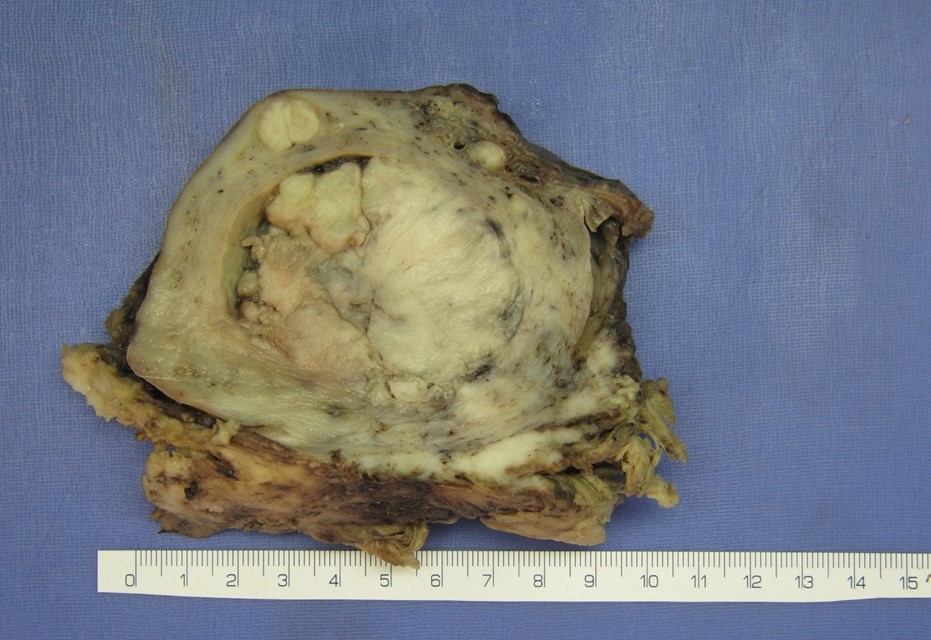
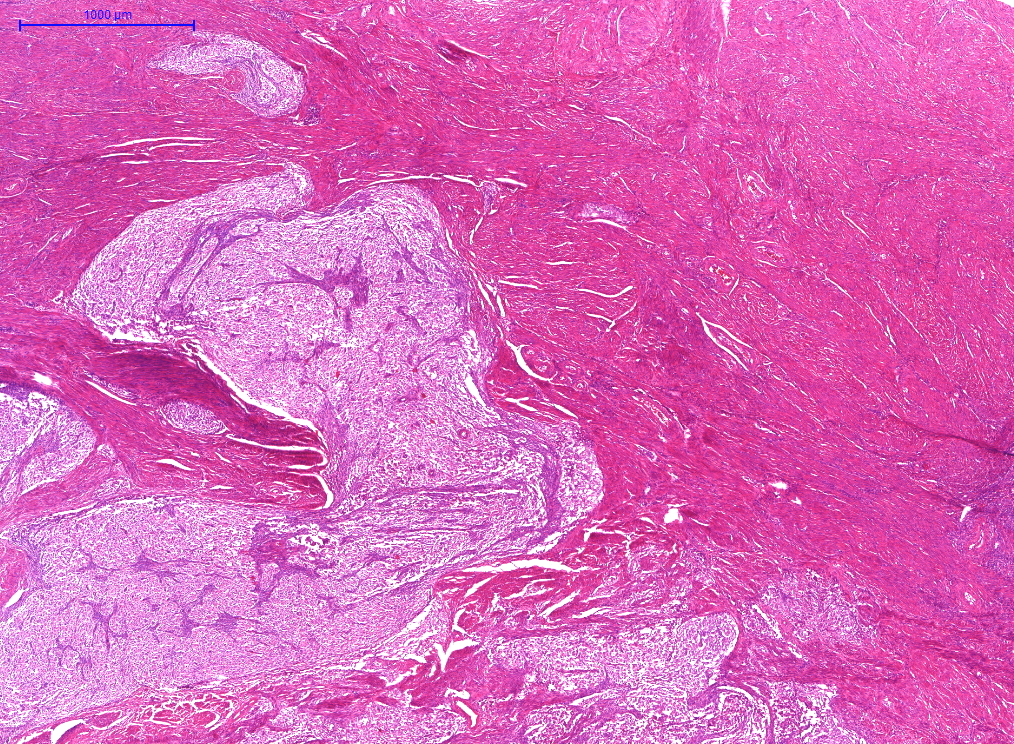
Gross description
- YWHAE::NUTM2A/B fusions (Histopathology 2015;67:1)
- 1 - 12 cm
- Gross mass with permeative myoinvasion
- BCOR rearranged (Mod Pathol 2018;31:674)
- 1.5 - 12 (median 9.7) cm
- Tan-pink to yellow
- Soft, fleshy or rubbery
- Can be polypoid involving the endometrium; rarely myometrial confined
- BCOR ITD (Am J Surg Pathol 2018;42:335, Oncology 2019;96:101)
- 2.5 - 14.5 (median 7) cm
- Can be polypoid with additional intramural nodular masses
Gross images
Frozen section description
- High grade sarcoma with spindled and epithelioid cells, defer to permanent sections and ancillary (immunohistochemical and molecular) studies
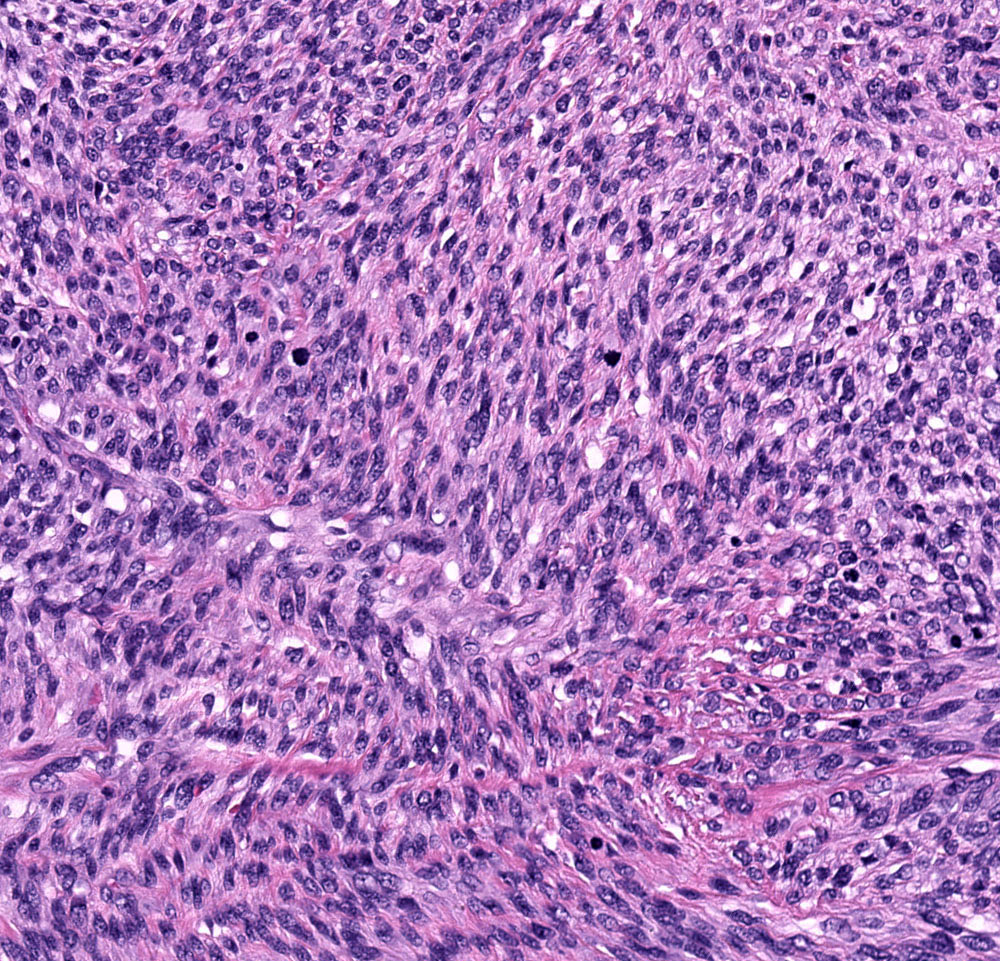
Microscopic (histologic) description
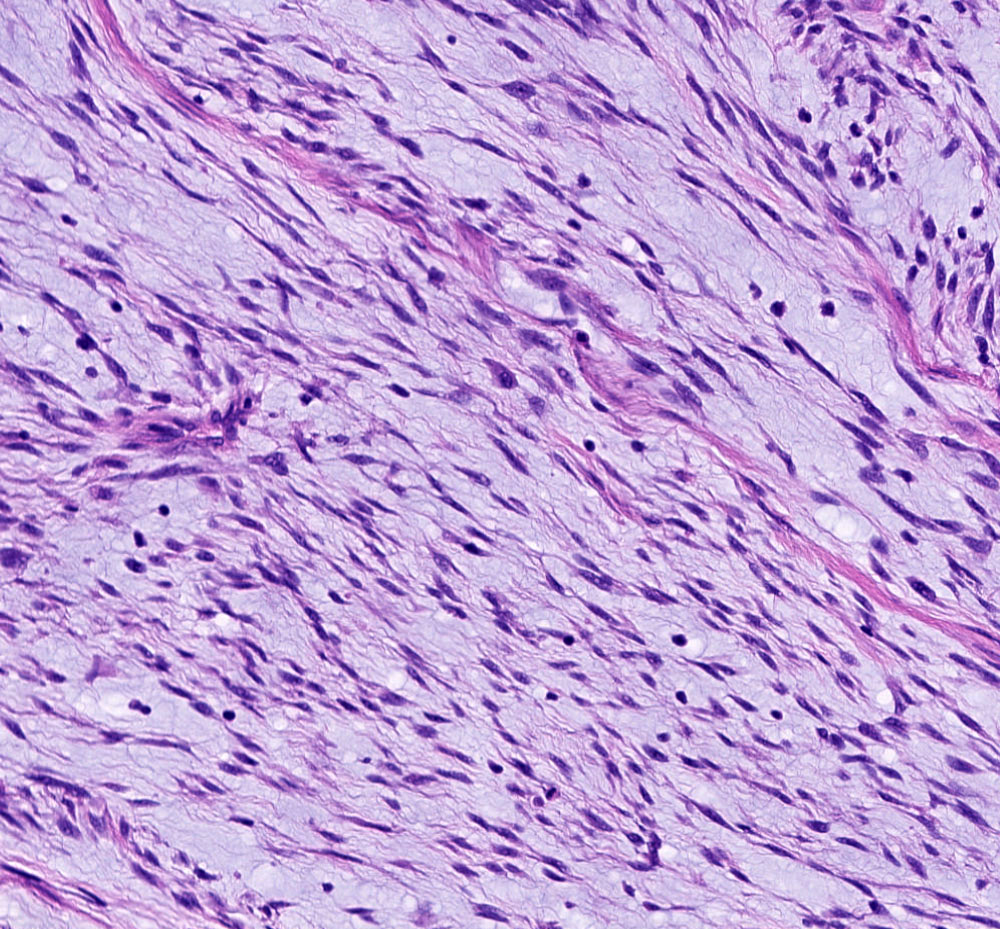
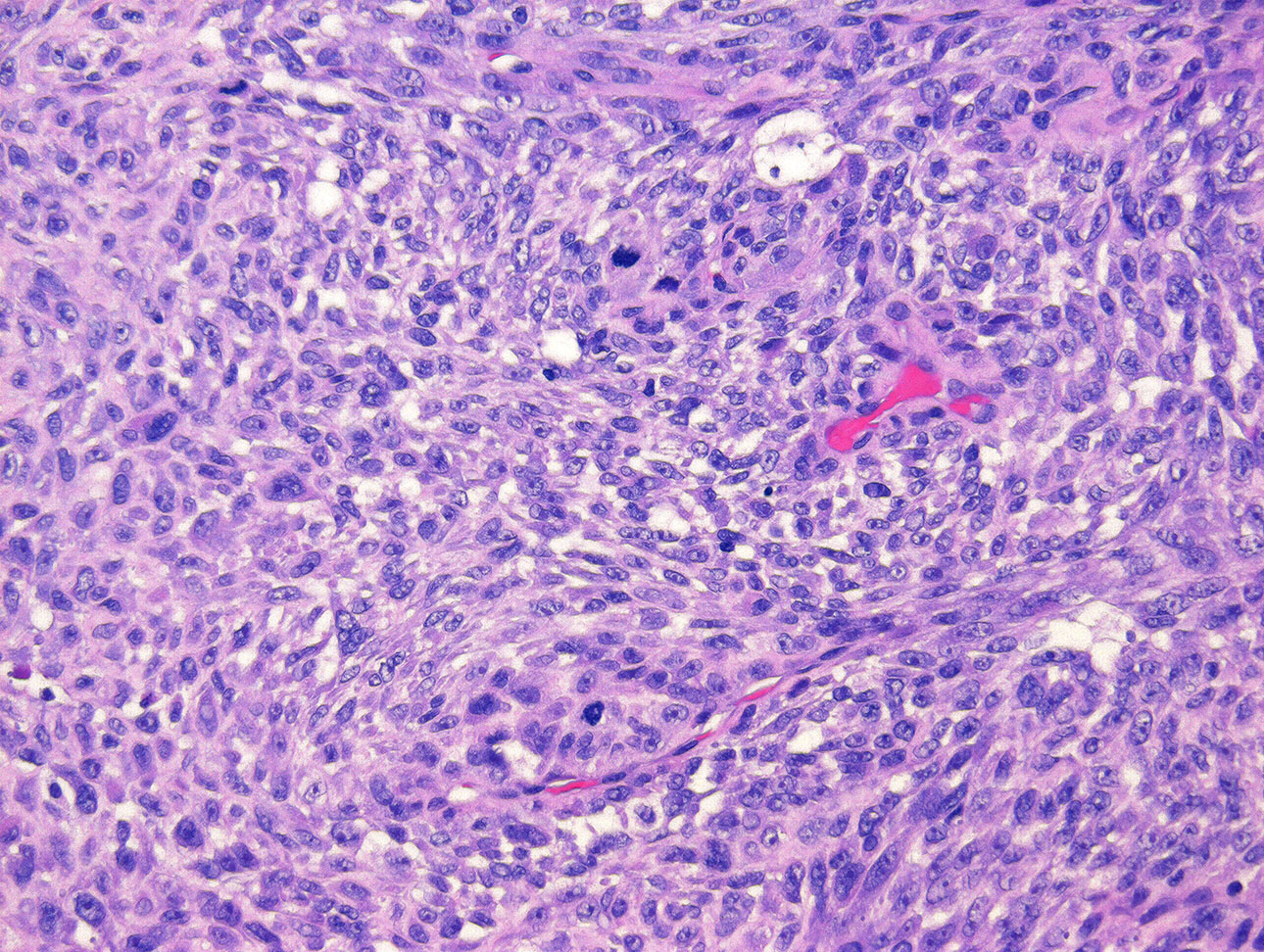
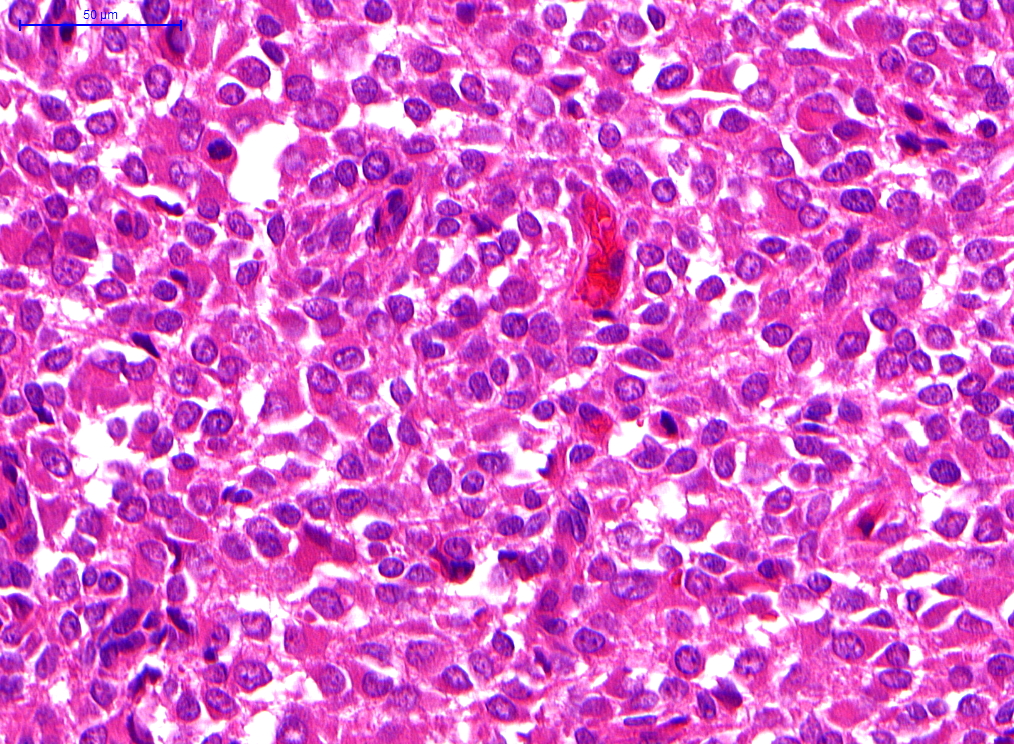
- YWHAE::NUTM2A/B fusions (Am J Surg Pathol 2012;36:641, Mod Pathol 2013;26:1390, Histopathology 2015;67:1, Pathology 2018;50:162):
- Permeative (tongue-like) invasion
- Vaguely nested growth of round cells with scant (small round blue cell appearance) to moderate eosinophilic cytoplasm and uniform nuclear atypia
- Brisk mitoses (> 10/10 high power fields)
- Tumor cell necrosis and lymphovascular invasion common
- Delicate network of arborizing or curvilinear vessels
- 50% associated with a low grade spindle cell component resembling low grade endometrial stromal sarcoma
- Admixed or occasionally well demarcated
- Monomorphic bland spindle cells
- Fibrous to fibromyxoid matrix
- Low mitoses (≤ 3/10 high power fields)
- Typically lacks necrosis
- Variant features include pseudoglandular or pseudopapillary appearance, sex cord-like differentiation, rosette-like formations
- Overt nuclear pleomorphism rare
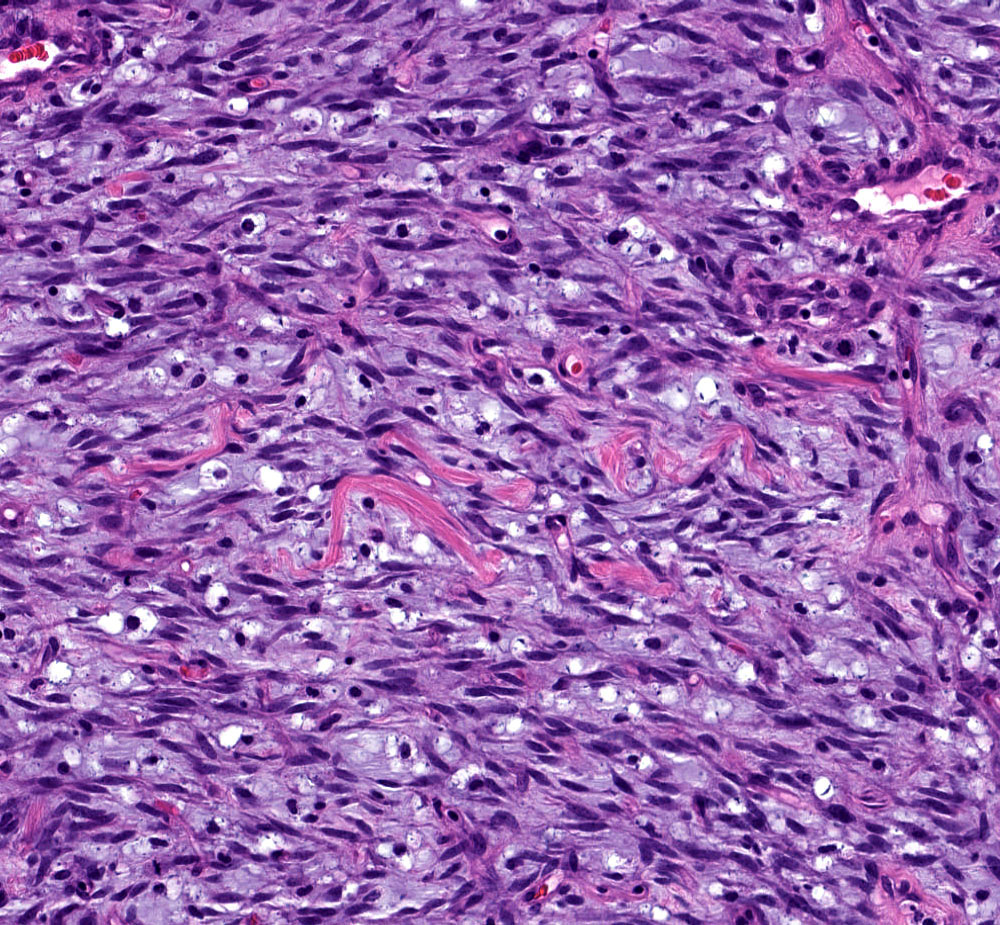
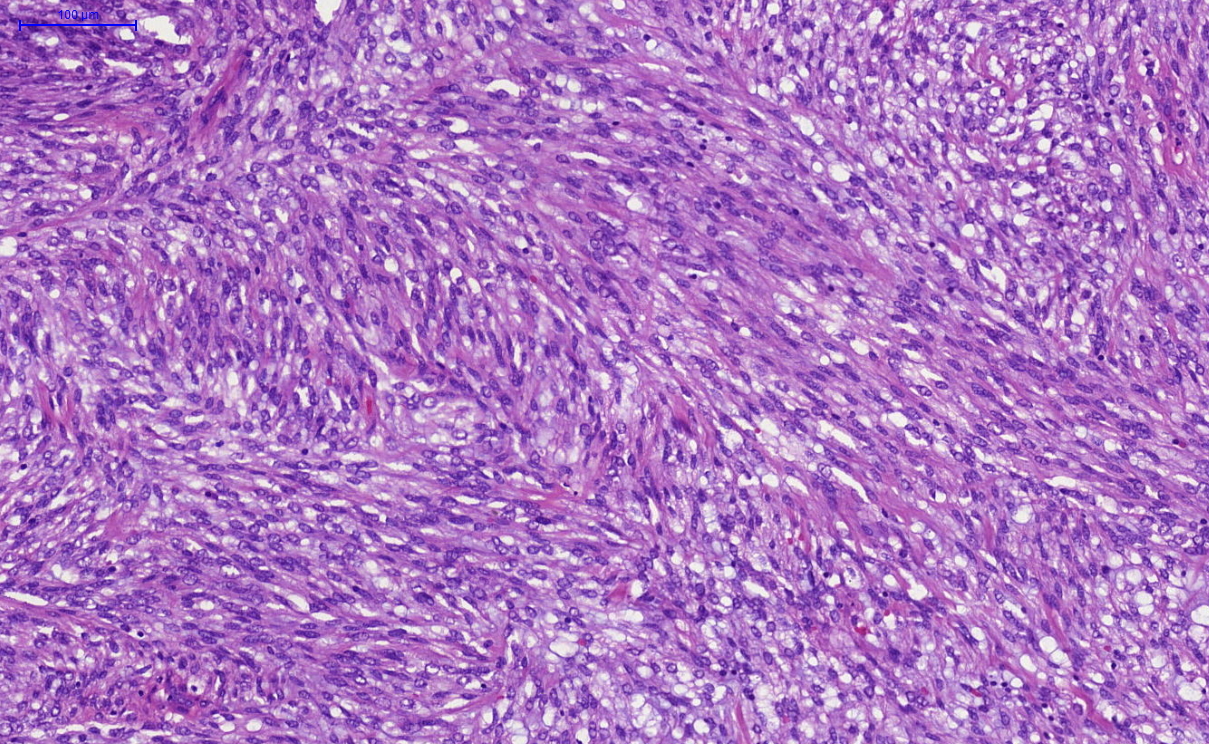
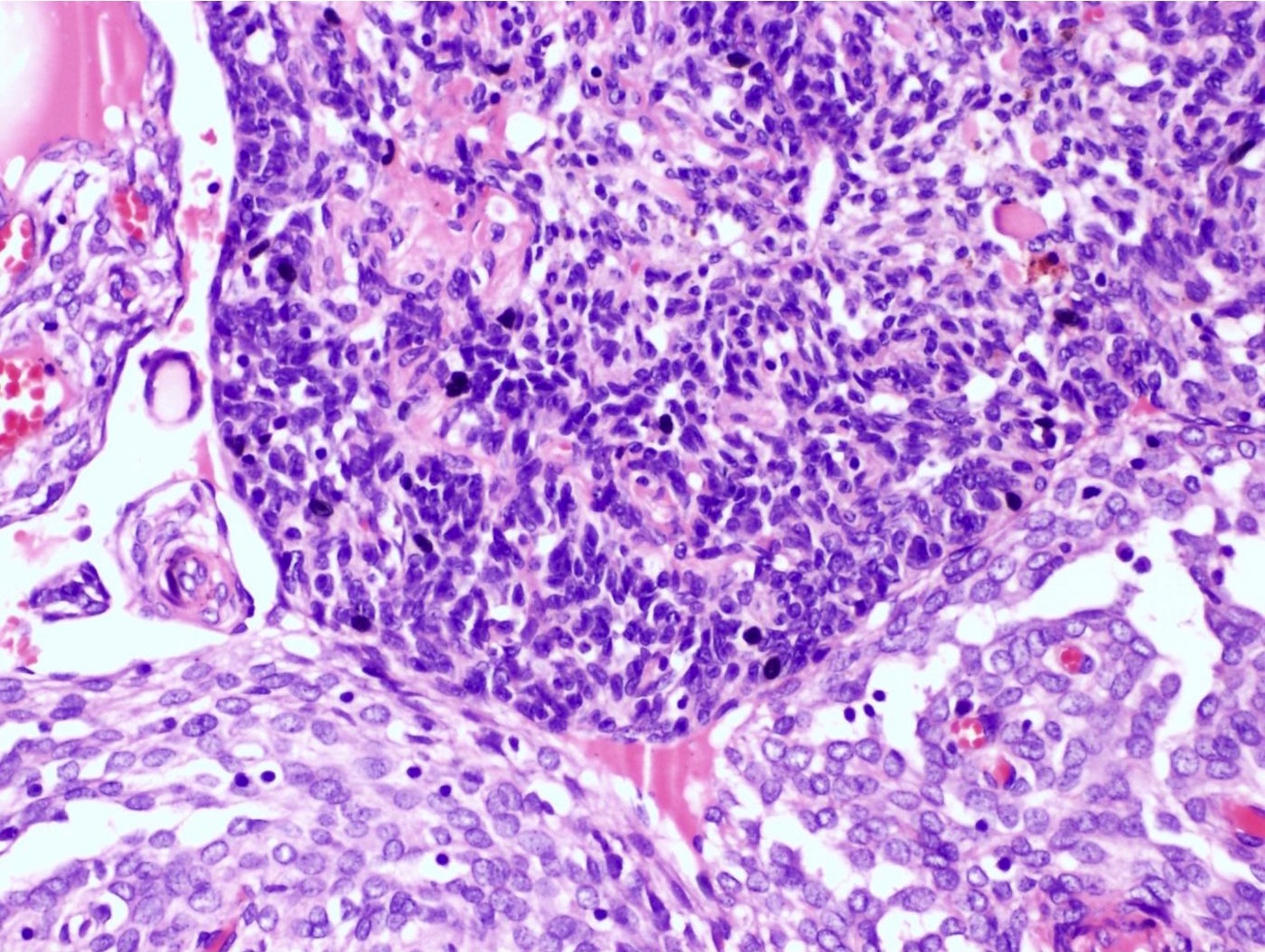
- BCOR rearranged (Mod Pathol 2018;31:674, Pathology 2018;50:162):
- Often involves endometrium and myometrium
- Tongue-like invasion or broad front with infiltrative borders
- Haphazard fascicles of uniformly atypical spindle cells with scant to moderate and eosinophilic or abundant and blue-gray cytoplasm
- Extensive myxoid stroma
- Collagen plaques in ~50%
- Brisk mitoses (≥ 10/10 high power fields)
- Small arterioles without perivascular whorling of tumor cells
- Lymphovascular invasion in ~50%
- Infarct type necrosis more common than tumor cell necrosis
- Overt nuclear pleomorphism rare
- No low grade component present
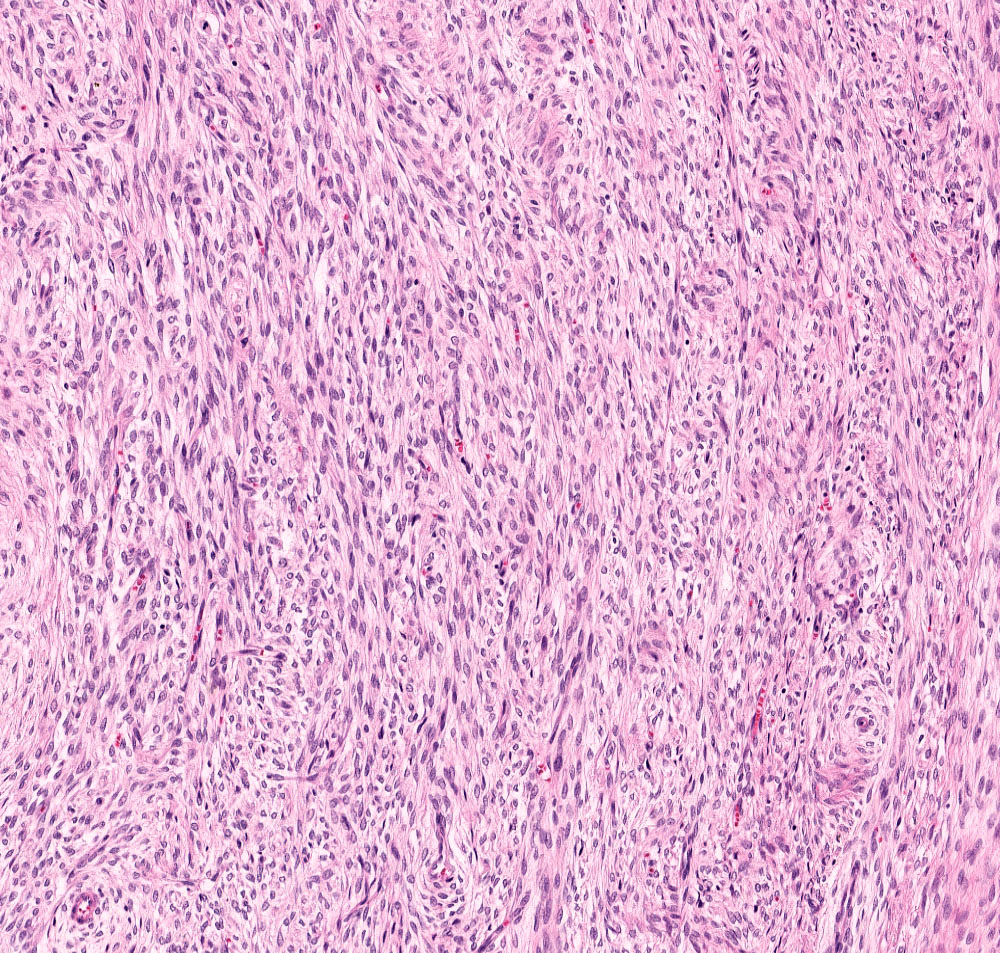
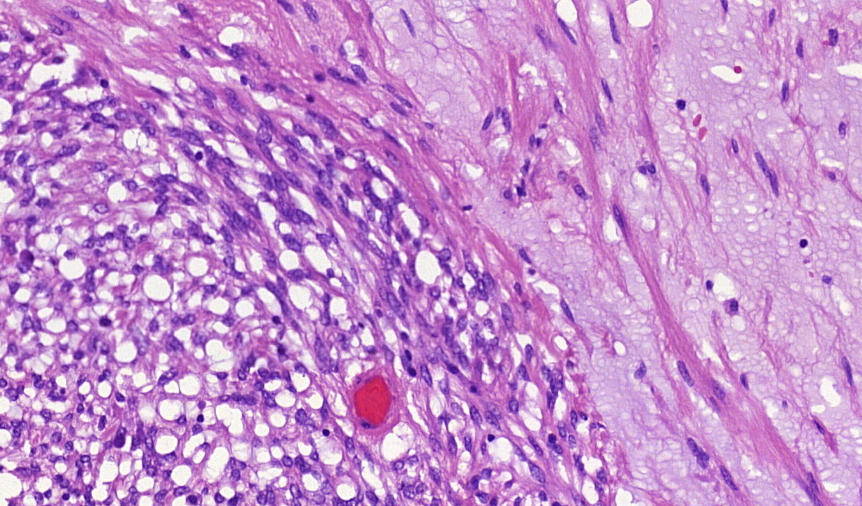
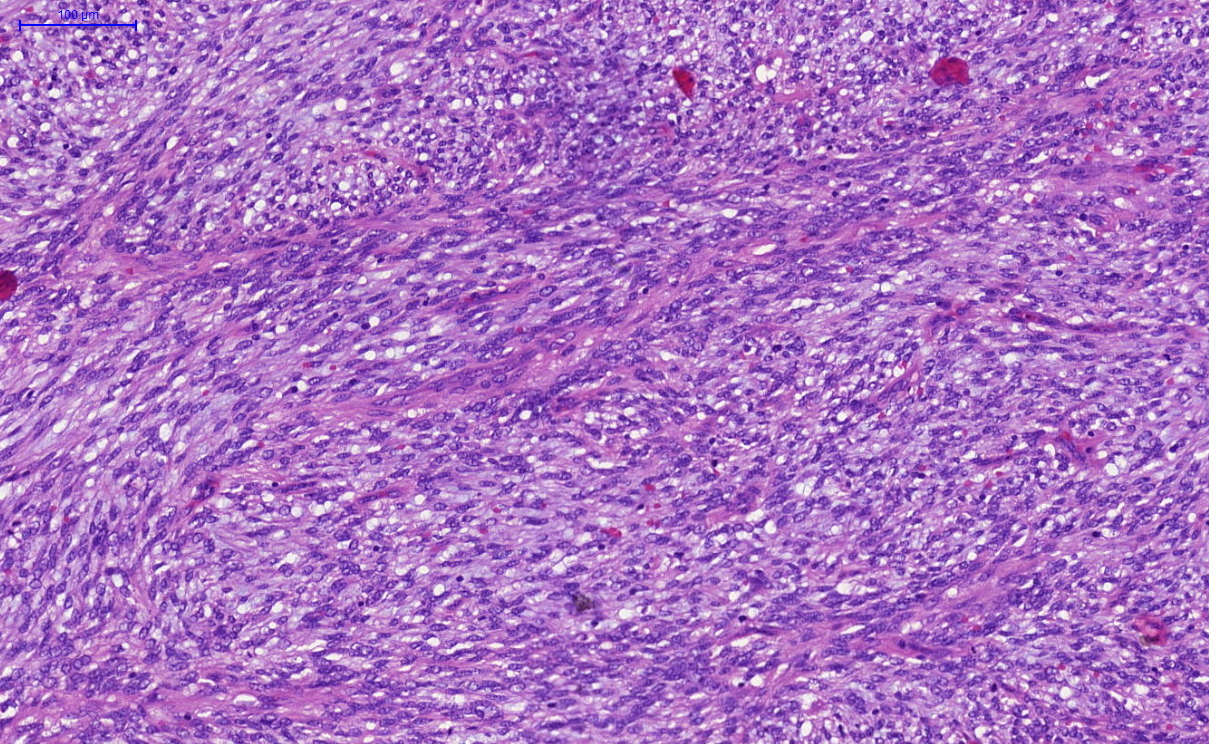
- BCOR ITD (Mod Pathol 2017;30:1251, Am J Surg Pathol 2018;42:335, Oncology 2019;96:101, Am J Surg Pathol 2019;43:662):
- Tongue-like invasion
- High grade round cell component with uniform atypia, high grade spindle cell component with uniform atypia, low grade fibromyxoid spindle cell component
- Myxoid matrix
- Brisk mitoses (≥ 10/10 high power fields)
- Lymphovascular invasion and tumor cell necrosis
- Overt nuclear pleomorphism rare
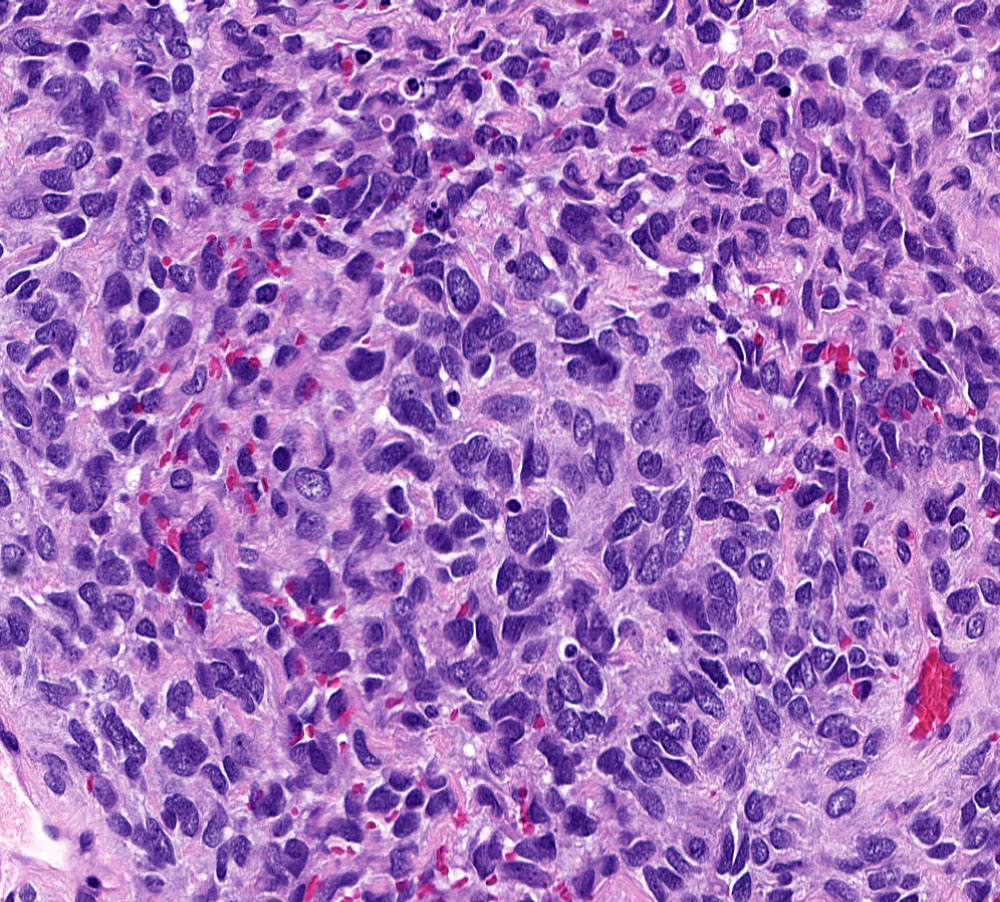
- High grade transformation of low grade endometrial stromal sarcoma (Mod Pathol 2020;33:1861):
- High grade transformation may occur in the primary, metastatic or recurrent tumor
- High grade component usually easily recognized from low grade component on low power magnification but occasionally is a gradual transition
- High grade component:
- Comprises 10 - 90% of tumor
- Sharply demarcated nodules often associated with sclerotic or less commonly myxoid stroma
- Rounded epithelioid cells with increased atypia (often uniform) and brisk mitoses (median, 16/10 high power fields)
- Delicate vasculature without perivascular tumor cell whorls
- Tumor cell necrosis uncommon
- Low grade component:
- Conventional low grade endometrial stromal sarcoma
- May show variant morphology (fibroblastic, smooth muscle differentiation, myxoid matrix, sex cord-like differentiation)
Microscopic (histologic) images
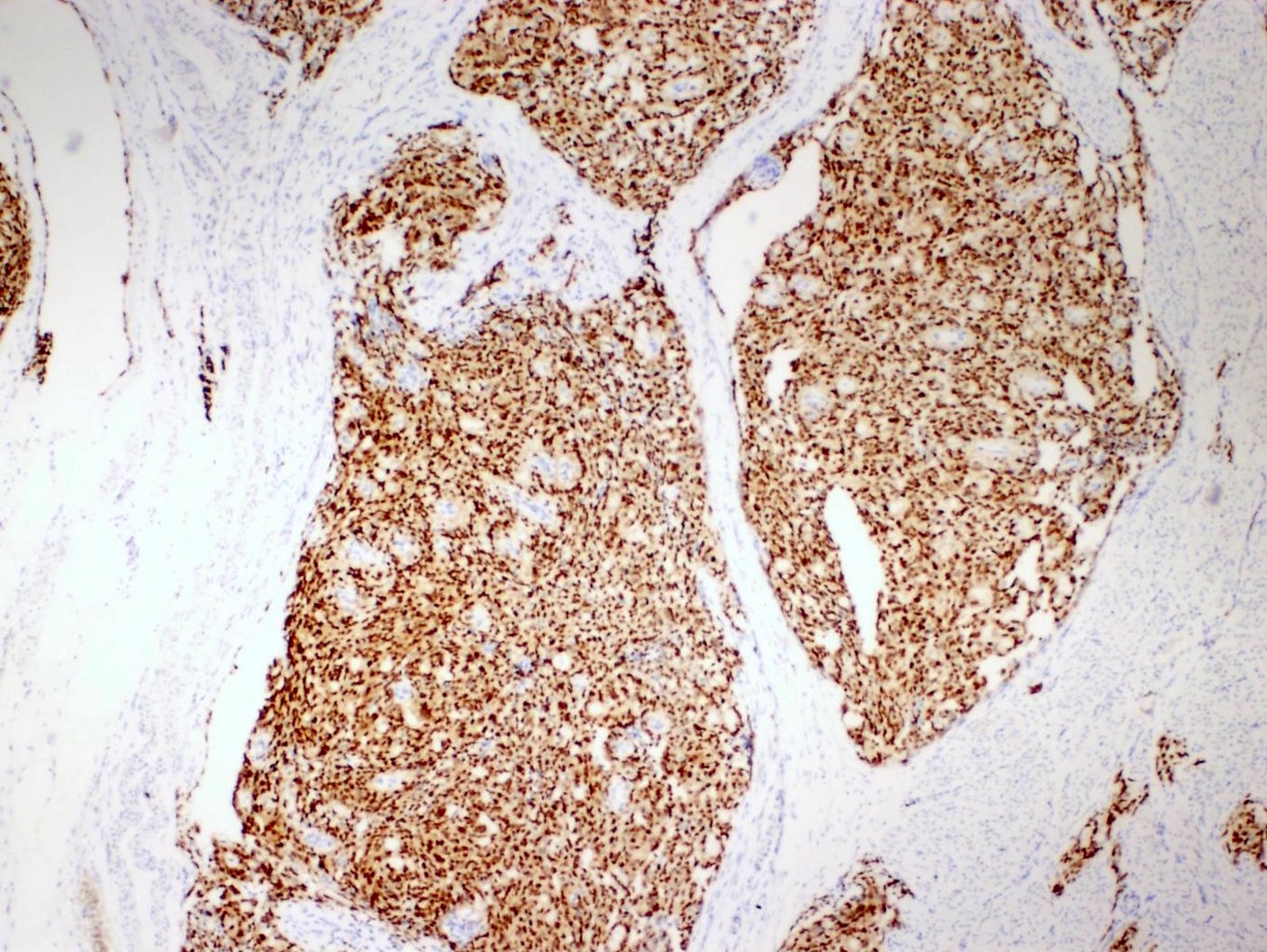
Contributed by Elizabeth Kertowidjojo, M.D., Ph.D., M.P.H., Jennifer A. Bennett, M.D., Ondrej Ondič, M.D., Ph.D. and Ayse Ayhan, M.D., Ph.D.
Virtual slides
Positive stains
- YWHAE::NUTM2A/B fusions (Pathology 2018;50:162, Int J Gynecol Pathol 2019;38:528):
- High grade component:
- Cyclin D1 (> 70% of cells)
- BCOR
- CD117 / KIT
- Pan-TRK (Mod Pathol 2021;34:1008)
- CD56
- CD99
- Low grade component:
- High grade component:
- BCOR rearranged (Mod Pathol 2018;31:674):
- CD10
- Cyclin D1 (> 70% of cells)
- Pan-TRK (Mod Pathol 2021;34:1008)
- BCOR (~50%)
- BCOR ITD (Am J Surg Pathol 2018;42:335, Am J Surg Pathol 2019;43:662, Histopathology 2020;76:64):
- BCOR (both high and low grade components)
- Cyclin D1 (both high and low grade components)
- Pan-TRK (Mod Pathol 2021;34:1008)
- High grade transformation of low grade endometrial stromal sarcoma (Mod Pathol 2020;33:1861):
Negative stains
- YWHAE::NUTM2A/B fusions (Pathology 2018;50:162):
- BCOR rearranged (Mod Pathol 2018;31:674, Histopathology 2020;76:64):
- BCOR ITD (Am J Surg Pathol 2018;42:335, Am J Surg Pathol 2019;43:662):
- High grade transformation of low grade endometrial stromal sarcoma (Mod Pathol 2020;33:1861):
Molecular / cytogenetics description
- YWHAE::NUTM2A/B fusions (Proc Natl Acad Sci U S A 2012;109:929, Mod Pathol 2013;26:1390):
- t(10;17)(q22;p13)
- Produces the 14-3-3 oncoprotein
- BCOR rearranged (Am J Surg Pathol 2017;41:12, Gynecol Oncol 2020;157:357, J Pathol Clin Res 2020;6:178):
- ZC3H7B is most common gene partner; t(X;22)(p11;q13)
- Less frequent partners include L3MBTL2, EP300, NUTM2G, RALGPS1, MAP7D2, RGAG1, ING3, NUGGC, KMT2D, CREBBP
- MDM2 amplification (45 - 100%)
- FRS2 amplification (40%)
- CDK4 amplification (38 - 60%)
- Homozygous deletion of CDKN2A (20 - 28%) and CDKN2B (18%)
- ZC3H7B is most common gene partner; t(X;22)(p11;q13)
- BCOR ITD (Am J Surg Pathol 2018;42:335, Oncology 2019;96:101, Gynecol Oncol 2020;157:357):
- Internal tandem duplications of different lengths involving exon 15
- CDKN2A / 2B homozygous deletion (20%)
- No MDM2 or CDK4 amplifications
- High grade transformation of low grade endometrial stromal sarcoma (Mod Pathol 2020;33:1861):
- JAZF1::SUZ12 fusions most common
- Rarely or JAZF1::PHF1, EPC1::PHF1 or BRD8::PHF1 fusions
- No YWHAE and BCOR alterations
Sample pathology report
- Uterus, fallopian tubes and ovaries, hysterectomy and bilateral salpingo-oophorectomy:
- ZC3H7B::BCOR rearranged high grade endometrial stromal sarcoma (14 cm) (see comment and synoptic report)
- Comment: The tumor shows tongue-like myometrial invasion and is composed of enlarged, hyperchromatic spindle cells percolating within a myxoid stroma. Mitoses number up to 15 per 10 high power fields. It is positive for BCOR, cyclin D1 and CD10 but negative for desmin, caldesmon and SMA. Molecular testing confirmed a ZC3H7B::BCOR fusion.
Differential diagnosis
- YWHAE::NUTM2A/B high grade endometrial stromal sarcoma:
- Undifferentiated carcinoma (Semin Diagn Pathol 2020 Nov 27 [Epub ahead of print]):
- Sheets of noncohesive round and monomorphic cells lacking epithelial differentiation
- Large areas of geographic necrosis and lymphovascular invasion
- Rhabdoid cells in ~25%
- Small foci of overt pleomorphism in 20%
- Often positive, at least focally, for cytokeratins (AE1 / AE3, CAM5.2, CK8/18) and EMA
- Subset are positive for synaptophysin, chromogranin or CD56
- May show mismatch repair protein (50%) or SWI / SNF protein (70%) deficiency
- Molecular alterations common to endometrial carcinomas (PTEN, PIK3CA, CTNNB1, TP53)
- Undifferentiated carcinoma (Semin Diagn Pathol 2020 Nov 27 [Epub ahead of print]):
- BCOR related high grade endometrial stromal sarcoma:
- High grade endometrial stromal sarcoma (in general):
- Low grade endometrial stromal sarcoma:
- Leiomyosarcoma (conventional / spindle cell type):
- Undifferentiated uterine sarcoma:
- Complex karyotype
- No known recurring genetic alterations
Board review style question #1
A 51 year old woman presents with vaginal bleeding. Histologic sections of the hysterectomy reveal an infiltrative spindle cell neoplasm. Immunohistochemically, the tumor is positive for CD10, cyclin D1 and BCOR but negative for smooth muscle actin, desmin and caldesmon. Next generation sequencing study reveals ZC3H7B::BCOR gene fusion. What is the correct diagnosis?
- High grade endometrial stromal sarcoma
- Inflammatory myofibroblastic tumor
- Leiomyosarcoma
- Low grade endometrial stromal sarcoma
- Undifferentiated uterine sarcoma
Board review style answer #1
A. High grade endometrial stromal sarcoma
Comment Here
Reference: High grade endometrial stromal sarcoma
Comment Here
Reference: High grade endometrial stromal sarcoma
Board review style question #2
A subclassification of high grade endometrial stromal sarcoma as per WHO 2020 is based on
- Identification of specific gene rearrangement involving YWHAE or BCOR or internal tandem duplication of BCOR gene
- Immunohistochemical coexpression of cyclin D1 and BCOR
- Immunohistochemical expression of BCOR
- Presence of myxoid stromal change
Board review style answer #2
A. Identification of specific gene rearrangement involving YWHAE or BCOR or internal tandem duplication of BCOR gene
Comment Here
Reference: High grade endometrial stromal sarcoma
Comment Here
Reference: High grade endometrial stromal sarcoma