Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagnosis | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Dasaraju S, Khalifa MA. Histology of specimens from gender affirming surgery in individuals assigned female at birth. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusfmtransgenderhistologic.html. Accessed April 23rd, 2024.
Definition / general
- Hysterectomy is part of gender affirming surgery for individuals assigned female at birth (AFAB)
- Vaginectomy is a rarely performed gender affirming surgery for individuals AFAB
- Surgery is typically performed following long periods of preoperative androgen administration
Essential features
- Cervical pathology in the form of ectocervical epithelial atrophy, often with transitional cell metaplasia, should not be mistaken for high grade dysplasia (Int J Gynecol Pathol 1997;16:89, Int J Gynecol Pathol 2019;38:520)
- Rarely, prostate type glands can be seen in the ectocervical epithelium (Histopathology 2022;80:946, Int J Gynecol Pathol 2017;36:328)
- Vaginal pathology shows epithelial atrophy, transitional cell metaplasia and prostatic metaplasia; these should not be mistaken for dysplasia or glandular proliferative abnormalities (Am J Clin Pathol 2022 Oct 7 [Epub ahead of print], Am J Surg Pathol 2020;44:1040, Arch Pathol Lab Med 2022;146:742)
- Ovaries often show large follicular cysts lined by nonluteinized granulosa cells (Int J Gynecol Pathol 2019;38:520)
- Follicular density (primordial, intermediate and primary follicular count per mm2) is higher than expected for the given age (Hormones (Athens) 2015;14:190, Int J Gynecol Pathol 2019;38:520)
ICD coding
Epidemiology
- Any age, typically 20 - 45 years old
Sites
- Uterus, cervix, vagina, ovary
Pathophysiology
- Long term androgenic medication administration
- Androgen receptor (AR) is present in endometrial cells and when activated, regulates genes involved in cytoskeletal organization and cell progression (Reprod Sci 2014;21:372)
- Ectocervical transitional cell metaplasia has been described in postmenopausal uteruses (Int J Gynecol Pathol 1997;16:89)
- Prostatic metaplasia and transitional cell metaplasia of the vagina is associated with long term androgen administration (Am J Surg Pathol 2020;44:1040)
- Abnormally high androgen levels are known to suppress normal follicular development (Hormones (Athens) 2015;14:190)
Etiology
- Histopathologic alterations seen in the uterus, vagina and ovary of individuals assigned female at birth are attributed to long term preoperative androgenic medication administration
Diagnosis
- Diagnosis is typically evident based on the information received from gynecologist (e.g., gender dysphoria)
Case reports
- 23 year old patient assigned female at birth with adrenogenital syndrome, presenting with transitional cell metaplasia and ectopic prostatic tissue in the uterine cervix and vagina (Int J Gynecol Pathol 2004;23:182)
- 3 cases of testosterone induced virilization of mesonephric duct remnants and cervical squamous epithelium in patients assigned female at birth (Int J Gynecol Pathol 2017;36:328)
- 12 patients assigned female at birth between 20 and 32 years old with uterine and ovarian changes during testosterone administration (Taiwan J Obstet Gynecol 2016;55:686)
- 13 patients assigned female at birth with prostatic metaplasia of the vagina and uterine cervix (Am J Surg Pathol 2020;44:1040)
- 27 patients assigned female at birth between 20 and 46 years old with histologic features of hysterectomy specimens (Int J Gynecol Pathol 2019;38:520)
- 55 patients assigned female at birth between 18 and 56 years old with histologic features of hysterectomy specimens (Arch Pathol Lab Med 2022;146:742)
Gross description
- Typically, gross appearance is unremarkable
Microscopic (histologic) description
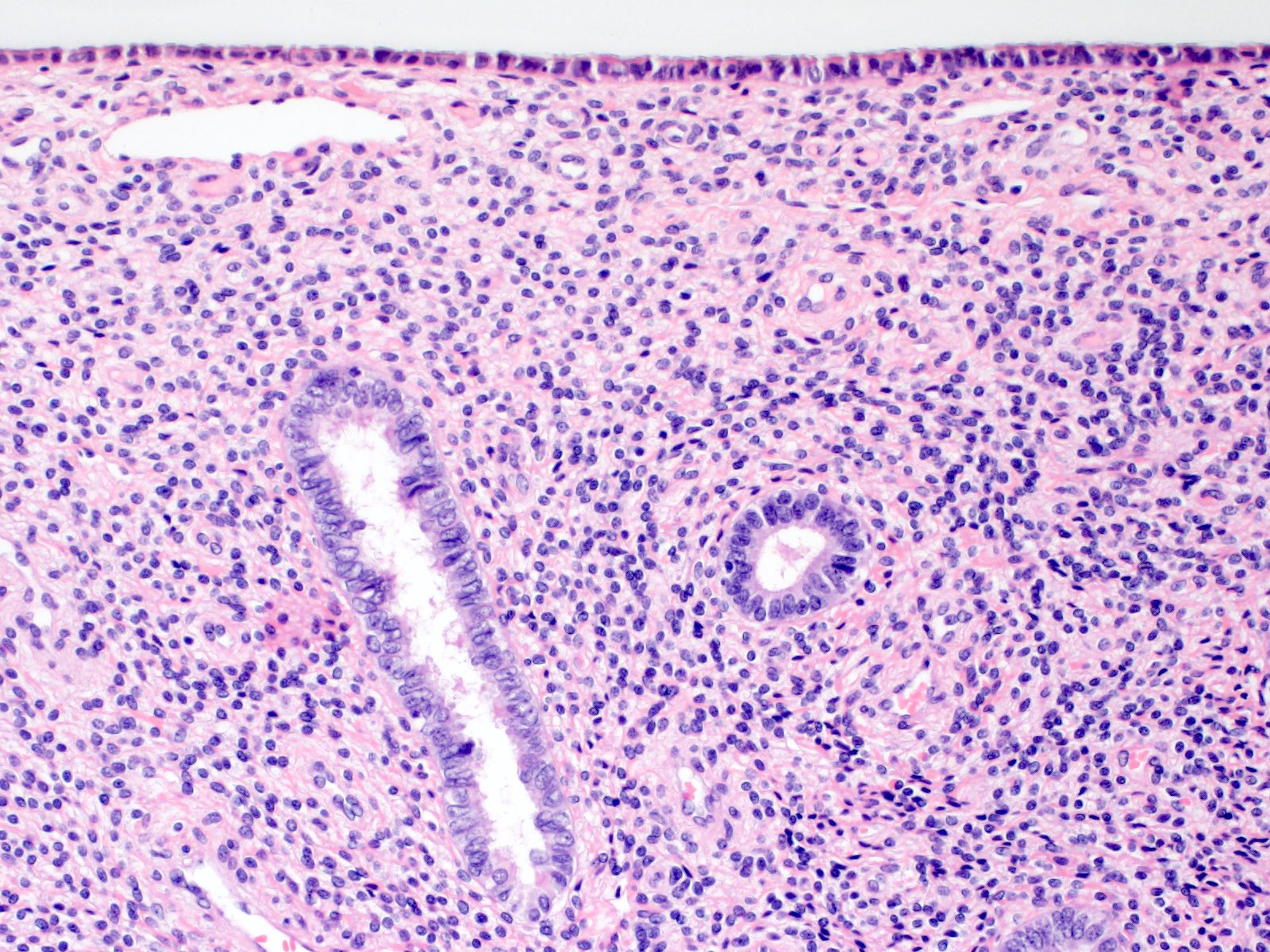
- Expanded endometrial stromal areas with decidua-like changes with or without glandular paucity (Reprod Sci 2014;21:372, Hum Reprod 1992;7:1461, Int J Gynecol Pathol 2019;38:520)
- Ectocervical epithelial atrophy, often with transitional cell metaplasia (Arch Pathol Lab Med 2022;146:742, Surg Pathol Clin 2022;15:421, Int J Gynecol Pathol 1997;16:89, Int J Gynecol Pathol 2019;38:520)
- Umbrella-like cells could be seen on the surface
- Nuclei often show nuclear grooves
- Koilocytotic atypia (with perinuclear halos) and viral cytopathic changes are distinctly absent
- Rarely, prostate type glands can be seen in the ectocervical epithelium (Histopathology 2022;80:946, Int J Gynecol Pathol 2017;36:328)
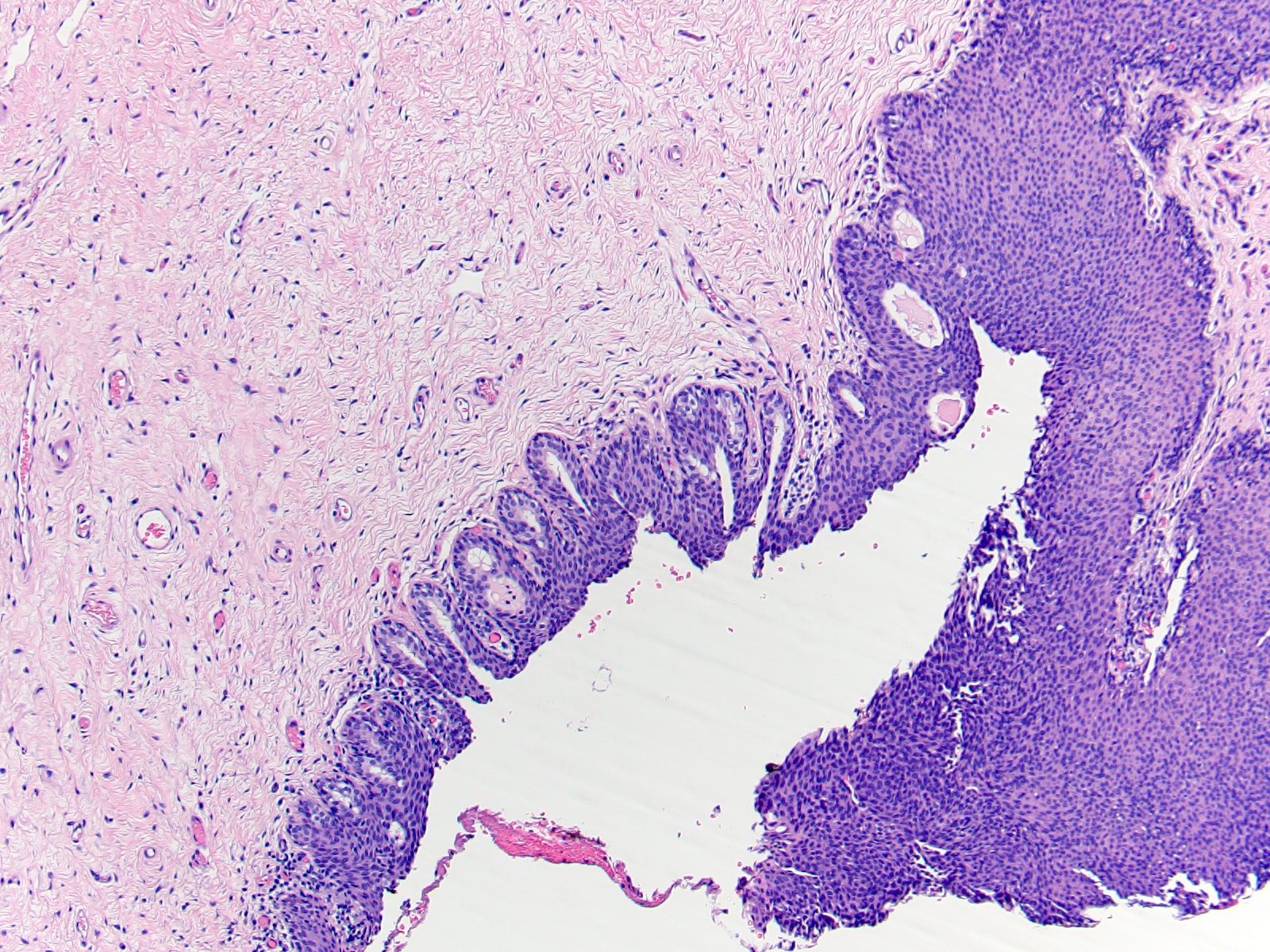
- Vaginal epithelial atrophy, transitional cell metaplasia and prostatic metaplasia (Int J Gynecol Pathol 2004;23:182, Am J Surg Pathol 2020;44:1040)
- Large ovarian cortical follicular cysts lined by nonluteinized granulosa cells (Int J Gynecol Pathol 2019;38:520)
- Follicular density (primordial, intermediate and primary follicular count per mm2) is higher than expected for the given age (Hormones (Athens) 2015;14:190, Int J Gynecol Pathol 2019;38:520)
- Rarely, periadnexal virilized mesonephric duct remnants (Int J Gynecol Pathol 2017;36:328)
Microscopic (histologic) images
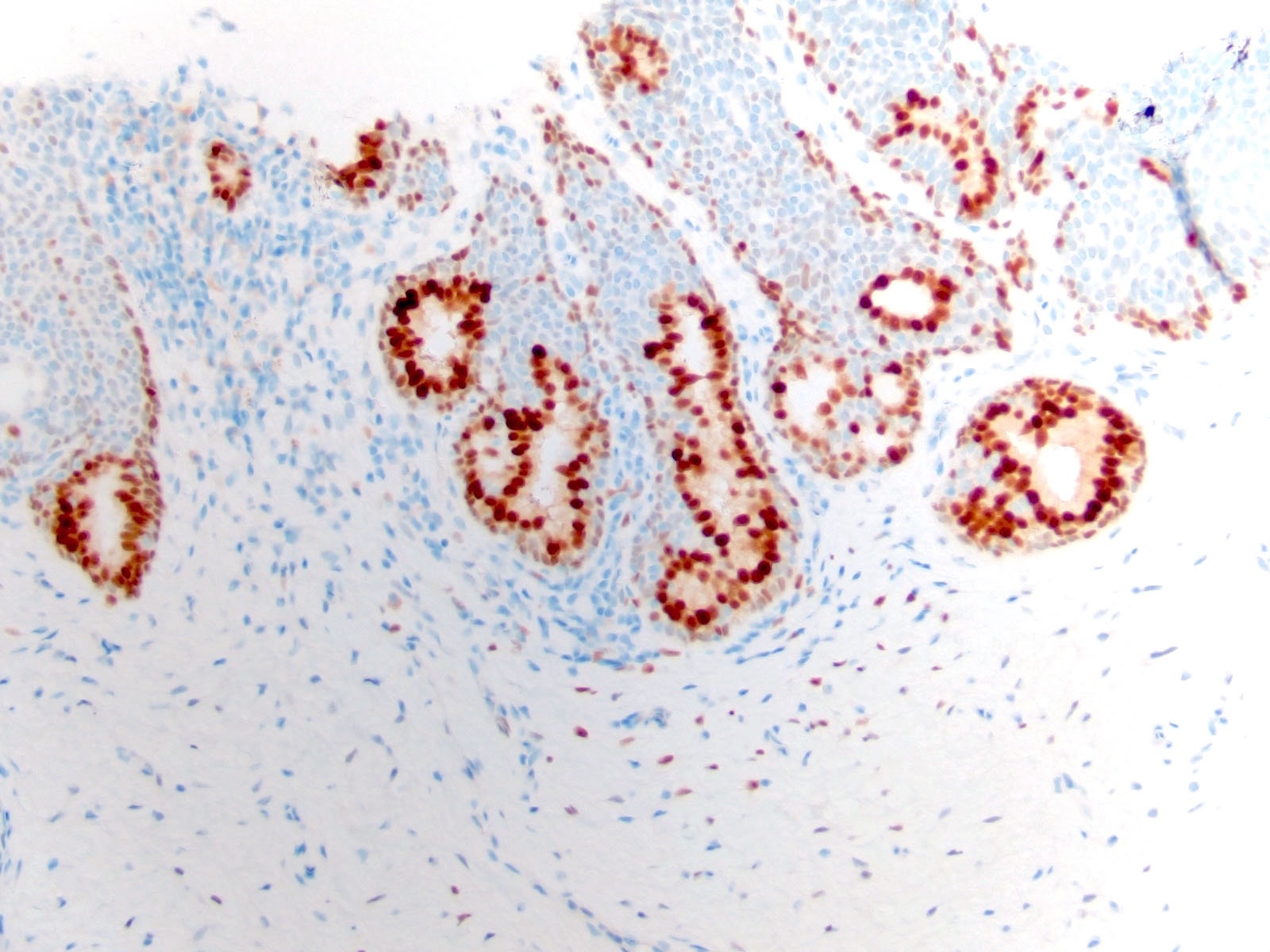
Positive stains
Negative stains
- p16 immunostaining in the cervix is negative and is used to distinguish transitional cell metaplasia from high grade squamous intraepithelial lesion
Sample pathology report
- Uterus, fallopian tubes and ovaries, hysterectomy with bilateral salpingo-oophorectomy:
- Inactive / atrophic endometrium with areas of focal decidualization and gland paucity
- Myometrium with no significant histologic abnormality
- Cervix with transitional cell metaplasia of ectocervix
- Ovaries with follicular cysts; follicular density is higher than expected for the patient's age
- Vagina, vaginectomy:
- Vaginal tissue with epithelial atrophy with focal transitional cell metaplasia and prostate-like glands / prostatic metaplasia
Differential diagnosis
- High grade squamous intraepithelial lesion (HSIL):
- Loss of polarity, cytologic atypia and mitotic figures
- Immature cells with high N:C ratio, irregular nuclear contour and coarse chromatin
- Superficial cells may show koilocytotic atypia and viral cytopathic changes
- p16 immunohistochemical staining shows diffuse and strong nuclear and cytoplasmic staining
Additional references
Board review style question #1
In a hysterectomy from a 27 year old individual with gender dysphoria, the cervical section exhibited the area depicted in the photomicrograph above. Which of the following is true about this field?
- Lack of epithelial maturation is consistent with high grade squamous intraepithelial lesion
- Occasional nuclear grooves and the presence of umbrella-like cells are interpreted as transitional cell metaplasia
- p16 immunohistochemistry will not be of value in this case since it is not reliable in cases of low grade squamous intraepithelial lesions
- Plump nuclei and prominent nucleoli suggest reactive inflammatory atypia and regeneration
- The presence of occasional perinuclear halos is in keeping with human papillomavirus infection
Board review style answer #1
B. Occasional nuclear grooves and the presence of umbrella-like cells are interpreted as transitional cell metaplasia
Comment Here
Reference: Histology of specimens from gender affirming surgery in individuals assigned female at birth
Comment Here
Reference: Histology of specimens from gender affirming surgery in individuals assigned female at birth
Board review style question #2
Which of the following is a known outcome of long term administration of androgen to a young individual who was assigned female at birth?
- Atypical endometrial hyperplasia
- Endocervical polyp
- Follicular cysts of the ovary
- Leiomyomata
- Serous carcinoma of the uterus
Board review style answer #2
C. Follicular cysts of the ovary
Comment Here
Reference: Histology of specimens from gender affirming surgery in individuals assigned female at birth
Comment Here
Reference: Histology of specimens from gender affirming surgery in individuals assigned female at birth
Board review style question #3
Which epithelial change is often encountered in transgender vaginectomy specimens?
- Endometriosis
- Mucinous metaplasia
- Prostatic metaplasia
- Tubal metaplasia
- Vaginal adenosis
Board review style answer #3
C. Prostatic metaplasia
Comment Here
Reference: Histology of specimens from gender affirming surgery in individuals assigned female at birth
Comment Here
Reference: Histology of specimens from gender affirming surgery in individuals assigned female at birth