Table of Contents
Definition / general | Essential features | Terminology | Physiology / embryology | Diagrams / tables | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Videos | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Srivastava P, Lanjewar S. Anatomy & histology - vulva, vagina & female urethra. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvaanatomy.html. Accessed September 15th, 2025.
Definition / general
- Vulva constitutes the portion of female genitalia that is external to the hymen
- Vagina is a fibromuscular tube that extends from the vestibule of vulva to uterine cervix
- Female urethra extends from the bladder to midurethra and exits the body between clitoris and vagina
Essential features
- Vulva is composed of mons pubis, clitoris, labia minora, labia majora, vulvar vestibule, vestibulovaginal bulbs, urethral meatus, hymen, Bartholin and Skene glands and ducts, vaginal introitus
- Vagina extends from vulva to uterine cervix and is derived from paired Müllerian ducts
Terminology
- Vulva
- Lies external to hymen and is limited by mons pubis anteriorly, anus posteriorly and inguinal gluteal folds laterally
- Vagina
- Fibromuscular canal that extends from the vestibule of vulva, between labia minora, to the uterine cervix
- Wolffian (mesonephric) duct, also known as Gartner duct, runs deeply along lateral vaginal walls
- Lymphatic drainage: external iliac nodes (upper third of the vagina), the common and internal iliac nodes (middle third) and the superficial inguinal and perirectal nodes (lower third)
- Female urethra
- Fibromuscular tube that takes urine from the urinary bladder to the exterior through the external urethral meatus
Physiology / embryology
- Germ cells from yolk sac migrate to the urogenital ridge, forming the epithelium and stroma of the gonads; genital tubercle becomes the clitoris and the parallel ridges become the labia minora
- Urorectal septum divides the cloaca into the urogenital sinus and anal canal; degeneration of the central portion of the urogenital membrane forms the hymen opening
- Lateral Müllerian ducts (paramesonephric ducts) give rise to upper vagina while the lower vagina is formed by the urogenital sinus
- Vaginal vestibule develops by the joining of the distal vagina and urogenital sinus
- Originates from endoderm, except near the urethra (ectoderm)
- Vestibular line of Hart marks the boundary between these tissues
- Epithelium of female urethra is derived from endoderm of the urogenital sinus while the surrounding connective tissue and smooth muscle tissue is derived from splanchnic mesenchyme (Sadler: Langman's Medical Embryology, 15th Edition, 2023, Am J Obstet Gynecol 1976;126:769)
Gross description
- Vulva
- Mons pubis
- Anteriormost region of vulva and is anatomically located over the prominence of pubic symphysis
- Hymen
- Corresponds to the distalmost extent of vagina and posterior aspect of vulvar vestibule
- Clitoris
- Erectile tissue similar to corpora cavernosa of penis and is located anterior to frenulum at the junction of labia minora
- Labia majora
- Form the lateral boundaries of the vulva
- Fuse anteriorly into mons pubis
- Posteriorly terminate 3 - 4 cm anterior to the anus where they are united by posterior commissure or fourchette
- Labia minora
- Are medial to labia majora and lateral to vulvar vestibule
- Anteriorly, labia minora divide into 2 parts; one part passes over clitoris to form prepuce and the other joins beneath clitoris and forms frenulum
- Posteriorly, they blend with medial surfaces of labia majora
- Hart line
- Lies at the inferior junction between vulvar vestibule and perineal skin
- Vestibule
- Area between the hymen (anteriorly), Hart line (posterolaterally) and labia minora (anterolaterally)
- Includes vaginal opening and urethral orifice
- Structures found in vestibule include major vestibular (Bartholin) glands, minor vestibular glands, periurethral (Skene) glands, urethra
- Bartholin glands
- Correspond to bulbourethral glands in male
- These are mucin producing glands and are located posterolaterally in the vulva
- Minor vestibular glands
- Correspond to penile glands of Littre
- Concentrically located within the vestibule
- Mons pubis
- Vagina
- Posterior to urinary bladder (from which it is separated by fibroadipose tissue)
- Anterior to rectum (from which is separated by rectouterine space in the upper 25%, rectovaginal septum in the middle portion and sphincter musculature in the distal portion of anal canal)
- Female urethra
- Extends from the bladder to the vestibule of the vagina to its opening posterior to the clitoris
- Measures 4 cm in length
- Striated muscle of the urogenital diaphragm forms the external voluntary sphincter as the urethra penetrates it
- Reference: StatPearls: Anatomy, Abdomen and Pelvis - Female External Genitalia [Accessed 21 August 2023]
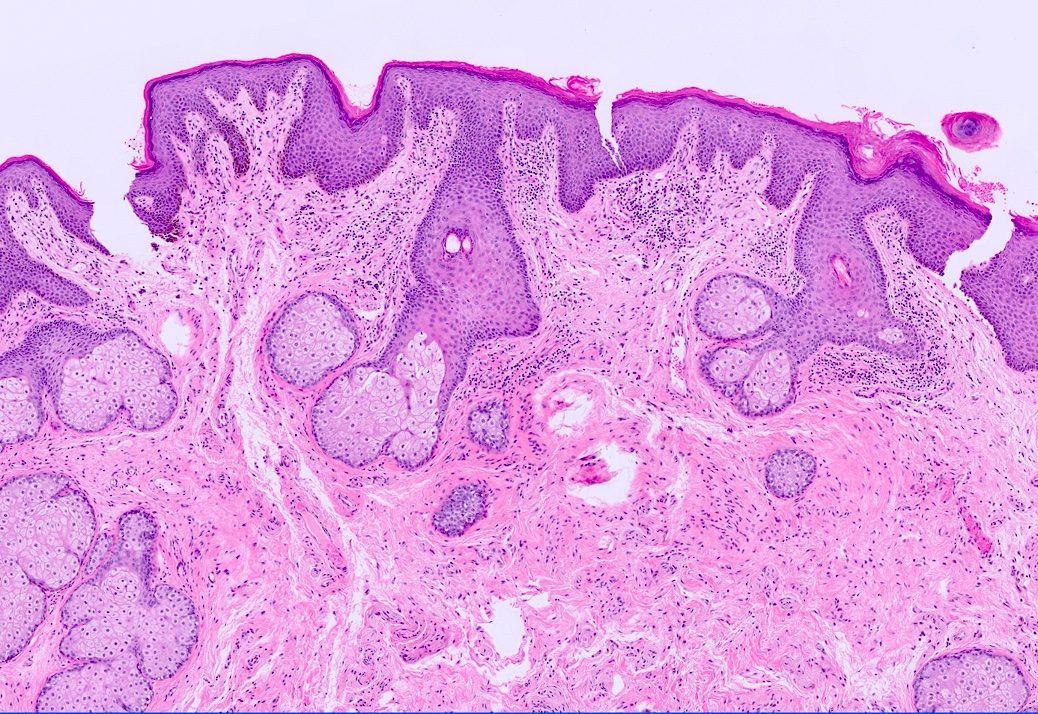
Microscopic (histologic) description
- Hymen
- Nonkeratinized stratified squamous epithelium
- Labia majora
- Composed of keratinized stratified squamous epithelium with hair follicles and eccrine, apocrine and sebaceous glands
- Labia minora
- Composed of keratinized stratified squamous epithelium, usually no adnexa
- Stroma
- Composed of stromal cells that can be spindled, stellate, fusiform and may have large multilobated nuclei
- Vestibule
- Lined by nonkeratinized squamous epithelium, may be glycogenated
- Minor vestibular gland
- Superficial glands lined by mucin secreting columnar cells that merge with squamous epithelium of the vestibule
- Open directly onto the surface
- Glands
- Apocrine glands (scent glands)
- Identical to those of axillae, breast and perianal regions
- Height of secretory cells varies
- Lumina of glands are large compared to lumina of eccrine glands
- Eccrine glands (sweat glands)
- Primarily involved in heat regulation
- Lined by layer of epithelial cells that contain eosinophilic cytoplasm
- Sebaceous glands
- Alveolar, holocrine glands that do not contain lumina
- Each gland is composed of several lobules
- Cells in each lobule form a delicate network filled with fat
- Skene glands
- Periurethral glands analogous to prostate
- Mucus secreting columnar epithelium merges with duct urothelium, then stratified squamous epithelium of vestibule
- Apocrine glands (scent glands)
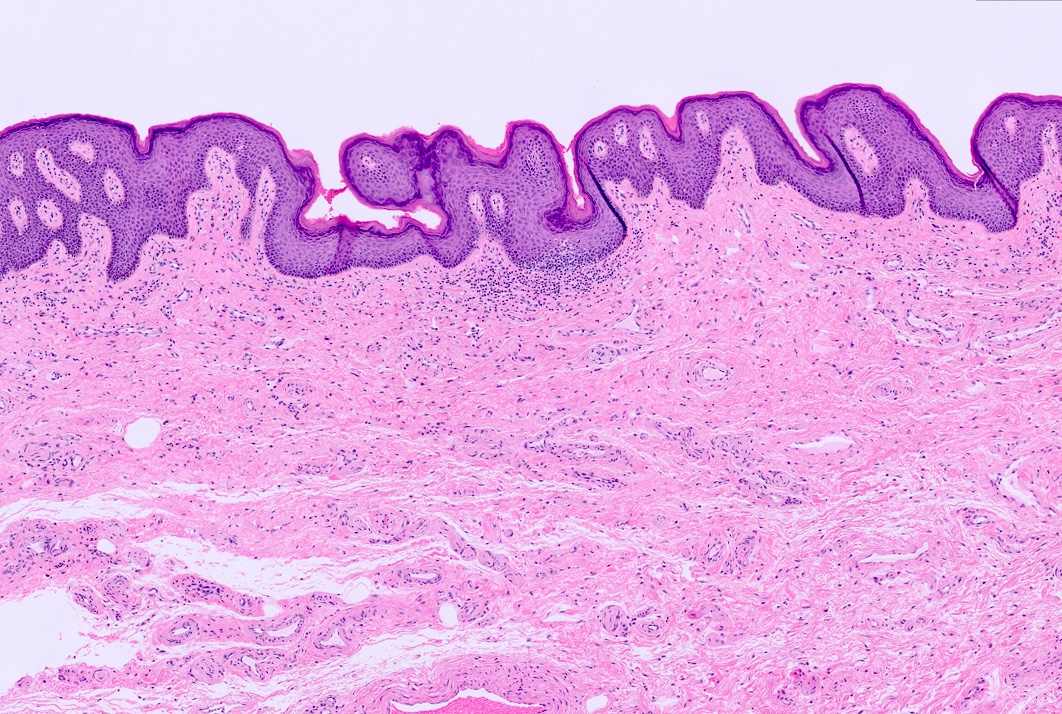
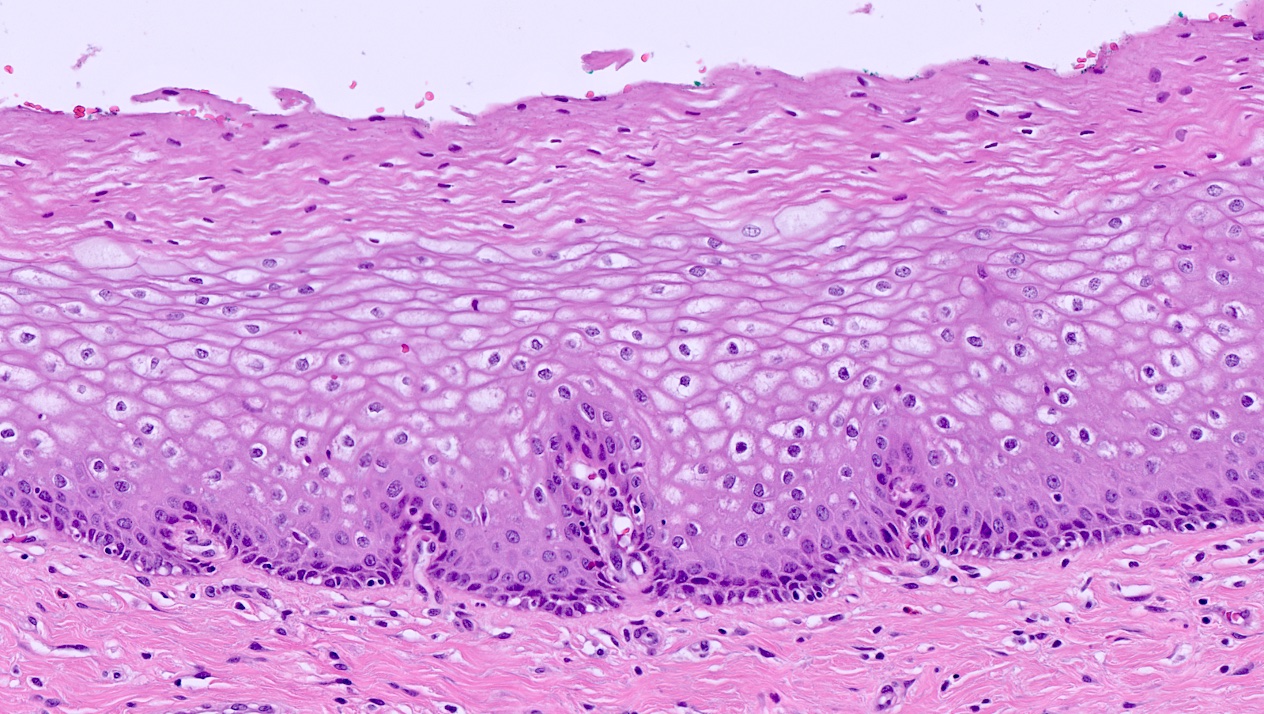
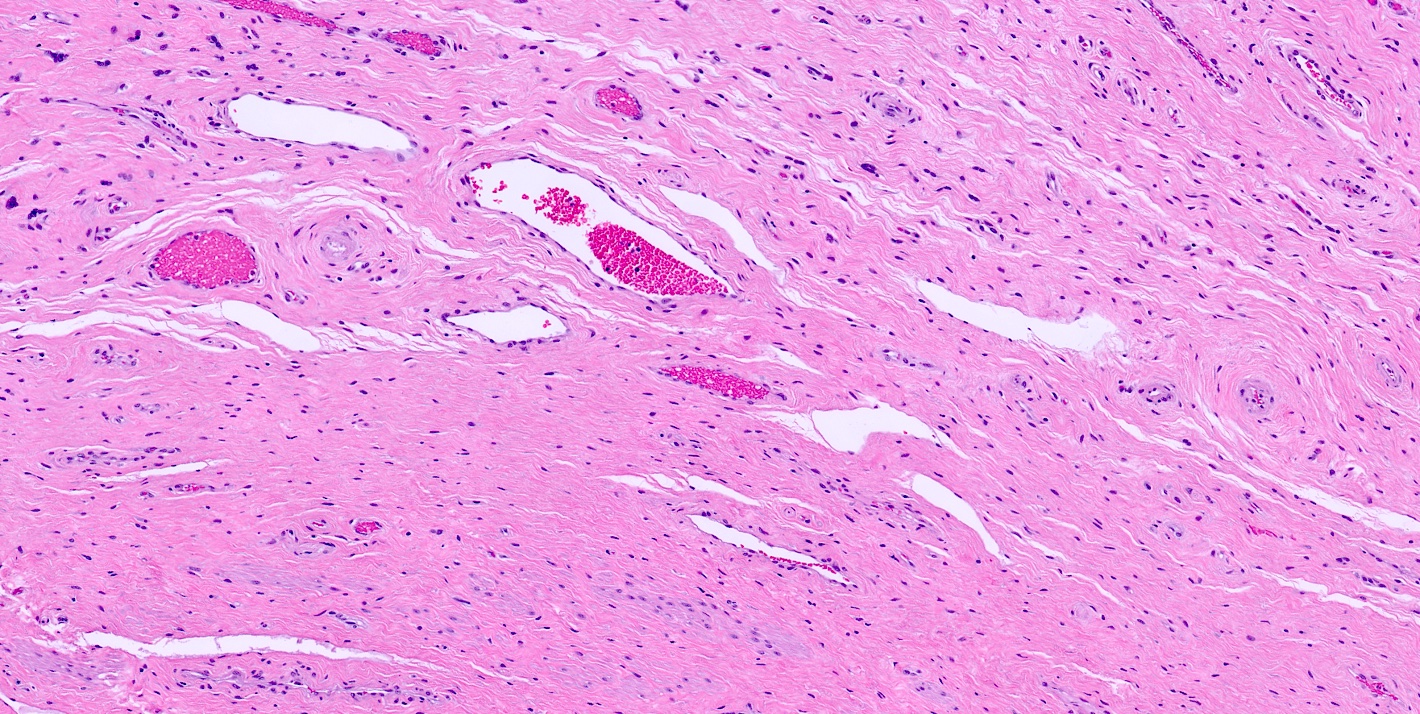
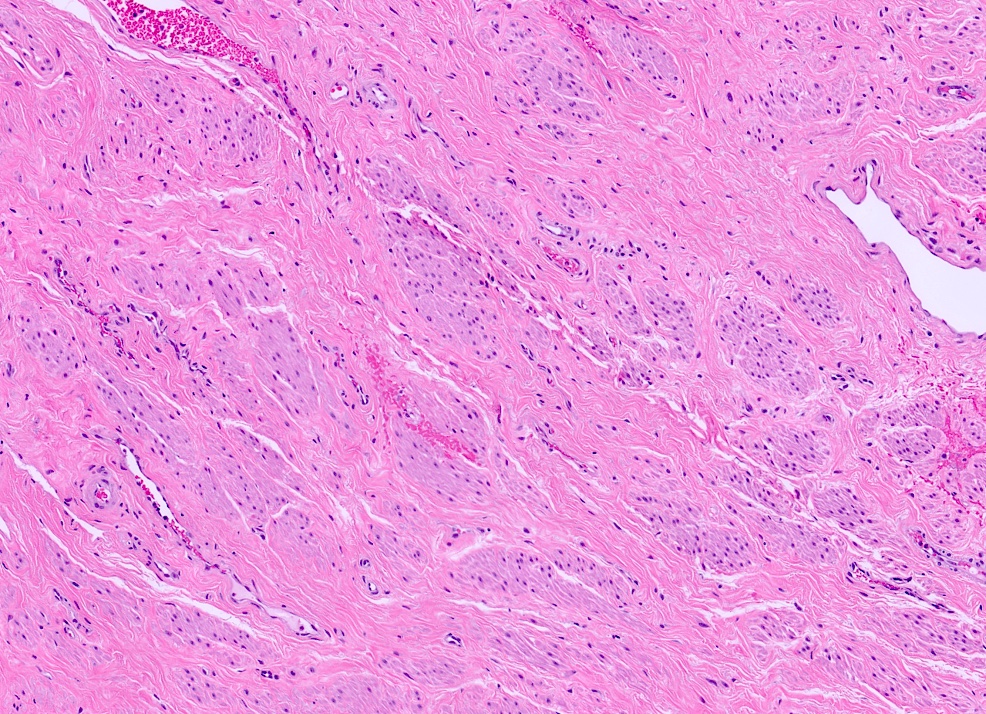
- Vagina
- Lined by nonkeratinized stratified squamous epithelium and is composed of basal, parabasal, intermediate and superficial cell layers
- Basal cell layer is composed of a single layer of columnar cells with high N:C ratio
- Parabasal layer lies above the basal layer and has cells with higher N:C ratio than the more superficial layers
- Intermediate cell layer has more abundant cytoplasm, which can be glycogenated
- Superficial cell layer appears flattened with cells showing pyknotic nuclei (J Mol Med (Berl) 2021;99:531)
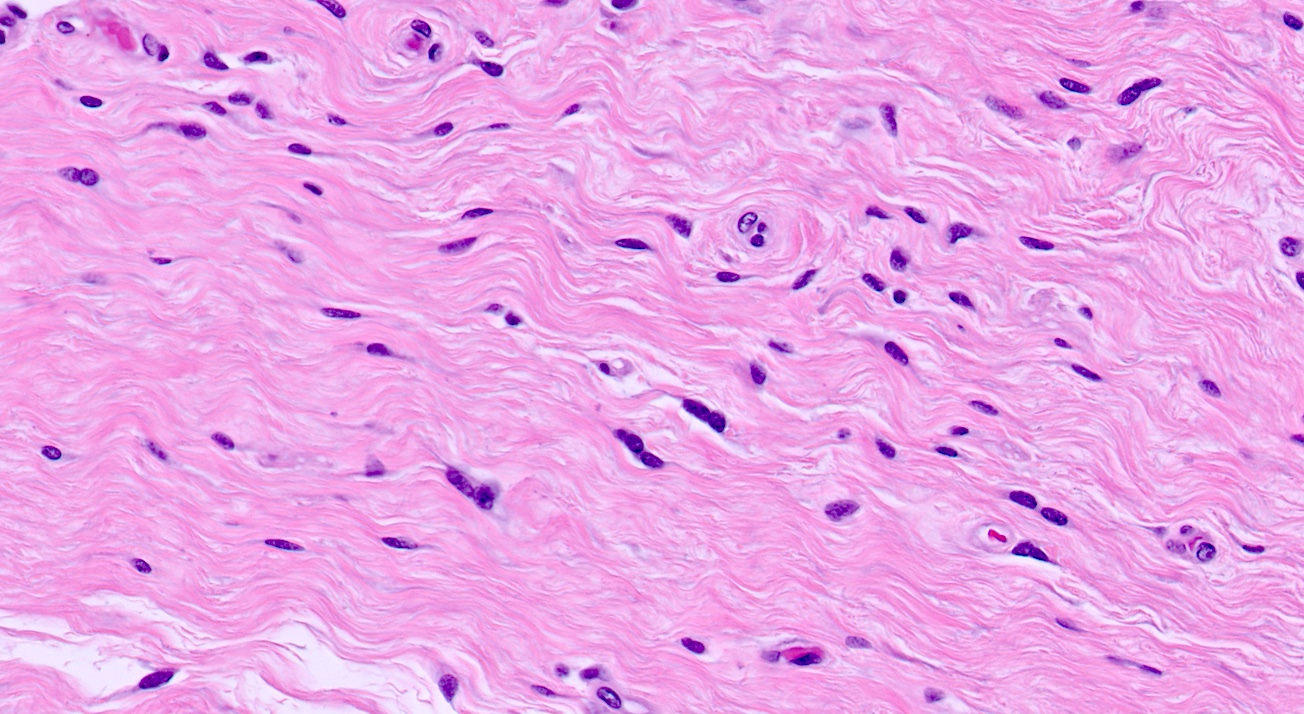
- Lamina propria (subepithelial stroma) is composed of loose connective tissue with elastic fibers, rich venous and lymphatic networks, spindle to stellate and some multinucleated stromal cells
- Muscle
- Outer longitudinal and thin inner circular layer of smooth muscle
- Adventitia is composed of inner dense connective tissue layer and outer loose connective tissue layer containing peripheral nerves, blood vessels and lymphatics
- Wolffian (mesonephric) duct, also known as Gartner duct, runs deeply along lateral vaginal walls; single small duct surrounded by a cluster of small glands lined by cuboidal epithelium with eosinophilic secretion in lumen
- Maturation index
- Ratio of parabasal to intermediate to superficial cells of vaginal epithelium (sampled at middle third of lateral vaginal wall)
- Sample is often obtained simultaneous with Pap smear to detect hormonal effects in menopausal and postmenopausal women
- Increased maturation in vaginal epithelium may be due to estrogenic effect of tamoxifen (Clin Exp Obstet Gynecol 1998;25:121)
- Lined by nonkeratinized stratified squamous epithelium and is composed of basal, parabasal, intermediate and superficial cell layers
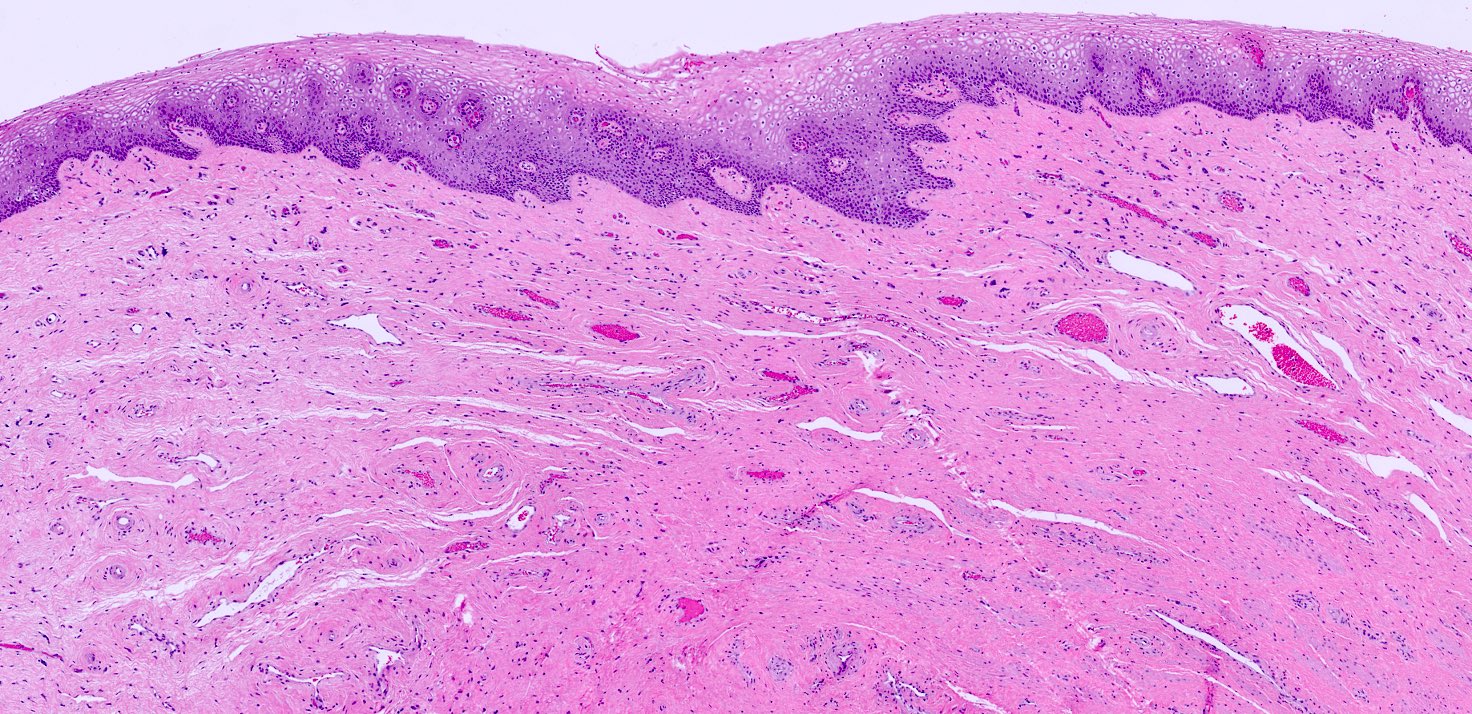
- Female urethra
- Lined by urothelium (proximal two - thirds), stratified and pseudostratified columnar and squamous epithelium (distal third)
- Basal layers composed of either low columnar or cuboidal cells, followed by several layers of polyhedral cells
- Most superficial layer is composed of round, dome shaped umbrella cells that are occasionally multinucleated and flattened according to amount of distention
- Nonkeratinized squamous epithelium: cuboidal (deepest), polymorphous (middle), squamous / flattened (superficial) (J Urol 1987;138:775)
- Periurethral (Skene) glands (homologous to the prostate gland) open into the distal portion
- Lined by columnar or cuboidal epithelium with surrounding connective tissue and smooth muscle
- Minor vestibular glands (homologous to glands of Littre in males) open along the entire length
- Tubuloacinar mucinous glands with uniform, pale eosinophilic to clear cytoplasm and basally flattened nuclei
- Lined by urothelium (proximal two - thirds), stratified and pseudostratified columnar and squamous epithelium (distal third)
Microscopic (histologic) images
Videos
Normal histology of vagina
Anatomy of female urethra
Histology of female urethra
Practice question #1
Practice answer #1
B. Labia majora. Labia majora is composed of keratinized stratified squamous epithelium with hair follicles and eccrine, apocrine and sebaceous glands. Answer A is incorrect because the ectocervix is lined by stratified squamous epithelium overlying fibrous stroma and endocervix is lined by simple, columnar mucinous epithelial cells. Answer C is incorrect because labia minora is lined by keratinized stratified squamous epithelium, without any adnexa. Answer D is incorrect because uterus is lined by endometrial glands, stroma, myometrium and serosa. Answer E is incorrect because vagina has nonkeratinized stratified squamous epithelium and is composed of basal, parabasal, intermediate and superficial cell layers.
Comment Here
Reference: Anatomy & histology - vulva, vagina & female urethra
Comment Here
Reference: Anatomy & histology - vulva, vagina & female urethra
Practice question #2
What is the epithelium of the labia minora classified as?
- Keratinized stratified squamous epithelium with adnexa
- Keratinized stratified squamous epithelium without adnexa
- Nonkeratinized stratified squamous epithelium with adnexa
- Simple, columnar mucinous epithelial cells
Practice answer #2
B. Keratinized stratified squamous epithelium without adnexa. This describes the lining of labia minora. Answer A is incorrect because it describes the lining of the labia majora. Answer C is incorrect because the epithelium of labia minora is keratinized and without adnexa. Answer D is incorrect because this describes the lining of endocervix.
Comment Here
Reference: Anatomy & histology - vulva, vagina & female urethra
Comment Here
Reference: Anatomy & histology - vulva, vagina & female urethra