Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Choschzick M. HPV independent VIN-vulva. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvadifferentiatedVIN.html. Accessed April 18th, 2024.
Definition / general
- Human papillomavirus (HPV) independent vulvar intraepithelial neoplasia is the putative precursor lesion of HPV independent vulvar squamous cell carcinoma
- Subtypes include p53 mutant differentiated vulvar intraepithelial neoplasia (dVIN) and p53 wild type lesions such as differentiated exophytic vulvar intraepithelial lesion (DEVIL) and vulvar acanthosis with altered differentiation (VAAD), recently also designated as vulvar aberrant maturation (VAM) or HPV independent, p53 wild type verruciform acanthotic vulvar intraepithelial neoplasia (Mod Pathol 2022;35:1317)
Essential features
- Highly differentiated with overlapping histological features to benign vulvar lesions
- Currently, there are no reliable immunohistochemical or molecular markers to establish the diagnosis
- HPV independent VIN can be p53 abnormal (dVIN) or p53 wild type (DEVIL, VAAD, VAM, vaVIN)
- Differentiated vulvar intraepithelial neoplasia is an aggressive lesion with higher potential to become invasive than HPV associated vulvar intraepithelial neoplasia (usual type)
Terminology
- Old: simplex vulvar intraepithelial neoplasia
ICD coding
Epidemiology
- Postmenopausal women, sixth to eighth decade; 2 - 29% of all vulvar intraepithelial neoplasia (Pathology 2016;48:291)
Sites
- Labia minora; commonly found adjacent to invasive squamous cell carcinoma (70%)
Etiology
- Background of chronic inflammatory dermatoses, lichen sclerosus, lichen simplex chronicus (J Low Genit Tract Dis 2016;20:180)
Clinical features
- Unifocal, gray-white papules or plaques
Diagnosis
- Difficult to diagnose in punch biopsies alone; overlapping histological features with other common vulvar lesions, especially lichen simplex
Prognostic factors
- More likely to progress to invasive carcinoma (32%) than usual vulvar intraepithelial neoplasia; shorter latency to become invasive (Eur J Cancer 2009;45:851, Int J Gynecol Cancer 2009;19:741)
- VAAD may be a possible precursor of verrucous carcinoma
Case reports
- 52 year old woman with progression to carcinoma (Int J Gynecol Pathol 2007;26:248)
- 6 55 - 82 year old women with dVIN in association with squamous cell carcinoma (Int J Gynecol Pathol 2008;27:125)
- 61 and 78 year old women with DEVIL, which was initially misinterpreted (J Low Genit Tract Dis 2022;26:283)
- 70 year old woman with background of lichen sclerosus (Am J Dermatopathol 2011;33:e27)
- 73 year old woman with longstanding illness and diagnosis of dVIN, VAAD and vulval carcinoma (JAAD Case Rep 2020;8:53)
- 82 year old woman with dVIN (JAAD Case Rep 2019;5:448)
- 85 year old woman with VAAD and progression to carcinoma (Int J Gynecol Pathol 2015;34:385)
Treatment
- Conservative excision, careful follow up (Best Pract Res Clin Obstet Gynaecol 2014;28:1051)
Microscopic (histologic) description
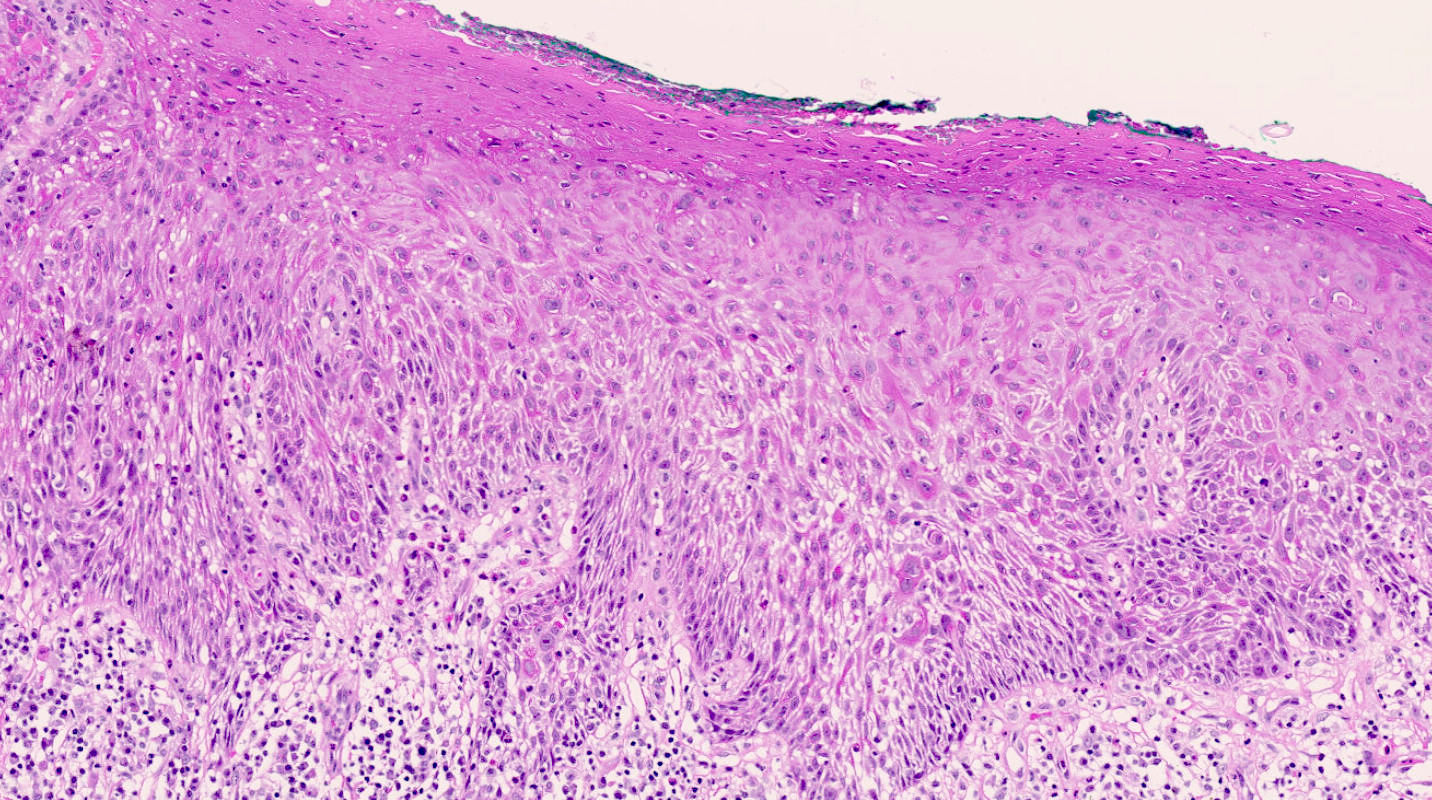
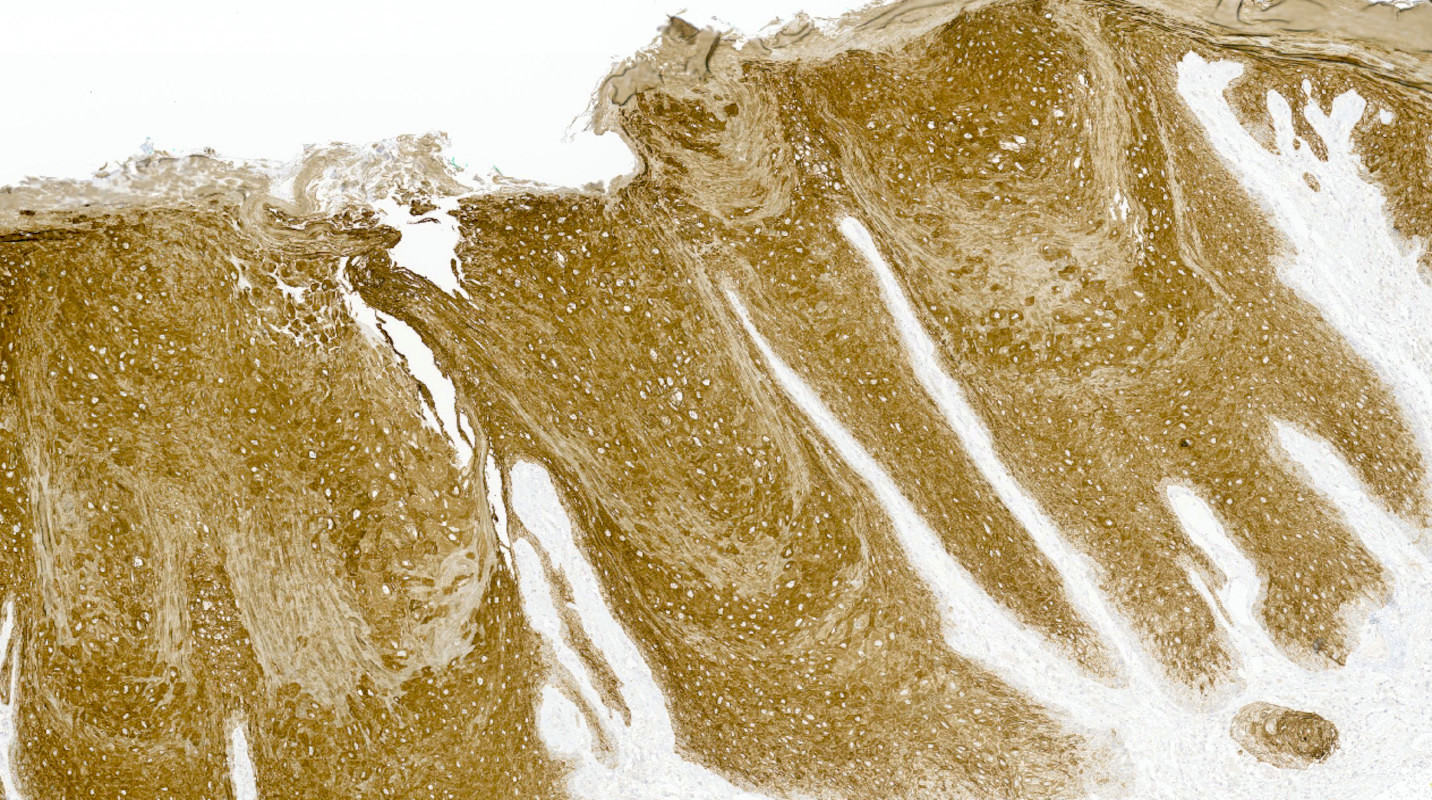
- dVIN
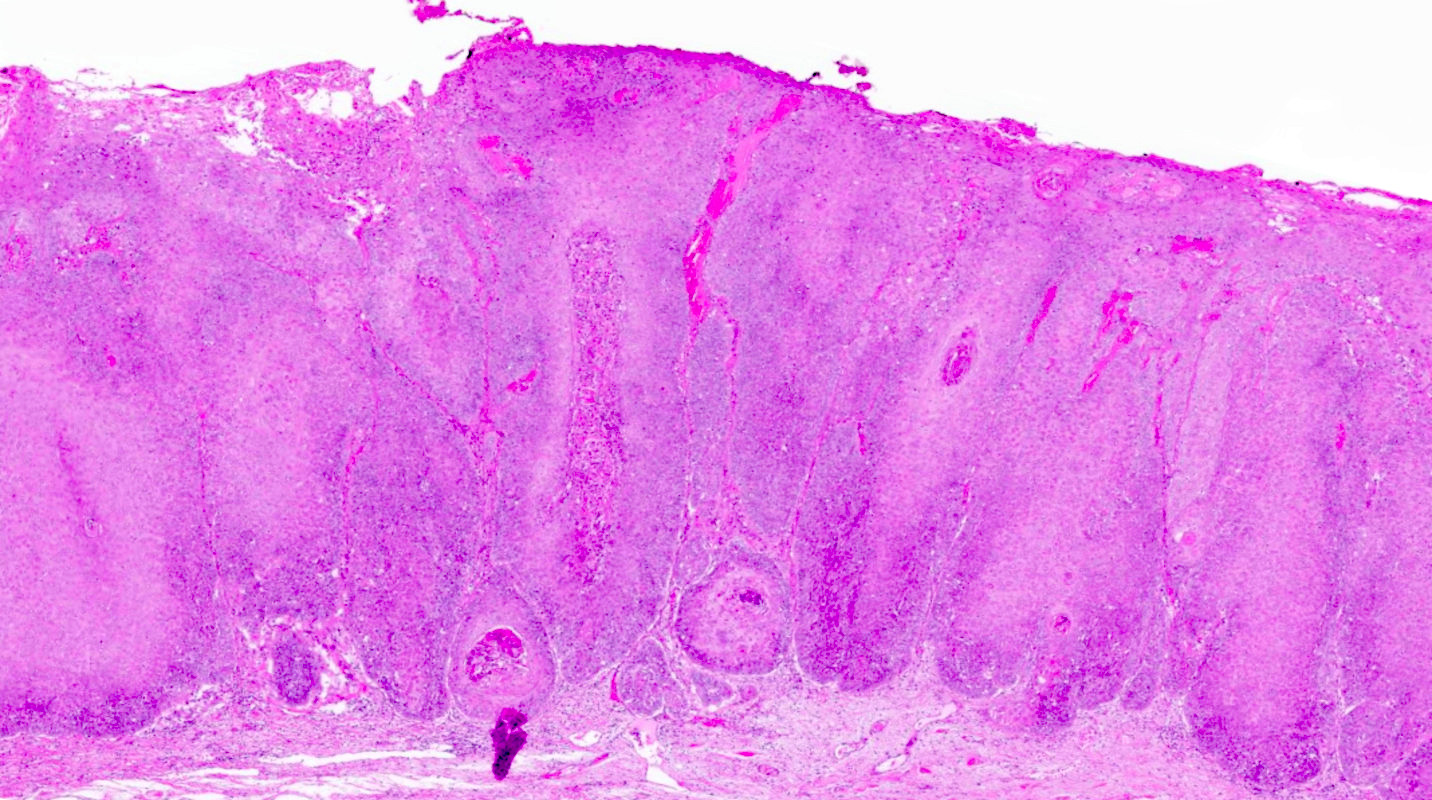
- Acanthosis, parakeratosis, elongation and anastomosis of rete ridges (Histopathology 2020;76:128, Semin Diagn Pathol 2021;38:27)
- Mild to moderate atypical cells in basal and parabasal layers with hyperchromatic nuclei; however, full thickness atypia is lacking
- Enlarged squamous cells with eosinophilic cytoplasm, vesicular nuclei and prominent nucleoli; prominent intercellular bridges
- Rare basaloid differentiation of dVIN with atypical cells in upper cell layers (Am J Surg Pathol 2009;33:1659, Am J Surg Pathol 2020;44:1506, Histopathology 2023;82:731)
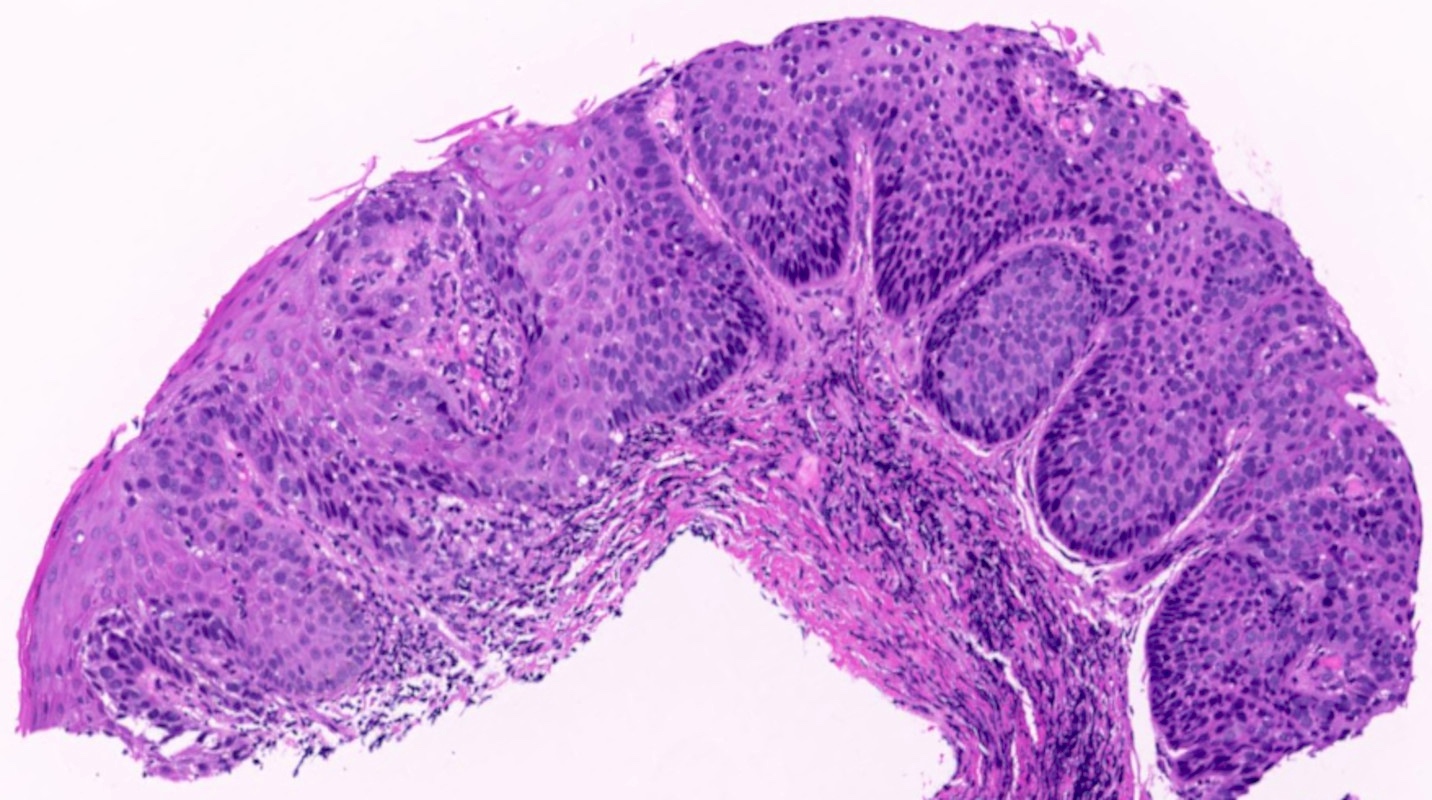
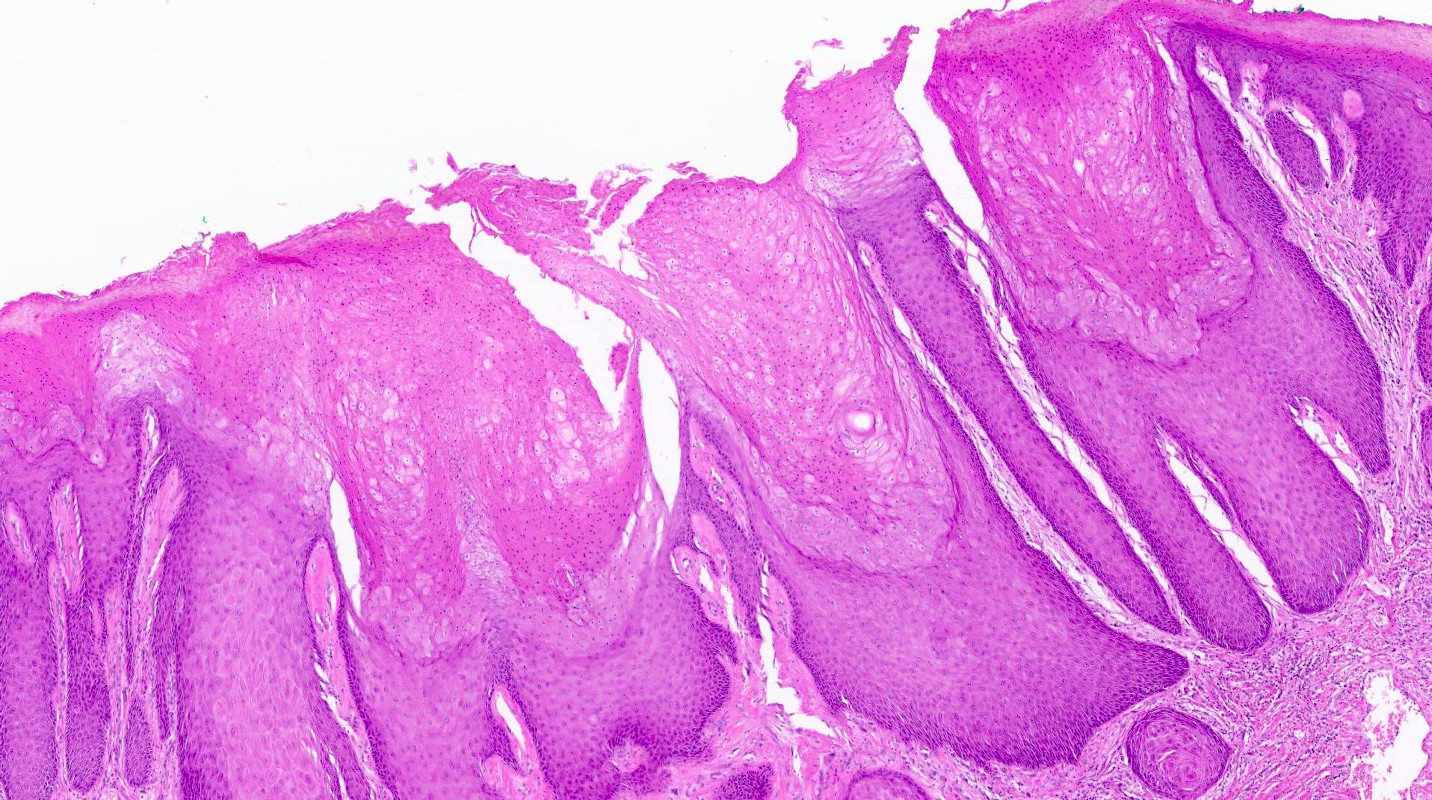
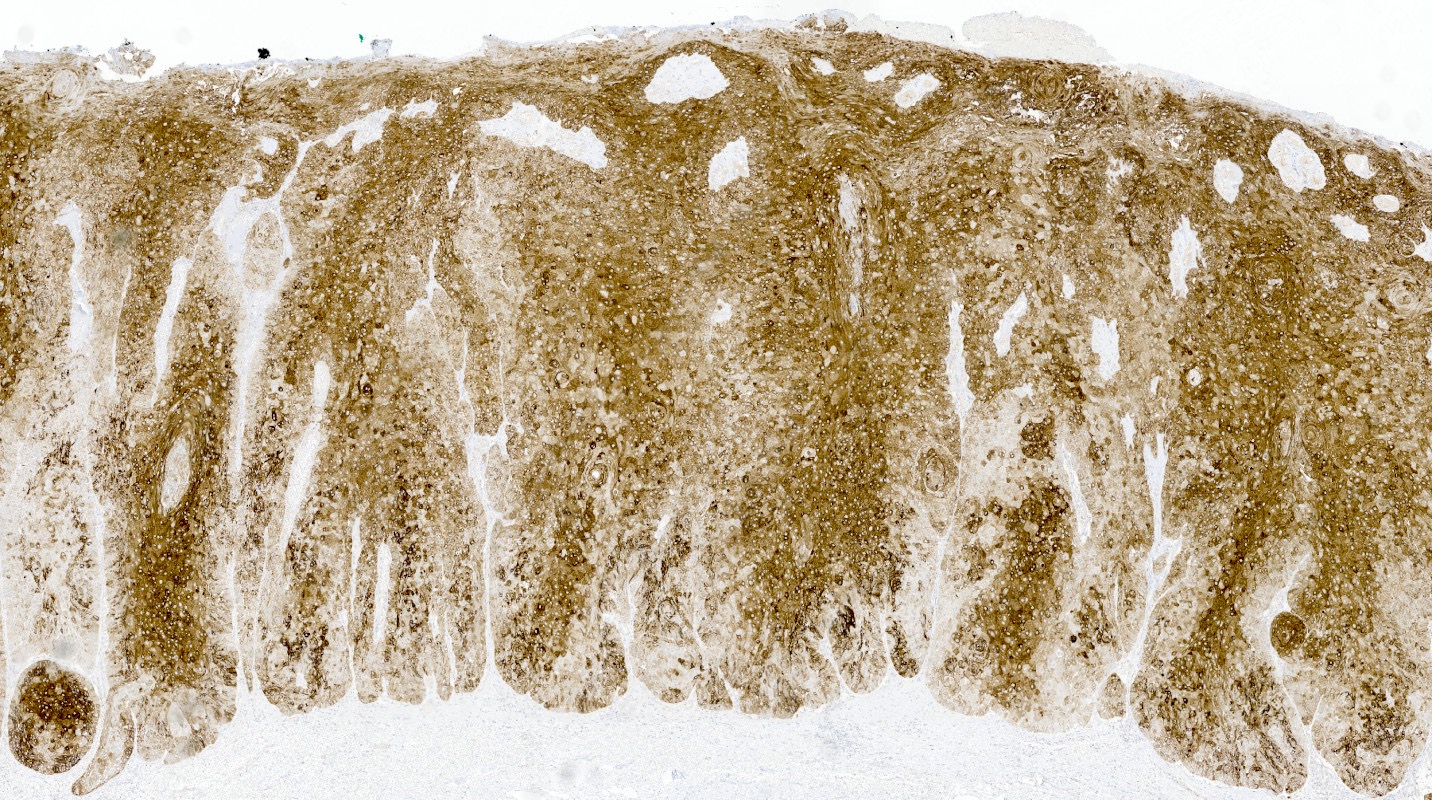
- DEVIL: exophytic verruciform lesion with acanthosis; no basal atypia, no koilocytosis (Mod Pathol 2017;30:448)
- VAAD: verruciform acanthosis, parakeratosis, absence of nuclear atypia, cytoplasmic pallor in superficial cells (Am J Surg Pathol 2004;28:638)
- p53 and p16 immunohistochemistry is recommended for classification (see below)
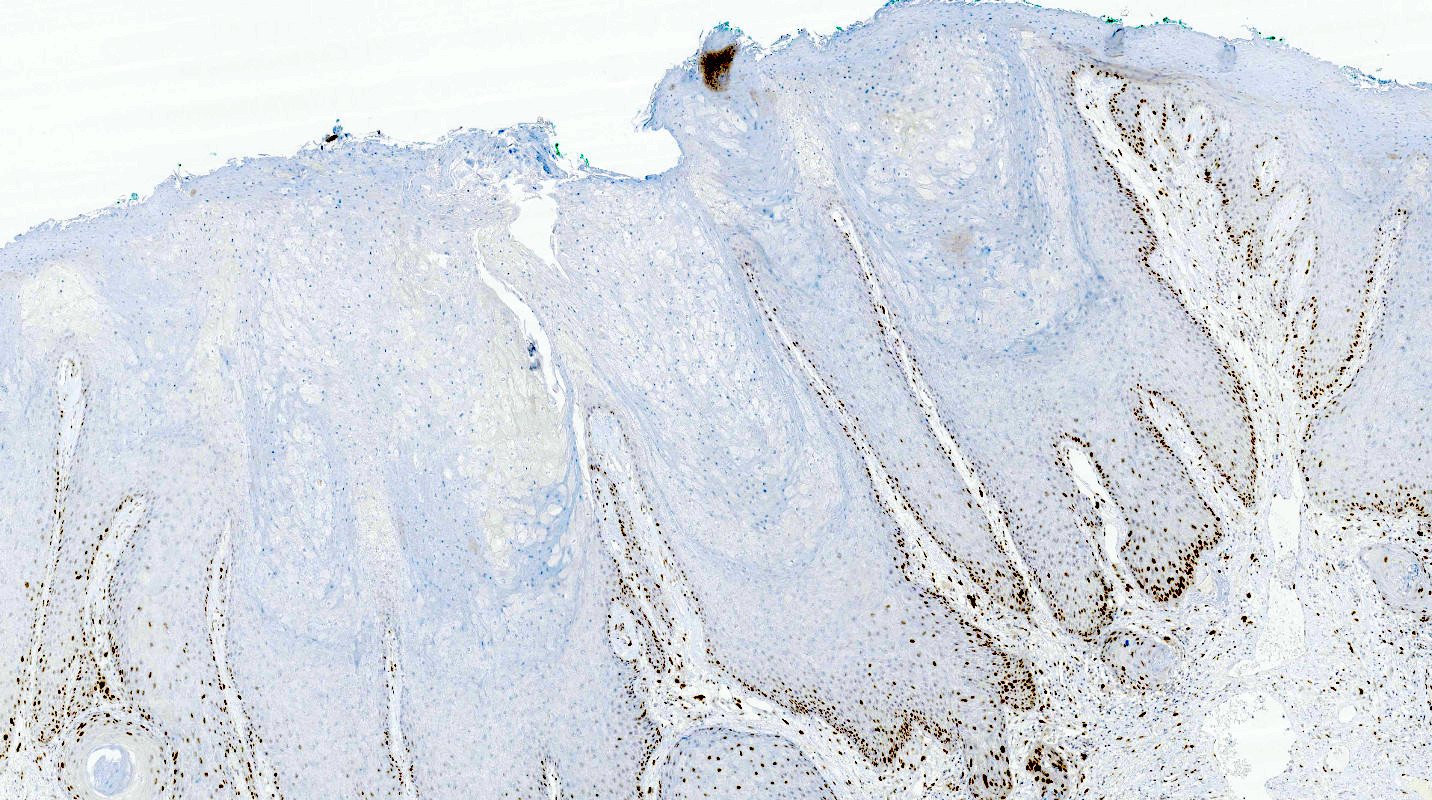
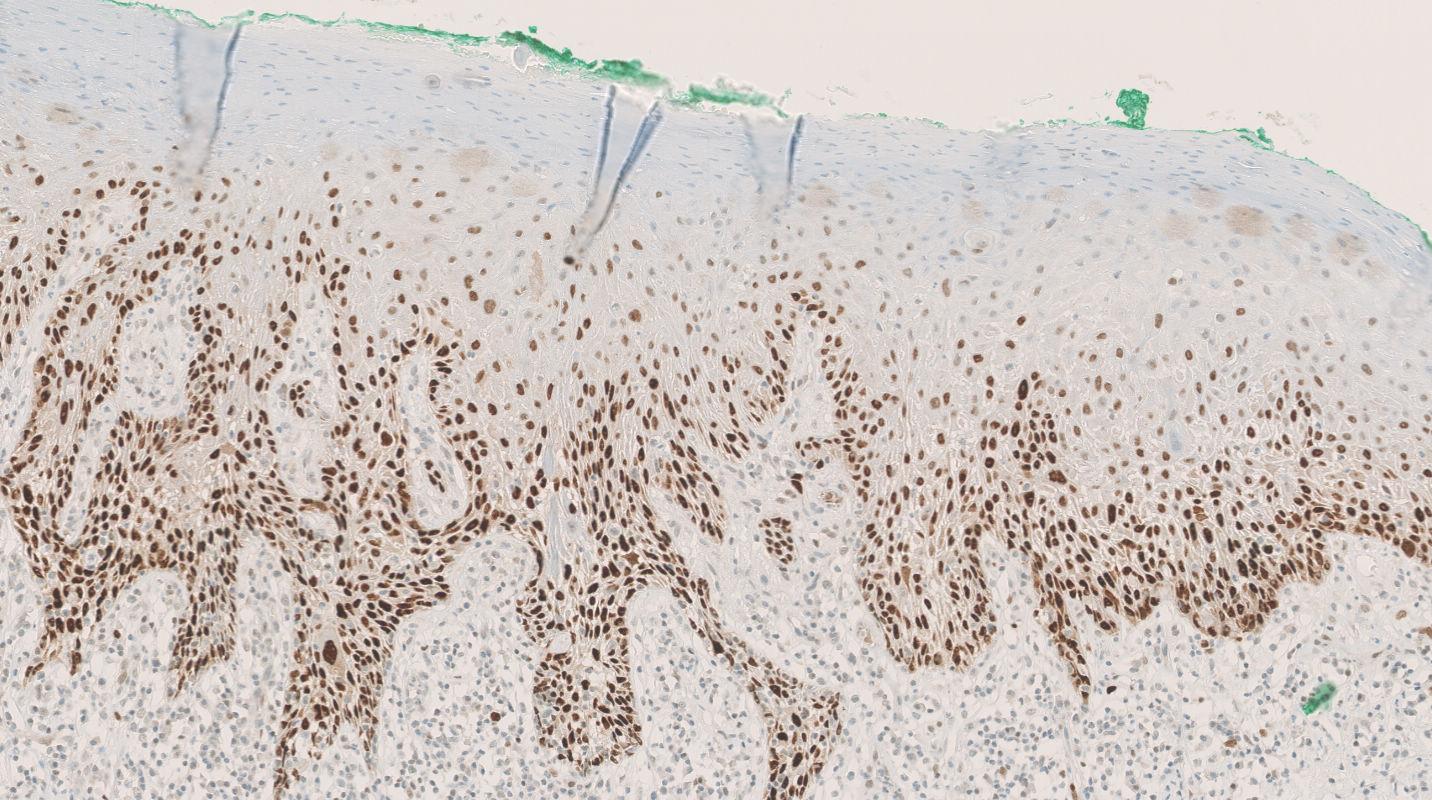
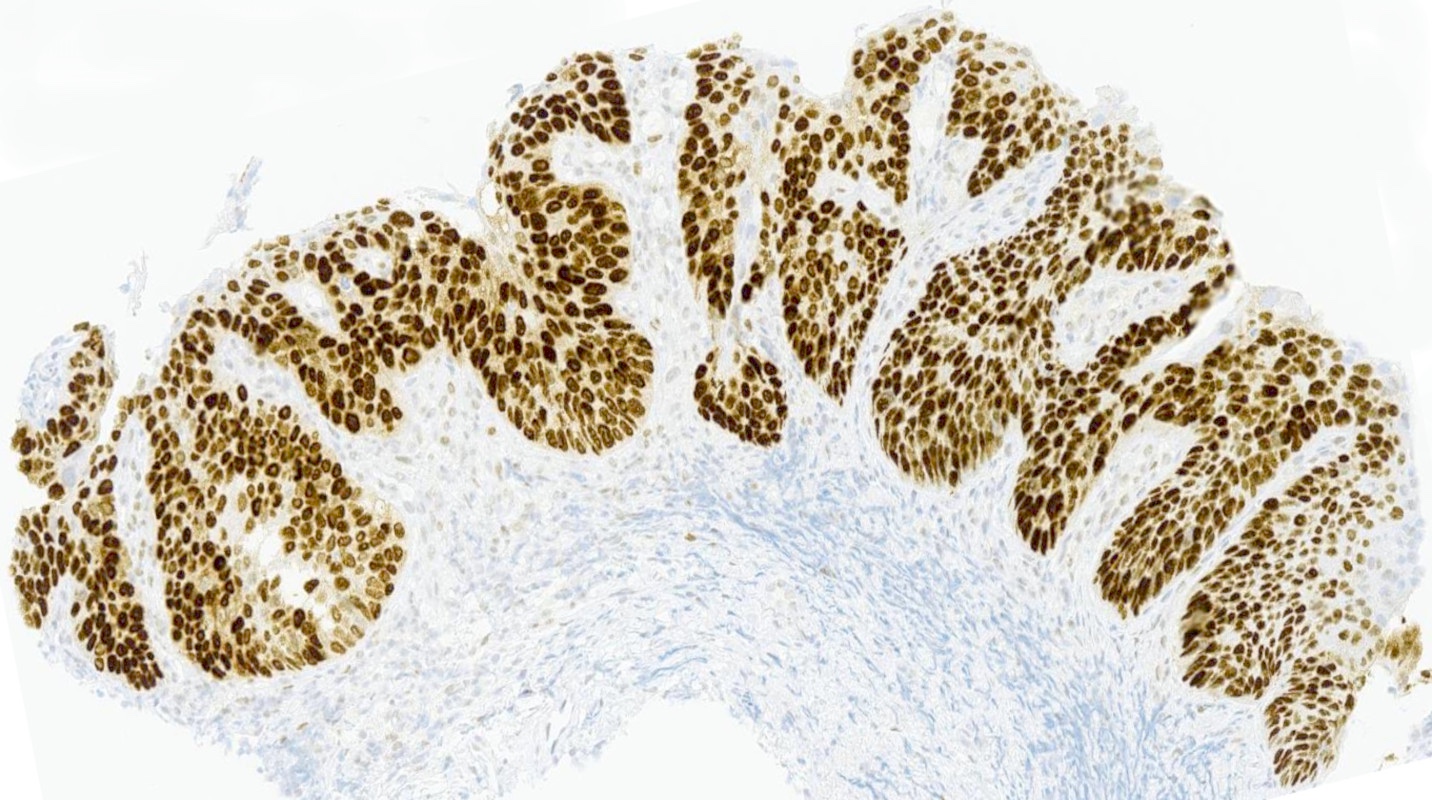
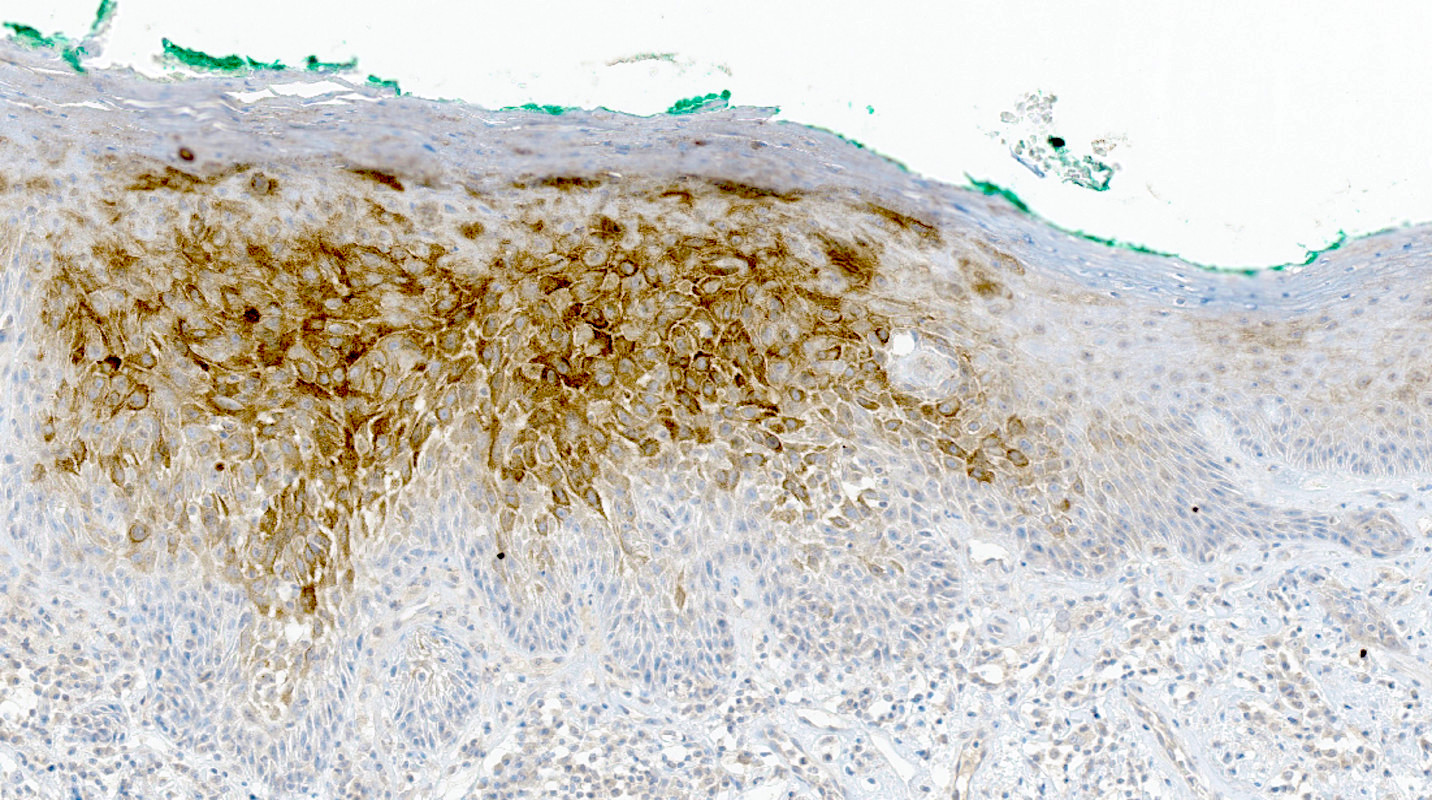
Microscopic (histologic) images
Positive stains
- p53
- Mutation type pattern in dVIN: basal overexpression, diffuse overexpression, absent (null) or cytoplasmic (Mod Pathol 2020;33:1595, Mod Pathol 2023;36:100145)
- Wild type in DEVIL and VAAD
- Interpretation may be difficult in small biopsies
- Ki67 confined to basal cell layers
- Retained CK17 expression (Int J Gynecol Pathol 2017;36:273)
Negative stains
- Loss of GATA3 expression (Mod Pathol 2018;31:1131)
- p16 negative or patchy (Histopathology 2005;46:718)
- HPV
Molecular / cytogenetics description
- HPV ISH negative
- Mutations in TP53 (Mod Pathol 2010;23:404)
Sample pathology report
- Labium majus, biopsy:
- Differentiated vulvar intraepithelial neoplasia (see comment)
- Comment: p16 is negative and p53 is overexpressed (aberrant pattern).
Differential diagnosis
- Condyloma:
- Mild nuclear atypia, most commonly superficially
- HPV related
- Lichen sclerosus:
- Lacks basal atypia
- May be concurrent
- Lichen simplex chronicus:
- Lacks basal atypia
- p53 wild type
- Hypertrophic lichen planus:
- Band-like chronic inflammation
- Lacks basal atypia
Additional references
Board review style question #1
Board review style answer #1
E. TP53 is most frequently mutated and probably most relevant for pathogenesis. Answer A is incorrect because it is not mutated. Answer B is incorrect because it is infrequently amplified. Answer C is incorrect because it is frequently mutated but probably not the most relevant. Answer D is incorrect because it is frequently mutated but mostly in HPV associated lesions.
Comment Here
Reference: HPV independent VIN-vulva
Comment Here
Reference: HPV independent VIN-vulva
Board review style question #2
Which immunohistochemical stain shows an aberrant pattern in differentiated vulvar intraepithelial neoplasia?
- CK18
- Ki67
- p16
- p53
- SOX10
Board review style answer #2
D. p53 frequently shows a mutation type aberrant staining pattern. Answer A is incorrect because CK18 is not overexpressed in differentiated vulvar intraepithelial neoplasia (dVIN), differentiated exophytic vulvar intraepithelial lesion (DEVIL) or vulvar acanthosis with altered differentiation (VAAD). Answer B is incorrect because Ki67 shows only a variable growth fraction as in many other lesions. Answer C is incorrect because p16 is overexpressed in HPV associated VIN. Answer E is incorrect because it is not aberrantly expressed in dVIN.
Comment Here
Reference: HPV independent VIN-vulva
Comment Here
Reference: HPV independent VIN-vulva