Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Erem AS, Turashvili G. Lichen planus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvalichenplanus.html. Accessed April 17th, 2024.
Definition / general
- Chronic, mucocutaneous, inflammatory disease, likely T cell mediated, characterized by band-like lymphocytic inflammation (Am J Surg Pathol 1998;22:473)
Essential features
- Papule or plaque located on hair bearing or hairless vulvar or perianal area
- Band-like lymphocytic infiltrate at the dermoepidermal junction
- Features of destruction of basal keratinocytes
Terminology
- Vulvovaginal lichen planus (VLP) with concomitant oral involvement described as vulvovaginal gingival syndrome (Ann Dermatol Venereol 1982;109:797)
- Although it was previously believed that desquamative inflammatory vaginitis (DIV) can occur as erosive VLP, it is now a distinct entity (Obstet Gynecol 2011;117:850, J Reprod Med 2008;53:124)
ICD coding
- ICD-O:
- ICD-10:
- ICD-11:
- EA91 - lichen planus
- EA91.0 - acute eruptive lichen planus
- EA91.1 - hypertrophic lichen planus
- EA91.2 - follicular lichen planus
- EA91.3 - lichen planus of genital skin and mucous membranes
- EA91.4 - lichen planus and lichenoid reactions of oral mucosa
- EA91.5 - lichen planus of the nails
- EA91.6 - subacute lichen planus
- EA91.Y - other specified lichen planus
- EA91.Z - lichen planus of unspecified type
Epidemiology
- Most commonly involving the introitus (nonhair bearing mucosa) (J Low Genit Tract Dis 2020;24:317, Australas J Dermatol 2016;57:284, Br J Dermatol 2013;169:226)
- Women in fifth to sixth decade
- Incidence of VLP has not been studied; ~1 - 2% worldwide at any site (Int J Womens Dermatol 2017;3:58, N Engl J Med 2012;366:723)
- In a study of 3,350 women over 13 years, 3.7% showed biopsy proven VLP, including 17.6% with erosive VLP (Br J Dermatol 2000;143:1349)
- Erosive VLP
- Up to 68% with concomitant oral lichen planus (OLP) (J Reprod Med 2007;52:43)
- 20% with concomitant cutaneous lichen planus (CLP) (J Eur Acad Dermatol Venereol 2005;19:301)
- 29% present with other autoimmune disorders, most commonly involving the thyroid gland, followed by alopecia areata and celiac disease (Arch Dermatol 2008;144:1432)
- 25 - 34% present with concomitant vulvar disease, most commonly contact dermatitis and atrophic vaginitis (J Reprod Med 2007;52:43)
- Well documented association between VLP and hepatitis C virus (HCV) in Japan but not in European studies (Eur J Clin Invest 1995;25:910, J Eur Acad Dermatol Venereol 2005;19:301, BJOG 2004;111:271)
Sites
- Skin: flexors of wrists, ankles, hands, scalp and genital skin
- Mucosa: genital and oral
Pathophysiology
- Although exact pathophysiology remains unknown, lichen planus is believed to be a T cell mediated autoimmune disease (Clin Exp Dermatol 2005;30:551)
- Epitopic alteration of basal keratinocytes in the epidermis may lead to lymphocytic attack, followed by their destruction and repair (Adv Anat Pathol 2017;24:278)
- Variety of cytokines may play a role in upregulation of cytotoxic T cells (Adv Anat Pathol 2017;24:278)
- Interferon γ, tumor necrosis factor α, interleukins and CXCL10, a chemokine selectively expressed by basal keratinocytes in the presence of cytotoxic T cells in lichenoid dermatoses
- ICAM1, an intercellular adhesion molecule, is crucial in the migration of the T cells to a particular skin site and is overexpressed in lichen planus
Etiology
- Associated with viruses (most commonly HCV)
- HCV may alter the cytokine expression that predisposes to lichen planus development (Adv Anat Pathol 2017;24:278)
- HCV and damaged keratinocytes may share epitopes that cytotoxic T cells target (Med Oral Patol Oral Cir Bucal 2005;10:E40)
- Contact allergens (metal amalgam in oral lichen planus) (Adv Anat Pathol 2017;24:278)
Diagrams / tables
Table 1: Diagnostic criteria of vulvar erosive lichen planus by the International Society of the Study of Vulvovaginal Disease (ISSVD) (adapted from Br J Dermatol 2013;169:337)
| 3 out of 9 criteria needed for diagnosis |
| Well demarcated erosions or glazed erythema of introitus |
| Wickham striae on surrounding skin |
| Pain or burning |
| Scarring or loss of architecture |
| Vaginal inflammation |
| Involvement of other mucosal surfaces |
| Well defined inflammatory band in superficial connective tissue involving dermoepidermal junction |
| Inflammatory band consists of predominantly lymphocytes |
| Evidence of basal cell layer degeneration (e.g., Civatte bodies, abnormal keratinocytes or basal apoptosis) |
Table 2: Summary of minimum clinicopathologic criteria to diagnose vulvar erosive lichen planus, more specific than those proposed by ISSVD (adapted from J Low Genit Tract Dis 2020;24:317)
| All 5 criteria must be present | |
| Clinical presentation (signs) | Well demarcated glazed red macule or patch located on vestibule, labia minora or vagina* |
| Histopathological correlate | Nonkeratinized squamous epithelium, mucocutaneous junction or adjacent hairless skin |
| Band-like lymphocytic infiltrate abuts the epithelial layer | |
Basal layer with one of the following patterns
| |
| Sclerosis is absent | |
- *Supportive features
- Architectural changes include midline fusion or labia minora, adhesions between affected opposed structures
- Common comorbidities: lichen sclerosis (LS), other types of locations of lichen planus, systemic autoimmune diseases
Table 3: Clinicopathologic features of classic hypertrophic lichen planus (adapted from J Low Genit Tract Dis 2020;24:317)
| Classic lichen planus | Hypertrophic lichen planus | |
| Clinical features | Red, gray-white or purple-brown plaque or papules on hairless or hair bearing skin | Circumferential red plaque over hairless and hair bearing skin of vulva or perianal area |
| Histopathological correlate | ||
| Stratum corneum* | Hyperkeratosis | Marked hyperkeratosis |
| Granular cell layer* | Hypergranulosis | Diffuse and marked hypergranulosis |
| Rete ridge morphology | Mild to moderate acanthosis with irregular rete ridges, often sawtoothed or spiky | Marked acanthosis with deep and irregular rete ridges |
| Basal layer | Apoptotic bodies, squamatization, vacuolar change Lymphocytosis | Apoptotic bodies, squamatization, vacuolar change may be confined to rete tips / basal layer above papillary processes
Lymphocytosis |
| Dermis | Band-like applied lymphocytic infiltrate | |
| Papillary dermal fibrosis | ||
- *May be altered by excoriation, especially in hypertrophic lichen planus
Clinical features
- Cutaneous
- Pleuritis, planar, polygonal, purple papules
- Wickham striae represent a fine reticulate network of white lines and are considered pathognomonic
- Mucosal
- Erosive lichen planus (ELP) is most common on vulvovaginal surface
- Reticular pattern and white lacy stria
- Less commonly, atrophic, hypertrophic, papular and bullous lesions
- Reference: J Low Genit Tract Dis 2020;24:317
Diagnosis
- Most reliable diagnosis is based on clinicopathologic correlations
- Vulvar ELP
- Clinical diagnosis is sufficient per the international electronic Delphi consensus exercise conducted by the International Society of the Study of Vulvovaginal Disease (ISSVD) (see Table 1) (Br J Dermatol 2013;169:337)
- To achieve the most reliable diagnosis of vulvar ELP, the recommended clinicopathologic criteria include clinical appearance, site and 3 histopathologic features: lymphocytic infiltrate, basal layer damage (degenerative / regenerative) and absence of sclerosis (see Table 2) (J Low Genit Tract Dis 2020;24:317)
- Biopsy should be taken at the edge of vulvar erosion (Br J Dermatol 2013;169:337)
- Classic and hypertrophic lichen planus diagnosis require their characteristic clinical appearance, accompanied by specific changes at the 5 epidermal layers (see Table 3) (J Low Genit Tract Dis 2020;24:317)
- Concurrent histopathologic evidence should be considered in the diagnosis of complex cases (J Low Genit Tract Dis 2020;24:317)
Prognostic factors
- Overall favorable for lichen planus with cutaneous involvement (self limiting within a year)
- Mucosal involvement is persistent and commonly refractory to the treatment
- Association of lichen planus with human papillomavirus (HPV) independent squamous cell carcinoma is unclear (J Low Genit Tract Dis 2018;22:159)
Case reports
- 30 year old woman with multiple vulvar hyperpigmented papulonodules (Int J STD AIDS 2017;28:1048)
- 32 year old woman with orovaginalvulvar lichen planus (J Med Case Rep 2021;15:97)
- 46 year old woman with severe oral and vulvovaginal erosive lichen planus (Int J Gynaecol Obstet 2022;156:172)
- 55 year old woman with erosive lichen planus vaginitis (Obstet Gynecol 2003;101:1121)
- 79 year old woman with a 3 cm verrucous carcinoma in an area of lichen planus (World J Surg Oncol 2017;15:7)
Treatment
- Topical
- First line: ultrapotent corticosteroids
- Second line: calcineurin inhibitors (can be used in combination with steroids, if there is no initial response to first line)
- Promising initial results in a limited study with aloe vera gel used as an adjunct anti-inflammatory treatment (82% of 17 patients showed significant clinical improvement compared with 1 in the placebo group)
- Topical photodynamic therapy (PDT): 1 session showed a similar reduction in clinical symptom scores compared with months long steroid therapy
- Intralesional injections: triamcinolone acetonide (Kenalog) 3 - 10 mg/mL used where topical steroids failed (Obstet Gynecol Surv 2020;75:624)
- Systemic
- Methotrexate as an additional treatment regimen in recalcitrant vulvovaginal disease
- Prednisone to treat flares of widespread desquamative disease
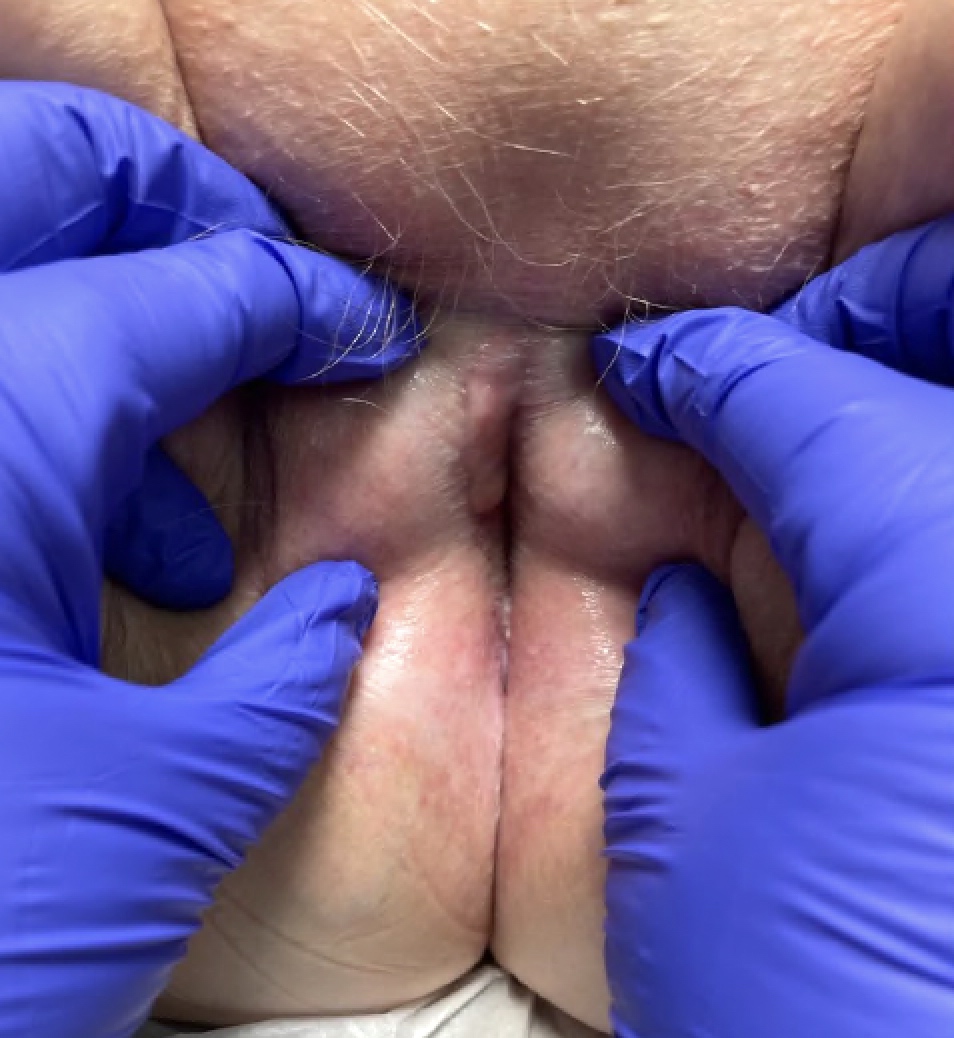
Clinical images
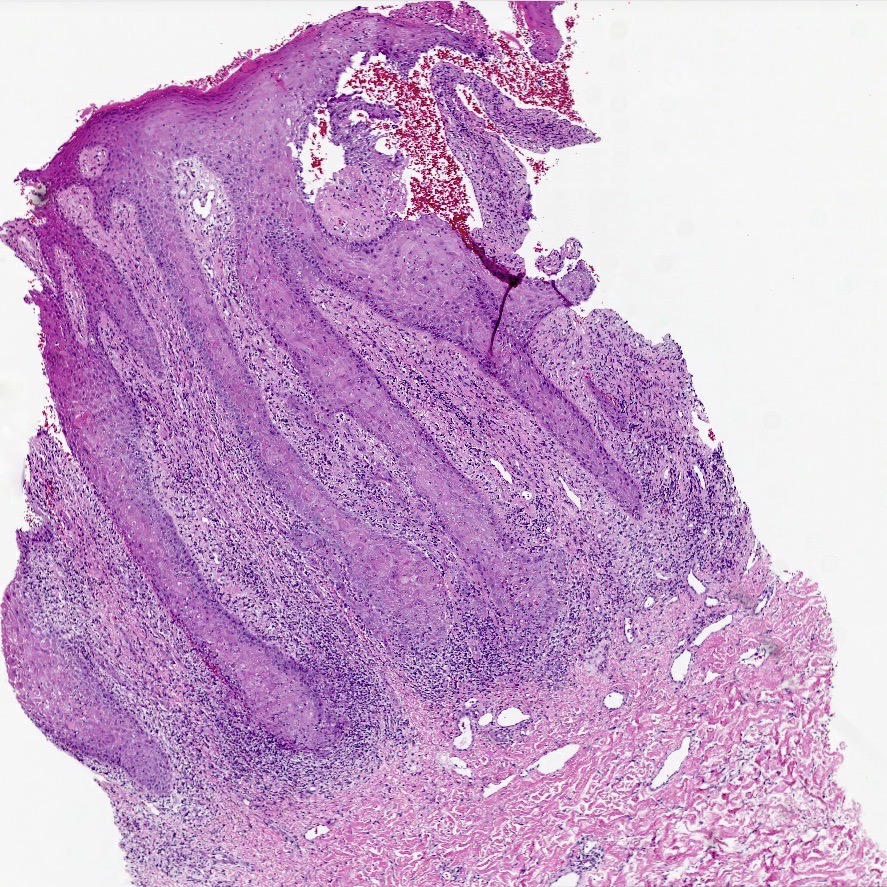
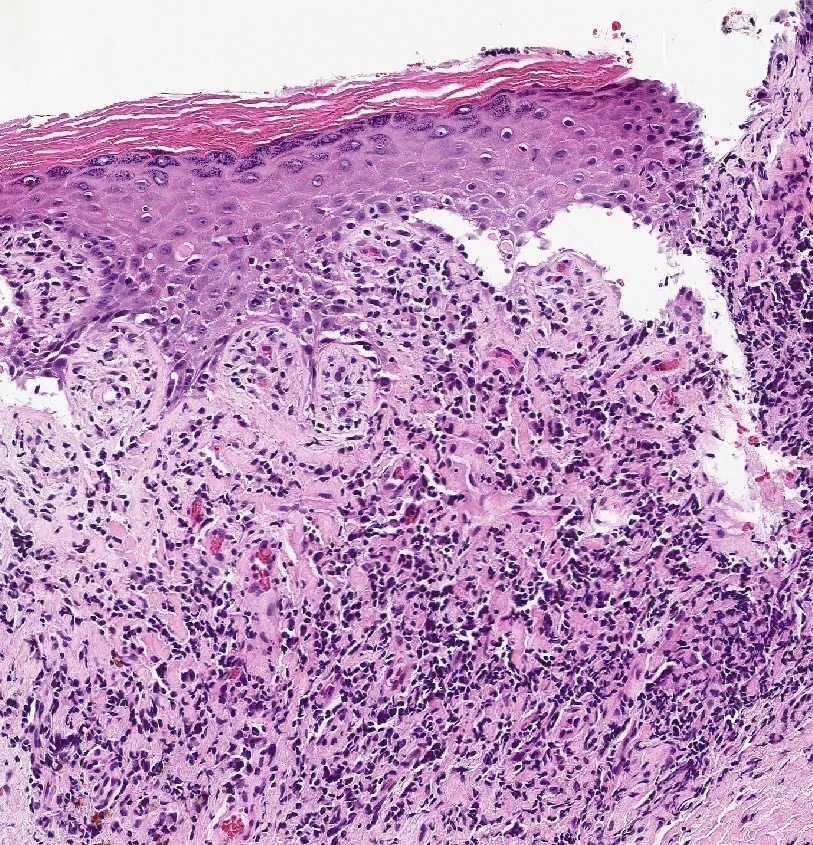
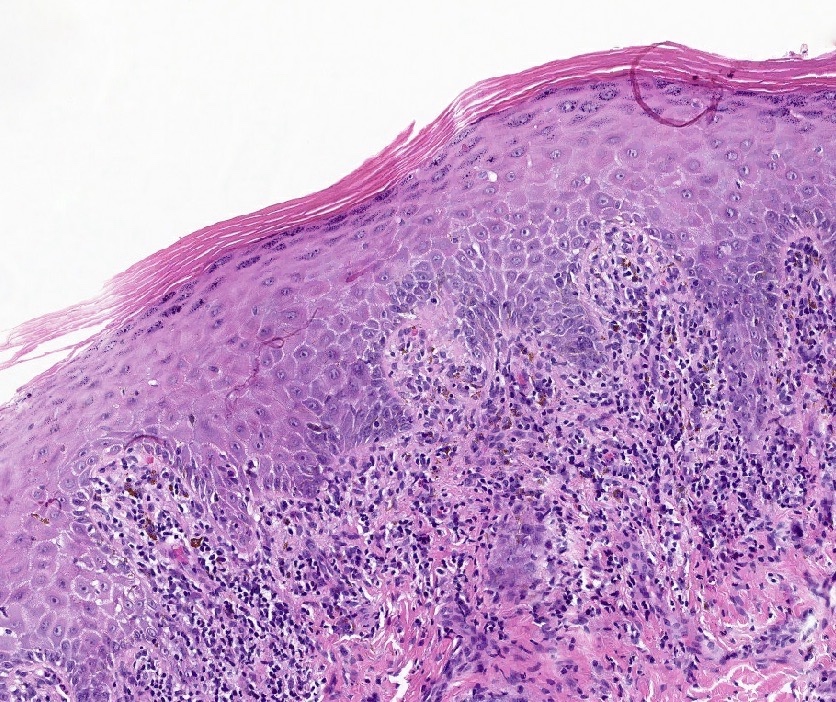
Microscopic (histologic) description
- The International Society of the Study of Vulvovaginal Disease (ISSVD) tasked the Difficult Pathologic Diagnoses Committee with development of a consensus document for the clinicopathologic diagnosis of vulvar ELP, distributed in 2013 based on the Delphi consensus exercise
- Well defined inflammatory band in superficial connective tissue involving dermoepidermal junction
- Inflammatory band consists of predominantly lymphocytes
- Evidence of basal cell layer degeneration (e.g., Civatte bodies, abnormal keratinocytes or basal apoptosis)
- Summary of microscopic findings only to diagnose vulvar ELP, more specific than proposed by ISSVD (see Diagrams / tables for the entire clinicopathologic criteria) (J Low Genit Tract Dis 2020;24:317)
- Nonkeratinized squamous epithelium, mucocutaneous junction or adjacent hairless skin
- Band-like lymphocytic infiltrate abuts the epithelial layer
- Basal layer with one of the following patterns
- Degenerative pattern: apoptotic bodies, vacuolar change or squamatization
- Specific features: Civatte bodies (dyskeratosis) within epidermis and colloid bodies in papillary dermis secondary to basal keratinocyte damage
- Regenerative patterns: high N:C ratio, mitoses, diminished epithelial maturation
- Degenerative pattern: apoptotic bodies, vacuolar change or squamatization
- Sclerosis is absent
- Classic lichen planus (see Diagrams / tables for the entire clinicopathologic criteria) (J Low Genit Tract Dis 2020;24:317)
- Hyperkeratosis and hypergranulosis
- Mild to moderate acanthosis with irregular rete ridges, often sawtoothed or spiky
- Apoptotic bodies squamatization, vacuolar change and lymphocytosis
- Dermis: band-like applied lymphocytic infiltrate
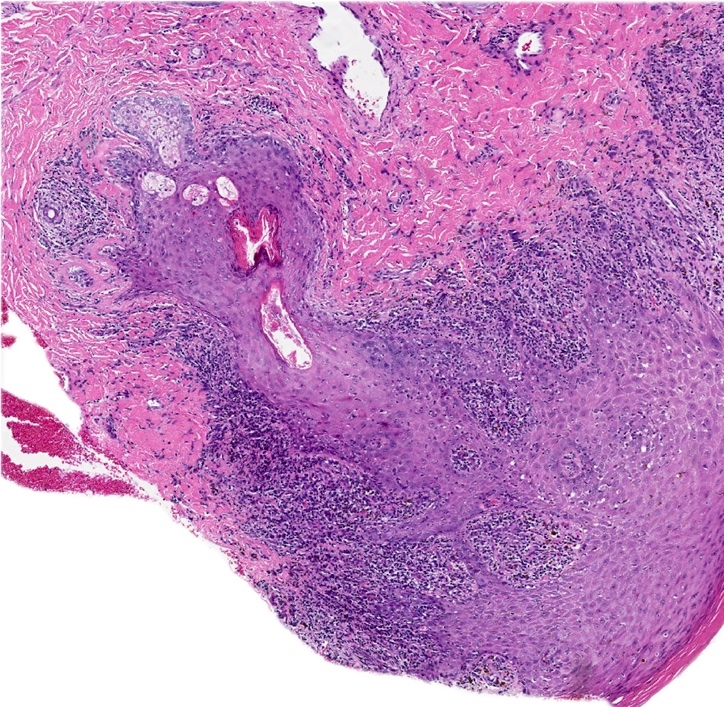
- Hypertrophic lichen planus (see Diagrams / tables for the entire clinicopathologic criteria) (J Low Genit Tract Dis 2020;24:317)
- Marked hyperkeratosis
- Diffuse and marked hypergranulosis
- Rete ridges morphology: marked acanthosis with deep and irregular rete ridges
- Basal layer: apoptotic bodies squamatization, vacuolar change may be confined to rete tips / basal layer above papillary processes and lymphocytosis
- Dermis: band-like applied lymphocytic infiltrate
- Papillary dermal fibrosis
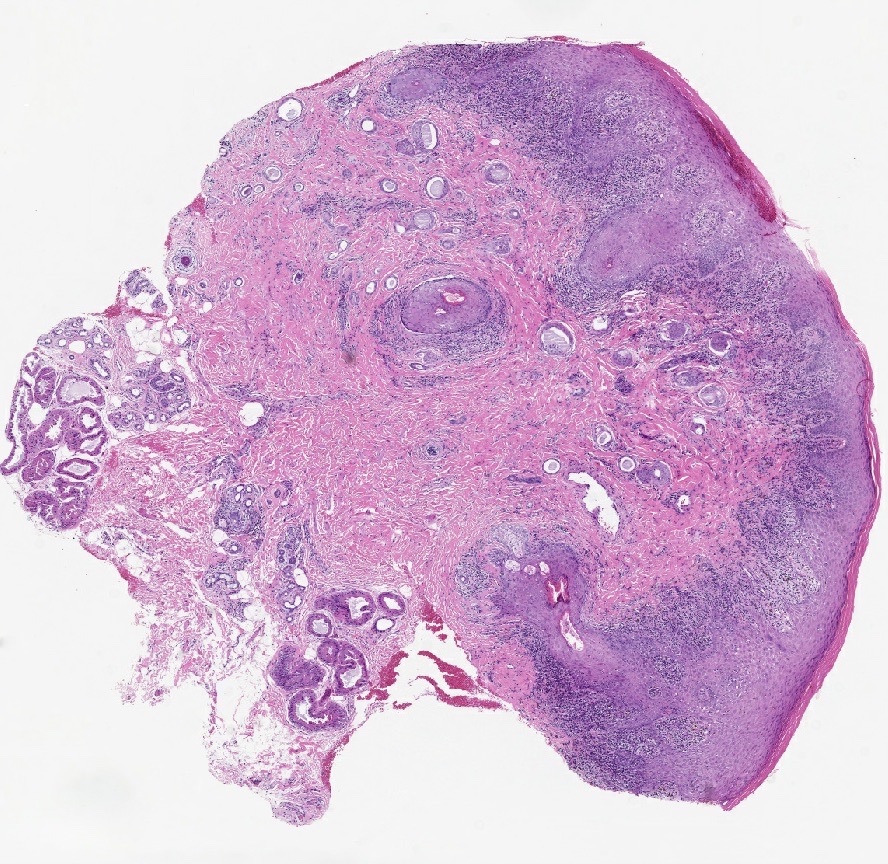
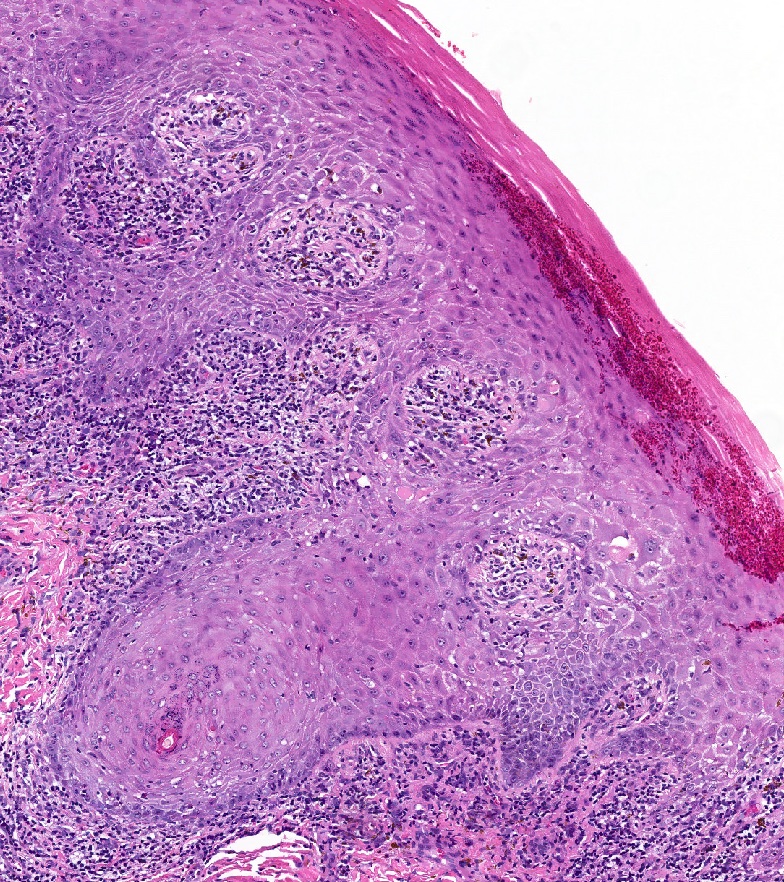
Microscopic (histologic) images
Virtual slides
Immunofluorescence description
- Although not specific, immunofluorescence can support diagnosis
- IgM > IgA, IgG, C3 deposits
- Fibrin stains colloid bodies
Positive stains
- p53: aberrant expression of basal cells in degenerative and regenerative areas
Negative stains
- p16: negative in regenerative areas, focally positive in degenerative areas of vulvar ELP
Videos
Lichen planus & hypertrophic lichen planus
Hypertrophic lichen planus: 5 minute pathology pearls
Lichen planus
Sample pathology report
- Vulva, labium majus, left, punch biopsy:
- Findings consistent with lichen planus (see comment)
- Comment: Sections show epidermal acanthosis, hypergranulosis and a lichenoid chronic inflammatory infiltrate with Civatte bodies. No basal atypia is seen. A special stain for PASF is negative for fungal organisms. A p53 immunohistochemical stain shows a wild type staining pattern. The morphologic features are consistent with lichen planus. Clinicopathologic correlation is recommended.
Differential diagnosis
- Lichenoid drug eruption:
- Parakeratosis and dyskeratosis
- Perivascular and periadnexal inflammatory infiltrate composed of plasma cells and eosinophils
- Early lichen sclerosus:
- Psoriasiform epidermal hyperplasia
- Superficial band-like chronic inflammation with lymphocytes extravasation into lower epidermis
- Papillary dermal fibrosis
- Vacuolization of basal epidermal layer
- Syphilis:
- Minimal dyskeratosis
- Early infection: neutrophilic infiltrate in early infection
- Granulomatous inflammation later in the disease
- Deep perivascular plasmacytic infiltrate
- Endothelial cell swelling (endarteritis)
- Positive T. pallidum immunohistochemistry or Warthin-Starry silver stain
- Plasmacytosis mucosae (Zoon vulvitis):
- 1 - 3 cm isolated brown-red patch or plaque
- ≥ 50% polyclonal plasmacytic infiltrate
- Loss of stratum granulosum with mild spongiotic change
- Red cell extravasation with hemosiderin deposition
- High grade squamous intraepithelial lesion (HSIL):
- Full thickness epithelial atypia with acanthosis, papillomatosis, suprabasal mitoses, extension in hair follicles and skin appendages
- Diffuse, block-like p16 expression
- Differentiated vulvar intraepithelial neoplasia (dVIN):
- Basal atypia with enlarged, hyperchromatic nuclei, prominent nucleoli, prominent intercellular bridges, eosinophilic cytoplasm
- Acanthosis, parakeratosis, elongation and anastomosis of rete ridges
- Aberrant p53 expression
- Desquamative inflammatory vaginitis:
- Purulent vaginal discharge with abnormal vaginal flora
- Mixed predominantly polymorphonuclear leukocytes in parabasal epithelial cells
- Thinning of adjacent epithelium
Additional references
Board review style question #1
A 63 year old woman previously diagnosed with lichen planus returns to the clinic with a persistent, well demarcated plaque and suboptimal treatment response. A biopsy shows lichenoid inflammation with minimal basal atypia. What result or clinical information would favor reactive process over neoplastic process?
- Complete loss of p53
- Diffuse, block-like expression of p16
- Prior history of HPV independent squamous cell carcinoma
- Wild type p53 expression
Board review style answer #1
D. Wild type p53 expression. Wild type p53 expression pattern supports the diagnosis of lichen planus, although aberrant expression can be seen in the basal cells of regenerative erosive lichen planus. Answer A is incorrect because the complete loss of p53 constitutes aberrant expression and would be concerning for differentiated vulvar intraepithelial neoplasia. Answer B is incorrect because diffuse block-like expression of p16 is characteristic in HPV associated with a high grade squamous intraepithelial lesion. Answer C is incorrect because prior history of HPV independent squamous cell carcinoma increases a pretest probability in a 63 year old woman with a persistent vulvar plaque and suboptimal treatment response.
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus
Board review style question #2
A 45 year old woman with a past medical history of hypothyroidism presents to the clinic with pain and burning discomfort in the vulvar area. On physical examination, a well delineated red plaque in the vaginal introitus is observed extending onto the labia majora. There is no scarring or obvious vaginal inflammation. A punch biopsy was obtained. PASF shows no fungal elements. Based on the microphotograph above and clinical information provided, what is the most likely diagnosis?
- Fixed drug reaction
- High grade squamous intraepithelial lesion (HSIL)
- Syphilis
- Vulvar hypertrophic lichen planus
Board review style answer #2
D. Vulvar hypertrophic lichen planus. The patient presented with a circumferential red plaque over the hairless and hair bearing skin of the vulva. The microphotograph shows marked acanthosis with deep and irregular rete ridges, hypergranulosis and dense, band-like lymphocytic infiltrate in the superficial dermis, with apoptotic bodies squamatization and superficial perivascular inflammation. Taken together with the clinical presentation, the findings are consistent with vulvar hypertrophic lichen planus. Answer A is incorrect because although it is important to evaluate medication history, there are no conspicuous eosinophils in the epidermis and superficial dermis, which makes a fixed drug reaction less likely. Answer B is incorrect because high grade squamous intraepithelial lesion can be ruled out based on the absence of full thickness epithelial atypia and increased suprabasal mitotic activity. Answer C is incorrect because syphilis is typically associated with minimal dyskeratosis and neutrophilic infiltrate in the early stages and granulomatous inflammation later in the disease, usually with deep perivascular inflammation.
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus