Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Salari E, Ma L. Paget disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvapagetsdisease.html. Accessed October 1st, 2025.
Definition / general
- Intraepithelial adenocarcinoma primarily involving the epidermis of vulvar skin, with or without an underlying invasive adenocarcinoma
- May be either primary or secondary
Essential features
- Large, round epithelial cells with abundant pale cytoplasm and large nuclei present within the epidermis
- In primary Paget disease, neoplastic cells are consistently strongly positive for CK7
- Recurrence of disease is common despite seemingly adequate excision
Terminology
- Extramammary Paget disease (EMPD)
- Primary cutaneous Paget disease
- Secondary Paget disease
ICD coding
Epidemiology
- Accounts for 1 - 2% of vulvar neoplasms (Cancers (Basel) 2023;15:1803)
- Typically affects postmenopausal White women > 60 years of age; mean age is 65 years (Australas J Dermatol 2013;54:9)
- Most cases are primary Paget disease
- ~15 - 20% of vulvar extramammary Paget disease cases are associated with invasive disease
Sites
- Labia majora is the most common site
- Labia minora, clitoris; can extend to the vaginal or (rarely) cervical mucosa (Diagn Cytopathol 2016;44:931)
- Can extend onto extravulvar skin
Pathophysiology
- Primary Paget disease (cutaneous)
- Presumably originates in the appendages
- Pluripotent stem cells of the adnexa, cells from sweat ducts or cells from anogenital mammary-like glands including the clear cells of Toker (Am J Dermatopathol 2005;27:185)
- Paget cells can thus display apocrine, eccrine and keratinocyte differentiation
- Presumably originates in the appendages
- Secondary Paget disease (extracutaneous)
- Associated primary anal, rectal, bladder, cervical or other noncutaneous adenocarcinoma secondarily involving vulvar skin
Clinical features
- Symptoms include pruritus, burning and vulvar pain; few cases are asymptomatic
- Generally appears as erythematous and eczematoid plaques; may also demonstrate crusting, focal erosion or discharge
- Frequently multifocal
- As most cases present similarly to inflammatory processes, delay in diagnosis is common and often occurs months to years after symptom onset (Gynecol Oncol 2011;122:42)
Diagnosis
- Vulvar biopsy
- Once diagnosis is confirmed, may be prudent to exclude secondary involvement by other underlying malignancy (e.g., rectal, bladder or cervical origin)
- May require physical, endoscopic or radiologic examination
Laboratory
- No validated tumor markers for extramammary Paget disease
- Tumor cells express carcinoembryonic antigen (CEA)
- Serum CEA may be elevated in patients with metastatic or invasive extramammary Paget disease (Br J Dermatol 2008;158:313)
- Elevated CEA levels have been associated with poor prognosis
Prognostic factors
- Generally good prognosis; 5 year overall survival rate is 75 - 95% (Dermatol Surg 2020;46:151)
- Recurrence is common, occurring in up to 44% of patients who undergo wide local excision
- Recurrence is common regardless of surgical margin status (Gynecol Oncol 2007;104:547)
- Negative prognostic factors include the presence of a nodule within the primary lesion, palpable lymphadenopathy, deep invasion into the dermis and lymph node metastases (Dermatol Surg 2012;38:1938)
- Increased p53 expression may be associated with invasion and thus poor prognosis (Hum Pathol 2003;34:880)
Case reports
- 59 year old woman with a history of low grade papillary urothelial carcinoma of the bladder status postresection and postimmunotherapy who later presented with severe vulvar pruritus (Diagn Pathol 2019;14:125)
- 65 year old woman presented with a 10 cm left vulvar slow growing pruritic erythematous plaque (Indian J Sex Transm Dis AIDS 2020;41:210)
- 72 year old woman presented with an erythematous and pruritic vulvar plaque (Rev Bras Ginecol Obstet 2019;41:412)
- 73 year old White woman presented with a 3 month history of left vulvar erythema and pruritus unresponsive to topical creams (Gynecol Obstet Invest 2017;82:1)
Treatment
- Primary treatment is wide local excision or vulvectomy (Gynecol Oncol 2020;157:146)
- Other treatment options include Mohs micrographic surgery, radiation and topical agents such as 5-fluorouracil, imiquimod, rapamycin and bleomycin
- Targeted therapy may be used to treat metastatic extramammary Paget disease when HER2 amplification is present
- Trastuzumab has been used alone and in combination with cytotoxic chemotherapy (JCO Precis Oncol 2018;2:1)
- In secondary Paget disease, treatment of the underlying malignancy is necessary
- May require managements tailored to the primary malignancy
Clinical images
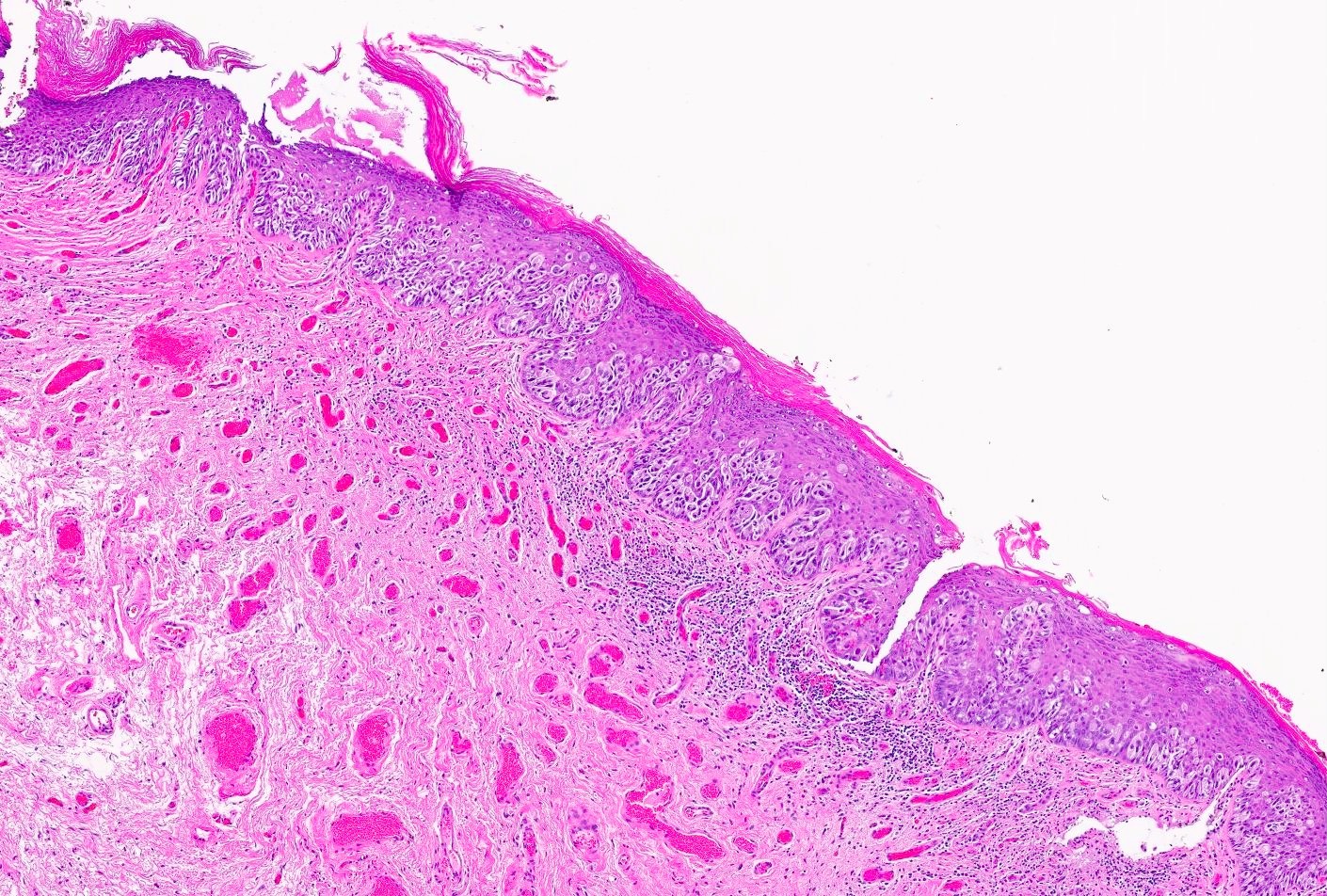
Gross description
- Often ill defined, raised, red scaly plaque(s)
Frozen section description
- Identifying Paget cells on frozen section is difficult
- Reported false negative rates of ~37% (Diagn Cytopathol 2016;44:931)
- Routine frozen section evaluation is not advised
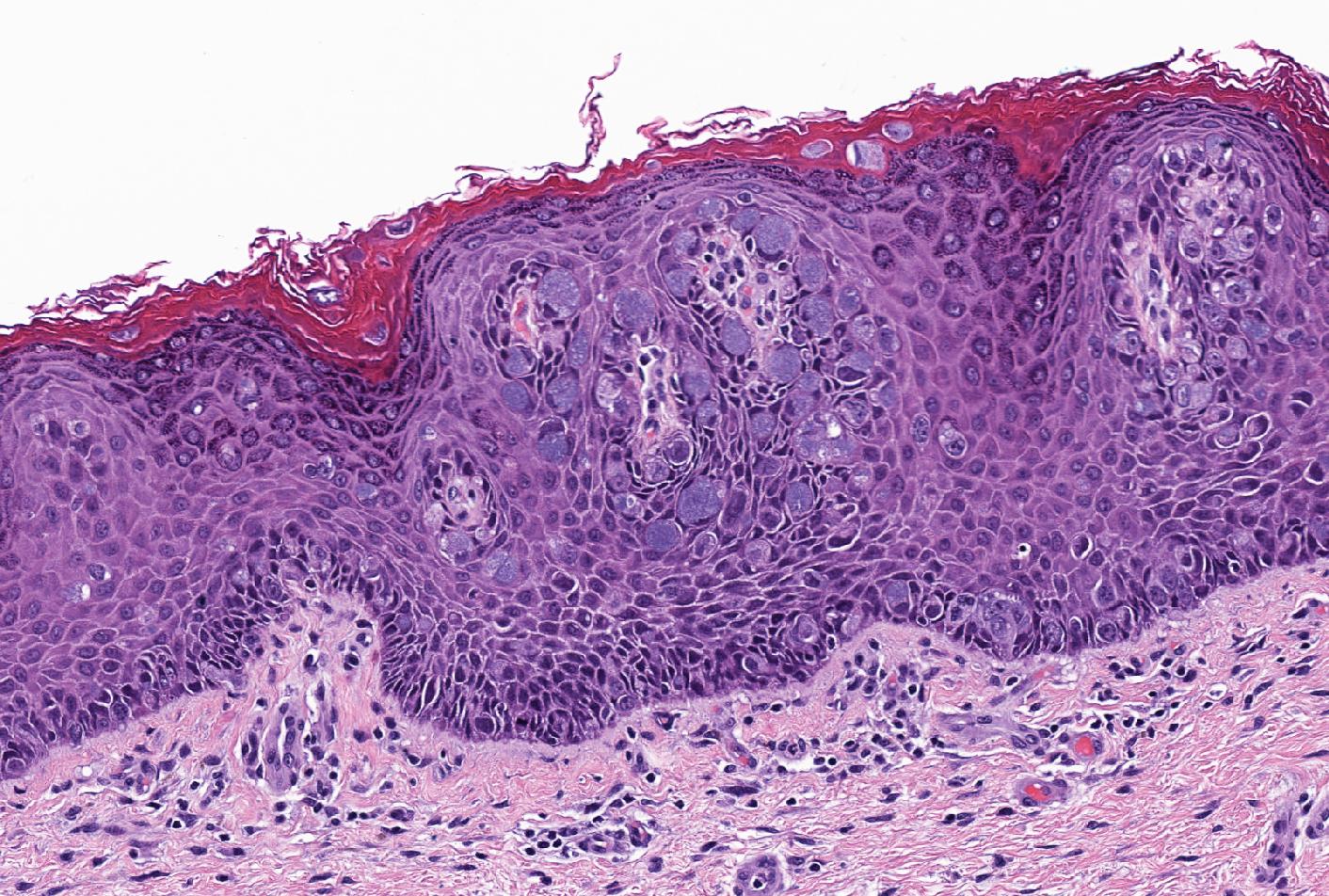
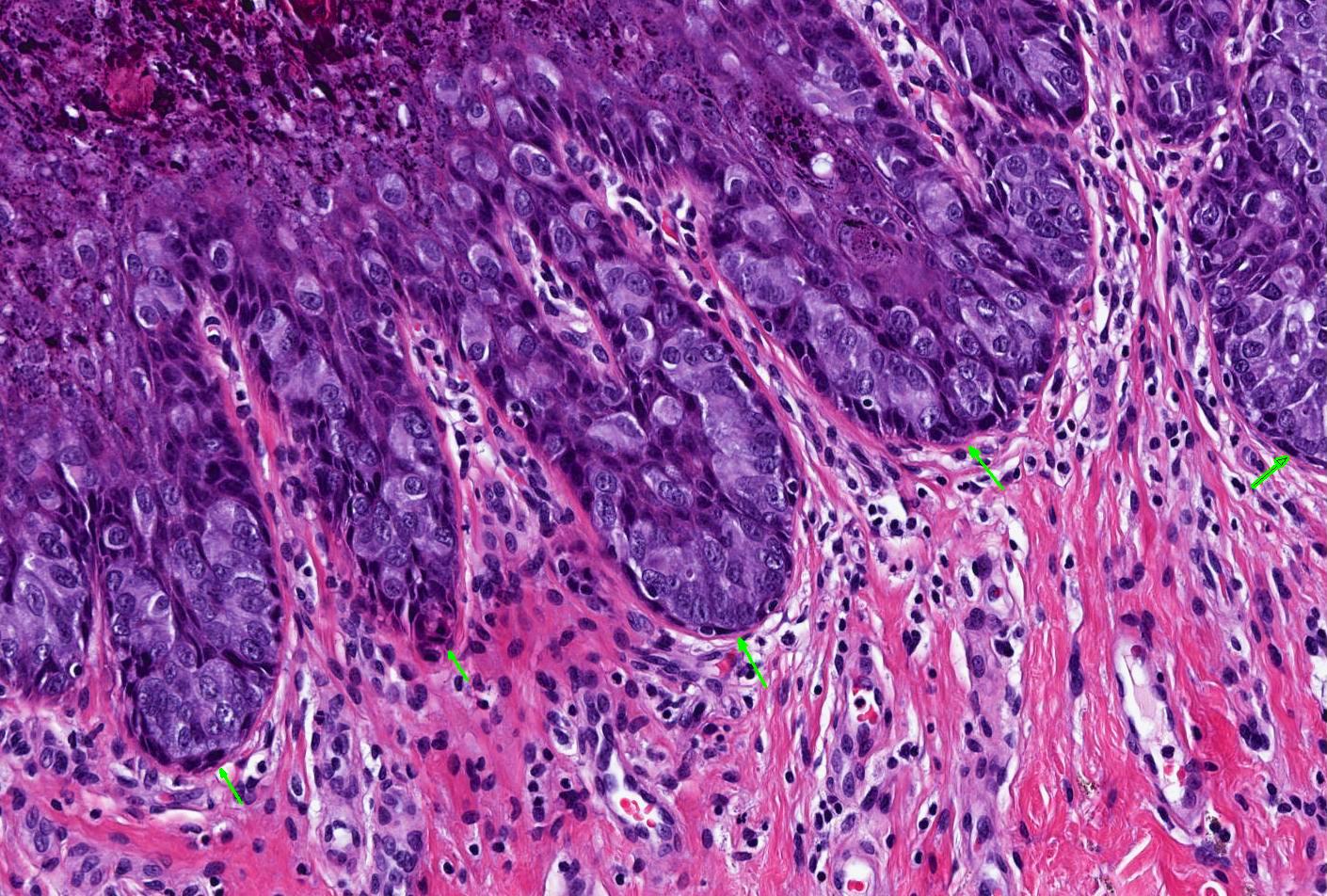
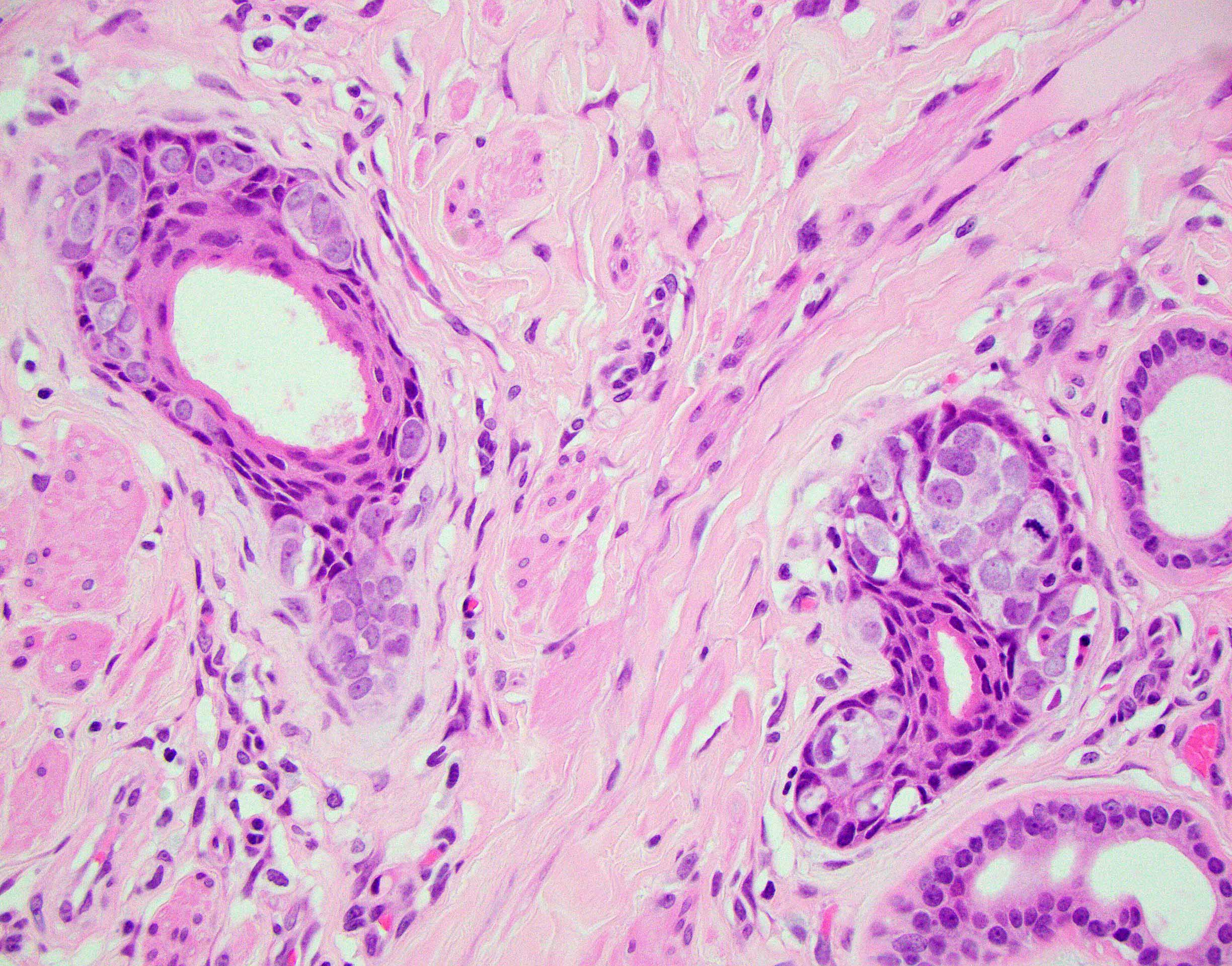
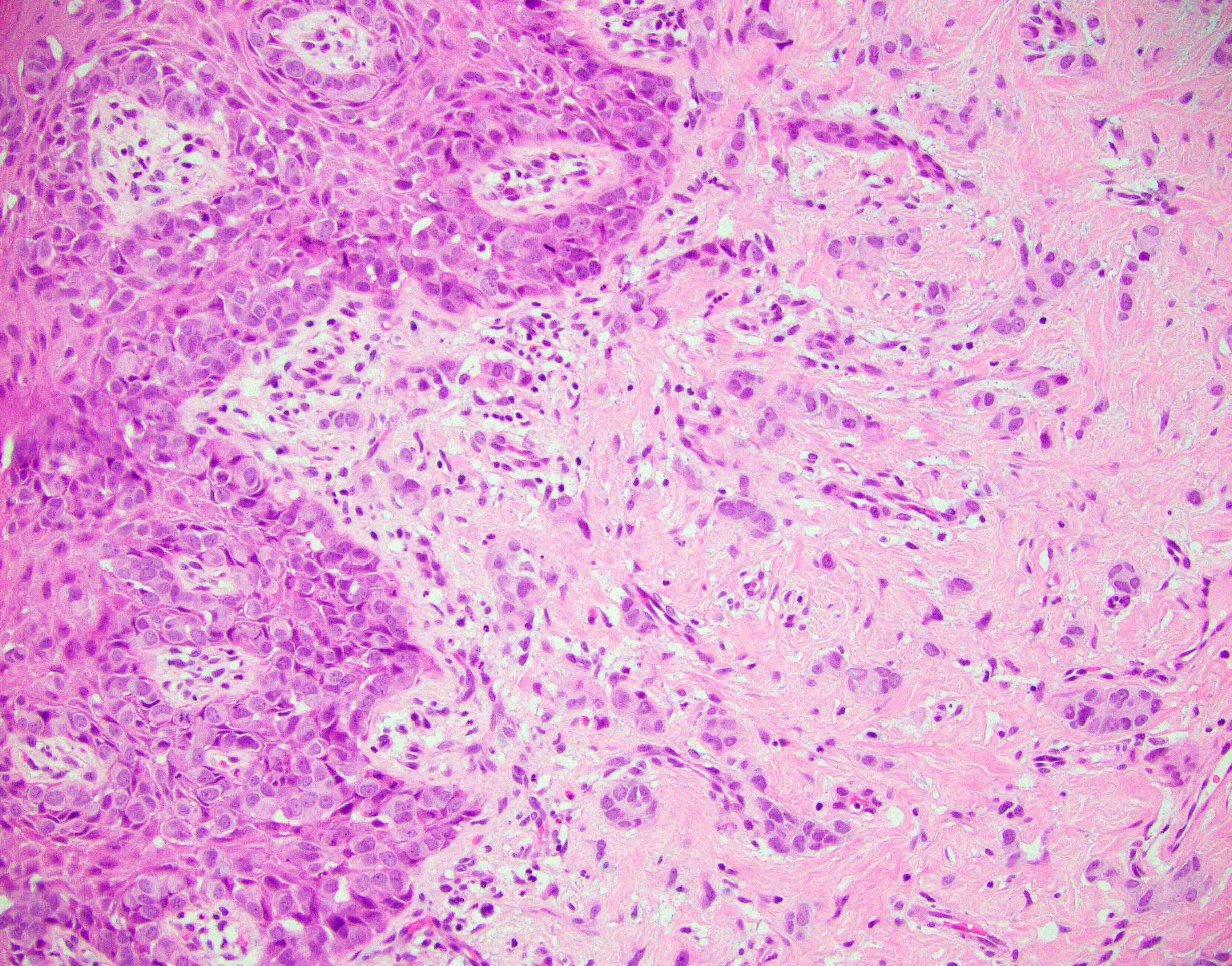
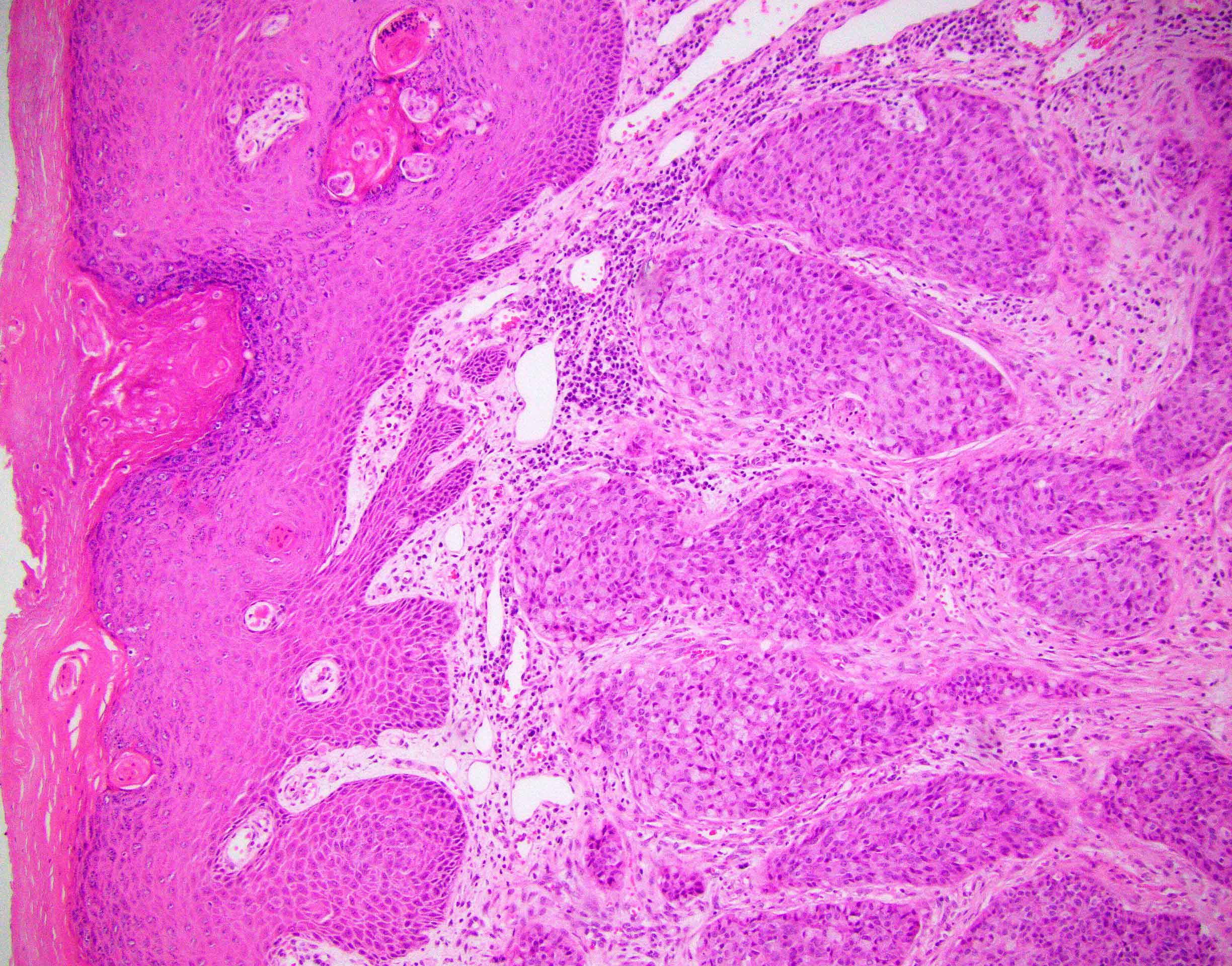
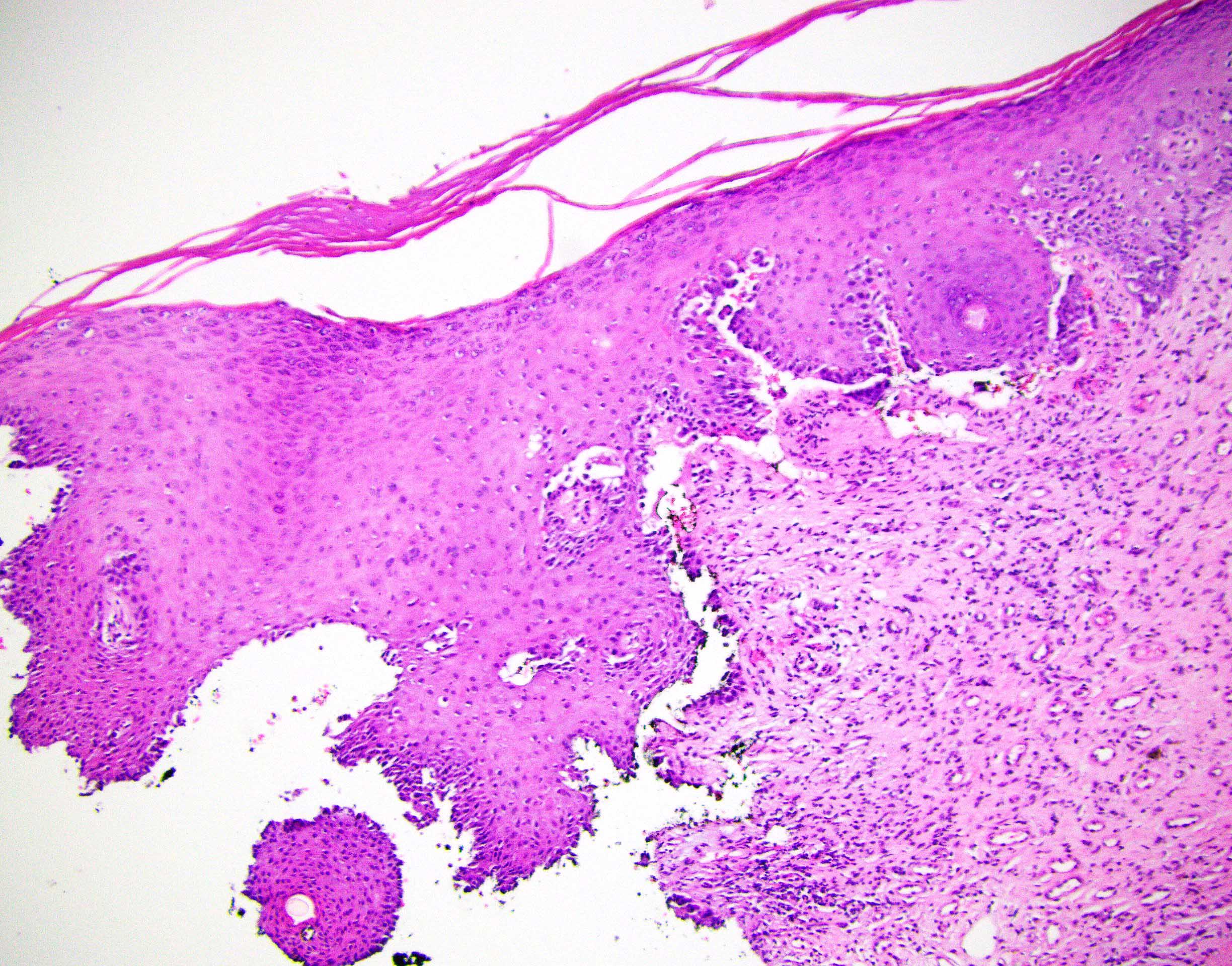
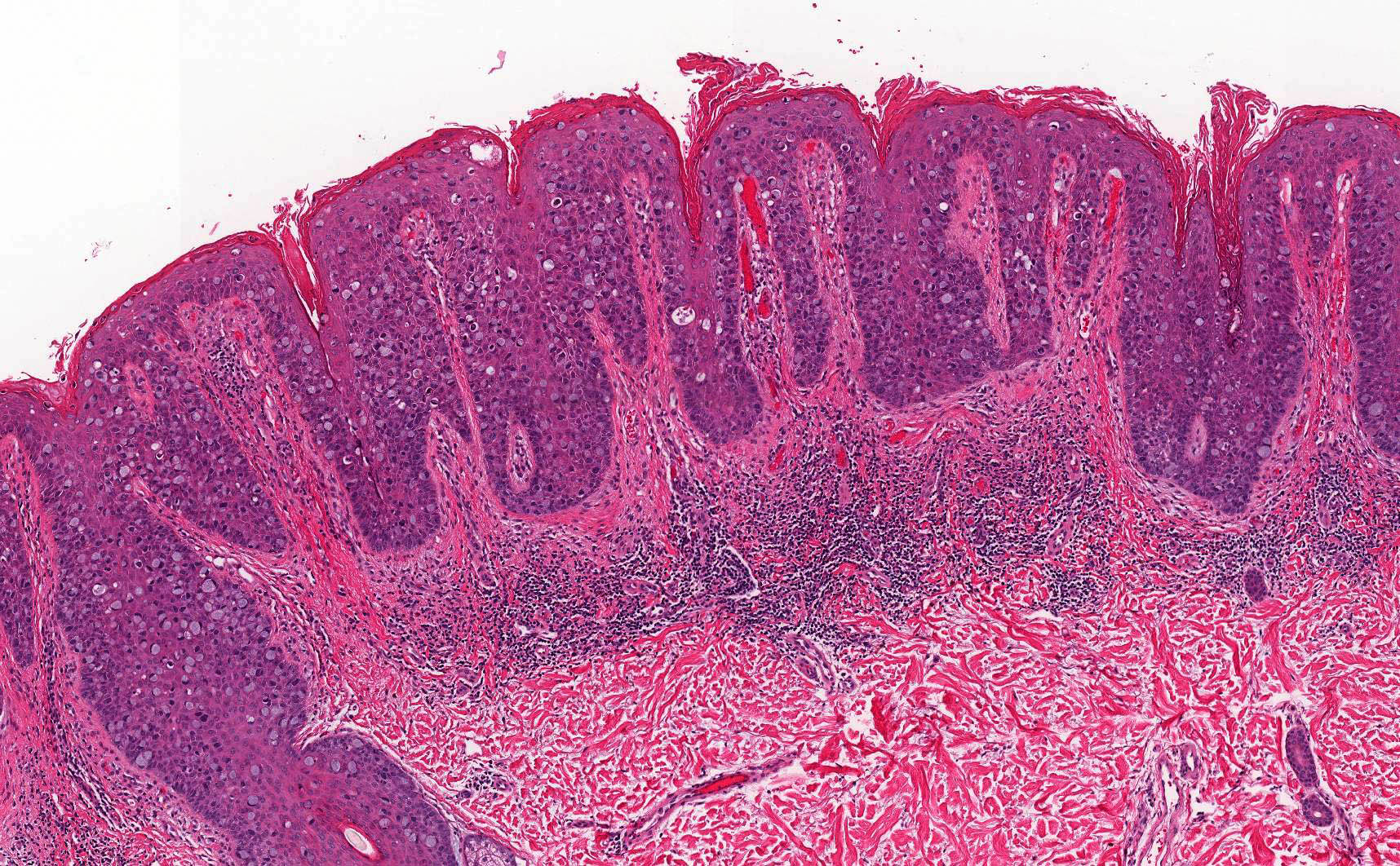
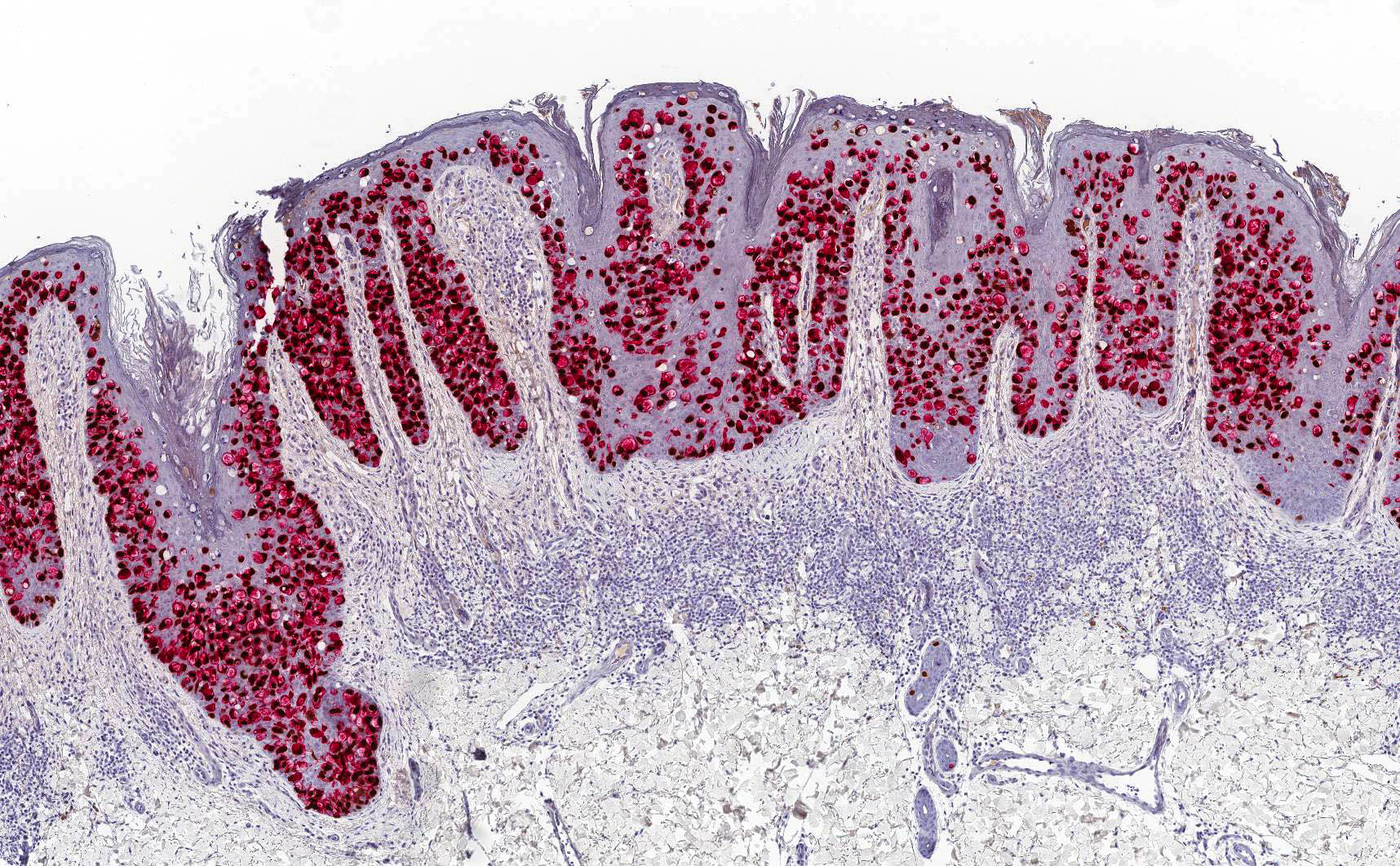
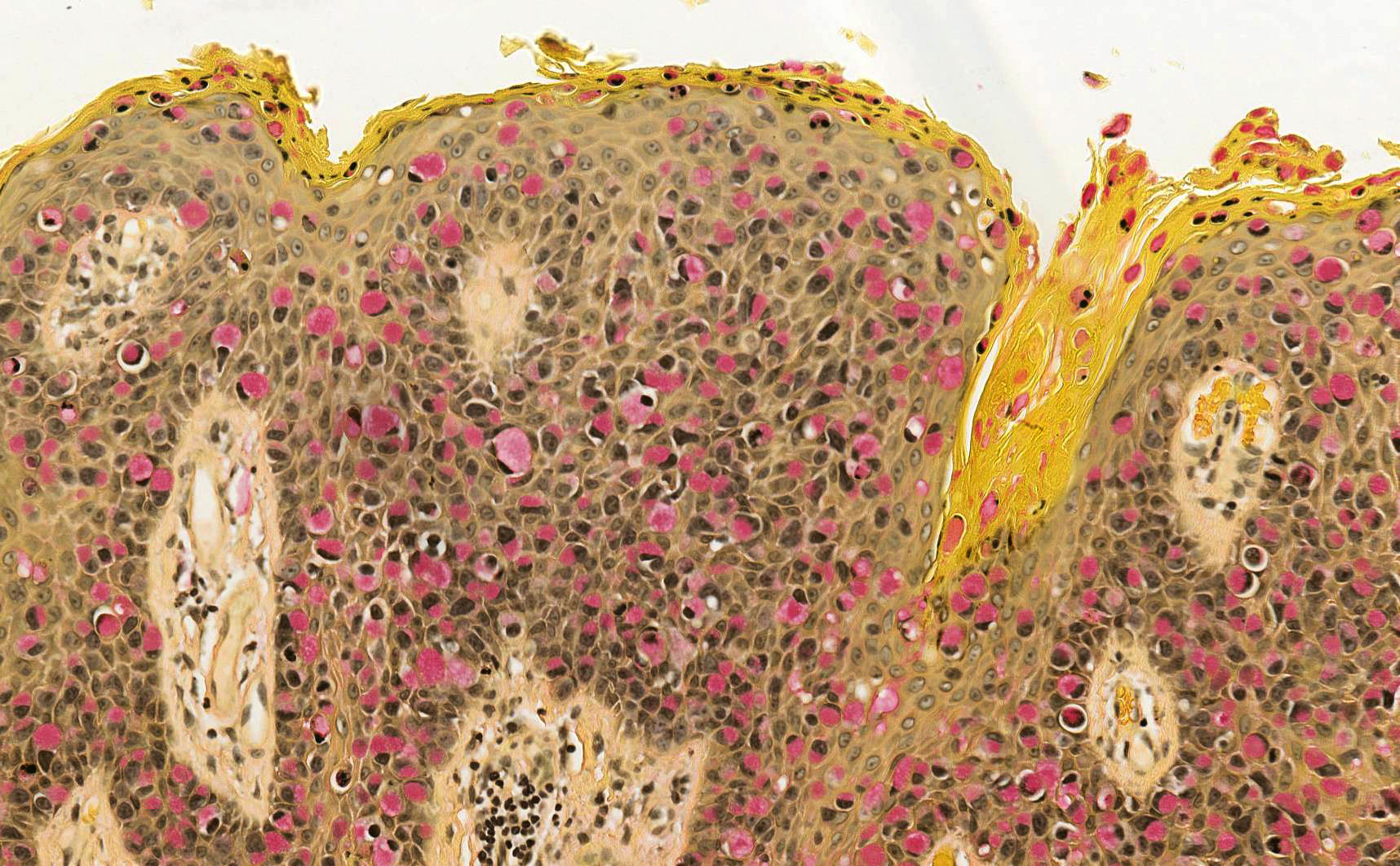
Microscopic (histologic) description
- Paget cells are enlarged polygonal epithelial cells with abundant pale cytoplasm, large nuclei and small to prominent nucleoli
- Intracytoplasmic mucin is frequently present
- Intracytoplasmic melanin pigment may be present (rare)
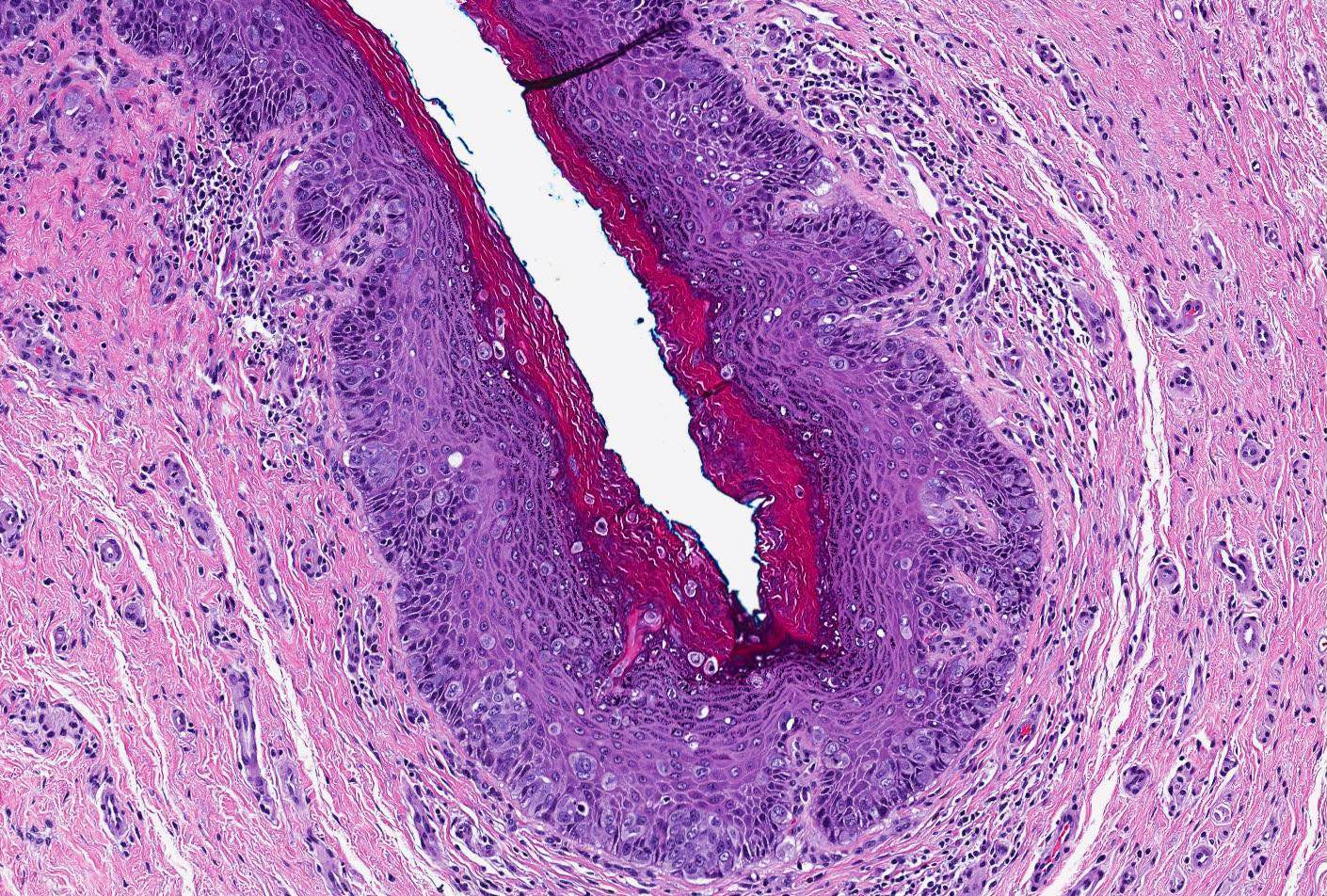
- Rarely, gland formation may be seen
- Predominantly located in the basal and parabasal portions of the squamous epithelium
- Extends upward as single cells or in small clusters
- Commonly involves the epithelium of skin adnexa
- Basal layer keratinocytes are preserved but may appear compressed by the tumor cells (Histopathology 2006;48:723)
- Prominent host inflammatory response in the superficial dermis is frequently seen
- Dermal invasion
- Single cells or small groups of cells infiltrating the dermis with an associated desmoplastic reaction
- Groups of cells may form glandular structures
- May be associated with dense dermal inflammatory response
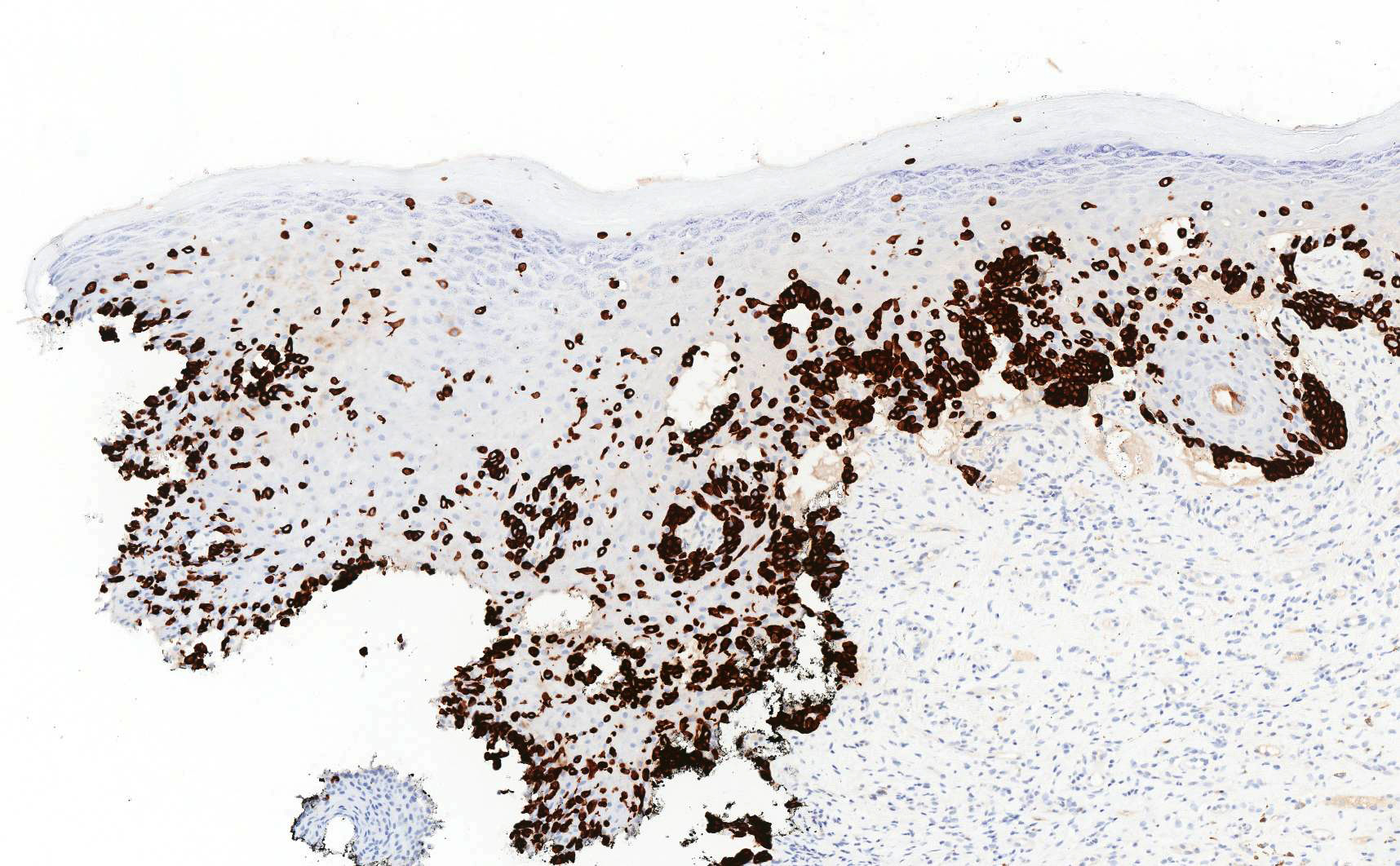
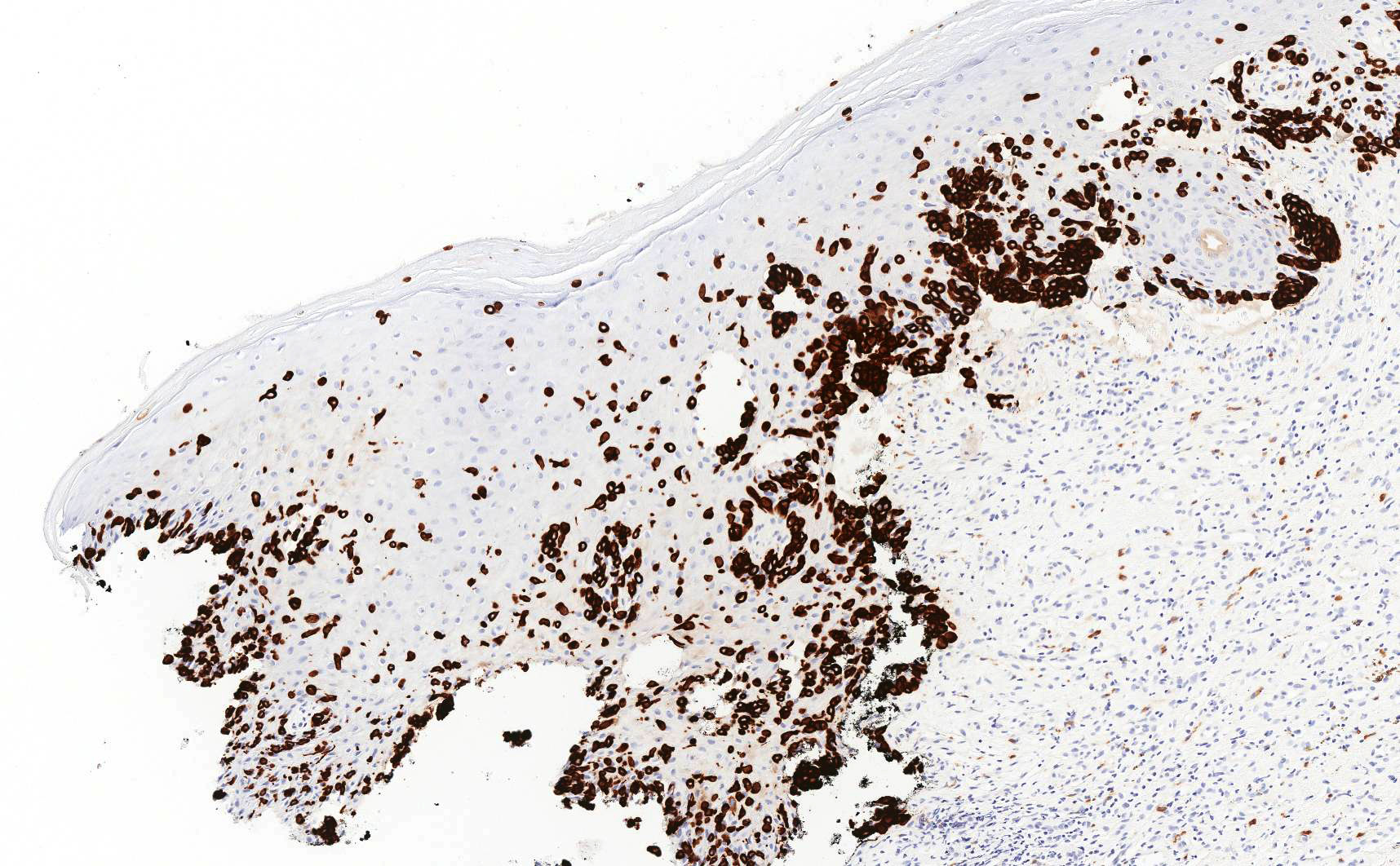
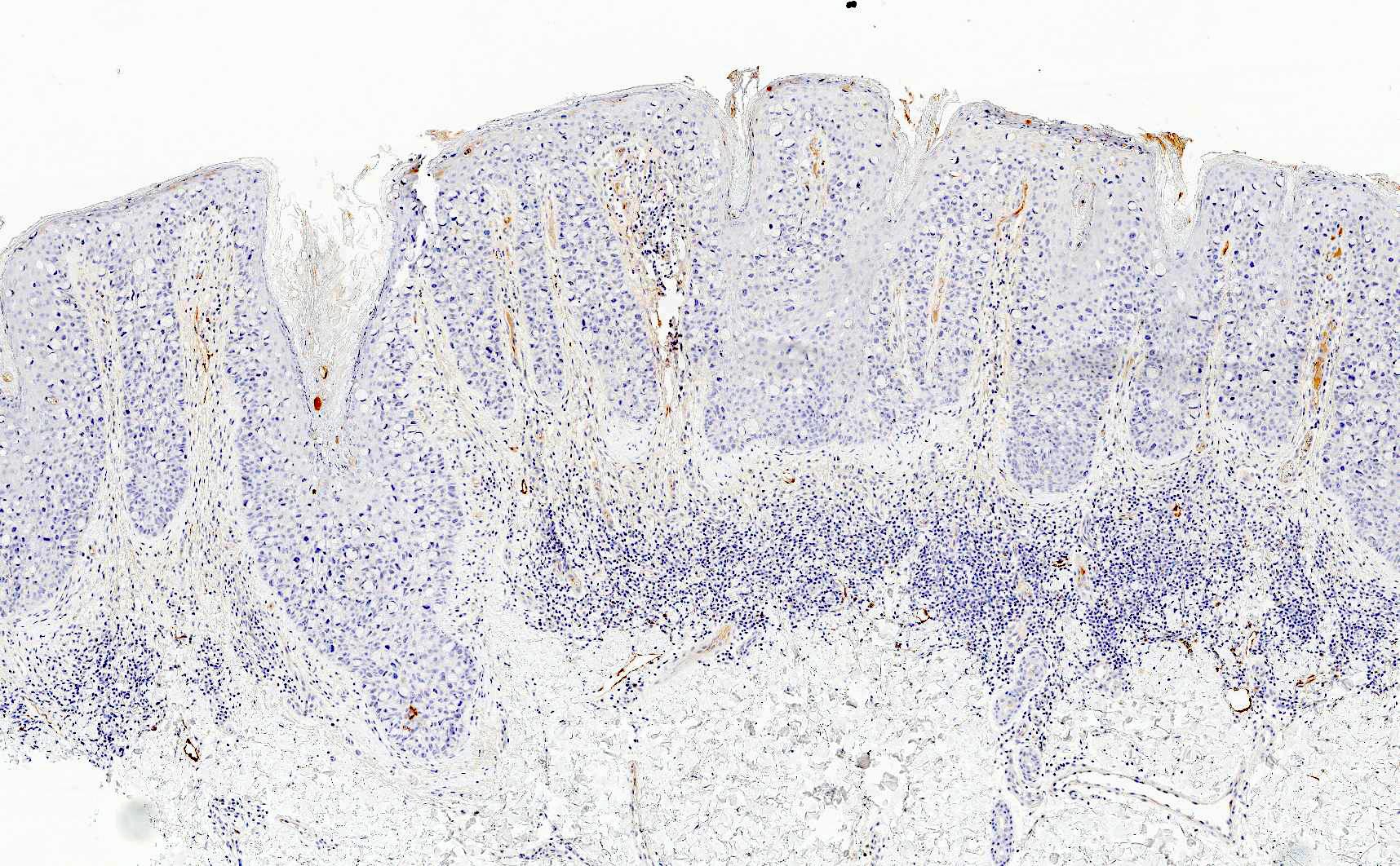
Microscopic (histologic) images
Contributed by Priya Nagarajan, M.D., Ph.D. and Lucy Ma, M.D.
Virtual slides
Cytology description
- Round to columnar, moderately enlarged atypical cells, dispersed or in loose groups, with abundant clear cytoplasm, vesicular nuclei and prominent nucleoli (Acta Cytol 2010;54:1007, Acta Cytol 2010;54:898, Diagn Cytopathol 2010;38:127)
- Nuclei can appear compressed due to vacuoles in the cytoplasm
Positive stains
- Primary and secondary Paget disease: CAM 5.2, EMA, CEA, mucicarmine, periodic acid-Schiff (PAS)
- Primary Paget disease: CK7, GATA3, GCDFP-15, androgen receptor, p16 (weak to moderate) (Am J Clin Pathol 2000;113:572)
- Secondary Paget disease, anorectal primary: CK20, CDX2, SATB2
- Secondary Paget disease, urothelial primary: CK7, CK20, GATA3, uroplakin III, p63
- Secondary Paget disease, cervical primary: CK7, PAX8, p16 (block positive), high risk HPV ISH
Negative stains
- Primary and secondary Paget disease: HMB45, MelanA, SOX10, MITF, p63, p40, CK5/6, ER and PR (Am J Clin Pathol 2000;113:572)
- Primary Paget disease: CK20
- Secondary Paget disease, anorectal primary: CK7, GATA3, GCDFP-15, uroplakin III
- Secondary Paget disease, urothelial primary: GCDFP-15
- Secondary Paget disease, cervical primary: CK20, GATA3, GCDFP-15
Molecular / cytogenetics description
- Mutations RAS and RAF genes (19%) and in PIK3CA and AKT1 genes (35%) (Int J Cancer 2013;132:824, Am J Dermatopathol 2017;39:358)
- Hypermethylation of CDH1 gene, which encodes for protein E-cadherin (Int J Cancer 2013;132:824)
- ERBB2 amplification (although rate is less frequent than Paget disease of the breast) (J Low Genit Tract Dis 2023;27:40)
- Amplification at chromosome Xcent-q21 and 19 and loss at 10q24-qter, indicating that androgen receptor may play a role in the pathogenesis (Br J Dermatol 2005;153:290)
Videos
Extramammary Paget disease: 5 minute pathology pearls
Paget disease versus melanoma versus squamous cell carcinoma in situ
Sample pathology report
- Vulva, left, wide local excision:
- Invasive extramammary Paget disease
- Invasive tumor size: 13 mm
- Depth of invasion: 6 mm
- Lymphovascular invasion: present
- Margins are negative for invasive tumor; extramammary (in situ) Paget disease extensively involves the medial peripheral margin
- Vulva, right, biopsy:
- Extramammary Paget disease (see comment)
- Comment: On immunostains, the neoplastic cells are strongly positive for CK7 and CAM 5.2 and negative for SOX10, supporting the diagnosis.
Differential diagnosis
- Melanoma in situ:
- Vulvar intraepithelial neoplasia (VIN), HPV associated and HPV independent:
- Sebaceous carcinoma:
- Tumor cells show multiple cytoplasmic vacuoles, which characteristically indent the nuclei
- CEA and GCDFP-15 negative
- Adipophilin and perilipin positive (due to the lipid content)
- Pagetoid dyskeratosis:
- Clear cells of Toker:
- CK7 positive but lacks cytologic atypia
- Not associated with clinical findings
- Clear cell papulosis:
- Generally seen in children (rarely in adults)
- Lacks cytologic atypia and mitoses
Additional references
Practice question #1
A vulvar biopsy reveals large polyhedral cells with large nuclei and pale cytoplasm trickling through the epidermis. Immunohistochemistry reveals that the tumor cells are positive for CK7, CK20, uroplakin III and p63. The tumor cells are negative for GCDFP-15, ER and PR. What is the best diagnosis?
- Primary extramammary Paget disease
- Secondary Paget disease, likely associated with breast carcinoma
- Secondary Paget disease, likely associated with rectal carcinoma
- Secondary Paget disease, likely associated with urothelial carcinoma
Practice answer #1
D. Secondary Paget disease, likely associated with urothelial carcinoma. Vulvar Paget disease secondary to urothelial carcinoma is positive for CK7, CK20, uroplakin III and p63. Answer A is incorrect because primary Paget disease of the vulva would be negative for uroplakin III and CK20. It is, however, positive for CK7. Answer C is incorrect because vulvar Paget disease secondary to anorectal carcinoma is generally negative for CK7 and uroplakin III. It is, however, positive for CK20. Answer B is incorrect because vulvar Paget disease secondary to breast carcinoma would be exceedingly rare. If such an entity were to occur, it would not be positive for uroplakin III and it would be unlikely for it to be positive for CK20; it could be CK7 positive.
Comment Here
Reference: Vulva & vagina - Paget disease
Comment Here
Reference: Vulva & vagina - Paget disease
Practice question #2
A 66 year old woman presents with a pruritic plaque on the right labia majora of 2 years duration. She has no significant oncologic history. As her symptoms have not improved, a punch biopsy is performed (image shown above). A mucicarmine stain is positive within the tumor cells. Which of the following ancillary stains would also likely be positive in this tumor?
- CK5/6
- CK7
- High risk HPV in situ hybridization
- HMB45
Practice answer #2
B. CK7. Given the history of a pruritic lesion of years in duration, along with the microscopic image of mucicarmine positive cells percolating through the epidermis, the diagnosis is most likely extramammary Paget disease, which is strongly CK7 positive. Answer D is incorrect because while melanoma is certainly in the differential diagnosis given the microscopic image, it would not be consistent with mucicarmine positivity; therefore, HMB45, a melanoma marker, is incorrect. Answer C is incorrect because while in theory high risk HPV ISH could potentially be positive in Paget disease of the vulva secondary to a HPV dependent cervical adenocarcinoma, primary vulvar Paget disease is far more common. Answer A is incorrect because CK5/6 is a high molecular weight cytokeratin, which stains squamous cells, not glandular cells.
Comment Here
Reference: Vulva & vagina - Paget disease
Comment Here
Reference: Vulva & vagina - Paget disease