Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Choschzick M. HPV associated squamous cell carcinoma-vulva. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvascc.html. Accessed April 25th, 2024.
Definition / general
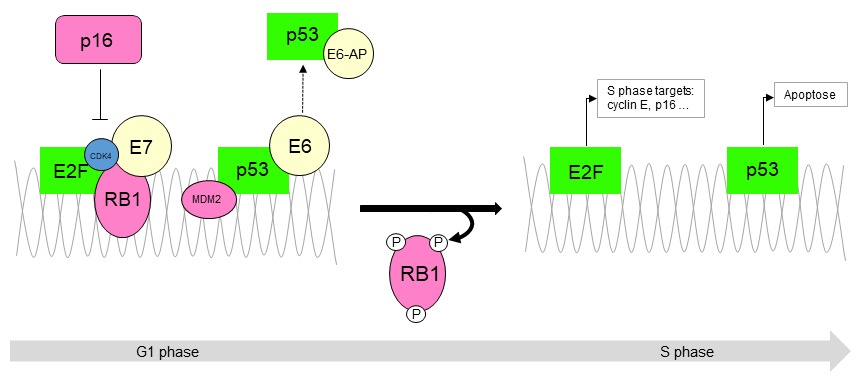
- Stromal invasive squamous cell carcinoma with immunohistochemically or molecularly verified association with human papillomavirus (HPV)
Essential features
- Stromal invasive squamous cell carcinoma
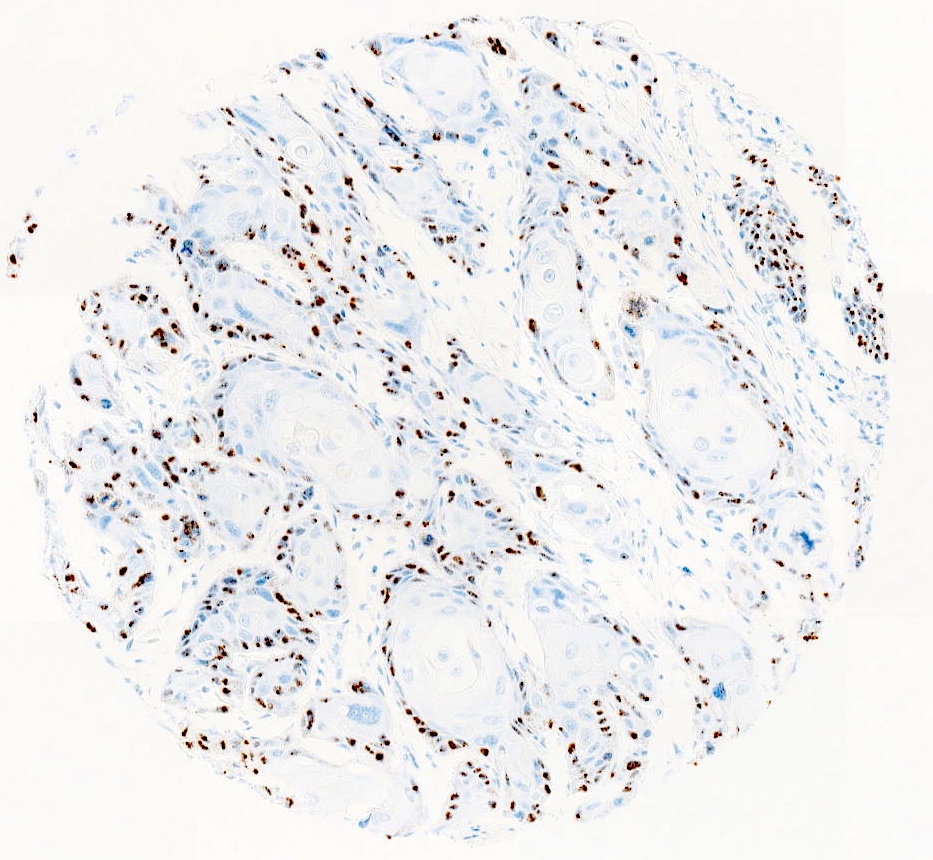
- p16 block type positivity or positive molecular testing (PCR or ISH) for HPV
- Coincident HPV associated vulvar intraepithelial neoplasia (VIN) (desirable)
ICD coding
- ICD-O: 8085/3 - squamous cell carcinoma, HPV positive
- ICD-10: C51 - malignant neoplasm of vulva
- ICD-11: 2C70.2 & XH0EJ7 - squamous cell carcinoma of vulva & squamous cell carcinoma, HPV positive
Epidemiology
- ~25 - 33% of all vulvar squamous cell carcinomas (Lancet Glob Health 2020;8:e180)
- Highest incidence in seventh decade but also younger patient ages
- HPV 16 is the most commonly associated virus subtype (Int J Cancer 2017;141:1161)
- > 90% of vulvar squamous cell carcinomas in sub-Saharan Africa are HPV associated (Int J Cancer 2023;152:496)
Sites
- All parts of the vulva including labia majora and minora, clitoris (midline carcinomas), vestibule, introitus
Etiology
- Human papillomaviruses: mostly high risk HPV 16 followed by HPV 33; very rare low risk HPV 6 and 11 (Lancet Oncol 2023;24:403)
Clinical features
- Risk factors: smoking, immunodeficiency
Diagnosis
- Punch biopsy, vulvectomy specimen
Prognostic factors
- Outcome of HPV associated vulvar squamous cell carcinoma (VSCC) is favorable compared to HPV independent VSCC (Int J Cancer 2018;142:1158, Histopathology 2017;71:238)
- 5 year overall survival: 59 - 89%
- Stage (tumor size and invasion depth) and lymph node status are the main prognostic factors (Semin Diagn Pathol 2021;38:37)
Case reports
- 22 year old woman with HPV positive squamous cell carcinoma of the vulva (Gynecol Oncol Rep 2021:36:100760)
- 58 year old woman with warty squamous cell carcinoma and condylomata acuminata (Med Arch 2017;71:72)
- 63 year old woman with combined squamous cell carcinoma and Merkel cell carcinoma (JAAD Case Rep 2015;1:196)
Treatment
- Wide local excision, partial or total vulvectomy depending on stage and patient condition (J Natl Compr Canc Netw 2017;15:121)
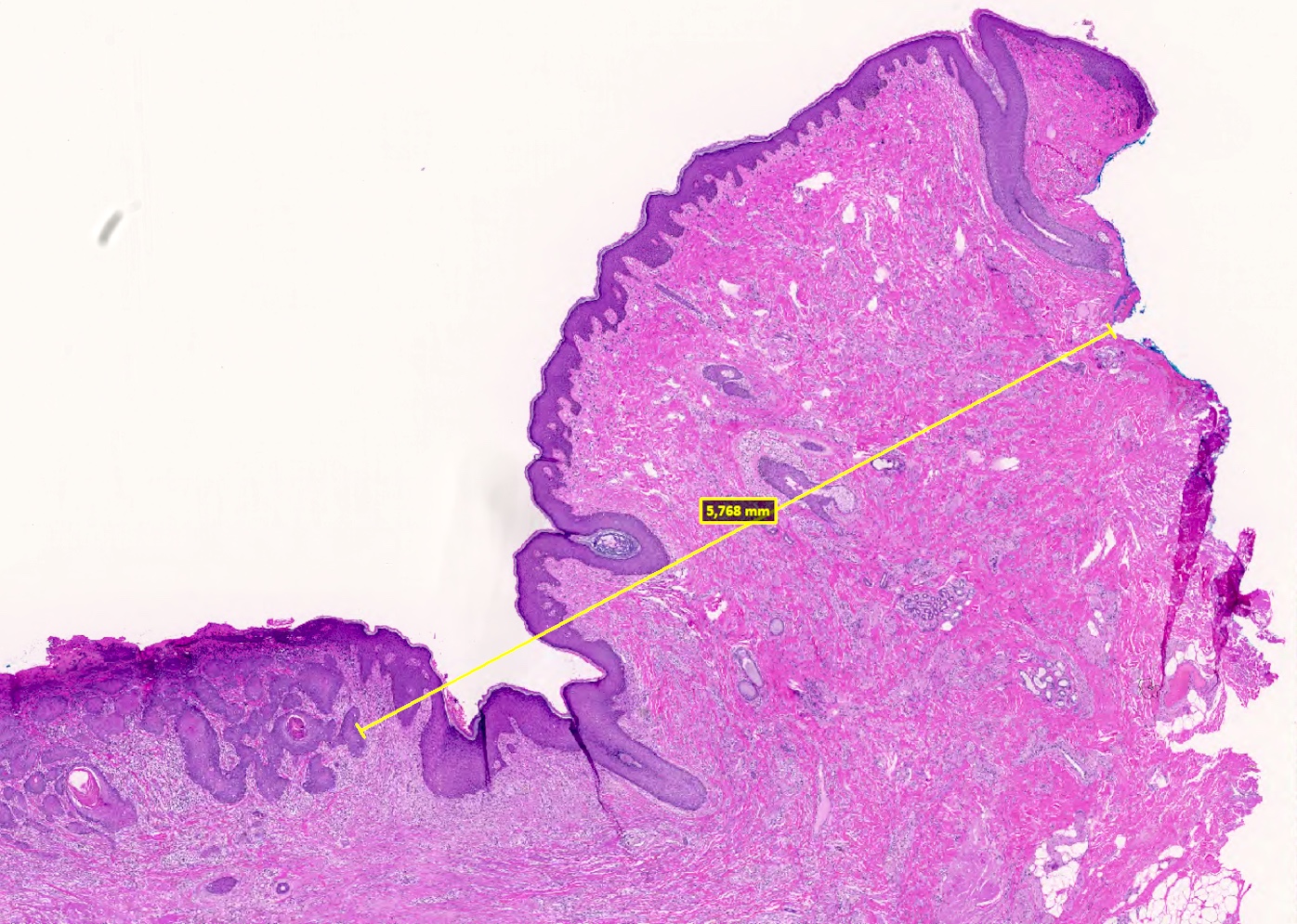
Gross description
- Exophytic mass or ulcerated lesion, frequently multifocal
- Tumor diameter should be measured in millimeters parallel to the skin surface
Microscopic (histologic) description
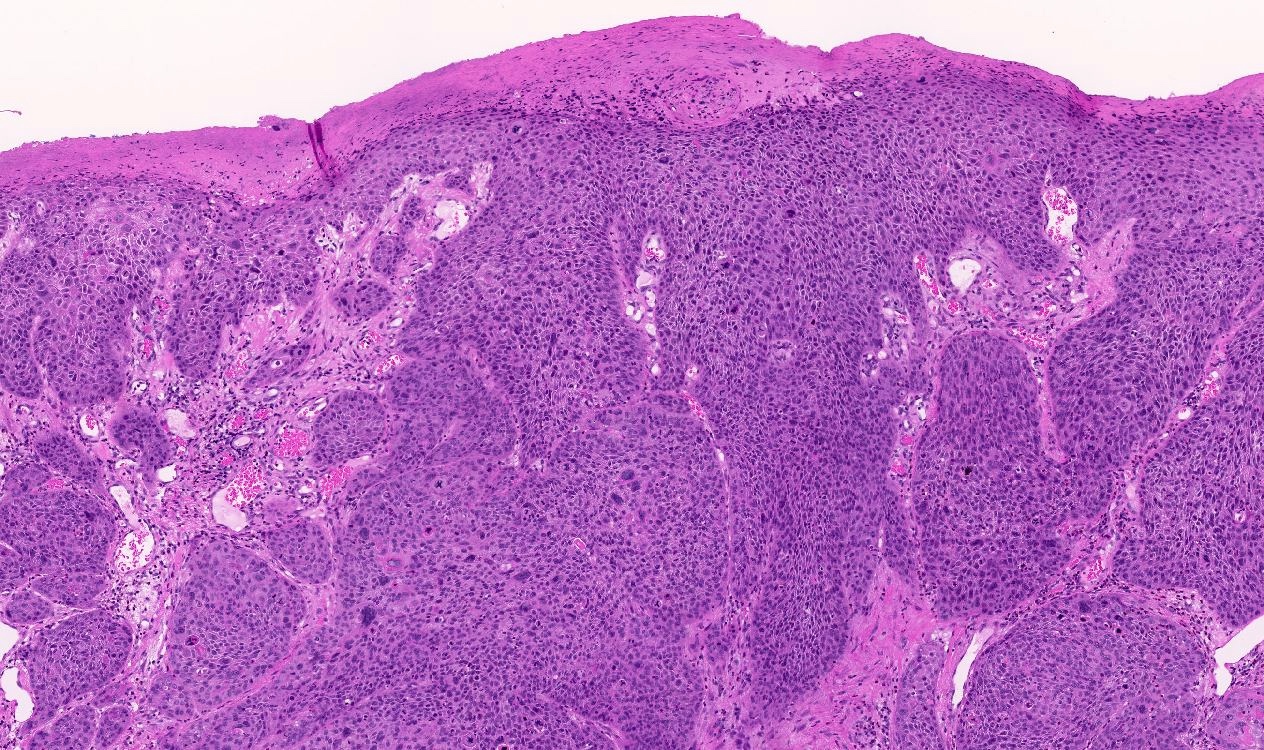
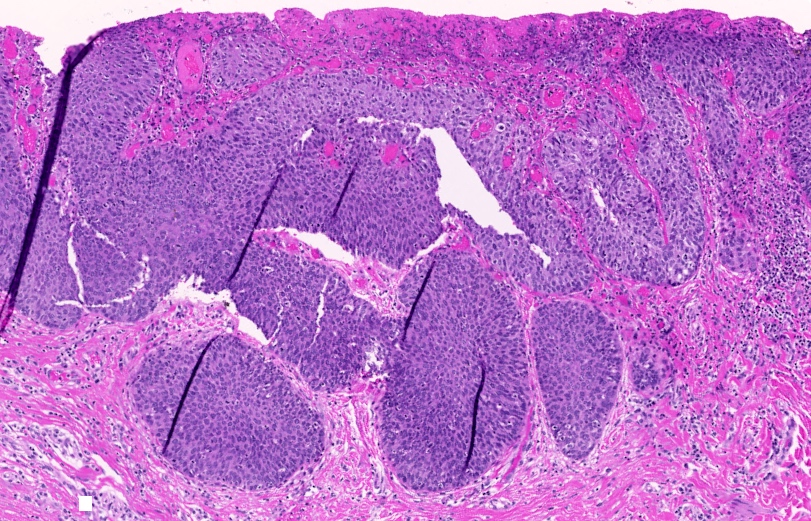
- Morphologic variants: keratinizing (~33%, most common), nonkeratinizing, basaloid, warty / condylomatous type (Int J Cancer 2017;141:2517)
- Basaloid and warty type are more frequent in HPV associated squamous cell carcinomas than in HPV independent tumors (blue appearance)
- Rare verrucous and spindle cell differentiation
- Frequent necrosis, koilocytic changes and nuclear pleomorphism
- There is no established grading system
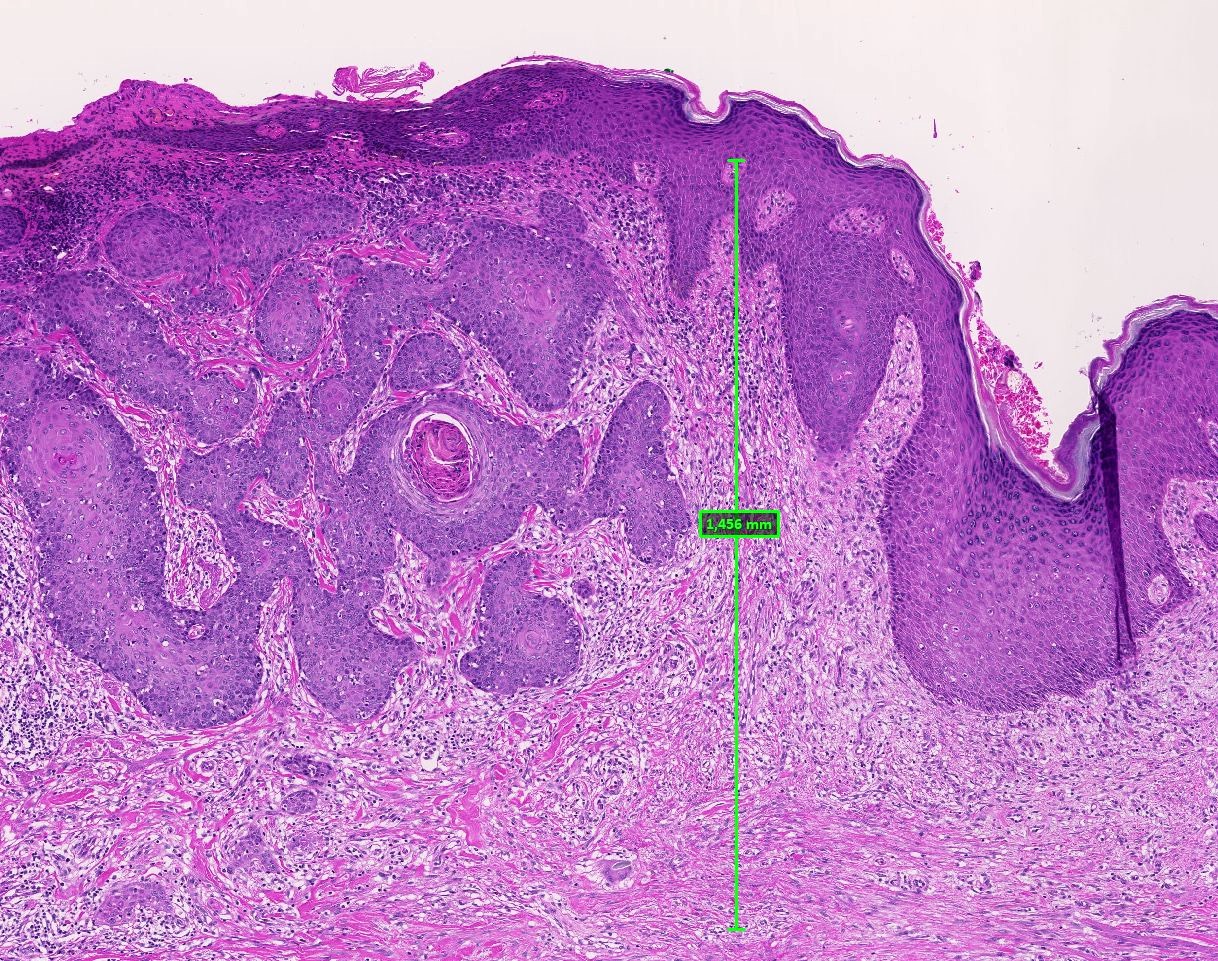
- Measurement of tumor invasion depth is as follows
- Union for International Cancer Control (UICC): from the tip of the nearest most superficial dermal papilla to the deepest tumor deposit
- International Federation of Gynecology and Obstetrics (FIGO): from the deepest adjacent dysplastic rete ridge to the deepest point of tumor invasion
- FIGO staging may downstage some tumors from IB to IA
- Surgical margin is measured from the peripheral edge of tumor straight to the nearest epithelial or stromal margin through tissue (Int J Gynecol Pathol 2020;39:420)
Microscopic (histologic) images
Negative stains
- p53 wild type pattern
Sample pathology report
- Vulva, wide local excision:
- Poorly differentiated basaloid squamous cell carcinoma (HPV associated) (see synoptic report)
- Comment: p16 IHC block-like positive
Differential diagnosis
- HPV independent squamous cell carcinoma:
- Frequently, keratinizing squamous cell carcinomas but significant overlap with morphologically identical HPV associated carcinomas
- HPV independent carcinomas are usually p16 negative with mutation type p53 expression in most cases
- VIN with tangential section or extension in adnexal structures:
- Regular tumor cell infiltrates with smooth outline, evidence of cross sectioning, adnexal structures with VIN, no single cells, no desmoplastic stroma, no paradoxical maturation
- Loose inflammatory infiltrates are common
Additional references
Board review style question #1
Board review style answer #1
D. p16. IHC for p16 shows highest specificity and sensitivity for HPV association. Answers A, B, C and E are incorrect because they are not relevant for verification of HPV association.
Comment Here
Reference: HPV associated squamous cell carcinoma-vulva
Comment Here
Reference: HPV associated squamous cell carcinoma-vulva
Board review style question #2
International Federation of Gynecology and Obstetrics (FIGO) and Union for International Cancer Control (UICC) have decided to use different instructions for measurement of infiltration depth in vulvar carcinomas. Which histomorphological structure is important for the measurement of tumor infiltration depth according UICC?
- Basal cell layer
- Dermal papilla
- Rete ridge
- Surface epidermis
- Tumor surface
Board review style answer #2
B. Dermal papilla. According to UICC, the infiltration depth of vulvar carcinomas should be measured from the top of the nearest dermal papilla to the deepest tumor cell infiltrate. Answer A is incorrect because VIN plays no role in this relation. Answer D is incorrect because the epidermial surface is not relevant for infiltration depth. Answer C is incorrect because rete ridges are important for FIGO staging. Answer E is incorrect because tumor surface is relevant for the measurement of tumor thickness.
Comment Here
Reference: HPV associated squamous cell carcinoma-vulva
Comment Here
Reference: HPV associated squamous cell carcinoma-vulva